Key Points
Question
Is hypertension in young adults, defined according to the 2017 American College of Cardiology/American Heart Association blood pressure guidelines, associated with the development of subsequent cardiovascular disease?
Findings
In this nationwide cohort study of 2 488 101 Koreans aged 20 through 39 years, stage 1 hypertension (systolic blood pressure, 130-139 mm Hg or diastolic blood pressure, 80-89 mm Hg) was associated with an increased risk of subsequent cardiovascular disease (hazard ratio, 1.25 for men; 1.27 for women).
Meaning
Young adults with stage 1 hypertension may be at increased risk for cardiovascular disease.
Abstract
Importance
Among young adults, the association of the 2017 American College of Cardiology/American Heart Association (ACC/AHA) High Blood Pressure Clinical Practice Guidelines with risk of cardiovascular disease (CVD) later in life is uncertain.
Objective
To determine the association of blood pressure categories before age 40 years with risk of CVD later in life.
Design, Setting, and Participants
This population-based cohort study from the Korean National Health Insurance Service consisted of 2 488 101 adults aged 20 through 39 years with blood pressure measurements taken twice from 2002 through 2005. Starting from January 1, 2006, participants were followed up until the date of CVD diagnosis, death, or December 31, 2015.
Exposures
Participants were categorized by blood pressure readings: normal (systolic, <120 mm Hg; diastolic, <80 mm Hg), elevated (sytolic, 120-129 mm Hg; diastolic, <80 mm Hg), stage 1 hypertension (systolic, 130-139 mm Hg; diastolic, 80-89 mm Hg), and stage 2 hypertension (systolic, ≥140 mm Hg; diastolic, ≥90 mm Hg).
Main Outcomes and Measures
The primary outcome was CVD defined as 2 or more days of hospitalization due to CVD or death due to CVD. The secondary outcomes were coronary heart disease (CHD) and stroke.
Results
The study population consisted of 2 488 101 participants (median age, 31 years [interquartile range, 27-36 years], 789 870 women [31.7%]). A total of 44 813 CVD events were observed during a median follow-up duration of 10 years. Men with baseline stage 1 hypertension compared with those with normal blood pressure had higher risk of CVD (incidence, 215 vs 164 per 100 000 person-years; difference, 51 per 100 000 person-years [95% CI, 48-55]; adjusted hazard ratio [HR], 1.25 [95% CI, 1.21-1.28]), CHD (incidence, 134 vs 103 per 100 000 person-years; difference, 31 per 100 000 person-years [95% CI, 28-33]; adjusted HR, 1.23 [95% CI, 1.19-1.27]), and stroke (incidence, 90 vs 67 per 100 000 person-years; difference, 23 per 100 000 person-years [95% CI, 21-26]; adjusted HR, 1.30 [95% CI, 1.25-1.36]). Women with baseline stage 1 hypertension compared with those with normal blood pressure had increased risk of CVD (incidence, 131 vs 91 per 100 000 person-years; difference, 40 per 100 000 person-years [95% CI, 35-45]; adjusted HR, 1.27 [95% CI, 1.21-1.34]), CHD (incidence, 56 vs 42 per 100 000 person-years; difference, 14 per 100 000 person-years [95% CI, 11-18]; adjusted HR, 1.16 [95% CI, 1.08-1.25]), and stroke (incidence, 79 vs 51 per 100 000 person-years; difference, 28 per 100 000 person-years [95% CI, 24-32]; adjusted HR [1.37, 95% CI, 1.29-1.46]). Results for state 2 hypertension were consistent.
Conclusions and Relevance
Among Korean young adults, stage 1 and stage 2 hypertension, compared with normal blood pressure, were associated with increased risk of subsequent cardiovascular disease events. Young adults with hypertension, defined by the 2017 ACC/AHA criteria, may be at increased risk of cardiovascular disease.
This population-based cohort study uses a national insurance database data to estimate long-term rates of cardiovascular disease among young Korean adults with elevated blood pressure and stage 1 and 2 hypertension defined by the 2017 ACC/AHA High Blood Pressure Clinical Practice Guideline.
Introduction
Hypertension is an important modifiable risk factor for cardiovascular disease (CVD).1 The population-attributable fraction of hypertension for CVD is approximately 60% in Asia.2,3 In 2017, the American College of Cardiology/American Heart Association (ACC/AHA) released an updated guideline with a new criteria for hypertension, defining stage 1 hypertension as systolic blood pressure as 130 mm Hg through 139 mm Hg or diastolic blood pressure as 80 mm Hg through 89 mm Hg.4 This lower threshold for hypertension was based on multiple meta-analyses that showed higher CVD risk in the stage 1 hypertension blood pressure range.5,6,7,8,9,10,11 However, most of the study populations from these studies were composed of middle-aged and elderly adults, leaving a relative lack of evidence for young adults aged 20 through 39 years.
Although previous cohort studies have investigated the association of blood pressure with CVD among young adults, such studies were limited to men and lacked consideration of certain confounders such as health behaviors or characteristics.12,13,14 Moreover, while the prevalence of hypertension among young adults has increased, hypertension awareness and management levels have nevertheless been low. For example, hypertension prevalence increased from 7.5% to 10.3% during years 2007 to 2016, whereas awareness and treatment levels for hypertension remained less than 20% among young adults aged 30 through 39 years in South Korea.15 Therefore, the lack of sufficient evidence on whether hypertension, particularly according to the stricter 2017 ACC/AHA criteria, is associated with higher CVD risk among young adults and the increasing prevalence of hypertension in this age group indicate that further studies are needed to investigate the association of blood pressure with CVD among young adults.
This nationwide population-based study aimed to investigate the association of blood pressure categories according to the 2017 ACC/AHA guidelines with the risk of CVD among 2.4 million young adults using the Korean National Health Insurance Service (NHIS) database.
Methods
Study Population
The Seoul National University Hospital Institutional Review Board approved this study (IRB number: 1703-039-836) and the requirement for informed consent was waived because the NHIS database was constructed after anonymization according to strict confidentiality guidelines.
