Key Points
Question
What are the risk factors for septorhinoplasty after the initial treatment of isolated nasal fracture?
Findings
This population-based analysis of 78 474 patients found that open treatment was associated with increased risk of subsequent septorhinoplasty in patients without a preexisting nasal obstruction or defect. In patients with a preexisting obstruction or defect, an observation-only approach was associated with greatest risk.
Meaning
Preexisting nasal obstruction or defect and other aspects of a patient’s history should be considered when managing nasal fracture to assess the likelihood of surgical revision.
Abstract
Importance
Initial treatment of nasal fractures can result in long-standing cosmetic or functional defects, but the risk factors for subsequent septorhinoplasty have not been explored.
Objective
To assess the risk factors for septorhinoplasty after the initial treatment of isolated nasal fracture.
Design, Setting, and Participants
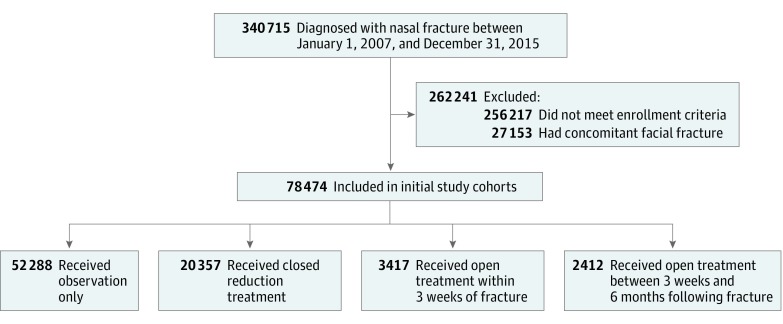
This retrospective population-based analysis of US patients diagnosed with nasal fracture between January 1, 2007, and December 31, 2015, used insurance claims data from the Commercial and Medicare Supplemental categories of the Truven Health MarketScan database. Of the 340 715 patients diagnosed with nasal fracture, 78 474 were included in the final study cohort, excluding those who did not meet enrollment criteria or were diagnosed with concomitant facial fracture. Patients were classified into 1 of 4 groups according to the type and timing of treatment.
Main Outcomes and Measures
Septorhinoplasty between 6 and 24 months after nasal fracture diagnosis. Explanatory variables included initial fracture treatment, demographics, comorbidities, and diagnoses associated with a preexisting nasal obstruction or defect.
Results
Most of the 78 474 patients were under 65 years of age (66 770 [85.1%]) and male (41 997 [53.5%]) and lived in an urban area (67 938 [86.6%]). Among patients with no preexisting diagnosis of nasal obstruction or defect, open treatment within 3 weeks (adjusted odds ratio [aOR], 1.76; 95% CI, 1.33-2.32) of nasal fracture and between 3 weeks and 6 months (aOR, 1.52; 95% CI, 1.14-2.04) after fracture were associated with increased risk of subsequent septorhinoplasty. In patients with a diagnosis of preexisting nasal obstruction or defect, observation (aOR, 3.56; 95% CI, 2.80-4.53), closed reduction treatment (aOR, 3.10; 95% CI, 1.93-4.96), and open treatment within 3 weeks (aOR, 2.02; 95% CI, 1.48-2.77) of fracture were all associated with increased risk of subsequent septorhinoplasty, with observation having the highest risk. Patients were also more likely to undergo subsequent septorhinoplasty if they were younger than 65 years, with the greatest risk seen in patients 18 to 34 years of age (aOR, 6.02; 95% CI, 4.26-8.50), lived in an urban area (aOR, 1.21; 95% CI, 1.01-1.44), or had a history of anxiety (aOR, 1.45; 95% CI, 1.18-1.78), but less likely if they were male (aOR, 0.82; 95% CI, 0.73-0.91).
Conclusions and Relevance
This study suggests that a preexisting diagnosis of nasal obstruction or defect and other aspects of a patient’s history are factors to consider when assessing the likelihood of surgical revision of initial treatment of nasal fracture.
Level of Evidence
NA.
This population-based analysis uses a large insurance claims database to identify risk factors associated with corrective septorhinoplasty after initial treatment for nasal fractures.
Introduction
Nasal fractures represent one of the most common traumatic injuries to the face, with close to 40% of all facial fractures involving the nose.1 Treatment decisions must address the acute presentation of the injury while optimizing long-term functional and cosmetic outcomes.2,3,4 Many treatment algorithms have, therefore, been devised to guide the classification and management of nasal fractures, but few studies have assessed the association between early treatment approaches and the likelihood of subsequent revision surgery.5 A recent systematic review found no evidence that closed and open reduction procedures result in different rates of nasal deformity,3 whereas other studies have suggested that open reduction or concomitant septorhinoplasty, compared with closed reduction treatment, can reduce the risk of subsequent surgery.1,5,6 Many of these studies, however, are limited in power because of their small sample size and rely on single-institution samples that may not be generalizable to all populations or geographies.
