Abstract
Background
Detecting and managing frailty at early stages can prevent disability and other adverse outcomes. The study aim was to evaluate whether a multifactorial intervention program could modify physical and cognitive frailty parameters in elderly individuals.
Methods
We conducted a multicenter, randomized, single-blind, parallel-group trial in community-living prefrail/frail elderly individuals in Barcelona. A total of 352 patients, aged ≥65 years old with positive frailty screening, was randomized into two groups to receive a 12-week multidisciplinary intervention or usual care, with concealed allocation. The intervention consisted of: exercise training, intake of hyperproteic nutritional shakes, memory training, and medication review. Main outcome assessments with multivariate analysis were conducted at 3 and 18 months.
Results
A total of 347 participants (98.6%) completed the study, mean age 77.3 years, 89 prefrail subjects (25.3%), and 75.3% female (n = 265). Eighteen-month assessments were performed in 76% of the sample. After 3 and 18 months, adjusted means difference between-groups showed significant improvements for the intervention group in all comparisons: Short Physical Performance Battery score improved 1.58 and 1.36 points (p < .001), handgrip strength 2.84 and 2.49 kg (p < .001), functional reach 4.3 and 4.52 cm (p < .001), and number of prescriptions decreased 1.39 and 1.09 (p < .001), respectively. Neurocognitive battery also showed significant improvements across all dimensions at 3 and 18 months.
Conclusions
A physical, nutritional, neurocognitive, and pharmacological multifaceted intervention was effective in reversing frailty measures both at short-term and 18 months. Lasting benefits of a multi-intervention program among frail elderly individuals encourage its prioritization.
Keywords: Frailty, Clinical Trials, Exercise, Cognition
Frailty, defined as vulnerability to multiple stressors (1), is a frequent geriatric condition. Nevertheless, its conceptualization, based on two major approaches: the phenotype model (2) or an accumulation of deficits (3), remains a challenge. Irrespective of the model employed, frailty predicts main adverse outcomes such as mobility loss, falling, disability, hospitalization, institutionalization, and mortality (4), and results in considerable medical and public expenditure. Frailty is a continuum: from a prefrail stage to mild impairment without a total loss of function (5). Due to its potential reversibility at early stages, it is vital to assess the individual’s degree of frailty (6). In fact, interventions to achieve healthy aging through prevention programs are currently priorities expressed by the World Health Organization (WHO) and recent European policies (7).
Although frailty is a multidimensional concept embracing physical, psychological, and environmental factors, most intervention studies have focused only on a one-dimensional, biomedical perspective (8). Rehabilitation models present satisfactory results in gait speed and improvement of the score in the short physical performance battery (SPPB) (9), but report inconclusive effects on functional ability and well-being (10).
A considerable number of protocols have been performed in institutions (11), at individuals’ homes (12), and with a small sample size of community-dwelling older adults (13). Other interventions have only encompassed strategies based on nutritional supplementation or hormones. They partially failed to decelerate the sarcopenia process, and revealed an unfavorable safety profile (14,15). Protein intake alone or combined with physical activity is the main nonpharmacological modality that effectively stimulates muscle protein synthesis (16).
Furthermore, elderly patients frequently present cognitive disorders (executive function, attention, processing speed), together with affected emotional and social domains, which may trigger a rapid decline. To date, however, the relationship between frailty and cognitive states remains unclear (17). Cognitive impairment as a key element in frailty characterization has been widely debated (18). Physical activity appears to enhance cognitive performance in risk patients and when combined with protein supplementation, although results are inconclusive (19). Memory stimulation programs also lead to positive performance changes in older adults with mild cognitive impairment (20).
Another fundamental and well-documented factor is polypharmacy (21). It has been associated with high morbidity and mortality rates in frail, elderly individuals, due to adverse drug reactions, interactions, underuse, nonadherence, and inappropriate prescribing. Nevertheless, the Screening Tool of Older Person’s potentially inappropriate Prescription (STOPP) and START guidelines offer a promising strategy to improve appropriate prescribing in the elderly adults (22). Moreover, emerging studies dealing with frailty have begun to ascertain whether it could be slowed down or even reversed with multi-intervention clinical trials (11,23,24) and have reported modest but encouraging outcomes.
The objective of our trial was to assess the effectiveness of a multifactorial intervention to modify frailty parameters: physical dimensions (muscle strength, elasticity, balance), cognitive performance, and polypharmacy in frail, elderly community-dwelling individuals. We carried out a 12-week multidisciplinary intervention involving clinicians, physiotherapists, speech therapists, and social workers, based on structured physical activity, diet supplementation, memory workshops, and medication review.
Methods
Study Design and Setting
A prospective, single-blind, parallel-group, pragmatic, randomized, multicenter, clinical trial was performed with an 18-month follow-up. Details of the methods have been previously published (25). Trial registration: ClinicalTrials.gov NCT01969526.
The study was conducted at 8 primary health care centers and involved 352 community-dwelling adults aged older than 65 from different areas of Barcelona. Changes from baseline frailty measurements at enrollment were compared between the intervention (IG) and control group (CG) at the end of the intervention, and 18 months later.