The NHIS provides mandatory health care for all Korean citizens, with an enrollment rate of 97%. The NHIS collects data from all hospital use including admission and outpatient visit records, drug prescriptions, and national health examination data. Adults aged 20 through 39 years, who are employee-insured or self-employed are required to undergo health examinations biannually, as provided by the NHIS.16 The health examination includes a self-reported questionnaire on health behaviors, measurements of height, weight, and blood pressure, and laboratory tests for urine and blood. The NHIS provides information from the claims data for research purposes, which include all of the above-mentioned information along with death records of cause of death and death date merged from the Statistics Korea database. The NHIS database has previously been used for epidemiological studies, and its validity is described elsewhere.16
Key Variables
Blood pressure was measured after participants rested for at least 2 minutes in sitting position by digital or automatic monitors during the health examination. For the main analysis, blood pressure measured nearest to the index date of January 1, 2006, was used. All participants were categorized by blood pressure measures: normal (systolic, <120 mm Hg; diastolic, <80 mm Hg), elevated (systolic, 120-129 mm Hg; diastolic, <80 mm Hg), stage 1 hypertension (systolic 130-139 mm Hg; diastolic, 80-89 mm Hg), and stage 2 hypertension (systolic, ≥140 mm Hg; diastolic, ≥90 mm Hg). Furthermore, the mean blood pressure levels from the first (2002-2003) and second (2004-2005) health examination periods were also calculated. For the mean values, the blood pressure measurement closest to January 1, 2002, was used for the first period and measurement closest to January 1, 2006, was used for the second period.
The primary outcome was CVD, and secondary outcomes included coronary heart disease (CHD) and stroke. A CVD event was defined as 2 or more days of hospitalization or death due to the International Classification of Diseases, Tenth Revision (ICD-10) codes pertaining to CVD.17,18 Upon admission, the NHIS requires physicians to designate ICD-10 codes for which the patient was hospitalized. Furthermore, causes of death were also determined by ICD-10 codes determined by the attending physician. Cardiovascular disease (ICD-10 codes, I20-I25, I60-I69) was divided into CHD (ICD-10 codes, I20-I25) and stroke (ICD-10 codes, I60-I69) in accordance with the AHA guidelines.19
Statistical Analysis
Participants were followed-up from January 1, 2006, until the date of a CVD event, death, or December 31, 2015, whichever came first. The multivariable adjusted hazard ratios (HRs) and 95% CIs for CVD, CHD, and stroke were determined by Cox proportional hazards regression analysis according to blood pressure after adjustments for all covariates. The considered covariates included age (continuous, years), household income (categorical, first, second, third, or fourth quartiles), smoking (categorical, never, past, and current smokers), physical activity (categorical, 0, 1-2, 3-4, 5-6, and 7 times per week), alcohol consumption (categorical, 0, <1, 1-2, 3-4, and ≥5 times per week), body mass index (BMI, continuous), fasting serum glucose (continuous, mg/dL), total cholesterol (continuous, mg/dL), and Charlson comorbidity index (continuous). Household income was determined according to the insurance premium, and body mass index, by dividing the weight in kilograms by height in meters squared. The proportional hazards assumption was graphically tested and verified using the Schoenfeld residual method. The assumption for proportionality was not violated. Participants with missing data on blood pressure or covariates were excluded from the final study population prior to analysis.
Starting from the index date of January 1, 2006, all participant prescription records were checked for antihypertensive prescriptions during outpatient department visits or hospitalizations until 2010. Participants with prescriptions for antihypertensive medications within the first 5 years of follow-up were categorized into those with antihypertensive medications. From this, a stratified analysis on the association of blood pressure with CVD according to subgroups of those prescribed antihypertensive medications during the first 5 years of follow-up was conducted, after which the subgroups were tested for interaction. Furthermore, CVD risk was determined using the mean blood pressure values during the first and second health examination measurements. The risk of blood pressure categories on CVD was determined with additive adjustments of covariates with 4 models. Stratified analyses of CVD for subgroups of age, BMI, fasting serum glucose levels, total cholesterol levels, and Charlson comorbidity index were conducted and compared using P values for interaction. Restricted cubic splines were constructed for adjusted HRs and 95% CIs according to blood pressure levels.20 In accordance with a previous study, 4 knots were placed at the fifth, 35th, 65th, and 95th percentiles of systolic or diastolic blood pressure.12,21
We defined 2-sided P values of <.05 as statistically significant. All data collection and statistical analyses were performed using SAS version 9.4 (SAS Institute Inc) and STATA version 14 (Stata Corp).
Results
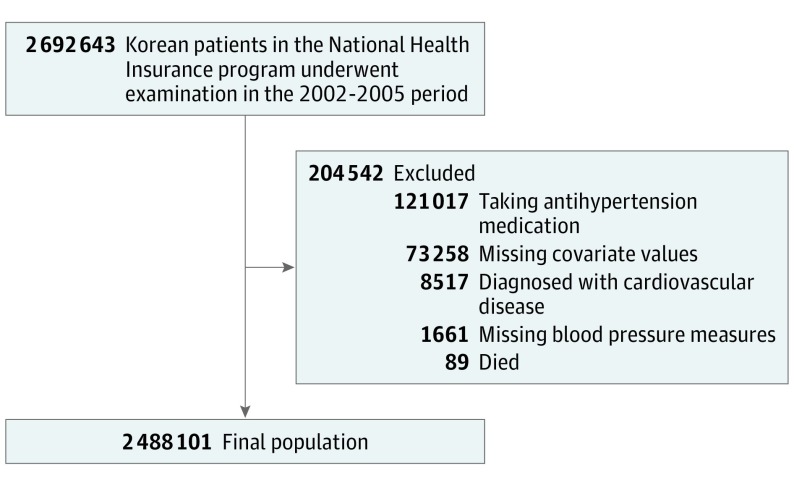
During the 2002-2005 period, 2 692 643 individuals aged 20 through 39 years underwent health examinations. Of those, 1661 participants (0.1%) with missing values for blood pressure and 73 258 (2.7%) with missing covariates were excluded. The 89 participants (<0.5%) who died and the 8517 (0.3%) who were diagnosed with CVD were also excluded; 121 017 participants (4.5%) who were prescribed antihypertensive medications were excluded, resulting in a final study population of 2 488 101 participants (Figure 1). eTable 1 in the Supplement shows the descriptive characteristics of the final study population and those excluded for being prescribed antihypertensives. Table 1 depicts the descriptive characteristics of the study population. The number of participants with normal blood pressure were 991 884; elevated blood pressure, 267 790; stage 1 hypertension, 938 908; and stage 2 hypertension, 289 519. The median follow-up duration was 10.0 years. Compared with normal individuals, those with stage 2 hypertension tended to be older, men, and current smokers, exercised more, consumed more alcohol, had higher BMI, and had higher fasting serum glucose and total cholesterol values.