Therefore, further analysis is needed to understand the association between the initial nasal fracture treatment and the likelihood of subsequent septorhinoplasty to better inform patients and physicians in the setting of acute injury. The objective of this study was to conduct a population-based analysis of a large insurance claims database to characterize initial treatment pathways for isolated nasal fracture and to determine the factors associated with septorhinoplasty after initial treatment.
Methods
Data and Study Cohort
A retrospective analysis of insurance claims data was conducted for the period January 1, 2007, through December 31, 2015, using the Commercial and Medicare Supplemental categories of the Truven Health MarketScan database. The database represents more than 200 million individuals across the United States who receive health insurance from self-insured employers and other private health plans and includes claims for inpatient and outpatient services as well as for outpatient pharmacy. Patients with Medicaid and original Medicare were not included. Procedures were identified using Current Procedural Terminology codes, and diagnoses used International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9 CM) codes (eTable in the Supplement). The Research and Compliance Office of Stanford University deemed this study exempt from human studies review.
All patients diagnosed with an isolated nasal fracture (ICD-9 CM code 802.0 or 802.1) were identified, and the date of the earliest encounter with nasal fracture diagnosis was recorded as the date of incidence. Patients were excluded if diagnosed with other facial fractures (eg, to the mandible, maxillary bones, or orbit) on the same date to limit the analysis to isolated nasal fractures. To ensure that observations reflected incident cases and that sufficient follow-up data were collected, patients were required to have 12 months of continuous enrollment prior to their nasal fracture diagnosis and 24 months of continuous enrollment after diagnosis. Follow-up time was standardized for all patients at 24 months.
Explanatory Variables
To assess treatment pathways immediately after nasal fracture, patients were classified into 1 of 4 groups according to the type and timing of treatment: (1) closed reduction treatment within 3 weeks of fracture; (2) open treatment within 3 weeks of fracture; (3) open treatment between 3 weeks and 6 months after fracture; or (4) observation, where neither closed nor open treatment was performed within 6 months after fracture. Open treatment included both open reduction and septorhinoplasty procedures to account for potential variation in coding practices and instances in which open reduction and septorhinoplasty were performed concurrently.7 Patients treated with closed reduction later than 3 weeks after fracture were excluded, as this method is unlikely to be effective and is infrequently performed after this point.5,8 The closed reduction and open treatment cohorts were further divided into subgroups on the basis of treatment timing: (1) closed reduction treatment between 0 and 10 days and between 11 and 21 days after fracture and (2) open treatment between 0 and 10 days, between 11 and 21 days, and between 22 days and 6 months after fracture.
Other patient and treatment characteristics included age; sex; insurance plan type; geographic region; and whether patients lived in an urban area, defined as any geography within a metropolitan statistical area.6,9,10 Treatment characteristics were also collected, such as time from nasal fracture to initial treatment (for patients with closed reduction treatment or open treatment) and time from fracture to first septorhinoplasty after initial treatment. Specific comorbidities captured included history of tobacco use, autoimmune disease or immunodeficiency, anxiety, deviated septum, turbinate hypertrophy, nasal obstruction, acquired deformity of the nose, congenital deformity of the nose, late effect of prior nasal injury, and malunion of prior nasal injury (eTable in the Supplement).9 These comorbidities were assessed in the year preceding 2 weeks prior to the fracture date, to ensure that they did not arise alongside the incident nasal fracture episode. Patients’ general comorbidity burden was also measured using the van Walraven formulation of the Elixhauser Comorbidity Index, which encapsulates 30 common comorbidities as a single numeric score that represents association with mortality.11
Outcome Variables
The primary outcome was the occurrence of septorhinoplasty, as defined by any record of a corresponding billing code (eTable in the Supplement) between 6 and 24 months after the initial diagnosis of nasal fracture, when edema has resolved and the nasal bones and septum have stabilized sufficiently for surgery.12
Statistical Methods
Descriptive statistics were used to summarize the distribution of variables across the study cohort. Differences in the van Walraven comorbidity index across the 4 treatment cohorts were tested for statistical significance using the nonparametric Kruskal-Wallis rank sum analysis of variance, and distributions of categorical variables were tested using a χ2 test. Differences in subsequent septorhinoplasty rates across treatment cohorts and among timing-based subgroups within a treatment cohort were assessed for statistical significance using a 2-tailed population proportion test. Statistical significance was determined at a threshold of P = .05.
The effect of a covariate on the risk of septorhinoplasty between 6 and 24 months after nasal fracture was assessed using multivariable logistic regression and was described as an adjusted odds ratio (aOR) that controls for the effect of other covariates. Additional multiple logistic regression models included interaction terms to assess the interactions of interest. Unadjusted ORs calculated from univariable logistic regression were also recorded for each covariate. Estimates were reported with 95% CIs.
