Abstract
Although histology still plays a critical role in diagnosing diffuse gliomas, additional ancillary testing is an essential tool for VA pathology laboratories.
Over the past few decades, our understanding of the molecular underpinning of primary neoplasms of the central nervous system (CNS) has progressed substantially. Thanks in large part to this expansion in our knowledge base, the World Health Organization (WHO) has recently updated its classification of tumors of the CNS.1 One of the key elements of this update was the inclusion of molecular diagnostic criteria for the classification of infiltrating gliomas. While the previous classification system was based upon histologic subtypes of the tumor (astrocytoma, oligodendroglioma, and oligoastrocytoma), the revised classification system incorporates molecular testing to establish the genetic characteristics of the tumor to reach a final integrated diagnosis.
In this article, we present 3 cases to highlight some of these recent changes in the WHO diagnostic categories of primary CNS tumors and to illustrate the role of specific molecular tests in reaching a final integrated diagnosis. We then propose a clinical practice guideline for the Veterans Health Administration (VHA) that recommends use of molecular testing for veterans as part of the diagnostic workup of primary CNS neoplasms.
PURPOSE
In 2013 the VHA National Director of Pathology & Laboratory Medicine Services (P&LMS) chartered a national molecular genetics pathology workgroup (MGPW) that was charged with 4 specific tasks: (1) Provide recommendations about the effective use of molecular genetic testing for veterans; (2) Promote increased quality and availability of molecular testing within the VHA; (3) Encourage internal referral testing; and (4) Create an organizational structure and policies for molecular genetic testing and laboratory developed tests. The workgroup is currently composed of 4 subcommittees: genetic medicine, hematopathology, pharmacogenomics, and molecular oncology. The molecular oncology subcommittee is focused upon molecular genetic testing for solid tumors.
This article is intended to be the first of several publications from the molecular oncology subcommittee of the MGPW that address some of the aforementioned tasks. Similar to the recent publication from the hematopathology subcommittee of the MGPW, this article focuses on CNS neoplasms.2
Scope of Problem
The incidence of tumors of the CNS in the US population varies among age groups. It is the most common solid tumor in children aged < 14 years and represents a significant cause of mortality across all age groups.3 Of CNS tumors, diffuse gliomas comprise about 20% of the tumors and more than 70% of the primary malignant CNS tumors.3 Analysis of the VA Central Cancer Registry data from 2010 to 2014 identified 1,186 veterans (about 237 veterans per year) who were diagnosed with diffuse gliomas. (Lynch, Kulich, Colman, unpublished data, February 2018). While the majority (nearly 80%) of these cases were glioblastomas (GBMs), unfortunately a majority of these cases did not undergo molecular testing (Lynch, Kulich, Colman, unpublished data, February 2018).
Although this low rate of testing may be in part reflective of the period from which these data were gleaned (ie, prior to the WHO release of their updated the classification of tumors of the CNS), it is important to raise VA practitioners’ awareness of these recent changes to ensure that veterans receive the proper diagnosis and treatment for their disease. Thus, while the number of veterans diagnosed with diffuse gliomas within the VHA is relatively small in comparison to other malignancies, such as prostatic adenocarcinomas and lung carcinomas, the majority of diffuse gliomas do not seem to be receiving the molecular testing that would be necessary for (1) appropriate classification under the recently revised WHO recommendations; and (2) making important treatment decisions.
CASE PRESENTATIONS
Case 1
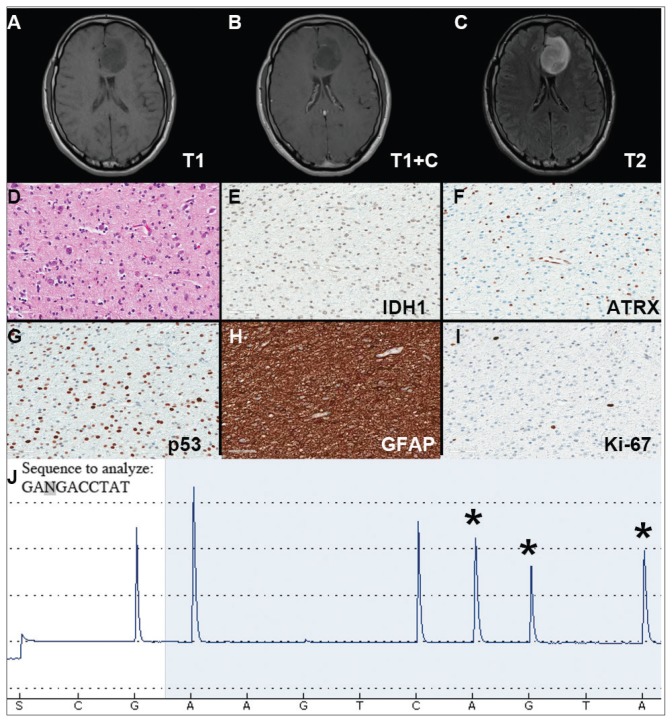
A veteran of the Gulf War presented with a 3-month history of possible narcoleptic events associated with a motor vehicle accident. Magnetic resonance imaging (MRI) revealed a large left frontal mass lesion with minimal surrounding edema without appreciable contrast enhancement (Figures 1A, 1B, and 1C). The patient subsequently underwent a stereotactic biopsy that revealed slightly hypercellular brain tissue composed of cells with round to ovoid hyperchromatic nuclei, which infiltrated the overlying cortex (Figure 1D).