Figure 1. Flow Diagram of the Study Population.
Table 1. Descriptive Characteristics of the Study Population.
| No. (%) of Patients, Systolic/Diastolic Blood Pressure Measures, mm Hg | ||||
|---|---|---|---|---|
| Normal, <120/<80 (n = 991 884) |
Elevated, 120-129/<80 (n = 267 790) |
Hypertension | ||
| Stage 1, 130-139/80-89 (n = 938 908) |
Stage 2, ≥140/≥90 (n = 289 519) |
|||
| Age, median (IQR), y | 30 (26-35) | 31 (27-35) | 32 (28-36) | 33 (29-36) |
| Sex | ||||
| Men | 497 673 (50.2) | 194 493 (72.6) | 747 362 (79.6) | 259 303 (89.6) |
| Women | 494 211 (49.8) | 73 297 (27.4) | 191 546 (20.4) | 30 216 (10.4) |
| Blood pressure, mean (SD), mm Hg | ||||
| Systolic | 107.1 (7.1) | 122.1 (2.8) | 124.7 (7.7) | 139.4 (11.5) |
| Diastolic | 67.2 (5.8) | 71.0 (4.2) | 80.3 (3.8) | 91.0 (7.6) |
| Household income, quartiles | ||||
| First (highest) | 281 773 (28.4) | 79 736 (29.8) | 286 747 (30.5) | 89 611 (31.0) |
| Second | 353 947 (35.7) | 96 931 (36.2) | 344 984 (36.7) | 105 382 (36.4) |
| Third | 236 872 (23.9) | 59 050 (22.1) | 198 157 (21.1) | 56 864 (19.6) |
| Fourth (lowest) | 119 292 (12.0) | 32 073 (12.0) | 109 020 (11.6) | 37 662 (13.0) |
| Smoking | ||||
| Never | 656 357 (66.2) | 139 153 (52.0) | 449 007 (47.8) | 116 710 (40.3) |
| Past | 80 280 (8.1) | 30 379 (11.3) | 112 652 (12.0) | 38 559 (13.3) |
| Current | 255 247 (25.7) | 98 258 (36.7) | 377 249 (40.2) | 134 250 (46.4) |
| Physical activity, times/wk | ||||
| 0 | 555 338 (56.0) | 130 029 (48.6) | 446 897 (47.6) | 125 761 (43.4) |
| 1-2 | 293 433 (29.6) | 92 043 (34.4) | 334 115 (35.6) | 112 845 (39.0) |
| 3-4 | 100 685 (10.2) | 31 791 (11.9) | 111 356 (11.9) | 36 158 (12.5) |
| 5-6 | 19 374 (2.0) | 6249 (2.3) | 20 861 (2.2) | 6449 (2.2) |
| 7 | 23 054 (2.3) | 7678 (2.9) | 25 679 (2.7) | 8306 (2.9) |
| Alcohol consumption, times/wk | ||||
| 0 | 453 716 (45.7) | 97 418 (36.4) | 311 922 (33.2) | 75 390 (26.0) |
| <1 | 284 608 (29.7) | 78 536 (29.3) | 261 041 (27.8) | 75 009 (25.9) |
| 1-2 | 208 080 (21.0) | 73 444 (27.4) | 285 507 (30.4) | 103 376 (35.7) |
| 3-4 | 38 795 (3.9) | 15 724 (5.9) | 68 529 (7.3) | 30 082 (10.4) |
| ≥5 | 6685 (0.7) | 2668 (1.0) | 11 909 (1.3) | 5662 (2.0) |
| Body mass index, mean (SD)a | 22.0 (2.9) | 23.2 (3.0) | 23.7 (3.1) | 25.1 (3.4) |
| <18.5 | 89 596 (9.0) | 11 446 (4.3) | 31 605 (3.4) | 4156 (1.4) |
| 18.5-22.9 | 561 240 (56.6) | 120 400 (45.0) | 362 549 (38.6) | 72 581 (25.1) |
| 23.0-24.9 | 189 389 (19.1) | 65 887 (24.6) | 236 026 (25.1) | 69 019 (23.8) |
| ≥25.0 | 151 659 (15.3) | 70 057 (26.2) | 308 728 (32.9) | 143 763 (49.7) |
| Fasting serum glucose, mean (SD), mg/dL | 87.9 (15.7) | 90.3 (17.3) | 91.1 (19.0) | 94.4 (23.4) |
| <100.0 | 847 090 (86.4) | 217 601 (81.3) | 747 360 (79.6) | 209 958 (72.5) |
| 100.0-125.9 | 123 352 (12.4) | 45 201 (16.9) | 168 521 (18.0) | 66 669 (23.0) |
| ≥126.0 | 11 442 (1.2) | 4988 (1.9) | 23 027 (2.5) | 12 892 (4.5) |
| Total cholesterol, mean (SD), mg/dL | 180.3 (35.9) | 185.4 (37.9) | 189.9 (39.2) | 197.9 (42.1) |
| <200.0 | 746 782 (75.3) | 186 279 (69.6) | 604 396 (64.4) | 160 001 (55.3) |
| 200.0-239.9 | 199 791 (20.1) | 65 006 (24.3) | 259 476 (27.6) | 94 193 (32.5) |
| ≥240.0 | 45 311 (4.6) | 16 505 (6.2) | 75 036 (8.0) | 35 325 (12.2) |
| Charlson Comorbidity indexb | ||||
| 0 | 493 932 (49.8) | 139 302 (52.0) | 498 502 (53.1) | 161 117 (55.7) |
| 1 | 354 833 (35.8) | 92 170 (34.4) | 314 773 (33.5) | 91 673 (31.7) |
| ≥2 | 143 119 (14.4) | 36 318 (13.6) | 125 633 (13.4) | 36 729 (12.7) |
Abbreviation: IQR, interquartile range.
SI conversion factors: to convert cholesterol from mg/dL to mmol/L, multiply by 0.0259; fasting glucose from mg/dL to mmol/L, multiply by 0.0555.
Calculated as weight in kilograms divided by height in meters squared.
Charlson comorbidity index: range, 0 (no comorbidities) to 37 (multiple comorbidities).