Data extraction and manipulation were performed using SAS, version 9.4 (SAS Institute Inc), and further statistical analysis was performed using R, version 3.4.2 (R Foundation for Statistical Computing).
Results
Patient Characteristics
A total of 340 715 patients were diagnosed with nasal fracture between January 1, 2007, and December 31, 2015 (Figure). Among these patients, 262 241 (77.0%) were excluded, 256 217 (75.2%) did not fulfill enrollment criteria, and 27 153 (8.0%) had concomitant facial fracture. Thus, 78 474 of 340 715 patients (23.0%) were included in the final study cohort, in which most patients were under 65 years of age (66 770 of 78 474 [85.1%]), were male (41 997 of 78 474 [53.5%]), and lived in an urban area (67 938 of 78 474 [86.6%]) (Table 1).
Figure. Study Flow Diagram.
Patients in the initial study cohort were classified into 4 groups (observation, closed reduction treatment, open treatment within 3 weeks of fracture, and open treatment between 3 weeks and 6 months after fracture) on the basis of initial nasal fracture treatment. Patients may not have met multiple exclusion criteria. There are patients who both did not meet enrollment criteria and had concomitant facial fracture. Adding the number of patients who met each exclusion criterion will result in a sum that is greater than the total number of patients excluded.
Table 1. Cohort Characteristics.
| Characteristic | Initial Treatment | Total | ||||
|---|---|---|---|---|---|---|
| Observation | Closed Reduction | Open, Within 3 wk | Open, Between 3 wk and 6 mo | P Value | ||
| No. | 52 288 | 20 357 | 3417 | 2412 | 78 474 | |
| Age group, y, No. (%) | ||||||
| ≤17 | 16 765 (32.1) | 8844 (43.4) | 770 (22.5) | 502 (20.8) | <.001 | 26 881 (34.3) |
| 18-34 | 10 726 (20.5) | 4753 (23.3) | 1182 (34.6) | 821 (34.0) | 17 482 (22.3) | |
| 35-44 | 4867 (9.3) | 1476 (7.3) | 520 (15.2) | 367 (15.2) | 7230 (9.2) | |
| 45-54 | 5494 (10.5) | 1585 (7.8) | 490 (14.3) | 366 (15.2) | 7935 (10.1) | |
| 55-64 | 5275 (10.1) | 1384 (6.8) | 332 (9.7) | 251 (10.4) | 7242 (9.2) | |
| ≥65 | 9161 (17.5) | 2315 (11.4) | 123 (3.6) | 105 (4.4) | 11 704 (14.9) | |
| Male sex, No. (%) | 27 033 (51.7) | 11 782 (57.9) | 1942 (56.8) | 1240 (51.4) | <.001 | 41 997 (53.5) |
| Plan type, No. (%) | ||||||
| Comprehensive | 5255 (10.1) | 1449 (7.1) | 133 (3.9) | 87 (3.6) | <.001 | 6924 (8.8) |
| EPO | 719 (1.4) | 298 (1.5) | 54 (1.6) | 43 (1.8) | 1114 (1.4) | |
| HMO | 7294 (13.9) | 2648 (13.0) | 421 (12.3) | 346 (14.3) | 10 709 (13.6) | |
| POS | 4234 (8.1) | 1674 (8.2) | 367 (10.7) | 178 (7.4) | 6453 (8.2) | |
| PPO | 29 547 (56.5) | 12 150 (59.7) | 2056 (60.2) | 1492 (61.9) | 45 245 (57.7) | |
| POS w/capitation | 290 (0.6) | 73 (0.4) | 26 (0.8) | 11 (0.5) | 400 (0.5) | |
| CDHP | 2153 (4.1) | 967 (4.8) | 162 (4.7) | 115 (4.8) | 3397 (4.3) | |
| HDHP | 1132 (2.2) | 502 (2.5) | 93 (2.7) | 58 (2.4) | 1785 (2.3) | |
| NA | 1664 (3.2) | 596 (2.9) | 105 (3.1) | 82 (3.4) | 2447 (3.1) | |
| Region, No. (%) | ||||||
| Northeast | 11 913 (22.8) | 4232 (20.8) | 673 (19.7) | 453 (18.8) | <.001 | 17 271 (22.0) |
| North central | 12 825 (24.5) | 5102 (25.1) | 736 (21.5) | 544 (22.6) | 19 207 (24.5) | |
| South | 17 043 (32.6) | 6814 (33.5) | 1136 (33.2) | 770 (31.9) | 25 763 (32.8) | |
| West | 9592 (18.3) | 3858 (19.0) | 822 (24.1) | 613 (25.4) | 14 885 (19.0) | |
| Unknown | 915 (1.7) | 351 (1.7) | 50 (1.5) | 32 (1.3) | 1348 (1.7) | |
| Urban area, No. (%) | 45 248 (86.5) | 17 556 (86.2) | 3014 (88.2) | 2120 (87.9) | .004 | 67 938 (86.6) |
| Year of fracture, No. (%) | ||||||
| 2008 | 6450 (12.3) | 2247 (11.0) | 445 (13.0) | 288 (11.9) | <.001 | 9430 (12.0) |