Participants and Recruitment
Inclusion criteria were: set gait time between 10 and 30 seconds in the Timed Get-up-and-Go test (TGUGT); scored Mini-Examination Cognitive of Lobo (MEC-35 Lobo) ≥18 points (no severe cognitive impairment); and Fried modified criteria. See Supplementary Table 1 for further details.
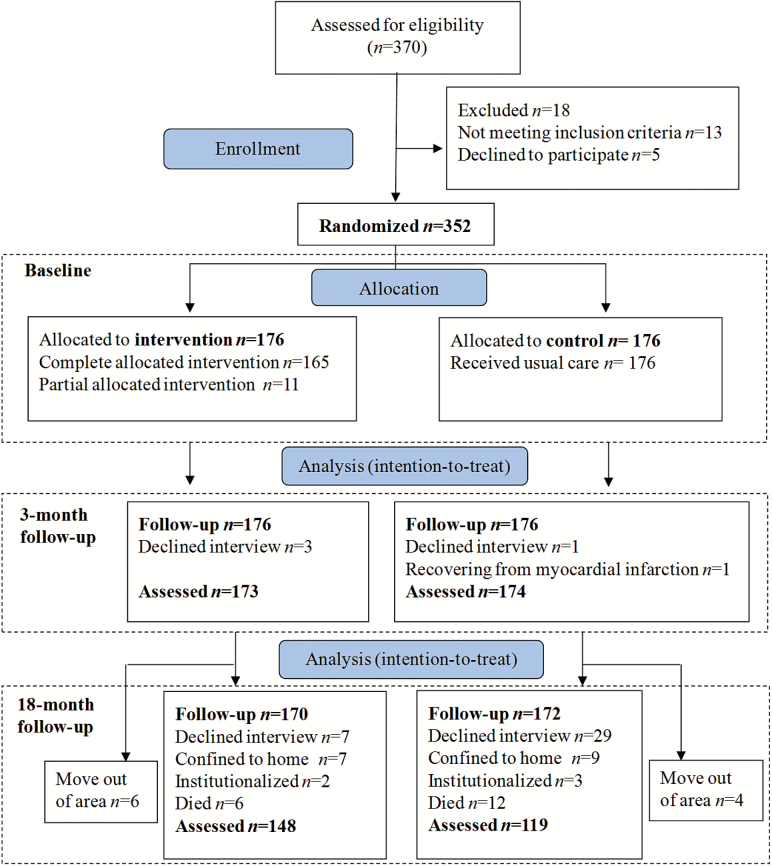
Eligible participants were randomized 1:1 to the IG and CG. Sequence was concealed until the interventions were assigned. Baseline and outcome measurements were blinded to group assignment. Follow-up evaluations were conducted by blind, clinical researchers. Figure 1 describes the flow-diagram of participants.
Figure 1.
CONSORT diagram reflecting flow of study participants.
Intervention
Briefly, participants in the IG received a multidisciplinary multifactorial therapy, consecutively applied to each subject in groups of 16 participants:
Structured physical activity, providing a well-established aerobics exercise program in each primary health care center, a 60-minute session twice a week on non-consecutive days for 6 weeks, conducted by physiotherapists.
Intake of 1 hyperproteic nutritional shake (Meritene Activ; Nestlé Health Science-NHS), which was taken daily for 6 weeks during the exercise training.
Memory workshops, consisting of a 90-minute session twice a week, 12 sessions of practical exercises (written, oral, corporal, and musical), conducted by speech therapists from the Rehabilitation Unit.
Medication Review, following STOPP criteria, with special focus on psychotropic drugs.
Control participants received the usual care. Both groups were also given counseling regarding dietary habits, lifestyle recommendations, and domestic hazards.
Outcome Variables
- Physical Dimension:
- a) SPPB, a standardized assessment tool of lower limb function (standing balance, repeated chair stands, gait speed).
- b) Evaluation of upper extremities’ strength by a handgrip dynamometer (HG).
- c) Functional Reach Test which measures standing balance and stretching.
- d) Unipodal Station Test which measures balance.
- Neuropsychological Performance:
- a) Short and Medium-Term Verbal Memory.
- b) Animal Naming Test which scores semantic verbal fluency category.
- c) Evocation of words beginning with one explicit letter which scores phonetic verbal fluency category.
- d) Designation of famous people’s names, which scores phonological retrieval failure.
- e) Verbal designation of images which scores visual recognition memory.
- f) Verbal abstraction of word pairs which scores connection between verbal recognition memory and neuroprocessing mechanisms.
Medication. Number of prescriptions.
See Supplementary Methods for further details.
Statistics
Outcome variables were assessed at baseline and at 3 and 18 months after randomization. Consistent with the protocol design, an intention-to-treat approach was employed. The incomplete cases were handled using the multiple imputation analysis by “mi impute pmm” procedure in Stata IC v12 statistical software. The estimates of the parameters for each imputed data set were combined using Rubin’s rules (26). Sensitivity analyses comparing complete cases versus multiple imputation analysis are shown in Supplementary Table 3.
The change of each outcome during the follow-up was assessed by multilevel mixed-effects linear regression adjusted by age, gender, marital status, educational status, income, and baseline TGUG and MEC-35. Interaction terms between the intervention, gender, and age were also tested and none were statistically significant.
Standardized effect sizes were calculated as the mean difference between IG and CG, divided by the pooled standard deviation of CG and IG change (27). Estimates were reported with corresponding 95% confidence intervals, and statistical significance was established as a p value less than .05.