Primary End Points
Cardiovascular disease outcomes, the primary end point, according to 2017 ACC/AHA guideline categories are shown in Table 2. A total of 44 813 CVD events occurred during follow-up. Compared with men with normal blood pressure, those with elevated blood pressure (incidence, 178 vs 164 per 100 000 person-years; difference, 14 per 100 000 person-years [95% CI, 8-20]; adjusted HR, 1.07 [95% CI 1.03-1.11]), stage 1 hypertension (incidence, 215 vs 164 per 100 000 person-years; difference, 51 per 100 000 person-years [95% CI, 48-55]; adjusted HR 1.25 [95% CI, 1.21-1.28]), and stage 2 hypertension (incidence, 336 vs 164 per 100 000 person-years; difference, 172 per 100 000 person-years [95% CI, 165-179]; adjusted HR, 1.76 [95% CI 1.70-1.81]) had elevated risk of CVD.
Table 2. Cardiovascular Disease Risk According to the 2017 ACC/AHA Guideline Hypertension Categories Among Young Adults.
| Systolic/Diastolic Blood Pressure Measures, mm Hga | ||||
|---|---|---|---|---|
| Normal, <120/<80 | Elevated, 120-129/<80 | Hypertension | ||
| Stage 1, 130-139/80-89 | Stage 2, ≥140/≥90 | |||
| Men | ||||
| Cardiovascular diseaseb | ||||
| Events | 8133 | 3442 | 16 027 | 8658 |
| Person-years | 4 956 470 | 1 936 762 | 7 438 815 | 2 576 789 |
| Incidence (events/100 000 person-years) | 164 | 178 | 215 | 336 |
| Adjusted HR (95% CI)c | 1 [Reference] | 1.07 (1.03-1.11) | 1.25 (1.21-1.28) | 1.76 (1.70-1.81) |
| Coronary heart diseased | ||||
| Events | 5086 | 2129 | 9883 | 5159 |
| Person-years | 4 932 594 | 1 927 079 | 7 395 062 | 2 555 118 |
| Incidence (events/100 000 person-years) | 103 | 110 | 134 | 202 |
| Adjusted HR (95% CI)c | 1 [Reference] | 1.05 (1.00-1.10) | 1.23 (1.19-1.27) | 1.68 (1.61-1.75) |
| Strokee | ||||
| Events | 3304 | 1424 | 6705 | 3882 |
| Person-years | 4 944 603 | 1 931 658 | 7 416 030 | 2 564 038 |
| Incidence (events/100 000 person-years) | 67 | 74 | 90 | 151 |
| Adjusted HR (95% CI)c | 1 [Reference] | 1.10 (1.03-1.17) | 1.30 (1.25-1.36) | 1.99 (1.90-2.09) |
| Women | ||||
| Cardiovascular diseaseb | ||||
| Events | 4483 | 830 | 2499 | 741 |
| Person-years | 4 931 236 | 731 171 | 1 910 506 | 301 010 |
| Incidence (events/100 000 person-years) | 91 | 114 | 131 | 246 |
| Adjusted HR (95% CI)c | 1 [Reference] | 1.13 (1.05-1.22) | 1.27 (1.21-1.34) | 1.85 (1.71-2.01) |
| Coronary heart diseased | ||||
| Events | 2085 | 356 | 1074 | 278 |
| Person-years | 4 920 920 | 729 405 | 1 905 383 | 299 719 |
| Incidence (events/100 000 person-years) | 42 | 49 | 56 | 93 |
| Adjusted HR (95% CI)c | 1 [Reference] | 1.04 (0.93-1.16) | 1.16 (1.08-1.25) | 1.46 (1.29-1.66) |
| Strokee | ||||
| Events | 2526 | 508 | 1513 | 487 |
| Person-years | 4 921 904 | 729 364 | 1 905 177 | 299 275 |
| Incidence (events/100 000 person-years) | 51 | 70 | 79 | 163 |
| Adjusted HR (95% CI)c | 1 [Reference] | 1.23 (1.12-1.36) | 1.37 (1.29-1.46) | 2.18 (1.97-2.41) |
Abbreviations: ACC/AHA, American College of Cardiology and American Heart Association; HR, hazard ratio.
Median follow-up for each category was 10 years.
Operational definition: hospitalization of 2 or more days or death due to coronary heart disease or stroke.
Hazard ratio calculated by Cox proportional hazards regression analysis after adjustments for age, household income, smoking, physical activity, alcohol consumption, body mass index, fasting serum glucose and total cholesterol levels, and Charlson comorbidity index.
Operational definition: hospitalization of 2 or more days or death due to coronary heart disease.
Operational definition: hospitalization of 2 or more days or death due to stroke.
Similarly, compared with women with normal blood pressure, those with elevated blood pressure (incidence, 114 vs 91 per 100 000 person-years; difference, 23 per 100 000 person-years [95% CI, 15-30]; adjusted HR, 1.13 [95% CI 1.05-1.22]), stage 1 hypertension (incidence, 131 vs 91 per 100 000 person-years; difference, 40 per 100 000 person-years [95% CI, 35-45]; adjusted HR, 1.27 [95% CI, 1.21-1.34]), and stage 2 hypertension (incidence, 246 vs 91 per 100 000 person-years; difference, 155 per 100 000 person-years [95% CI, 138-173]; adjusted HR, 1.85 [95% CI, 1.71-2.01]) had elevated risk of CVD.
Secondary End Points
Compared with normal blood pressure, men with stage 1 hypertension (incidence, 134 vs 103 per 100 000 person-years; difference, 31 per 100 000 person-years [95% CI, 28-33]; adjusted HR, 1.23 [95% CI 1.19-1.27]) and women with stage 1 hypertension (incidence, 56 vs 42 per 100 000 person-years; difference, 14 per 100 000 person-years [95% CI, 11-18]; adjusted HR, 1.16 [95% CI, 1.08-1.25]) had higher CHD risk. Similarly, men with stage 2 hypertension (incidence, 202 vs 103 per 100 000 person-years; difference, 99 per 100 000 person-years [95% CI, 94-105]; adjusted HR, 1.68 [95% CI, 1.61-1.75]) and women with stage 2 hypertension (incidence, 93 vs 42 per 100 000 person-years; difference, 51 per 100 000 person-years [95% CI, 40-62]; adjusted HR, 1.46 [95% CI, 1.29-1.66]) had higher CHD risk.