| 2009 | 9622 (18.4) | 3363 (16.5) | 708 (20.7) | 479 (19.9) | 14 172 (18.1) | |
| 2010 | 10 475 (20.0) | 3877 (19.0) | 708 (20.7) | 481 (19.9) | 15 541 (19.8) | |
| 2011 | 9118 (17.4) | 3740 (18.4) | 546 (16.0) | 411 (17.0) | 13 815 (17.6) | |
| 2012 | 9717 (18.6) | 4099 (20.1) | 579 (16.9) | 453 (18.8) | 14 848 (18.9) | |
| 2013 | 6906 (13.2) | 3031 (14.9) | 431 (12.6) | 300 (12.4) | 10 668 (13.6) | |
| van Walraven index, median (IQR) | 0.00 (0.00-5.00) |
0.00 (0.00-3.00) |
0.00 (0.00-3.00) |
0.00 (0.00-3.00) |
<.001 | 0.00 (0.00-4.00) |
| Prior comorbidities, No. (%) | ||||||
| Tobacco use | 1237 (2.4) | 351 (1.7) | 83 (2.4) | 52 (2.2) | <.001 | 1723 (2.2) |
| Autoimmune or immunodeficiency disease | 880 (1.7) | 235 (1.2) | 45 (1.3) | 26 (1.1) | <.001 | 1186 (1.5) |
| Anxiety | 2711 (5.2) | 874 (4.3) | 184 (5.4) | 158 (6.6) | <.001 | 3927 (5.0) |
| Deviated septum | 1078 (2.1) | 175 (0.9) | 1101 (32.2) | 279 (11.6) | <.001 | 2633 (3.4) |
| Turbinate hypertrophy | 516 (1.0) | 94 (0.5) | 424 (12.4) | 119 (4.9) | <.001 | 1153 (1.5) |
| Nasal obstruction | 962 (1.8) | 248 (1.2) | 504 (14.7) | 140 (5.8) | <.001 | 1854 (2.4) |
| Other nasal injurya | 223 (0.4) | 39 (0.2) | 297 (8.7) | 60 (2.5) | <.001 | 619 (0.8) |
Abbreviations: CDHP, consumer-driven health plan; EPO, exclusive provider organization; HDHP, high-deductible health plan; HMO, health maintenance organization; IQR, interquartile range; NA, not applicable or missing; POS, point of service; PPO, preferred provider organization.
Includes acquired and congenital deformities of the nose, late effect of fracture of skull and face, and malunion of previous fracture.
Initial Treatment and Rates of Subsequent Septorhinoplasty
Across the final study cohort, 52 288 of 78 474 patients (66.6%) were managed with observation only, 20 357 (26.0%) underwent closed reduction treatment, 3417 (4.4%) underwent open treatment within 3 weeks of nasal fracture, and 2412 (3.1%) underwent open treatment between 3 weeks and 6 months after fracture (Figure). The median (interquartile range [IQR]) time between fracture and initial treatment was 0 (0-6) days for closed reduction treatment, 1 (0-8) day for open treatment within 3 weeks of fracture, and 64 (40-102) days for open treatment between 3 weeks and 6 months after fracture.
Rates of septorhinoplasty between 6 and 24 months after nasal fracture were 1.7% (896 of 52 288) for observation, 1.6% (331 of 20 357) for closed reduction treatment, 3.6% (123 of 3417) for open treatment within 3 weeks of fracture, and 2.9% (71 of 2412) for open treatment between 3 weeks and 6 months after fracture (Table 2)—differences that were statistically significant (P < .001). Among patients treated with closed reduction, 1.6% (298 of 18 912) treated between 0 and 10 days after fracture had subsequent septorhinoplasty, compared with 2.3% (33 of 1445) of those treated between 11 and 21 days after fracture, a difference that was not statistically significant (P = .05). Among patients with open treatment, 3.4% (95 of 2766) treated between 0 and 10 days after fracture had subsequent septorhinoplasty, compared with 4.3% (28 of 644) of those treated between 11 and 21 days and 2.9% (71 of 2412) treated between 22 days and 6 months after fracture, differences that were also not statistically significant (P = .19). The median (IQR) time between fracture and septorhinoplasty after initial treatment was 11.4 (8.0-16.3) months for observation, 11.2 (7.9-16.1) months for closed reduction treatment, 12.5 (9.0-16.6) months for open treatment within 3 weeks of fracture, and 12.6 (9.6-16.6) months for open treatment between 3 weeks and 6 months after fracture.