Results
Between January 2013 and January 2015, participants were randomized to the multi-intervention (n = 176) or the control (n = 176) groups. The main characteristics of our study sample according to randomization group are presented in Table 1. A total of 265 participants (75.3%) were female, mean age 77.3 years, nearly half of them living alone (47.2%), The baseline features of the two groups were similar in terms of inclusion criteria, age, sex, civil status, cohabitation, comorbidity, and biological variables, including nutritional, functional, and mental performance, as shown in Supplementary Table 2.
Table 1.
Baseline Characteristics by Treatment Group
| Control Group (n = 176) | Intervention Group (n = 176) | p Value | ||
|---|---|---|---|---|
| Gender, n (%) | Male | 45 (25.6) | 42 (23.9) | .711 |
| Female | 131 (74.4) | 134 (76.1) | ||
| Age, years, mean (SD) | 77.4 (7.7) | 77.2 (6.8) | .770 | |
| Living alone, n (%) | 83 (47.2) | 83 (47.2) | 1.00 | |
| Marital Status, n (%) | Single | 23 (13.1) | 22 (12.5) | .884 |
| Widowed | 76 (43.2) | 80 (45.5) | ||
| Married | 67 (38.1) | 67 (38.1) | ||
| Divorced | 10 (5.7) | 7 (4.0) | ||
| Educational status, n (%) | Unfinished studies | 67 (38.1) | 78 (44.3) | .037 |
| Primary school | 80 (45.5) | 60 (34.1) | ||
| Secondary school | 25 (14.2) | 25 (14.2) | ||
| University degree | 4 (2.3) | 13 (7.4) | ||
| Falls, previous year, n (%) | 59 (33.5) | 57 (32.4) | .821 | |
| Hospital admissions, previous year, n (%) | 33 (18.8) | 40 (22.7) | .357 | |
| MEC-35 Lobo score, mean (SD) | 30.6 (4.1) | 31.2 (3.2) | .135 | |
| Lawton & Brody Scale, mean (SD) | 6.5 (1.9) | 6.6 (1.76) | .660 | |
| Barthel Index, mean (SD) | 96.1 (7.5) | 96.0 (6.2) | .938 | |
| Number of drugs/day, mean (SD) | 6.6 (3.8) | 7.7 (3.2) | .004 | |
| Charlson Index, mean (SD) | 1.3 (1.5) | 1.5 (1.6) | .203 | |
| TGUGT, mean (SD) | 14.5 (4.9) | 15.0 (4.9) | .368 | |
| Frailty criteria, n (%)a | Prefrail | 44 (25.0) | 45 (25.6) | .900 |
| Frail | 132 (75.0) | 131 (74.4) | ||
Note: n = number of subjects; SD = Standard deviation; TGUGT = Timed get up and go test.
aAdapted from ref. (2).
At the 12-week evaluation, follow-up data from 173 participants in the IG and 174 in the CG were available for analysis. At 18 months, 148 and 119 participants were reassessed, respectively (76% of the baseline sample, see Figure 1). The participants that were not assessed at the 18-month interview (n = 85) were similar to the interviewed group in terms of gender and baseline inclusion criteria, but 2 years older. Sixty-seven percent of the missing data group belonged to the CG, but there were no differences in baseline characteristics between IG and CG in terms of age, gender, inclusion criteria, and SPPB.
After the intervention, there were significant improvements in all major variables related to frailty measures in the IG while in the CG the result was inverse. There was a significant average increase of the difference between groups in SPPB score means adjusted by potential confounders at 3 and 18 months: 1.58 and 1.36 (p < .001), respectively. Standardized effect sizes at 3 and 18 months were rated as very large (1.18) and moderate (0.69), respectively.
Similar results were seen in strength of upper extremities and balance measurements, and in the mental performance battery, with also significant mean improvements between groups and medium and large standardized effect size indices at 3 months, but small at 18 months. All evaluated changes in physical and cognitive performance at 3 and 18 months are shown in Tables 2 and 3. Percentage of polypharmacy decreased 9.6% in the IG, but increased 4.5% in the CG after the intervention. Prescribed benzodiazepines decreased in the IG compared to the CG (−0.011 vs +0.023) but did not reach statistical significance.
Table 2.