Similarly, stage 1 hypertension was associated with higher risk of stroke among men (incidence, 90 vs 67 per 100 000 person-years; difference, 23 per 100 000 person-years [95% CI, 21-26]; adjusted HR, 1.30 [95% CI, 1.25-1.36]). Stage 1 hypertension was also associated with higher risk of stroke among women (incidence, 79 vs 51 per 100 000 person-years; difference, 28 per 100 000 person-years [95% CI, 24-32]; adjusted HR, 1.37 [95% CI, 1.29-1.46]).
The trend of greater risk of stroke held true among men with stage 2 hypertension (incidence, 151 vs 67 per 100 000 person-years; difference, 84 per 100 000 person-years [95% CI, 80-89]; adjusted HR, 1.99 [95% CI, 1.90-2.09]). The trend of greater risk of stroke also held true for women with stage 2 hypertension (incidence, 163 vs 51 per 100 000 person-years; difference, 112 per 100 000 person-years [95% CI, 98-127]; adjusted HR, 2.18 [95% CI, 1.97-2.41]). The risk-increasing association of blood pressure categories with CVD was similar upon using mean blood pressure values (eTable 2 in the Supplement).
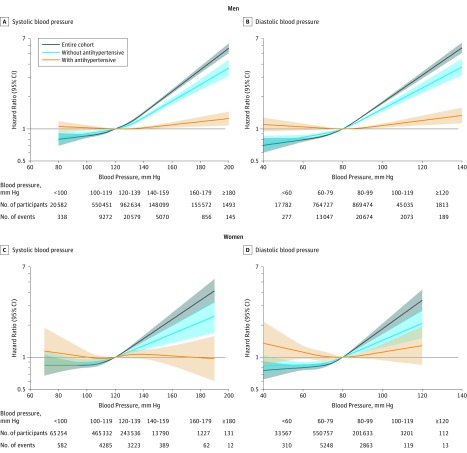
Table 3 depicts the stratified analysis on the association of 2017 ACC/AHA categories on CVD according to subgroups of antihypertensive medication prescribed within the first 5 years of follow-up. Although stage 1 hypertension was associated with higher risk of CVD among men without treatment (incidence, 167 vs 137 per 100 000 person-years; difference, 30 per 100 000 person-years [95% CI, 27-33]; adjusted HR, 1.17 [95% CI, 1.13-1.21]) as it was for women (incidence, 106 vs 81 per 100 000 person-years; difference, 25 per 100 000 person-years [95% CI, 20-30]; adjusted HR, 1.18 [95% CI, 1.12-1.25]), patients with stage 1 hypertension who were prescribed antihypertensive medications did not have increased CVD risk. The incidence for men was 706 vs 656 per 100 000 person-years (difference, 50 per 100 000 person-years [95% CI, 30-70]; adjusted HR, 1.03 [95% CI, 0.97-1.09]). The incidence for women was 562 vs 511 per 100 000 person-years (difference, 51 per 100 000 person-years [95% CI, 16-98]; adjusted HR, 1.02 [95% CI, 0.90-1.14]). There was a significant difference in the association of 2017 ACC/AHA categories on CVD according to subgroups of those with and without antihypertensive medication prescribed within the first 5 years of follow-up (P for interaction, <.001 for both men and women). Similar relationships were observed when restricted cubic splines were used to treat systolic and diastolic blood pressure as continuous variables for men and women (Figure 2).
Table 3. Stratified Analysis on the Association of the 2017 ACC/AHA Guideline Hypertension Categories on Cardiovascular Disease According to Subgroups of Antihypertensive Medication Prescription Within the First 5 Years of Follow-up.
| Systolic/Diastolic Blood Pressure Measures, mm Hg | ||||
|---|---|---|---|---|
| Normal, <120/<80 mm Hg | Elevated, 120-129/<80 mm Hg | Hypertension | ||
| Stage 1, 130-139/80-89 mm Hg | Stage 2, ≥140/≥90 mm Hg | |||
| Men | ||||
| Without antihypertensive medicationsa | ||||
| Events | 6445 | 2580 | 11 275 | 4486 |
| Person-years | 4 699 087 | 1 817 577 | 6 765 350 | 2 009 630 |
| Incidence (events/100 000 person-years) | 137 | 142 | 167 | 223 |
| Adjusted HR (95% CI)b | 1 [Reference] | 1.02 (0.98-1.07) | 1.17 (1.13-1.21) | 1.46 (1.41-1.52) |
| With antihypertensive medicationsa | ||||
| Events | 1688 | 862 | 4752 | 4172 |
| Person-years | 257 384 | 119 185 | 673 465 | 567 160 |
| Incidence (events/100 000 person-years) | 656 | 723 | 706 | 736 |
| Adjusted HR (95% CI)b | 1 [Reference] | 1.08 (0.99-1.18) | 1.03 (0.97-1.09) | 1.03 (0.97-1.09) |
| Women | ||||
| Without antihypertensive medicationsa | ||||
| Events | 3906 | 672 | 1914 | 408 |
| Person-years | 4 818 403 | 704 185 | 1 806 338 | 246 289 |
| Incidence (events/100 000 person-years) | 81 | 95 | 106 | 166 |
| Adjusted HR (95% CI)b | 1 [Reference] | 1.08 (0.99-1.17) | 1.18 (1.12-1.25) | 1.51 (1.36-1.68) |
| With antihypertensive medicationsa | ||||
| Events | 577 | 158 | 585 | 333 |
| Person-years | 112 833 | 26 986 | 104 168 | 54 721 |
| Incidence (events/100 000 person-years) | 511 | 585 | 562 | 609 |
| Adjusted HR (95% CI)b | 1 [Reference] | 1.10 (0.92-1.31) | 1.02 (0.90-1.14) | 1.04 (0.90-1.20) |
Abbreviation: ACC/AHA, American College of Cardiology and American Heart Association.
Antihypertensive medication prescription within the first 5 years of follow-up.
Hazard ratio calculated by Cox proportional hazards regression analysis after adjustments for age, household income, smoking, physical activity, alcohol consumption, body mass index, fasting serum glucose, total cholesterol, and Charlson comorbidity index.
Figure 2. Hazard Ratios for Cardiovascular Disease According to Index Blood Pressure Among Young Adults With and Without Stratification According to Antihypertensive Medication Prescription Within the First 5 Years of Follow-up.