Table 2. Rate of Septorhinoplasty Between 6 and 24 Months After Nasal Fracture, by Initial Treatment Modality and Timing.
| Treatment | No. of Patients | No. of Patients Receiving Septorhinoplasty 6-24 mo After Initial Treatment | Subsequent Septorhinoplasty Rate, % | P Value |
|---|---|---|---|---|
| Initial treatment | ||||
| Observation | 52 288 | 896 | 1.7 | <.001 |
| Closed | 20 357 | 331 | 1.6 | |
| Open within 3 wk | 3417 | 123 | 3.6 | |
| Open between 3 wk and 6 mo | 2412 | 71 | 2.9 | |
| Initial treatment, days after fracture diagnosis | ||||
| Closed | ||||
| 0-10 | 18 912 | 298 | 1.6 | .05 |
| 11-21 | 1445 | 33 | 2.3 | |
| Opena | .19 | |||
| 0-10 | 2766 | 95 | 3.4 | |
| 11-21 | 644 | 28 | 4.3 | |
| 22 d-6 mo | 2412 | 71 | 2.9 | |
Seven of 5829 patients (0.1%) who received open treatment were not reflected in the analysis of septorhinoplasty rates by timing, because they received open treatment in more than 1 of the assessed time intervals.
Factors in Subsequent Septorhinoplasty
Multivariable logistic regression identified several factors that were independently associated with risk of septorhinoplasty between 6 and 24 months after nasal fracture (Table 3). Age younger than 65 years was associated with increased risk of subsequent septorhinoplasty, with the greatest risk seen in patients 18 to 34 years of age (aOR, 6.02; 95% CI, 4.26-8.50). Patients were less likely to have undergone subsequent septorhinoplasty if they were male (aOR, 0.82; 95% CI, 0.73-0.91). Patients were more likely to have undergone subsequent septorhinoplasty if they lived in an urban area (aOR, 1.21; 95% CI, 1.01-1.44) or in the western US region (aOR, 1.30 [compared with the southern region]; 95% CI, 1.12-1.51). History of anxiety was associated with increased risk of subsequent septorhinoplasty (aOR, 1.45; 95% CI, 1.18-1.78), as was history of preexisting nasal obstruction or defect—specifically, previous diagnoses of deviated septum (aOR, 2.26; 95% CI, 1.77-2.88); nasal obstruction (aOR, 1.48; 95% CI, 1.14-1.93); or other nasal injuries, including acquired or congenital defects and late effect or malunion of previous fractures (aOR, 1.50; 95% CI, 1.04-2.17). A statistically significant association was not seen with a previous diagnosis of turbinate hypertrophy.
Table 3. Analysis of Factors Associated With Septorhinoplasty After Initial Treatment of Nasal Fracture.
| Characteristic | OR (95% CI) | |
|---|---|---|
| Unadjusted | Adjusted | |
| Age group, y | ||
| ≤17 | 3.17 (2.39-4.20) | 3.64 (2.57-5.14) |
| 18-34 | 5.88 (4.44-7.78) | 6.02 (4.26-8.50) |
| 35-44 | 5.65 (4.18-7.65) | 5.44 (3.79-7.8) |
| 45-54 | 4.75 (3.50-6.44) | 4.7 (3.29-6.72) |
| 55-64 | 4.05 (2.96-5.55) | 4.14 (2.90-5.90) |
| ≥65 | 1 [Reference] | 1 [Reference] |
| Male sex | 0.9 (0.81-1) | 0.82 (0.73-0.91) |
| Plan type | ||
| Comprehensive | 1 [Reference] | 1 [Reference] |
| EPO | 3.16 (1.94-5.12) | 1.14 (0.68-1.90) |
| HMO | 2.95 (2.17-4.01) | 1.1 (0.78-1.55) |
| POS | 2.43 (1.74-3.39) | 0.95 (0.65-1.37) |
| PPO | 2.63 (1.98-3.50) | 1.03 (0.75-1.43) |
| POS w/capitation | 1.39 (0.50-3.86) | 0.51 (0.18-1.44) |
| CDHP | 2.93 (2.04-4.22) | 1.1 (0.74-1.64) |
| HDHP | 2.43 (1.55-3.81) | 0.87 (0.54-1.40) |
| Region | ||
| Northeast | 0.99 (0.85-1.15) | 0.94 (0.80-1.10) |
| North central | 0.97 (0.84-1.12) | 1.03 (0.89-1.19) |
| South | 1 [Reference] | 1 [Reference] |
| West | 1.4 (1.22-1.61) | 1.30 (1.12-1.51) |
| Unknown | 0.91 (0.59-1.42) | 0.87 (0.56-1.36) |
| Urban area | 1.28 (1.08-1.52) | 1.21 (1.01-1.44) |
| Year of fracture | ||
| 2008 | 1 [Reference] | 1 [Reference] |
| 2009 | 1.07 (0.88-1.30) | 1.06 (0.87-1.29) |
| 2010 | 1 (0.82-1.21) | 0.94 (0.77-1.15) |
| 2011 | 1 (0.82-1.22) | 0.97 (0.79-1.18) |
| 2012 | 1 (0.82-1.21) | 0.95 (0.78-1.16) |
| 2013 | 1 (0.81-1.23) | 0.98 (0.79-1.21) |
| van Walraven index | 0.97 (0.96-0.98) | 1 (0.99-1.01) |
| Previous comorbidities | ||
| Tobacco use | 1.26 (0.92-1.74) | 1.02 (0.73-1.43) |