Change in Physical Performance Measures and Prescriptions Between Intervention and Control Groups at 3 and 18 mo
| Control Group N = 176 | Intervention Group N = 176 | Adjusted Mean Difference (95% CI) Between Groups (IG-CG)a,b | |||
|---|---|---|---|---|---|
| Mean (SD)a | Mean (SD)a | p Value | SESc | ||
| Physical tests | |||||
| SPPB (range 0–12) | |||||
| Pre-I | 7.3 (2.4) | 7.1 (2.3) | <.001 | 1.18 | |
| Post-3 mo | 6.8 (2.3) | 8.1 (2.2) | 1.58 (1.29–1.86) | ||
| Post-18 mo | 7.0 (2.6) | 8.1 (2.3) | 1.36 (0.89–1.83) | <.001 | 0.69 |
| Handgrip (kg) | |||||
| Pre-I | 16.5 (7.4) | 16.5 (7.7) | <.001 | 1.12 | |
| Post-3 mo | 15.8 (6.9) | 18.6 (7.7) | 2.86 (2.32–3.41) | ||
| Post-18 mo | 15.7 (7.8) | 18.2 (7.9) | 2.49 (1.09–3.89) | .001 | 0.41 |
| Functional reach (cm) | |||||
| Pre-I | 82.2 (9.3) | 80.7 (10.1) | <.001 | 0.96 | |
| Post-3 mo | 80.7 (8.8) | 83.5 (9.3) | 4.34 (3.35–5.32) | ||
| Post-18 mo | 79.7 (10.5) | 82.7 (10.7) | 4.52 (2.32–6.72) | <.001 | 0.47 |
| Unipodal station (seconds) | |||||
| Pre-I | 8.2 (9.7) | 6.9 (8.0) | <.001 | 0.75 | |
| Post-3 mo | 7.3 (9.2) | 9.6 (9.1) | 3.58 (2.57–4.59) | ||
| Post-18 mo | 7.7 (9.0) | 9.3 (8.7) | 2.98 (1.11–4.84) | .002 | 0.37 |
| Number of drugs/day | |||||
| Pre-I | 6.6 (3.8) | 7.7 (3.2) | <.001 | 0.99 | |
| Post-3 mo | 7.2 (4.0) | 6.9 (3.2) | −1.39 (−1.69–−1.10) | ||
| Post-18 mo | 7.5 (4.1) | 7.5 (3.4) | −1.09 (−1.71–−0.47) | .001 | 0.37 |
Note: CG = Control group; CI = Confidence interval; I = Intervention; IG = Intervention group; N = Number; SD = Standard deviation; SES = Standardized effect size; SPPB = Short physical performance battery.
aIntention to treat analyses using missing value imputation. bMultilevel mixed-effects linear regression adjusted by age, gender, marital status, educational status, income, MEC-35 Lobo, TGUGT. cCohen’s d.
Table 3.
Change in Neuropsychological Performance Measures Between Intervention and Control Groups at 3 and 18 mo
| Control Group N = 176 | Intervention Group N = 176 | Adjusted Mean Difference (95% CI) Between Groups (IG-CG)a,b | |||
|---|---|---|---|---|---|
| Mean (SD)a | Mean (SD)a | p Value | SESc | ||
| Short-Term Verbal Memory (range 0–21) | |||||
| Pre-I | 5.6 (2.5) | 5.3 (2.7) | <.001 | 0.67 | |
| Post-3 mo | 5.0 (2.2) | 5.9 (2.7) | 1.19 (0.82–1.57) | ||
| Post-18 mo | 5.0 (2.4) | 5.3 (2.2) | 0.67 (0.13–1.21) | .015 | 0.28 |
| Medium-Term Verbal Memory: Retest (range 0–21) | |||||
| Pre-I | 4.0 (2.3) | 3.9 (2.4) | <.001 | 0.71 | |
| Post-3 mo | 3.8 (1.9) | 4.9 (2.4) | 1.11 (0.78–1.44) | ||
| Post-18 mo | 3.4 (2.2) | 4.0 (2.1) | 0.69 (0.12–1.21) | .016 | 0.31 |
| Animal Naming Test | |||||
| Pre-I | 15.0 (5.1) | 15.2 (4.6) | <.001 | 0.77 | |
| Post-3 mo | 14.4 (4.9) | 16.6 (4.8) | 2.01 (1.46–2.56) | ||
| Post-18 mo | 14.7 (5.3) | 15.9 (4.7) | 1.05 (0.12–1.97) | .026 | 0.26 |
| Evocation of words | |||||
| Pre-I | 19.1 (7.9) | 19.4 (8.5) | <.001 | 0.93 | |
| Post-3 mo | 17.8 (7.1) | 21.9 (8.8) | 3.64 (2.81–4.47) | ||
| Post-18 mo | 18.3 (7.9) | 20.8 (8.0) | 2.10 (0.50–3.71) | .010 | 0.32 |
| Designation of famous people’s names | |||||
| Pre-I | 19.8 (6.1) | 20.8 (6.2) | <.001 | 0.67 | |
| Post-3 mo | 19.1 (5.8) | 22.1 (6.1) | 1.92 (1.31–2.53) | ||
| Post-18 mo | 20.7 (6.3) | 22.4 (6.2) | 0.71 (−0.41–1.83) | .212 | 0.15 |
| Verbal designation of images (number in ≤3 seconds) | |||||
| Pre-I | 13.1 (1.2) | 13.1 (1.4) | <.001 | 0.59 | |
| Post-3 mo | 12.8 (1.6) | 13.5 (1.1) | 0.71 (0.46–0.97) | ||
| Post-18 mo | 12.9 (1.6) | 13.4 (1.2) | 0.53 (0.20–0.86) | .002 | 0.36 |
| Verbal abstraction of word pairs | |||||
| Pre-I | 3.5 (1.4) | 3.5 (1.5) | <.001 | 0.35 | |
| Post-3 mo | 3.2 (1.3) | 3.6 (1.5) | 0.40 (0.16–0.65) | ||
| Post-18 mo | 2.7 (1.5) | 3.1 (1.6) | 0.46 (0.40–0.89) | .032 | 0.25 |
Note: CG = Control group; CI = Confidence interval; I = Intervention; IG = Intervention group; N = Number; SD = Standard deviation; SES = Standardized effect size; SPPB = Short physical performance battery.
aIntention to treat analyses using missing value imputation. bMultilevel mixed-effects linear regression adjusted by age, gender, marital status, educational status, income, MEC-35 Lobo, TGUGT. c Cohen’s d.