FIGURE 1. Case 1 Imaging, Immunohistochemical Stains, and Pyrosequencing.
(A–C) Imaging studies demonstrating a left frontal lesion; representative images of hematoxylin & eosin (D) and the indicated immunohistochemical (E–I) stained slides of lesion; (J) Pyrogram of IDH1 gene pyrosequencing (wild-type sequence GACGA corresponding to compliment of nucleotides 397–393 of IDH1 cDNA, c.394C>T; p.R132C mutation).
Neither mitotic figures nor endothelial proliferation were identified. Immunohistochemical stains revealed a lack of R132H mutant IDH1 protein expression, a loss of nuclear staining for ATRX protein within a substantial number of cells, and a clonal pattern of p53 protein overexpression (Figures 1E, 1F, and 1G). The lesion demonstrated diffuse glial fibrillary acidic protein (GFAP) immunoreactivity and a low proliferation index (as determined by Ki-67 staining; estimated at less than 5%) (Figures 1H and 1I).
Based upon these results, an initial morphologic diagnosis of diffuse glioma was issued, and tissue was subjected to a variety of nucleic acid-based tests. While fluorescence in situ hybridization (FISH) studies were negative for 1p/19q codeletion, pyrosequencing analysis revealed the presence of a c.394C>T (R132C) mutation of the IDH1 gene (Figure 1J). The University of Pittsburgh Medical Center’s GlioSeq targeted next-generation sequence (NGS) analysis confirmed the presence of the c.394C > T mutation in IDH1 gene.4 Based upon this additional information, a final integrated morphologic and molecular diagnosis of diffuse astrocytoma, IDH-mutant was rendered.
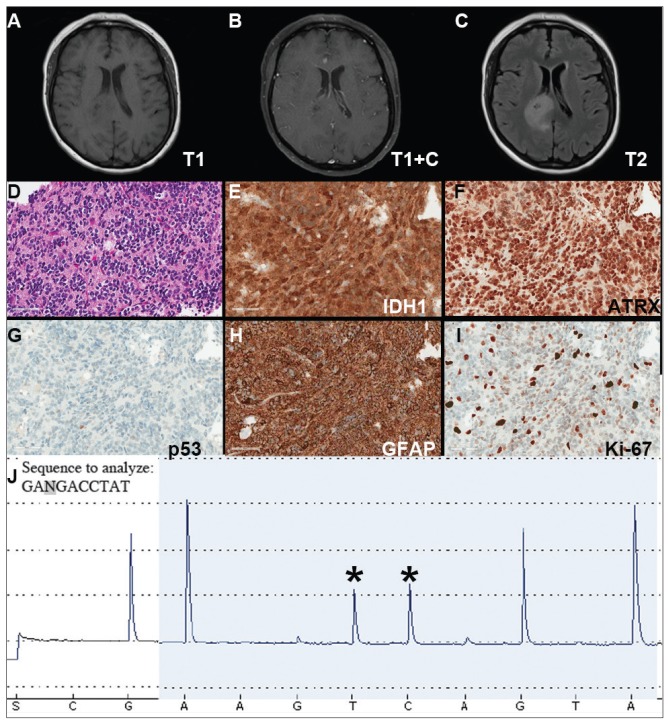
Case 2
A Vietnam War veteran presented with a 6-week history of new onset falls with associated left lower extremity weakness. A MRI revealed a right frontoparietal mass lesion with surrounding edema without appreciable contrast enhancement (Figures 2A, 2B, and 2C). The patient subsequently underwent a diagnostic craniotomy that revealed a variably cellular neoplasm composed of cells with round to ovoid nuclei, which infiltrated the overlying cortex and contained rare psammoma bodies. The neoplasm contained multiple nodular foci of hypercellularity, focally brisk mitotic activity, and focal endothelial proliferation, although areas of necrosis were not identified.
FIGURE 2. Case 2 Imaging, Immunohistochemical Stains, and Pyrosequencing.
