Abstract
This database study evaluated the efficacy of monitoring flat symmetric pigmented spitzoid-looking lesions in prepubertal children.
According to recently introduced guidelines, the management of spitzoid-looking lesions should depend on the patient’s age.1 Specifically, any spitzoid-looking lesion after the age of 12 years and any asymmetric and nodular lesion at any age should be excised, whereas lesions with a typical starburst pattern before puberty should be monitored until stabilization.1,2 We aimed to evaluate the efficacy of monitoring flat symmetric pigmented spitzoid-looking lesions in prepubertal children.
Methods
We retrospectively screened our databases for eligible cases from January 1, 2015, through December 31, 2017. Inclusion criteria were (1) clinical diagnosis of Spitz or Reed nevus; (2) no older than 12 years at the baseline visit; (3) monitoring as selected management; and (4) availability of follow-up data at least 2 years after baseline. The patients’ age and sex and the location of the lesion were recorded. The primary outcome was the number and percentage of lesions that underwent surgical excision during the study period. Ethics committee approval was waived for this retrospective database review.
Results
We included 212 patients (113 girls [53.3%] and 99 boys [46.7%]; mean [SD] age, 6.1 [3.6] years). The most frequent anatomical sites of tumor development were the lower extremities (97 [45.8%]), upper extremities (39 [18.4%]), and head and/or neck (29 [13.7%]). The mean (SD) follow-up period was 28.2 (14.2) months, and the mean (SD) number of follow-up visits was 5.9 (2.7). Of 212 lesions, 45 (21.2%) were excised during follow-up. The mean (SD) time to excision from the baseline visit was 6.4 (4.4) months. In all cases, the histopathologic diagnosis was Spitz or Reed nevus.
Discussion
Our results suggest that monitoring Spitz and Reed nevi in children is not an efficient strategy, because it leads to unnecessary excisions without offering any actual benefit. Monitoring a spitzoid-looking lesion is based on the notion that nevi are expected to grow symmetrically to all directions until stabilization, whereas asymmetric changes should raise the suspicion of melanoma.1 In the realm of flat, pigmented spitzoid-looking lesions in prepubertal children, the latter strategy is associated with 2 significant drawbacks.
First, the probability of a symmetric Reed nevus–like melanoma in this age group is exceedingly low. Pediatric spitzoid melanomas do exist, but they present as Spitz nevus–like nodules or display an asymmetric pigmented Reed nevus–like (starburst) pattern.3 Atypical Spitz tumors also exist, but they are nonpigmented nodules or typified by a multicomponent dermoscopic pattern.4 No case of melanoma or atypical Spitz tumor characterized by a symmetric starburst pattern has ever been described in prepubertal children. This finding is further confirmed by the results of the present retrospective analysis, which found no melanoma in this age group among flat lesions typified by a symmetric starburst pattern.
Second, as highlighted by the present study, a significant proportion of Spitz and Reed nevi do not follow an ideally symmetric growth pattern. In our sample, 21.2% of Spitz and Reed nevi changed asymmetrically, prompting us to excise them (Figure 1). Because all these lesions were histopathologically diagnosed as Spitz or Reed nevi, we may conclude that monitoring was the source of a false concern and 45 unnecessary excisions. The main limitation of the present study is associated with the retrospective design, which does not allow consideration of confounding factors that might have influenced the management decision.
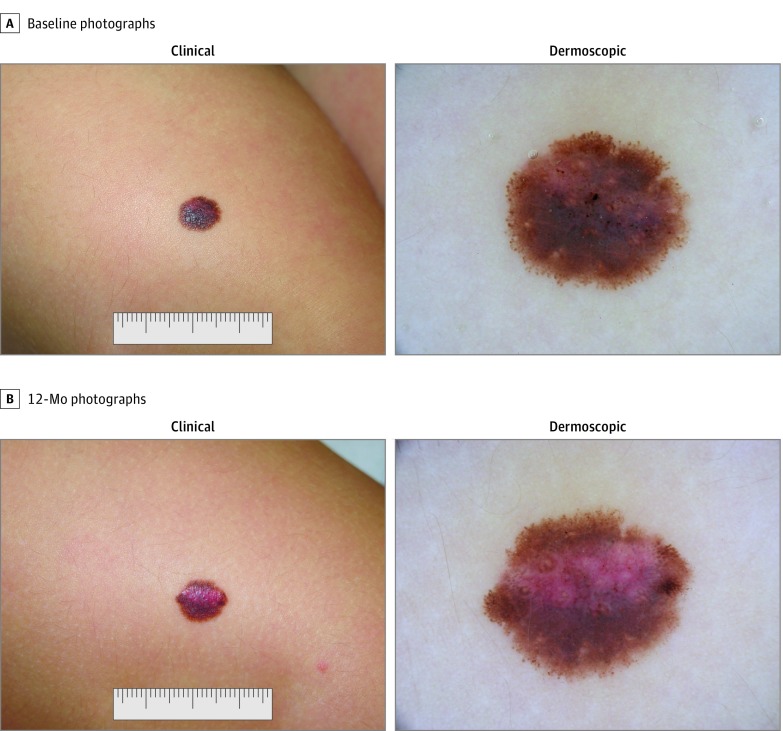
Figure 1. Clinical and Dermoscopic Photographs of a Pigmented Spitz (Reed) Nevus in a Prepubertal Patient.