Solid lines indicate hazard ratios and shaded areas indicate 95% CIs using restricted cubic spline regression. Without antihypertensive medication indicates that patients had not been prescribed antihypertensive medication within the first 5 years of follow-up; with antihypertensive medication indicates that they were prescribed antihypertensive medication within the first 5 years of follow-up. Restricted cubic splines were constructed with 4 knots placed at the fifth, 35th, 65th, and 95th percentiles. Hazard ratios were calculated by Cox proportional hazards regression analysis after adjustments for age, household income, physical activity, smoking, alcohol consumption, body mass index, fasting serum glucose and total cholesterol levels, and Charlson comorbidity index.
The association of systolic and diastolic blood pressure with CVD is shown in Figure 2. Systolic blood pressure higher than 120 mm Hg was associated with elevated CVD risk in a dose-responsive manner for both men and women. Similarly, diastolic blood pressure higher than 80 mm Hg was associated with increased risk of CVD for both men and women. The risk-increasing association of high blood pressure with CVD risk was preserved among unadjusted (eFigure 1 in the Supplement) and age-adjusted (eFigure 2 in the Supplement) models. The association of blood pressure categories with CVD risk according to additive adjustments of covariates is shown in eTable 3 in the Supplement. Compared with participants with normal blood pressure, those with stage 1 hypertension had an additional 5.1 and 3.9 CVD events per 1000 men and women, respectively (eTable 4 in the Supplement). Participants with stage 1 hypertension for all subgroups of age, BMI, fasting serum glucose, total cholesterol, and Charlson comorbidity index had higher risk of CVD than did those with normal blood pressure (eTable 5 in Supplement).
Discussion
In this nationwide population-based study of more than 2.4 million young adults, stage 1 hypertension according to the 2017 ACC/AHA guideline was associated with higher subsequent risk of CVD. This is the first study, to our knowledge, in a Korean population to show that stage 1 hypertension was associated with increased CVD risk among young men and women aged 20 to 39 years.
In 2017, the ACC/AHA issued a blood pressure management guideline with a new definition for hypertension starting from blood pressure of 130/80 mm Hg.4 Previously, hypertension was defined as blood pressure of 140/90 mm Hg or higher, while the systolic blood pressure ranging between 130 and 139 and diastolic blood pressure between 80 and 89 mm Hg had been defined as prehypertension.22 The 2017 ACC/AHA criteria was based on many large-scale studies that showed that the stage 1 hypertension blood pressure range was associated with higher CVD risk.23,24,25,26,27,28 For example, in an analysis including a total of 346 570 participants from 36 cohort studies, the stage 1 hypertension blood pressure range was associated with increased risk of CHD (adjusted HR,1.31; 95% CI, 1.14-1.50), ischemic stroke (adjusted HR, 1.60; 95% CI, 1.33-1.92), and hemorrhagic stroke (adjusted HR, 2.17; 95% CI, 1.69-2.79).29 Despite this, the 2018 European Guidelines for the management of arterial hypertension announced in August 2018 retained its existing hypertension definition of 140/90 mm Hg or higher.30 However, the results from this study give further support to the 2017 ACC/AHA guideline recommendations by showing that stage 1 hypertension was associated with higher CVD risk among young adults aged 20 through 39 years.
Results from previous studies that determined the association of blood pressure on CVD among young adults are in line with those from this study. In a study involving 9887 young men aged 15 through 29 years, it has been shown that every 10 mm Hg increase in systolic blood pressure was associated with an adjusted HR of 1.14 (95% CI, 1.05-1.23) for CVD mortality.14 Similarly, another study consisting of 10 874 men aged 18 through 39 years demonstrated that increases in 15 mm Hg of systolic blood pressure or 10 mm Hg of diastolic blood pressure were associated with an adjusted HR of 1.26 (95% CI, 1.11-1.44) or 1.17 (95% CI, 1.01-1.35) for CHD mortality, respectively.13 A nationwide cohort study involving 1 207 141 adolescent men showed that blood pressure higher than 120/80 mm Hg was associated increased risk of CVD mortality.12 However, previous studies were limited to men and lacked adjustments for certain potentially important confounders such as BMI, fasting serum glucose concentrations, or total cholesterol levels. This study not only included women but also demonstrated that the higher CVD risk associated with higher blood pressure was also true after adjustments for a wide range of covariates including BMI, fasting serum glucose, and total cholesterol, thus enhancing the generalizability of the results.
Participants with antihypertensive medication prescribed before the index date were excluded as the duration of hypertension since initial diagnosis or dose and types of antihypertensive medications prescribed may have effects on both blood pressure levels and CVD risk.31 Nevertheless, in an attempt to determine whether pharmacological management may be associated with a lower risk of CVD particularly among patients with stage 1 hypertension, a stratified analysis according to subgroups of antihypertensive medication prescription within the first 5 years of follow-up was conducted. Although patients with stage 1 hypertension not taking antihypertensive medications had higher risk of CVD, those who were prescribed antihypertensives did not have increased CVD risk compared with their respective normal blood pressure groups. Although this appears to suggest that early antihypertensive management of stage 1 hypertension even among young adults may be associated with reduced CVD risk, this result is subject to a number of potentially confounding factors such as differences in access to care and number of medical contacts. Therefore, future prospective studies are needed to validate these findings.
Although the absolute risks for CVD were lower in this age group than that of previous studies involving middle-aged and elderly adults,32 there were nevertheless increases in absolute risk for stage 1 hypertension compared with participants with normal blood pressure. Compared with those with normal blood pressure, men with stage 1 hypertension had additional 5.1 events and women, an additional 3.9 events per 1000. Therefore, despite the relatively low absolute risk, the difference in absloute risk and the fact that sustained hypertension during longer durations is associated with higher risk of CVD indicate that early blood pressure management among young adults may lead to significant public health benefits by reducing CVD risk later in life.
This study has a number of strengths. The large study population as well as the inclusion of women add to the reliability of the findings. Furthermore, a number of confounders, including household income, health behaviors, and health characteristics, and comorbidities were taken into account.