(A–C) Imaging studies demonstrating a right frontoparietal lesion; representative images of H&E hematoxylin & eosin (D) and the indicated immunohistochemical (E–I) stained slides of lesion; (J) Pyrogram of IDH1 gene pyrosequencing (wild-type sequence GACGA corresponding to compliment of nucleotides 397–393 of IDH1 cDNA, c.395G>A; p.R132H mutation)
Immunohistochemical stains revealed R132H mutant IDH1 protein expression, retention of nuclear staining for ATRX protein, the lack of a clonal pattern of p53 protein overexpression, diffuse GFAP immunoreactivity, and a proliferation index (as determined by Ki-67 staining) focally approaching 20% (Figures 2E, 2F, 2G, 2H and 2I).
Based upon these results, an initial morphologic diagnosis of diffuse (high grade) glioma was issued, and tissue was subjected to a variety of nucleic acid-based tests. The FISH studies were positive for 1p/19q codeletion, and pyrosequencing analysis confirmed the immunohistochemical findings of a c.395G>A (R132H) mutation of the IDH1 gene (Figure 2J). GlioSeq targeted NGS analysis confirmed the presence of the c.395G>A mutation in the IDH1 gene, a mutation in the telomerase reverse transcriptase (TERT) promoter, and possible decreased copy number of the CIC (chromosome 1p) and FUBP1 (chromosome 19q) genes.
A final integrated morphologic and molecular diagnosis of anaplastic oligodendroglioma, IDH-mutant and 1p/19q-codeleted was rendered based on the additional information. With this final diagnosis, methylation analysis of the MGMT gene promoter, which was performed for prognostic and predictive purposes, was identified in this case.5,6
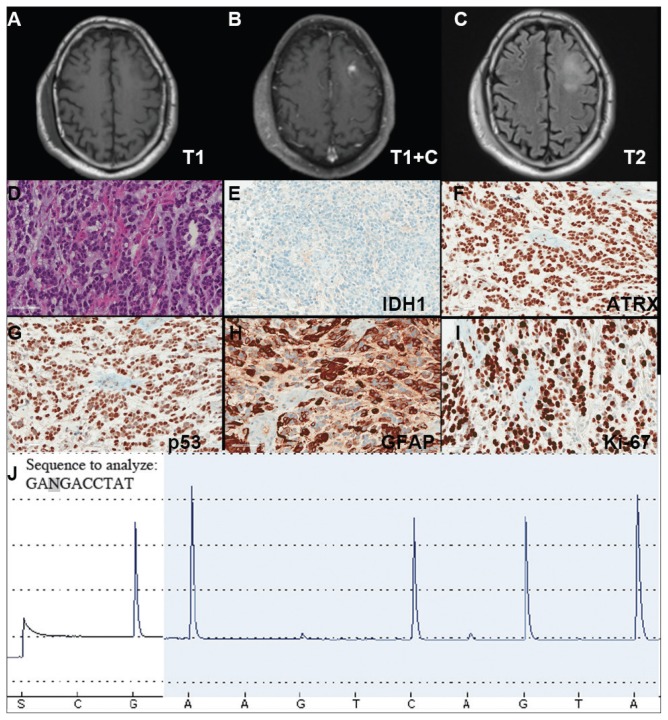
Case 3
A veteran of the Vietnam War presented with a new onset seizure. A MRI revealed a focally contrast-enhancing mass with surrounding edema within the left frontal lobe (Figures 3A, 3B, and 3C). The patient subsequently underwent a diagnostic craniotomy that revealed a poorly demarked mucoid lesion. Intraoperative cytology revealed a noncohesive, process poor neoplasm predominantly composed of cells with small-to-medium round to slightly irregular nuclei in the background of thin vessels. Rare mitotic figures as well as scattered cells with fibrillary processes and larger hyperchromatic nuclei with irregular nuclear membranes were identified.
FIGURE 3. Case 3 Imaging, Immunohistochemical Stains, and Pyrosequencing.
(A–C) Imaging studies demonstrating a left frontal lesion; representative images of H&E hematoxylin & eosin (D) and indicated immunohistochemical (E–I) stained slides of lesion; (J) Pyrogram of IDH1 gene pyrosequencing (wild-type sequence GACGA corresponding to compliment of nucleotides 397–393 of IDH1 cDNA)
Hematoxylin and eosin (H&E) stained sections following formalin fixation and paraffin embedding demonstrated similar findings (Figure 3D), and while mitotic figures were readily identified, areas of necrosis were not identified and endothelial proliferation was not a prominent feature. Immunohistochemical stains revealed no evidence of R132H mutant IDH1 protein expression, retention of nuclear staining for ATRX protein, a clonal pattern of p53 protein overexpression, patchy GFAP immunoreactivity, and a proliferation index (as determined by Ki-67 staining) focally approaching 50% (Figures 3E, 3F, 3G, 3H, and 3I).