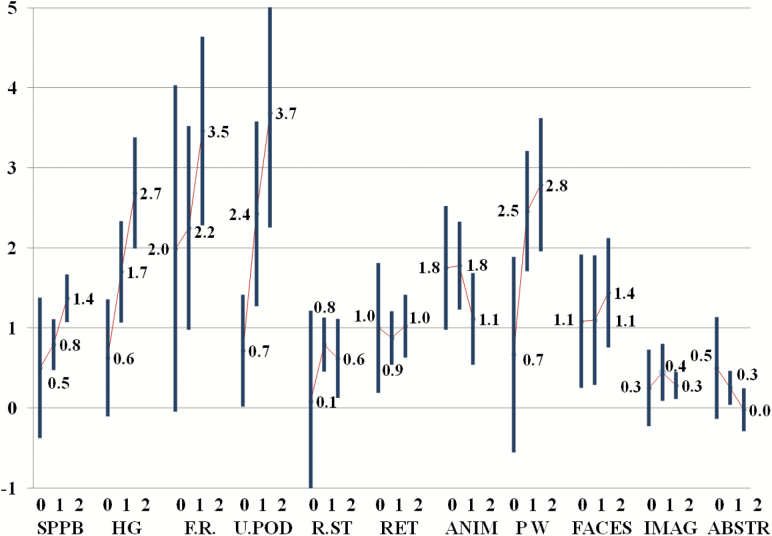
In the IG, the mean number of sessions attended was 13, out of a total of 24 in the program. Figure 2 shows mean change in the physical and cognitive variables at 3 months according to the range of sessions attended.
Figure 2.
Mean change score (95% CI) in outcome variables at 3 months, stratified by total number of sessions attended in the intervention group. Note: 0 = no sessions attended; 1 = 1–12 sessions; 2 = 13–24 sessions; SPPB = Short physical performance battery; HG = Hand grip; F.R. = Functional reach; U.POD = Unipodal station; R.ST = Short-term verbal memory; RET = Medium-term verbal memory; ANIM = Animal naming test; PW = Evocation of words beginning with P; FACES = Designation of people’s names; IMAG = Designation of images; ABSTR = Verbal abstraction of pairs.
Finally, attendance at the educational sessions was 48% in the CG and 52% in the IG.
Discussion
Our main finding is that a combined intervention that includes physical activity plus protein intake, along with memory workshops and medication review, improved functional and cognitive performance in frail/prefrail, community-dwelling, older adults at 12 weeks from commencing the intervention. The effect was significantly maintained up to at least 18 months. To the best of our knowledge, this is the first quadruple interventional trial performed to improve different frailty domains.
There is considerable evidence regarding the positive short and medium term impact of physical activity on strength, balance, and falls in moderately frail, elderly community-dwellers (28,29). Consistent with previous studies, our results in the IG showed a clear improvement in mobility, balance (better SPPB score), stretching, and muscle strength (handgrip), showing also sustained effects at long term.
Nutritional interventions with protein and energy supplementation have also reported good results in physical function for elderly people at risk of malnutrition (30). Our study revealed positive physical benefits for protein-calorie and micronutrient intake supplementation in association with physical activity, irrespective of basal nutritional status. However, further studies are required to determine whether this finding is explained by an adding effect or attributable to individual variables of dietary intake. As far as we are aware, only one study has demonstrated that nutritional supplementation alone can reduce frailty (31).
Frailty and cognition interact in the cycle leading to disability and dependency (32), and interventions in cognitive areas should be encouraged to prevent or even reverse further physical decline (33). It has also been reported that physical exercise training improves cognitive functioning and psychological well-being in frail, older adults (34). In agreement with these studies, we found that cognitive training program targeting short and medium-term memory, attention, and executive functions, along with physical training, had an effect on cognition (significant changes in memory and abstraction tests), and also improved motor balance and strength. Transference of cognitive remediation effects to mobility, as described by other authors (33), could be related to an indirect enhancement of social and functioning abilities among the IG participants.
An association between polypharmacy and frailty has been reported (35), and polypharmacy itself is considered to be a risk factor for negative outcomes (falls, cognitive impairment, mortality). As expected, our review of all medicated subjects led to a reduction of prescriptions (an average of one drug per subject, especially psychotropic medication). In concurrence with recent studies (36), the reduction was more effective in patients receiving polypharmacy than those who were not.
The combination of complex strategies is nowadays considered the optimum approach to improve frailty standards of care beyond current clinical practice (37). Recently, a comprehensive review (38) highlighted promising results related to these individually- tailored, multidisciplinary interventions, which appear to produce short-medium term benefits in decelerating frailty.