Limitations
This study has several limitations. First, blood pressure was measured only once and measurements were not conducted according to rigorous contemporary standards, which could lead to inaccurate blood pressure values. However, blood pressure measurement instruments in all health examination institutions receive quality assessment every 3 years according to the Basic Act on National Health Examination. Furthermore, because mean blood pressure calculated from repeated measurements may be better associated with CVD risk,33 we also used mean blood pressure measurements from 2 separate blood pressure values over a 2-year span and determined their association with CVD risk, the results of which were consistent with those from the main findings. Nevertheless, future studies that use other methods of blood pressure measurement are needed to validate the findings of this study, particularly since white coat hypertension has been reported to be prevalent among young adults.34 Second, the operational definition of CVD may be prone to misdiagnosis, as evidenced by the unusually higher rate of CHD compared with stroke among men and the low autopsy rate (1.9% of all deaths according to a report in 201335) in South Korea. Although the operational definition of CVD used in this study has been adopted from multiple previous studies using the same data source,17,18 future studies that use a more accurate definition of CVD are needed to validate these findings.
Third, the study population was from a single country, so the results may not necessarily be generalizable to people of other racial or ethnic backgrounds. Fourth, ischemic and hemorrhagic stroke could not be analyzed separately due to lack of data. Future studies that investigate the association of blood pressure on ischemic and hemorrhagic stroke are needed. Fifth, we did not take into account other CVD medications outside of antihypertensives that also lower blood pressure. Sixth, there was also no data available on adherence to reduced salt intake or other dietary recommendations, as well as type of physical activity, which may be important confounders in the association of blood pressure with CVD. Future studies that take into account a more comprehensive range of factors including CVD medications, dietary habits, and physical activity type are needed to validate the findings of this study.
Conclusions
Among Korean young adults, stage 1 and stage 2 hypertension, compared with normal blood pressure, were associated with increased risk of subsequent cardiovascular disease events. Young adults with hypertension, defined by the 2017 ACC/AHA criteria, may be at increased risk of cardiovascular disease.
eTable 1. Descriptive characteristics of the final study population and participants prescribed anti-hypertensive medication during 2002-2005.
eTable 2. Cardiovascular disease risk according to the 2017 ACC/AHA guideline hypertension categories from mean blood pressure values among young adults.
eFigure 1. Unadjusted risk for cardiovascular disease according to blood pressure among young adults.
eFigure 2. Age-adjusted risk for cardiovascular disease according to blood pressure among young adults.
eTable 3. Cardiovascular disease risk according to the 2017 ACC/AHA guideline hypertension categories among young adults with additive adjustments for covariates.
eTable 4. Absolute risk and difference in absolute risk of cardiovascular disease according to the 2017 ACC/AHA guideline hypertension categories among young adults.
eTable 5. Stratified analysis on cardiovascular disease risk according to the 2017 ACC/AHA guideline defined hypertension categories among young adults by subgroups of age, body mass index, fasting serum glucose, total cholesterol, and Charlson comorbidity index.
References
- 1.Mancia G, Fagard R, Narkiewicz K, et al. ; Task Force Members . 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31(7):1281-1357. doi: 10.1097/01.hjh.0000431740.32696.cc [DOI] [PubMed] [Google Scholar]
- 2.Ueshima H, Sekikawa A, Miura K, et al. . Cardiovascular disease and risk factors in Asia: a selected review. Circulation. 2008;118(25):2702-2709. doi: 10.1161/CIRCULATIONAHA.108.790048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martiniuk AL, Lee CM, Lawes CM, et al. ; Asia-Pacific Cohort Studies Collaboration . Hypertension: its prevalence and population-attributable fraction for mortality from cardiovascular disease in the Asia-Pacific region. J Hypertens. 2007;25(1):73-79. doi: 10.1097/HJH.0b013e328010775f [DOI] [PubMed] [Google Scholar]
- 4.Whelton PK, Carey RM, Aronow WS, et al. . 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCN: A guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):e13-e115. [DOI] [PubMed] [Google Scholar]
- 5.Guo X, Zhang X, Guo L, et al. . Association between pre-hypertension and cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Curr Hypertens Rep. 2013;15(6):703-716. doi: 10.1007/s11906-013-0403-y [DOI] [PubMed] [Google Scholar]
- 6.Huang Y, Cai X, Li Y, et al. . Prehypertension and the risk of stroke: a meta-analysis. Neurology. 2014;82(13):1153-1161. doi: 10.1212/WNL.0000000000000268 [DOI] [PubMed] [Google Scholar]
- 7.Huang Y, Cai X, Liu C, et al. . Prehypertension and the risk of coronary heart disease in Asian and Western populations: a meta-analysis. J Am Heart Assoc. 2015;4(2):e001519. doi: 10.1161/JAHA.114.001519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huang Y, Wang S, Cai X, et al. . Prehypertension and incidence of cardiovascular disease: a meta-analysis. BMC Med. 2013;11:177. doi: 10.1186/1741-7015-11-177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee M, Saver JL, Chang B, Chang KH, Hao Q, Ovbiagele B. Presence of baseline prehypertension and risk of incident stroke: a meta-analysis. Neurology. 2011;77(14):1330-1337. doi: 10.1212/WNL.0b013e3182315234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shen L, Ma H, Xiang MX, Wang JA. Meta-analysis of cohort studies of baseline prehypertension and risk of coronary heart disease. Am J Cardiol. 2013;112(2):266-271. doi: 10.1016/j.amjcard.2013.03.023 [DOI] [PubMed] [Google Scholar]
- 11.Wang S, Wu H, Zhang Q, Xu J, Fan Y. Impact of baseline prehypertension on cardiovascular events and all-cause mortality in the general population: a meta-analysis of prospective cohort studies. Int J Cardiol. 2013;168(5):4857-4860. doi: 10.1016/j.ijcard.2013.07.063 [DOI] [PubMed] [Google Scholar]