Based upon these results, an initial morphologic diagnosis of diffuse (high grade) glioma was issued, and the tissue was subjected to a variety of nucleic acid-based tests. The FISH studies were negative for EGFR gene amplification and 1p/19q codeletion, although a gain of the long arm of chromosome 1 was detected. Pyrosequencing analysis for mutations in codon 132 of the IDH1 gene revealed no mutations (Figure 3J). GlioSeq targeted NGS analysis identified mutations within the NF1, TP53, and PIK3CA genes without evidence of mutations in the IDH1, IDH2, ATRX, H3F3A, or EGFR genes or the TERT promoter. Based upon this additional information, a final integrated morphologic and molecular diagnosis of GBM, IDH wild-type was issued. The MGMT gene promoter was negative for methylation, a finding that has prognostic and predictive impact with regard to treatment with temazolamide.7–9
NEW DIFFUSE GLIOMA CLASSIFICATION
Since the issuance of the previous edition of the WHO classification of CNS tumors in 2007, several sentinel discoveries have been made that have advanced our understanding of the underlying biology of primary CNS neoplasms. Since a detailed review of these findings is beyond the scope and purpose of this manuscript and salient reviews on the topic can be found elsewhere, we will focus on the molecular findings that have been incorporated into the recently revised WHO classification.10 The importance of providing such information for proper patient management is illustrated by the recent acknowledgement by the American Academy of Neurology that molecular testing of brain tumors is a specific area in which there is a need for quality improvement.11 Therefore, it is critical that these underlying molecular abnormalities are identified to allow for proper classification and treatment of diffuse gliomas in the veteran population.
As noted previously, based on VA cancer registry data, diffuse gliomas are the most commonly encountered primary CNS cancers in the veteran population. Several of the aforementioned seminal discoveries have been incorporated into the updated classification of diffuse gliomas. While the recently updated WHO classification allows for the assignment of “not otherwise specified (NOS)” diagnostic designation, this category must be limited to cases where there is insufficient data to allow for a more precise classification due to sample limitations and not simply due to a failure of VA pathology laboratories to pursue the appropriate diagnostic testing.
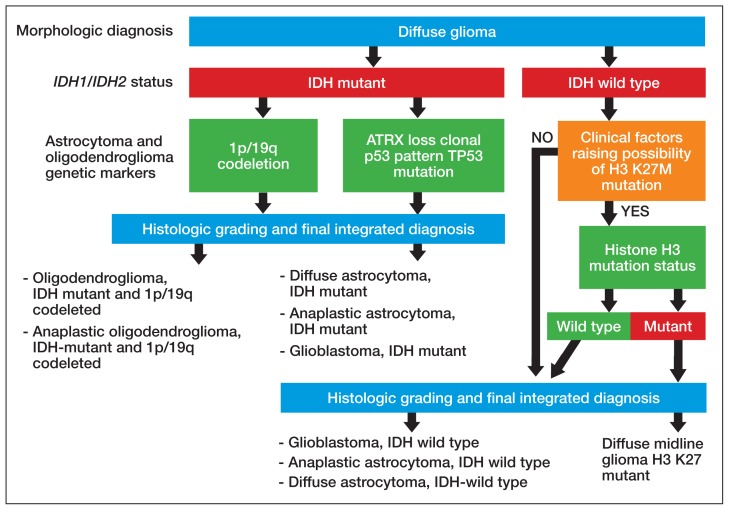
Figure 4 presents the recommended diagnostic workflow for the workup of diffuse gliomas. As illustrated in the above cases, a variety of different methodologies, including immunohistochemical, FISH, loss of heterozygosity analysis, traditional and NGS may be applied when elucidating the status of molecular events at critical diagnostic branch points. Each of these methods has their individual strengths and weaknesses. In addition, tests like assessment of mutations within selected histone genes probably are applied best to cases where such entities commonly occur (ie, midline tumors) and not in every case. Similarly, although in the cases presented above several different redundant methodologies were employed to answer questions critical in the proper classification of diffuse gliomas (eg, immunohistochemical, pyrosequencing, and NGS analysis of IDH1 mutational status), these were presented for illustrative purposes only. Once a given test identifies the genetic changes that allow for proper classification of diffuse gliomas, additional confirmatory testing is not mandatory. Although not recommended, due to the rarity of non-R132H IDH1 and IDH2 mutations in GBM occurring in the elderly, immunohistochemistry for R132H mutant IDH1 may be considered sufficient for initial determination of IDH mutational status in this patient population (eg, appropriate histology for the diagnosis of GBM in an elderly patient). However, caution must be exercised in cases where other entities lower grade lesions, such as pilocytic astrocytoma, pleomorphic astrocytoma, and ganglioglioma, enter the histologic differential diagnosis. In such scenarios, additional sequencing of IDH1 and IDH2 genes, as well as sequencing of other potentially diagnostically relevant alterations (eg, BRAF) may be reasonable. This decision may be aided by a web-based application for calculating the probability of an IDH1/2 mutation in a patient’s diffuse glioma (www.kcr.uky.edu/webapps/IDH/app.html).12 Finally, once the diagnosis of a high-grade diffuse glioma has been reached, assessment of the methylation status of the MGMT promoter should be performed, particularly in elderly patients with GBM, to provide important predictive and prognostic information.6,13,14
FIGURE 4. Suggested Workflow for Diffuse Glioma Diagnosisa.