| Autoimmune or immunodeficiency disease | 1.07 (0.71-1.63) | 1.14 (0.74-1.76) |
| Anxiety | 1.61 (1.32-1.96) | 1.45 (1.18-1.78) |
| Deviated septum | 3.46 (2.90-4.12) | 2.26 (1.77-2.88) |
| Turbinate hypertrophy | 3.18 (2.45-4.13) | 1.03 (0.74-1.43) |
| Nasal obstruction | 2.64 (2.10-3.31) | 1.48 (1.14-1.93) |
| Other nasal injurya | 3.62 (2.59-5.04) | 1.50 (1.04-2.17) |
| Initial treatment | ||
| Observation | 1.05 (0.93-1.20) | 1.05 (0.92-1.19) |
| Closed | 1 [Reference] | 1 [Reference] |
| Open within 3 wk | 2.26 (1.83-2.79) | 1.13 (0.89-1.45) |
| Open between 3 wk and 6 mo | 1.83 (1.41-2.38) | 1.22 (0.93-1.60) |
Abbreviations: CDHP, consumer-driven health plan; EPO, exclusive provider organization; HDHP, high-deductible health plan; HMO, health maintenance organization; OR, odds ratio; POS, point of service; PPO, preferred provider organization.
Includes acquired and congenital deformities of the nose, late effect of fracture of skull and face, and malunion of previous fracture.
Initial treatment was not associated with subsequent septorhinoplasty in multivariable regression without interaction analyses, although open treatment within 3 weeks (OR, 2.26; 95% CI, 1.83-2.79) of fracture and between 3 weeks and 6 months (OR, 1.83; 95% CI, 1.41-2.38) after fracture was associated with greater risk of subsequent septorhinoplasty compared with closed reduction treatment in unadjusted univariable analysis. As initial treatment selection may depend on whether preexisting obstruction or defect is present, a multivariable regression model was developed with an interaction term to assess whether preexisting nasal obstruction or defect could modify the association of treatment with subsequent septorhinoplasty risk (Table 4). For patients with no preexisting nasal obstruction or defect, open treatment within 3 weeks (aOR, 1.76; 95% CI, 1.33-2.32) of fracture and between 3 weeks and 6 months (aOR, 1.52; 95% CI, 1.14-2.04) after fracture was associated with increased risk of subsequent septorhinoplasty compared with closed reduction treatment. For patients with preexisting nasal obstruction or defect, observation (aOR, 3.56; 95% CI, 2.80-4.53), closed reduction treatment (aOR, 3.10; 95% CI, 1.93-4.96), and open treatment within 3 weeks (aOR, 2.02; 95% CI, 1.48-2.77) of fracture were associated with increased risk of subsequent septorhinoplasty, with observation having the highest risk.
Table 4. Modification of the Association of Initial Treatment With Subsequent Septorhinoplasty by Diagnosis of Preexisting Nasal Obstruction or Defect.
| Initial Treatment | aOR (95% CI)a | ||
|---|---|---|---|
| No Preexisting Obstruction or Defectb | Preexisting Obstruction or Defectb | Preexisting Obstruction or Defect Within Treatment Strata | |
| Observation | 1.02 (0.89-1.17) | 3.56 (2.80-4.53) | 3.48 (2.79-4.35) |
| Closed | 1 [Reference] | 3.10 (1.93-4.96) | 3.10 (1.93-4.96) |
| Open within 3 wk | 1.76 (1.33-2.32) | 2.02 (1.48-2.77) | 1.15 (0.78-1.69) |
| Open between 3 wk and 6 mo | 1.52 (1.14-2.04) | 1.41 (0.73-2.69) | 0.92 (0.46-1.84) |
Abbreviation: aOR, adjusted odds ratio.
Odds ratios are adjusted for age, sex, plan type, region, urban area, year of fracture diagnosis, van Walraven comorbidity index, tobacco use, autoimmune or immunodeficiency disease, anxiety, and turbinate hypertrophy.
Preexisting nasal obstruction or defect defined as the diagnosis of deviated septum, nasal obstruction, acquired and congenital deformities of the nose, late effect of fracture of skull and face, and malunion of previous fracture.
Discussion
Previous studies that have assessed outcomes after management of nasal fracture may be limited by small sample size and poor generalizability. The present study represents, to our knowledge, the first population-based analysis of treatment pathways after nasal fracture and risk factors associated with septorhinoplasty after initial fracture treatment.