As previously stated, this is the first randomized controlled trial with intention-to-treat analysis which adds the novelty of concomitant cognition and medication interventions and their postevaluation. Our multistrategy resulted in a clear improvement in mobility and strength performance tests, enhancement of mental performance, and reduction of polypharmacy, with marked effect sizes for most comparisons at 3 months follow-up. Moreover, despite the fact that the intervention was not maintained beyond 3 months, significant improvements were still observed at 18 months. In contrast, in a study conducted in Sydney, the benefit of a multidomain intervention was not evident at 12 weeks follow-up and only apparent at 12 months (23).
Frailty is globally considered to be reversible and preventable in its initial phases (6), and prefrailty is a field of growing interest. Thus, identifying the target population for enrollment in programs addressing this issue is a challenge. Based on gait speed and balance (TGUGT), our study tackled a full segment of community-dwellers who ranged from prefrail to medium-frail when applying Fried criteria. We found similar improvements in all the patients’ parameters, suggesting that triage through simple performance measures such as TGUGT could be sufficient to enroll the elderly in potentially effective activities.
Following the guidelines of the Frailty Working Group (39), we carried out physical assessment through several complementary tests the results of which were partly self-reported and partly performance-based. Nevertheless, the primary outcomes (the SPPB, neurocognitive tests, and prescriptions) were objective measures that should reduce observer bias.
In contrast to other studies (30), our intervention was designed as a global, combined approach. Thus, the individual effect of protein supplementation and memory workshops could not be analyzed. Another limitation could be that, as nutritional parameters did not form part of the inclusion criteria, it is difficult to assess the real effect of the protein intake in the IG.
Intention-to-treat analysis was conducted to assess final outcomes, and missing values imputation and sensitivity analyses were performed using the recommended strategy (26). Although at 12 weeks only five individuals were not contacted, at 18 months 24% of the sample could not be reassessed (mainly from the CG) either due to worse health status or lacking motivation to participate in the reassessment. Nevertheless, bias caused by differential losses seems unlikely as baseline characteristics are similar between IG and CG in the complete data and missing data groups. Full attendance at the exercise activities and memory workshops was not achieved by most participants: mean attendance was 13 out of 24 sessions. We found a dose-respond pattern between number of attended sessions and improvements in physical outcomes, although this pattern was inconsistent in the cognitive ones (Figure 2).
As with the frailty phenotype, baseline characteristics were not likely to affect the intensity of the effect we found, and the final model was adjusted to those characteristics. Neither was any gender interaction observed, the effect was similar in both men and women.
There were no adverse events. Occasional absences from the sessions were due to external social events or acute-short illness unrelated to the intervention.
The intervention is readily transferable to routine clinical practice in integrated, elderly, healthcare settings with specific, clinically experienced teams. Indeed, it would be of interest to conduct trials testing the intervention in different environments, where our experience could be easily adapted. In this regard, the myriad physical, cognitive, and social activities taking place in most communities, if properly designed and conducted, could easily replace the more supervised and controlled interventions performed in trials. Moreover, the economic burden of falls, hospital admissions, and disability in the elderly is greater than the cost-effective specific interventions that could be carried out (40). Adherence to interventions may be a handicap. Nevertheless, although participants in the IG did not attend all the activities, we still found high adherence mainly due mainly to their enjoying social interaction in historically proactive districts. Although the intervention was limited to 3 months, the enhancement of community networks may also have added to the sustained long-term improvement found in the IG.
Conclusions
The results of this study provide further evidence regarding the beneficial effect for frail, elderly individuals of a multifactorial intervention including exercise training (combining functional, resistance, and aerobic exercise modes), protein intake, cognition workshops, and medication review as a global strategy to reduce loss of autonomy and its risk factors. Our findings show the feasibility of identifying frail/prefrail individuals through simple performance measures in primary care settings, and how a multidisciplinary, coordinated care approach improves function and cognition in elderly community-dwellers. Our results, the long term changes in frailty parameters, and the social empowerment achieved, may lead to the prevention of future negative outcomes in the frail population. The scalability of our intervention encourages future collaboration with community organizations in elderly-friendly cities.
Availability of Data and Material
The datasets used are available from the corresponding author on reasonable request.
Funding
This study was supported by ISCIII, Ministry of Economy and Competitiveness, Spain, Technical, Scientific and Innovation Research National Plan 2008–2011, cofunded with European Union ERDF funds; PI12/01503.
Conflict of Interest
None reported.
Supplementary Material
References
- 1. Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. The Lancet. 2013;381:752–762. doi:10.1016/S0140-6736(12)62167–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fried LP, Tangen CM, Walston J, et al. ; Cardiovascular Health Study Collaborative Research Group Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–M156. [DOI] [PubMed] [Google Scholar]
- 3. Mitnitski AB, Mogilner AJ, Rockwood K. Accumulation of deficits as a proxy measure of aging. ScientificWorldJournal. 2001;1:323–336. doi:10.1100/tsw.2001.58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Shamliyan T, Talley KM, Ramakrishnan R, Kane RL. Association of frailty with survival: a systematic literature review. Ageing Res Rev. 2013;12:719–736. doi:10.1016/j.arr.2012.03.001 [DOI] [PubMed] [Google Scholar]
- 5. Gill TM, Gahbauer EA, Allore HG, Han L. Transitions between frailty states among community-living older persons. Arch Intern Med. 2006;166:418–423. doi:10.1001/archinte.166.4.418 [DOI] [PubMed] [Google Scholar]
- 6. Wilson JF. Frailty--and its dangerous effects--might be preventable. Ann Intern Med. 2004;141:489–492. http://www.ncbi.nlm.nih.gov/pubmed/15381535. Accessed March 13, 2017. [DOI] [PubMed] [Google Scholar]
- 7. Regional Committee for Europe Sixty-second Session Strategy and Action Plan for Healthy Ageing in Europe Strategy and Action Plan for Healthy Ageing in http://www.euro.who.int/en/who-we-are/governance. Accessed March 13, 2017.