aThe diagnosis of diffuse midline glioma, H3 K27M-mutant is to be restricted to entities that fulfill all 4 criteria (diffuse, midline, glioma, and possess a K27M mutation in H3 as this mutation has been described in other entities such as pilocytic astrocytomas, gangliogliomas, and ependymomas.
DIAGNOSTIC USES OF MOLECULAR TESTING
While the case studies in this article demonstrate the use of ancillary testing and provide a suggested strategy for properly subclassifying diffuse gliomas, inherent in this strategy is the assumption that, based upon the initial clinical and pathologic information available, one can accurately categorize the lesion as a diffuse glioma. In reality, such a distinction is not always a straightforward endeavor. It is well recognized that a proportion of low-grade, typically radiologically circumscribed, CNS neoplasms, such as pilocytic astrocytomas and glioneuronal tumors, may infiltrate the surrounding brain parenchyma. In addition, many of these low-grade CNS neoplasms also may have growth patterns that are shared with diffuse gliomas, a diagnostic challenge that often can be further hampered by the inherent limitations involved in obtaining adequate samples for diagnosis from the CNS.
Although there are limitations and caveats, molecular diagnostic testing may be invaluable in properly classifying CNS tumors in such situations. The finding of mutations in the IDH1 or IDH2 genes has been shown to be very valuable in distinguishing low-grade diffuse glioma from both nonneoplastic and low-grade circumscribed neuroepithelial neoplasms that may exhibit growth patterns that can mimic those of diffuse gliomas.15–17 Conversely, finding abnormalities in the BRAF gene in a brain neoplasm that has a low-grade morphology suggests that the lesion may represent one of these low-grade lesions such as a pleomorphic xanthoastrocytoma, pilocytic astrocytoma, or mixed neuronalglial tumor as opposed to a diffuse glioma.18,19
Depending upon the environment in which one practices, small biopsy specimens may be prevalent, and unfortunately, it is not uncommon to obtain a biopsy that exhibits a histologic growth pattern that is discordant from what one would predict based on the clinical context and imaging findings. Molecular testing may be useful in resolving discordances in such situations. If a biopsy of a ring-enhancing lesion demonstrates a diffuse glioma that doesn’t meet WHO grade IV criteria, applying methodologies that look for genetic features commonly encountered in high-grade astrocytomas may identify genetic abnormalities that suggest a more aggressive lesion than is indicated by the histologic findings. The presence of genetic abnormalities such as homozygous deletion of the CDKN2A gene, TERT promoter mutation, loss of heterozygosity of chromosome 10q and/or phosphatase and tensin homolog (PTEN) mutations, EGFR gene amplification or the presence of the EGFR variant III are a few findings that would suggest the aforementioned sample may represent an undersampling of a higher grade diffuse astrocytoma, which would be important information to convey to the treating clinicians.20–26
TESTING IN THE VA
The goals of the MPWG include promoting increased quality and availability of genetic testing within the VHA as well as encouraging internal referral testing. An informal survey of the chiefs of VA Pathology and Laboratory Medicine Services was conducted in November of 2017 in an attempt to identify internal VA pathology laboratories currently conducting testing that may be of use in the workup of diffuse gliomas (Table 1). It is the hope of this subcommittee that, in light of the recent revision of the WHO classification of tumors of the nervous system, this testing will be more widespread and readily available within VA laboratories to allow for a cost-effective yet comprehensive molecular assessment of diffuse gliomas.
TABLE 1.