Most patients in the final study cohort were managed with observation alone after nasal fracture; of the patients who were treated, closed reduction treatment was more common than open treatment. The observation-only and closed reduction treatment groups had similar rates of subsequent septorhinoplasty (1.7% and 1.6%, respectively), whereas open treatment was associated with a higher rate of subsequent surgery (3.6% when treated within 3 weeks of fracture, and 2.9% when treated between 3 weeks and 6 months after fracture). Within the open treatment and closed reduction treatment groups, no statistically significant difference was observed in subsequent septorhinoplasty rates among the subgroups split by timing of treatment after fracture.
The association of initial treatment with the risk of subsequent septorhinoplasty depended on whether a preexisting diagnosis of nasal obstruction or defect was present. In patients without a preexisting diagnosis of nasal obstruction or defect, open treatment was found to increase the likelihood of subsequent septorhinoplasty, compared with observation or closed reduction treatment. Fractures involving other facial bones were excluded, but this analysis could not directly account for differences in the mean severity of nasal fractures treated by each approach. Open treatment involving limited septoplasty or osteotomy may be more common among fractures with increased severity and therefore be more strongly associated with subsequent septorhinoplasty.13 Similarly, reduced complexity cases with minimal changes in nasal bone alignment or airway patency may be managed with either observation or closed reduction treatment, resulting in lower subsequent septorhinoplasty rates.12 Therefore, it is possible that the open treatment groups had a higher mean treatment severity compared with the closed reduction treatment and observation groups and thus had greater risk of subsequent septorhinoplasty among patients without a preexisting nasal obstruction or defect.
However, among patients who had a preexisting diagnosis of nasal obstruction or defect, those treated more conservatively with observation had a greater risk of subsequent surgery than those in the open treatment groups. In addition, preexisting diagnosis of nasal obstruction or defect was found to increase the risk of subsequent septorhinoplasty for both the observation and closed reduction treatment groups. Previous studies have established that a preexisting nasal obstruction or defect may decrease the likelihood that a closed reduction treatment is successful and that open treatment may therefore be more appropriate in this setting.5,10,13,14,15,16 Our findings support the hypothesis that conservative treatment in the presence of a preexisting obstruction or defect may increase the likelihood of revision surgery in the future, compared with an open treatment approach; this conclusion warrants further prospective study. Furthermore, this association may be greater than the degree of confounding within our analysis from different mean severity among treatment groups, which may explain why initial treatment was not associated with subsequent septorhinoplasty when assessed across the entire study cohort without accounting for interaction with a preexisting nasal obstruction or defect.
Other factors independently associated with increased risk of subsequent septorhinoplasty after initial nasal fracture treatment were age younger than 65 years, female sex, urban area, western US region, and a history of anxiety, many of which agree with previously reported findings.9 Specifically, Honigman et al17 report that psychological comorbidities, including anxiety, are associated with poor psychological outcomes and patient dissatisfaction after cosmetic surgery, which may predispose patients to seek future surgical revision independent of technical outcome. With respect to the association between urban environment and septorhinoplasty after initial fracture treatment, previous studies have described an asymmetric distribution of surgeons across the United States: A disproportionately high concentration of surgeons practice in urban areas, where demand—especially for more highly reimbursed cosmetic procedures—is higher.18,19 Patients living in rural areas may, therefore, face greater travel distance and time to undergo septorhinoplasty, decreasing their access to this elective specialist care.20,21
Limitations
The limitations of this study are primarily associated with the insurance claims database used. First, the database includes only procedures that have been reimbursed by insurance; thus, procedures paid out of pocket or deemed medically unnecessary are not captured. Our analysis is, therefore, more complete for septorhinoplasty procedures that have a functional component because purely cosmetic procedures are unlikely to be reimbursed, which may underestimate the true rate of septorhinoplasty after nasal fracture. Likewise, this analysis is only valid for patients with commercial or supplemental Medicare insurance, as Medicaid and original Medicare patients are not included in this database. Second, more than 75% of patients diagnosed with nasal fracture were excluded from our analysis, nearly all of whom did not fulfill enrollment criteria. Consequently, this analysis is only valid for the population of patients with characteristics similar to those of the final study cohort. Finally, clinical or patient-reported outcomes, operative techniques, or other variables (eg, provider type, race/ethnicity, socioeconomic status) that are not explicitly or unambiguously coded for billing purposes could not be assessed, necessitating further prospective study in these areas.22
Conclusions
Clinical practice guidelines for rhinoplasty emphasize the importance of educating patients undergoing treatment for nasal injury about the risk of future follow-up surgery, which can be associated with morbidity and increased costs.23 To our knowledge, this analysis represents the first population-based study of initial treatment pathways after isolated nasal fracture, and it provides valuable information regarding the risk factors for subsequent corrective septorhinoplasty. Future prospective studies are needed to validate our results, but we believe that a preexisting diagnosis of nasal obstruction or defect as well as other aspects of a patient’s history should be considered when managing nasal fractures to assess the likelihood of surgical revision.