- 8. Theou O, Stathokostas L, Roland KP, et al. . The effectiveness of exercise interventions for the management of frailty: a systematic review. J Aging Res. 2011;2011:569194. doi:10.4061/2011/569194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Giné-Garriga M, Roqué-Fíguls M, Coll-Planas L, Sitjà-Rabert M, Salvà A. Physical exercise interventions for improving performance-based measures of physical function in community-dwelling, frail older adults: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2014;95:753–769.e3. doi:10.1016/j.apmr.2013.11.007 [DOI] [PubMed] [Google Scholar]
- 10. Ollonqvist K, Grönlund R, Karppi SL, Salmelainen U, Poikkeus L, Hinkka K. A network-based rehabilitation model for frail elderly people: development and assessment of a new model. Scand J Caring Sci. 2007;21:253–261. doi:10.1111/j.1471-6712.2007.00464.x [DOI] [PubMed] [Google Scholar]
- 11. Abizanda P, López MD, García VP, et al. . Effects of an oral nutritional supplementation plus physical exercise intervention on the physical function, nutritional status, and quality of life in frail institutionalized older adults: the ACTIVNES Study. J Am Med Dir Assoc. 2015;16(5):439.e9-439.e16. doi:10.1016/j.jamda.2015.02.005 [DOI] [PubMed] [Google Scholar]
- 12. Gill TM, Baker DI, Gottschalk M, Peduzzi PN, Allore H, Byers A. A program to prevent functional decline in physically frail, elderly persons who live at home. N Engl J Med. 2002;347:1068–1074. doi:10.1056/NEJMoa020423 [DOI] [PubMed] [Google Scholar]
- 13. Frost H, Haw S, Frank J. Interventions in community settings that prevent or delay disablement in later life: an overview of the evidence. Qual Ageing Older Adults. 2012;13:212–230. doi:10.1108!14717791211264241 [Google Scholar]
- 14. Volpi E, Mittendorfer B, Rasmussen BB, Wolfe RR. The response of muscle protein anabolism to combined hyperaminoacidemia and glucose-induced hyperinsulinemia is impaired in the elderly. J Clin Endocrinol Metab. 2000;85:4481–4490. doi:10.1210/jcem.85.12.7021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Basaria S, Coviello AD, Travison TG, et al. . Adverse events associated with testosterone administration. N Engl J Med. 2010;363:109–122. doi:10.1056/NEJMoa1000485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Malafarina V, Uriz-Otano F, Iniesta R, Gil-Guerrero L. Effectiveness of nutritional supplementation on muscle mass in treatment of sarcopenia in old age: a systematic review. J Am Med Dir Assoc. 2013;14:10–17. doi:10.1016/j.jamda.2012.08.001 [DOI] [PubMed] [Google Scholar]
- 17. Canevelli M, Cesari M, van Kan GA. Frailty and cognitive decline: how do they relate?Curr Opin Clin Nutr Metab Care. 2015;18:43–50. doi:10.1097/MCO.0000000000000133 [DOI] [PubMed] [Google Scholar]
- 18. Avila-Funes JA, Amieva H, Barberger-Gateau P, et al. . Cognitive impairment improves the predictive validity of the phenotype of frailty for adverse health outcomes: the three-city study. J Am Geriatr Soc. 2009;57:453–461. doi:10.1111/j.1532-5415.2008.02136.x [DOI] [PubMed] [Google Scholar]
- 19. van de Rest O, van der Zwaluw NL, Tieland M, et al. . Effect of resistance-type exercise training with or without protein supplementation on cognitive functioning in frail and pre-frail elderly: secondary analysis of a randomized, double-blind, placebo-controlled trial. Mech Ageing Dev. 2014;136–137: doi:10.1016/j.mad.2013.12.005 [DOI] [PubMed] [Google Scholar]
- 20. Olchik MR, Farina J, Steibel N, Teixeira AR, Yassuda MS. Memory training (MT) in mild cognitive impairment (MCI) generates change in cognitive performance. Arch Gerontol Geriatr. 2013;56:442–447. doi:10.1016/j.archger.2012.11.007 [DOI] [PubMed] [Google Scholar]
- 21. Wang R, Chen L, Fan L, et al. . Incidence and effects of polypharmacy on clinical outcome among patients aged 80+: a five-year follow-up study. Pietropaolo M, ed. PLoS One. 2015;10(11):e0142123. doi:10.1371/journal.pone.0142123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Patterson SM, Cadogan CA, Kerse N, et al. . Interventions to improve the appropriate use of polypharmacy for older people. Hughes C, ed. Cochrane Database Syst Rev. 2014;(10):CD008165. doi:10.1002/14651858.CD008165.pub3 [DOI] [PubMed] [Google Scholar]
- 23. Cameron ID, Fairhall N, Langron C, et al. . A multifactorial interdisciplinary intervention reduces frailty in older people: randomized trial. BMC Med. 2013;11:65. doi:10.1186/1741-7015-11-65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tarazona-Santabalbina FJ, Gómez-Cabrera MC, Pérez-Ros P, et al. . A multicomponent exercise intervention that reverses frailty and improves cognition, emotion, and social networking in the community-dwelling frail elderly: a randomized clinical trial. J Am Med Dir Assoc. 2016;17:426–433. doi:10.1016/j.jamda.2016.01.019 [DOI] [PubMed] [Google Scholar]