VA Pathology Laboratories Currently Offering Selected Tests for Workup of Diffuse Gliomas
| Tests | VA Facilities Currently Offering Tests |
|---|---|
| IDH1 R132H immunohistochemistry | VA Pittsburgh Healthcare System |
| ATRX immunohistochemistry | VA Pittsburgh Healthcare System |
| H3F3A K27M immunohistochemistry | None |
| IDH1 and/or IDH2 gene mutational analysis | VA Pittsburgh Healthcare System (IDH1 only) |
| BRAF (V600E; c.1799T>A) gene mutational analysis | Minneapolis VA Health Care System VA Greater Los Angeles Healthcare System VA Pittsburgh Healthcare System |
| 1p/19q codeletion analysis (FISH or LOH) | Richard L. Roudebush VAMC, Indianapolis VA Greater Los Angeles Healthcare System |
| EGFR FISH | None |
| MGMT promoter methylation | None |
| Next generation sequencing panel covering diffuse glioma genetic alterations | Nonea |
Abbreviations: EGFR, epidermal growth factor receptor; FISH, fluorescence in situ hybridization; LOH, loss of heterozygosity.
Performed in commercial laboratories as part of the VA Precision Oncology Program.
The VA currently offers NGS panels for patients with advanced-stage malignancies under the auspices of the Precision Oncology Program, whose reports provide both (1) mutational analyses for genes such as TP53, ATRX, NF1, BRAF, PTEN, TERT IDH1, and IDH2 that may be useful in the proper classifying of high-grade diffuse gliomas; and (2) information regarding clinical trials for which the veteran may be eligible for based on their glioma’s mutational profile. Interested VA providers should visit tinyurl.com/precisiononcology/ for more information about this program. Finally, although internal testing within VA laboratories is recommended to allow for the development of more cost-effective testing, testing may be performed through many nationally contracted reference laboratories.
CONCLUSION
In light of the recent progress made in our understanding of the molecular events of gliomagenesis, the way we diagnose diffuse gliomas within the CNS has undergone a major paradigm shift. While histology still plays a critical role in the process, we believe that additional ancillary testing is a requirement for all diffuse gliomas diagnosed within VA pathology laboratories. In the context of recently encountered cases, we have provided a recommended workflow highlighting the testing that can be performed to allow for the proper diagnosis of our veterans with diffuse gliomas (Figure 4).
Unless limited by the amount of tissue available for such tests, ancillary testing must be performed on all diffuse gliomas diagnosed within the VA system to ensure proper diagnosis and treatment of our veterans with diffuse gliomas. See Table 2 for recommended applications for various tests. Finally, while we have attempted to identify laboratories within the VA system that perform some of these critical tests with the hope of encouraging collaborative, cost-effective testing of diffuse gliomas within the VA system, there are currently apparent gaps in our ability to provide the comprehensive ancillary testing required for diffuse gliomas exclusively within the VA laboratory environment.
TABLE 2.
Testing Recommendations for Diffuse Gliomasa
| Tests | Recommended Applications |
|---|---|
| IDH1\IDH2 gene mutational status | All diffuse gliomas As needed for cases of histologic mimics of diffuse gliomas |
| ATRX immunohistochemistry | As needed in IDH mutant diffuse gliomas to define oligodendroglioma vs astrocytoma lineage |
| H3F3A K27M immunohistochemistry | IDH wild-type diffuse gliomas in younger patients with midline lesions |
| BRAF (V600E; c.1799T>A) gene mutational analysis | Differentiating selected low-grade gliomas (extracerebellar pilocytic astrocytomas, gangliogliomas, and pleomorphic xanthoastrocytomas) from diffuse gliomas Suspected cases of epithelioid glioblastoma |
| 1p/19q codeletion analysis (FISH or LOH) | All IDH mutant diffuse gliomas |
| EGFR FISH | Problematic diffuse glioma cases where diagnosis of primary glioblastoma is suspected |
| MGMT promoter methylation | All anaplastic (WHO grades III and IV) diffuse gliomas |
Abbreviations: EGFR, epidermal growth factor receptor; FISH, fluorescence in situ hybridization; LOH, loss of heterozygosity; WHO, World Health Organization.
In cases where unequivocal astrocytic differentiation has been demonstrated by other ancillary tests (ATRX loss\mutation, TP53 mutation) assessment of 1p/19q status may not be necessary.
ACKNOWLEDGMENTS
The authors thank Dr. Craig M. Horbinski (Feinberg School of Medicine, Northwestern University) and Dr. Geoffrey H. Murdoch (University of Pittsburgh) for their constructive criticism of the manuscript. We also thank the following individuals for past service as members of the molecular oncology subcommittee of the MGPW: Dr. George Ansstas (Washington University School of Medicine), Dr. Osssama Hemadeh (Bay Pines VA Health Care System), Dr. James Herman (VA Pitts-burgh Healthcare System), and Dr. Ryan Phan (formerly of the VA Greater Los Angeles Healthcare System) as well as the members of the Veterans Administration pathology and laboratory medicine service molecular genetics pathology workgroup.