Baseline photographs were obtained of the nevus on the thigh of a girl in her first decade of life, displaying the characteristic starburst pattern. After 12 months, dermoscopy revealed an eccentric zone with irregularly distributed dotted vessels and loss of pigmentation and an overall asymmetry of colors and structures. The lesion was excised, and histopathologic diagnosis was a Spitz nevus.
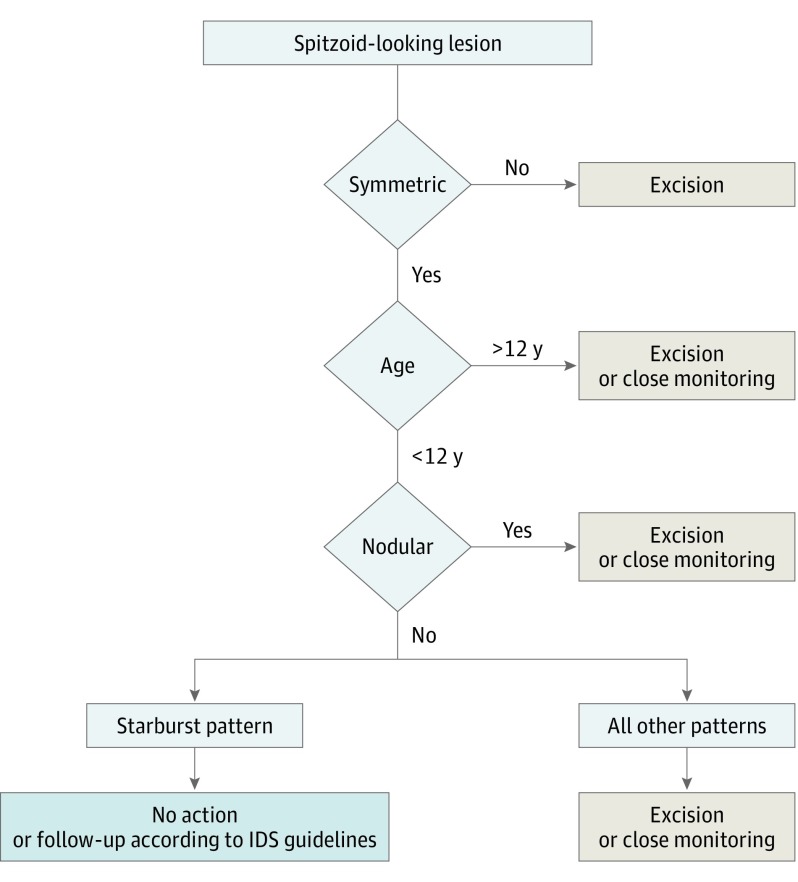
Considering that the accuracy of baseline diagnosis in this group of lesions was perfect and significantly decreased (in terms of specificity) after follow-up, we suggest that the baseline recognition of a flat pigmented dermoscopically symmetric Spitz or Reed nevus in prepubertal patients should not warrant any further action. However, clinicians in the daily routine must account for the stress and emotional needs of patients and their families. Therefore, monitoring of Spitz and Reed nevi will most probably continue to occur. Clinicians should at least be aware of the limitations of monitoring Spitz and Reed nevi and communicate them accordingly. We, therefore, suggest a slight modification of the recently released guidelines,1 aiming to help clinicians apply them more efficiently in the clinical practice (Figure 2).
Figure 2. Modified Version of the Guidelines for Management of Spitzoid-Looking Lesions.
IDS indicates International Dermoscopy Society.
References
- 1.Lallas A, Apalla Z, Ioannides D, et al. ; International Dermoscopy Society . Update on dermoscopy of Spitz/Reed naevi and management guidelines by the International Dermoscopy Society. Br J Dermatol. 2017;177(3):645-655. doi: 10.1111/bjd.15339 [DOI] [PubMed] [Google Scholar]
- 2.Lallas A, Moscarella E, Longo C, et al. . Likelihood of finding melanoma when removing a spitzoid-looking lesion in patients aged 12 years or older. J Am Acad Dermatol. 2015;72(1):47-53. doi: 10.1016/j.jaad.2014.09.037 [DOI] [PubMed] [Google Scholar]
- 3.Carrera C, Scope A, Dusza SW, et al. . Clinical and dermoscopic characterization of pediatric and adolescent melanomas: multicenter study of 52 cases. J Am Acad Dermatol. 2018;78(2):278-288. doi: 10.1016/j.jaad.2017.09.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moscarella E, Lallas A, Kyrgidis A, et al. . Clinical and dermoscopic features of atypical Spitz tumors: a multicenter, retrospective, case-control study. J Am Acad Dermatol. 2015;73(5):777-784. doi: 10.1016/j.jaad.2015.08.018 [DOI] [PMC free article] [PubMed] [Google Scholar]