- 12.Sundström J, Neovius M, Tynelius P, Rasmussen F. Association of blood pressure in late adolescence with subsequent mortality: cohort study of Swedish male conscripts. BMJ. 2011;342:d643. doi: 10.1136/bmj.d643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miura K, Daviglus ML, Dyer AR, et al. . Relationship of blood pressure to 25-year mortality due to coronary heart disease, cardiovascular diseases, and all causes in young adult men: the Chicago Heart Association Detection Project in Industry. Arch Intern Med. 2001;161(12):1501-1508. doi: 10.1001/archinte.161.12.1501 [DOI] [PubMed] [Google Scholar]
- 14.McCarron P, Smith GD, Okasha M, McEwen J. Blood pressure in young adulthood and mortality from cardiovascular disease. Lancet. 2000;355(9213):1430-1431. doi: 10.1016/S0140-6736(00)02146-2 [DOI] [PubMed] [Google Scholar]
- 15.Moon JY, Park KJ, Hwangbo Y, et al. . A trend analysis of the prevalence, awareness, treatment, and control of hypertension by age group. J Prev Med Public Health. 2013;46(6):353-359. doi: 10.3961/jpmph.2013.46.6.353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cheol Seong S, Kim YY, Khang YH, et al. . Data Resource Profile: The National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017;46(3):799-800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Choi S, Kim K, Kim SM, et al. . Association of obesity or weight change with coronary heart disease among young adults in South Korea. JAMA Intern Med. 2018;178(8):1060-1068. doi: 10.1001/jamainternmed.2018.2310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim K, Park SM, Lee K. Weight gain after smoking cessation does not modify its protective effect on myocardial infarction and stroke: evidence from a cohort study of men. Eur Heart J. 2018;39(17):1523-1531. doi: 10.1093/eurheartj/ehx761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mozaffarian D, Benjamin EJ, Go AS, et al. ; Writing Group Members; American Heart Association Statistics Committee; Stroke Statistics Subcommittee . Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation. 2016;133(4):e38-e360. [DOI] [PubMed] [Google Scholar]
- 20.Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8(5):551-561. doi: 10.1002/sim.4780080504 [DOI] [PubMed] [Google Scholar]
- 21.Harrell FJ. Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis. New York, NY: Springer; 2001. doi: 10.1007/978-1-4757-3462-1 [DOI] [Google Scholar]
- 22.The sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1997;157(21):2413-2446. doi: 10.1001/archinte.1997.00440420033005 [DOI] [PubMed] [Google Scholar]
- 23.Vasan RS, Larson MG, Leip EP, et al. . Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med. 2001;345(18):1291-1297. doi: 10.1056/nejmoa003417 [DOI] [PubMed] [Google Scholar]
- 24.Liszka HA, Mainous AG III, King DE, Everett CJ, Egan BM. Prehypertension and cardiovascular morbidity. Ann Fam Med. 2005;3(4):294-299. doi: 10.1370/afm.312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hsia J, Margolis KL, Eaton CB, et al. ; Women’s Health Initiative Investigators . Prehypertension and cardiovascular disease risk in the Women’s Health Initiative. Circulation. 2007;115(7):855-860. doi: 10.1161/circulationaha.106.656850 [DOI] [PubMed] [Google Scholar]
- 26.Conen D, Ridker PM, Buring JE, Glynn RJ. Risk of cardiovascular events among women with high normal blood pressure or blood pressure progression: prospective cohort study. BMJ. 2007;335(7617):432. doi: 10.1136/bmj.39269.672188.AE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Murakami Y, Hozawa A, Okamura T, Ueshima H; Evidence for Cardiovascular Prevention From Observational Cohorts in Japan Research Group (EPOCH-JAPAN) . Relation of blood pressure and all-cause mortality in 180 000 Japanese participants: pooled analysis of 13 cohort studies. Hypertension. 2008;51(6):1483-1491. doi: 10.1161/HYPERTENSIONAHA.107.102459 [DOI] [PubMed] [Google Scholar]
- 28.He J, Gu D, Chen J, et al. . Premature deaths attributable to blood pressure in China: a prospective cohort study. Lancet. 2009;374(9703):1765-1772. doi: 10.1016/S0140-6736(09)61199-5 [DOI] [PubMed] [Google Scholar]
- 29.Arima H, Murakami Y, Lam TH, et al. ; Asia Pacific Cohort Studies Collaboration . Effects of prehypertension and hypertension subtype on cardiovascular disease in the Asia-Pacific Region. Hypertension. 2012;59(6):1118-1123. doi: 10.1161/hypertensionaha.111.187252 [DOI] [PubMed] [Google Scholar]
- 30.Williams B, Mancia G, Spiering W, et al. ; ESC Scientific Document Group . 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021-3104. doi: 10.1093/eurheartj/ehy339 [DOI] [PubMed] [Google Scholar]
- 31.Pool LR, Ning H, Wilkins J, Lloyd-Jones DM, Allen NB. Use of long-term cumulative blood pressure in cardiovascular risk prediction models[published online September 5, 2018]. JAMA Cardiol. 2018. doi: 10.1001/jamacardio.2018.2763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Colantonio LD, Booth JN III, Bress AP, et al. . 2017 ACC/AHA blood pressure treatment guideline recommendations and cardiovascular risk. J Am Coll Cardiol. 2018;72(11):1187-1197. doi: 10.1016/j.jacc.2018.05.074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Paige E, Barrett J, Pennells L, et al. . Use of repeated blood pressure and cholesterol measurements to improve cardiovascular disease risk prediction: an individual-participant-data meta-analysis. Am J Epidemiol. 2017;186(8):899-907. doi: 10.1093/aje/kwx149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gan SK, Loh CY, Seet B. Hypertension in young adults—an underestimated problem. Singapore Med J. 2003;44(9):448-452. [PubMed] [Google Scholar]
- 35.Na J, Park J, Park H, Lee B, Choi Y, Seo J. The statistical analysis on legal autopsy performed in Korea during 2012 Year. Korean J Leg Med. 2013;37:198-207. doi: 10.7580/kjlm.2013.37.4.198 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Descriptive characteristics of the final study population and participants prescribed anti-hypertensive medication during 2002-2005.
eTable 2. Cardiovascular disease risk according to the 2017 ACC/AHA guideline hypertension categories from mean blood pressure values among young adults.
eFigure 1. Unadjusted risk for cardiovascular disease according to blood pressure among young adults.
eFigure 2. Age-adjusted risk for cardiovascular disease according to blood pressure among young adults.
eTable 3. Cardiovascular disease risk according to the 2017 ACC/AHA guideline hypertension categories among young adults with additive adjustments for covariates.
eTable 4. Absolute risk and difference in absolute risk of cardiovascular disease according to the 2017 ACC/AHA guideline hypertension categories among young adults.
eTable 5. Stratified analysis on cardiovascular disease risk according to the 2017 ACC/AHA guideline defined hypertension categories among young adults by subgroups of age, body mass index, fasting serum glucose, total cholesterol, and Charlson comorbidity index.