APPENDIX
Current Membership of Molecular Oncology Subcommittee of Molecular Genetics Pathology Workgroup
| Members | Affiliations |
|---|---|
| Scott M. Kulich, MD, PhD (Chair) | VA Pittsburgh Healthcare System, University of Pittsburgh, Department of Pathology, Division of Neuropathology |
| Daniel Becker, MD | VA-New York Harbor Healthcare System, Manhattan Campus, New York University School of Medicine |
| Howard Colman, MD, PhD | Huntsman Cancer Institute and Department of Neurosurgery, University of Utah, Department of Medicine (Hematology/Oncology), George E. Wahlen VA Medical Center, Salt Lake City |
| Sanja Dacic, MD\PhD | University of Pittsburgh, Department of Pathology |
| Umamaheswar Duvvuri, MD, PhD | VA Pittsburgh Healthcare System, University of Pittsburgh, Department of Otolaryngology |
| Dmitriy W. Gutkin, MD, PhD | VA Pittsburgh Healthcare System, University of Pittsburgh, Department of Pathology |
| Ping Hou, MD, PhD | St. Louis VA Medical Center |
| Pamela L. Lyle, MD | Bay Pines VA Health Care System |
| Bruce Montgomery, MD | VA Puget Sound Health Care System, Seattle |
| Vida Passero, MD, MBA | VA Pittsburgh Healthcare System, Section Chief, Hematology/Oncology |
| Ronald M. Przygodzki, MD | Department of Veterans Affairs, Director of Genomic Medicine Implementation, Associate Director of Genomic Medicine |
Footnotes
AUTHOR DISCLOSURES
The authors report no actual or potential conflicts of interest with regard to this article.
DISCLAIMER
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the US Government, or any of its agencies.
REFERENCES
- 1.Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 2016;131(6):803–820. doi: 10.1007/s00401-016-1545-1. [DOI] [PubMed] [Google Scholar]
- 2.Wang-Rodriguez J, Yunes A, Phan R, et al. The challenges of precision medicine and new advances in molecular diagnostic testing in hematolymphoid malignancies: impact on the VHA. Fed Pract. 2017;34(suppl 5):S38–S49. [PMC free article] [PubMed] [Google Scholar]
- 3.Ostrom QT, Gittleman H, Liao P, et al. CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2010–2014. Neuro Oncol. 2017;19(suppl 5):v1–v88. doi: 10.1093/neuonc/nox158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nikiforova MN, Wald AI, Melan MA, et al. Targeted next-generation sequencing panel (GlioSeq) provides comprehensive genetic profiling of central nervous system tumors. Neuro Oncol. 2016;18(3):379–387. doi: 10.1093/neuonc/nov289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cairncross JG, Ueki K, Zlatescu MC, et al. Specific genetic predictors of chemotherapeutic response and survival in patients with anaplastic oligodendrogliomas. J Natl Cancer Inst. 1998;90(19):1473–1479. doi: 10.1093/jnci/90.19.1473. [DOI] [PubMed] [Google Scholar]
- 6.van den Bent MJ, Erdem-Eraslan L, Idbaih A, et al. MGMT-STP27 methylation status as predictive marker for response to PCV in anaplastic oligodendrogliomas and oligoastrocytomas. A report from EORTC study 26951. Clin Cancer Res. 2013;19(19):5513–5522. doi: 10.1158/1078-0432.CCR-13-1157. [DOI] [PubMed] [Google Scholar]
- 7.Stupp R, Hegi ME, Mason WP, et al. European Organisation for Research and Treatment of Cancer Brain Tumour and Radiation Oncology Groups; National Cancer Institute of Canada Clinical Trials Group. Effects of radio-therapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol. 2009;10(5):459–466. doi: 10.1016/S1470-2045(09)70025-7. [DOI] [PubMed] [Google Scholar]
- 8.Malmstrom A, Gronberg BH, Marosi C, et al. Temozolomide versus standard 6-week radiotherapy versus hypo-fractionated radiotherapy in patients older than 60 years with glioblastoma: the Nordic randomised, phase 3 trial. Lancet Oncol. 2012;13(9):916–926. doi: 10.1016/S1470-2045(12)70265-6. [DOI] [PubMed] [Google Scholar]
- 9.van den Bent MJ, Kros JM. Predictive and prognostic markers in neurooncology. J Neuropathol Exp Neurol. 2007;66(12):1074–1081. doi: 10.1097/nen.0b013e31815c39f1. [DOI] [PubMed] [Google Scholar]