- 25. Romera L, Orfila F, Segura JM, et al. . Effectiveness of a primary care based multifactorial intervention to improve frailty parameters in the elderly: a randomised clinical trial: rationale and study design. BMC Geriatr. 2014;14:125. doi:10.1186/1471-2318-14-125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. White IR, Horton NJ, Carpenter J, Pocock SJ. Strategy for intention to treat analysis in randomised trials with missing outcome data. BMJ. 2011;342:d40. doi:10.1136/bmj.d40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sullivan GM. FAQs about effect size. J Grad Med Educ. 2012;4:283–284. doi:10.4300/JGME-D-12-00162.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cesari M, Vellass B, Hsu FC, et al. ; LIFE Study Group A physical activity intervention to treat the frailty syndrome in older persons-results from the LIFE-P study. J Gerontol A Biol Sci Med Sci. 2015;70:216–222. doi:10.1093/gerona/glu099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Stubbs B, Brefka S, Denkinger MD. What Works to prevent falls in community-dwelling older adults? Umbrella review of meta-analyses of randomized controlled trials. Phys Ther. 2015;95:1095–1110. doi:10.2522/ptj.20140461 [DOI] [PubMed] [Google Scholar]
- 30. Kim CO, Lee KR. Preventive effect of protein-energy supplementation on the functional decline of frail older adults with low socioeconomic status: a community-based randomized controlled study. J Gerontol A Biol Sci Med Sci. 2013;68:309–316. doi:10.1093/gerona/gls167 [DOI] [PubMed] [Google Scholar]
- 31. Ng TP, Feng L, Nyunt MS, et al. . Nutritional, physical, cognitive, and combination interventions and frailty reversal among older adults: a randomized controlled #rial. Am J Med. 2015;128:1225–1236.e1. doi:10.1016/j.amjmed.2015.06.017 [DOI] [PubMed] [Google Scholar]
- 32. Robertson DA, Savva GM, Kenny RA. Frailty and cognitive impairment–a review of the evidence and causal mechanisms. Ageing Res Rev. 2013;12:840–851. doi:10.1016/j.arr.2013.06.004 [DOI] [PubMed] [Google Scholar]
- 33. Vergheese J, Mahoney J, Ambrose AF, Wang C, Holtzer R. Effect of cognitive remediation on gait in sedentary seniors. J Gerontol A Biol Sci Med Sci. 2010;65:1338–1343. doi:10.1093/gerona/glq127 [DOI] [PubMed] [Google Scholar]
- 34. Langlois F, Vu TT, Chassé K, Dupuis G, Kergoat MJ, Bherer L. Benefits of physical exercise training on cognition and quality of life in frail older adults. J Gerontol B Psychol Sci Soc Sci. 2013;68:400–404. doi:10.1093/geronb/gbs069 [DOI] [PubMed] [Google Scholar]
- 35. Herr M, Robine JM, Pinot J, Arvieu JJ, Ankri J. Polypharmacy and frailty: prevalence, relationship, and impact on mortality in a French sample of 2350 old people. Pharmacoepidemiol Drug Saf. 2015;24:637–646. doi:10.1002/pds.3772 [DOI] [PubMed] [Google Scholar]
- 36. Hayashi Y, Godai A, Yamada M, et al. . Reduction in the numbers of drugs administered to elderly in-patients with polypharmacy by a multidisciplinary review of medication using electronic medical records. Geriatr Gerontol Int. 2017;17:653–658. doi:10.1111/ggi.12764 [DOI] [PubMed] [Google Scholar]
- 37. Beswick AD, Rees K, Dieppe P, et al. . Complex interventions to improve physical function and maintain independent living in elderly people: a systematic review and meta-analysis. Lancet. 2008;371:725–735. doi:10.1016/S0140-6736(08)60342-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Puts MT, Toubasi S, Atkinson E, et al. . Interventions to prevent or reduce the level of frailty in community-dwelling older adults: a protocol for a scoping review of the literature and international policies. BMJ Open. 2016;6. (3):e010959. doi:10.1136/bmjopen-2015-010959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ferrucci L, Guralnik JM, Studenski S, Fried LP, Cutler GB Jr, Walston JD; Interventions on Frailty Working Group Designing randomized, controlled trials aimed at preventing or delaying functional decline and disability in frail, older persons: a consensus report. J Am Geriatr Soc. 2004;52:625–634. doi:10.1111/j.1532-5415.2004.52174.x [DOI] [PubMed] [Google Scholar]
- 40. McLean K, Day L, Dalton A. Economic evaluation of a group-based exercise program for falls prevention among the older community-dwelling population. BMC Geriatr. 2015;15:33. doi:10.1186/s12877-015-0028-x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.