- 10.Chen R, Smith-Cohn M, Cohen AL, Colman H. Glioma subclassifications and their clinical significance. Neurotherapeutics. 2017;14(2):284–297. doi: 10.1007/s13311-017-0519-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jordan JT, Sanders AE, Armstrong T, et al. Quality improvement in neurology: neuro-oncology quality measurement set. Neurology. 2018;90(14):652–658. doi: 10.1212/WNL.0000000000005251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen L, Voronovich Z, Clark K, et al. Predicting the likelihood of an isocitrate dehydrogenase 1 or 2 mutation in diagnoses of infiltrative glioma. Neuro Oncol. 2014;16(11):1478–1483. doi: 10.1093/neuonc/nou097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hegi ME, Diserens AC, Gorlia T, et al. MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med. 2005;352(10):997–1003. doi: 10.1056/NEJMoa043331. [DOI] [PubMed] [Google Scholar]
- 14.Wick W, Platten M, Meisner C, et al. NOA-08 Study Group of Neuro-oncology Working Group (NOA) of German Cancer Society. Temozolomide chemotherapy alone versus radiotherapy alone for malignant astrocytoma in the elderly: the NOA-08 randomised, phase 3 trial. Lancet Oncol. 2012;13(7):707–715. doi: 10.1016/S1470-2045(12)70164-X. [DOI] [PubMed] [Google Scholar]
- 15.Horbinski C, Kofler J, Kelly LM, Murdoch GH, Nikiforova MN. Diagnostic use of IDH1/2 mutation analysis in routine clinical testing of formalin-fixed, paraffin-embedded glioma tissues. J Neuropathol Exp Neurol. 2009;68(12):1319–1325. doi: 10.1097/NEN.0b013e3181c391be. [DOI] [PubMed] [Google Scholar]
- 16.Camelo-Piragua S, Jansen M, Ganguly A, Kim JC, Louis DN, Nutt CL. Mutant IDH1-specific immunohistochemistry distinguishes diffuse astrocytoma from astrocytosis. Acta Neuropathol. 2010;119(4):509–511. doi: 10.1007/s00401-009-0632-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Horbinski C, Kofler J, Yeaney G, et al. Isocitrate dehydrogenase 1 analysis differentiates gangliogliomas from infiltrative gliomas. Brain Pathol. 2011;21(5):564–574. doi: 10.1111/j.1750-3639.2011.00480.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berghoff AS, Preusser M. BRAF alterations in brain tumours: molecular pathology and therapeutic opportunities. Curr Opin Neurol. 2014;27(6):689–696. doi: 10.1097/WCO.0000000000000146. [DOI] [PubMed] [Google Scholar]
- 19.Korshunov A, Meyer J, Capper D, et al. Combined molecular analysis of BRAF and IDH1 distinguishes pilocytic astrocytoma from diffuse astrocytoma. Acta Neuropathol. 2009;118(3):401–405. doi: 10.1007/s00401-009-0550-z. [DOI] [PubMed] [Google Scholar]
- 20.Fuller CE, Schmidt RE, Roth KA, et al. Clinical utility of fluorescence in situ hybridization (FISH) in morphologically ambiguous gliomas with hybrid oligodendroglial/astrocytic features. J Neuropathol Exp Neurol. 2003;62(11):1118–1128. doi: 10.1093/jnen/62.11.1118. [DOI] [PubMed] [Google Scholar]
- 21.Horbinski C. Practical molecular diagnostics in neuropathology: making a tough job a little easier. Semin Diagn Pathol. 2010;27(2):105–113. doi: 10.1053/j.semdp.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 22.Fuller GN, Bigner SH. Amplified cellular oncogenes in neoplasms of the human central nervous system. Mutat Res. 1992;276(3):299–306. doi: 10.1016/0165-1110(92)90016-3. [DOI] [PubMed] [Google Scholar]
- 23.Brennan CW, Verhaak RG, McKenna A, et al. TCGA Research Network. The somatic genomic landscape of glioblastoma. Cell. 2013;155(2):462–477. doi: 10.1016/j.cell.2013.09.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aldape K, Zadeh G, Mansouri S, Reifenberger G, von Deimling A. Glioblastoma: pathology, molecular mechanisms and markers. Acta Neuropathol. 2015;129(6):829–848. doi: 10.1007/s00401-015-1432-1. [DOI] [PubMed] [Google Scholar]
- 25.Killela PJ, Reitman ZJ, Jiao Y, et al. TERT promoter mutations occur frequently in gliomas and a subset of tumors derived from cells with low rates of self-renewal. Proc Natl Acad Sci U S A. 2013;110(15):6021–6026. doi: 10.1073/pnas.1303607110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nikiforova MN, Hamilton RL. Molecular diagnostics of gliomas. Arch Pathol Lab Med. 2011;135(5):558–568. doi: 10.5858/2010-0649-RAIR.1. [DOI] [PubMed] [Google Scholar]