eTable. Billing Codes Used to Define Data Elements
References
- 1.Hung T, Chang W, Vlantis AC, Tong MCF, van Hasselt CA. Patient satisfaction after closed reduction of nasal fractures. Arch Facial Plast Surg. 2007;9(1):40-43. [DOI] [PubMed] [Google Scholar]
- 2.Mondin V, Rinaldo A, Ferlito A. Management of nasal bone fractures. Am J Otolaryngol. 2005;26(3):181-185. [DOI] [PubMed] [Google Scholar]
- 3.Hwang K, Yeom SH, Hwang SH. Complications of nasal bone fractures. J Craniofac Surg. 2017;28(3):803-805. [DOI] [PubMed] [Google Scholar]
- 4.Basheeth N, Donnelly M, David S, Munish S. Acute nasal fracture management: a prospective study and literature review. Laryngoscope. 2015;125(12):2677-2684. [DOI] [PubMed] [Google Scholar]
- 5.Reilly MJ, Davison SP. Open vs closed approach to the nasal pyramid for fracture reduction. Arch Facial Plast Surg. 2007;9(2):82-86. [DOI] [PubMed] [Google Scholar]
- 6.Kim J, Jung HJ, Shim WS. Corrective Septorhinoplasty in Acute Nasal Bone Fractures. Clin Exp Otorhinolaryngol. 2018;11(1):46-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim JH, Lee JW, Park CH. Cosmetic rhinoseptoplasty in acute nasal bone fracture. Otolaryngol Head Neck Surg. 2013;149(2):212-218. [DOI] [PubMed] [Google Scholar]
- 8.Staffel JG. Optimizing treatment of nasal fractures. Laryngoscope. 2002;112(10):1709-1719. [DOI] [PubMed] [Google Scholar]
- 9.Spataro E, Piccirillo JF, Kallogjeri D, Branham GH, Desai SC. Revision rates and risk factors of 175 842 patients undergoing septorhinoplasty. JAMA Facial Plast Surg. 2016;18(3):212-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fernandes SV. Nasal fractures: the taming of the shrewd. Laryngoscope. 2004;114(3):587-592. [DOI] [PubMed] [Google Scholar]
- 11.van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47(6):626-633. [DOI] [PubMed] [Google Scholar]
- 12.Hoffmann JF. An algorithm for the initial management of nasal trauma. Facial Plast Surg. 2015;31(3):183-193. [DOI] [PubMed] [Google Scholar]
- 13.Fedok FG, Ondik MP, Preston TW, Goldenberg D. Management of Trauma to the Nasal Bones and Septum In: Stucker FJ, de Souza C, Kenyon GS, Lian TS, Draf W, Schick B, eds. Rhinology and Facial Plastic Surgery. Berlin, Germany: Springer; 2009:793-799. [Google Scholar]
- 14.Fomon S, Schattner A, Bell JW, Kleinfeld L, Lewy R. Management of recent nasal fractures. AMA Arch Otolaryngol. 1952;55(3):321-342. [DOI] [PubMed] [Google Scholar]
- 15.Verwoerd CD. Present day treatment of nasal fractures: closed versus open reduction. Facial Plast Surg. 1992;8(4):220-223. [DOI] [PubMed] [Google Scholar]
- 16.Rohrich RJ, Adams WP Jr. Nasal fracture management: minimizing secondary nasal deformities. Plast Reconstr Surg. 2000;106(2):266-273. [DOI] [PubMed] [Google Scholar]
- 17.Honigman RJ, Phillips KA, Castle DJ. A review of psychosocial outcomes for patients seeking cosmetic surgery. Plast Reconstr Surg. 2004;113(4):1229-1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bauder AR, Sarik JR, Butler PD, et al. Geographic variation in access to plastic surgeons. Ann Plast Surg. 2016;76(2):238-243. [DOI] [PubMed] [Google Scholar]
- 19.Rosenthal MB, Zaslavsky A, Newhouse JP. The geographic distribution of physicians revisited. Health Serv Res. 2005;40(6 Pt 1):1931-1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chan L, Hart LG, Goodman DC. Geographic access to health care for rural Medicare beneficiaries. J Rural Health. 2006;22(2):140-146. [DOI] [PubMed] [Google Scholar]
- 21.Moubayed SP, Ioannidis JPA, Saltychev M, Most SP. The 10-Item Standardized Cosmesis and Health Nasal Outcomes Survey (SCHNOS) for Functional and Cosmetic Rhinoplasty. JAMA Facial Plast Surg. 2018;20(1):37-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Romo T III, Abraham MT. The ethnic nose. Facial Plast Surg. 2003;19(3):269-278. [DOI] [PubMed] [Google Scholar]
- 23.Ishii LE, Tollefson TT, Basura GJ, et al. Clinical practice guideline: improving nasal form and function after rhinoplasty. Otolaryngol Head Neck Surg. 2017;156(2_suppl):S1-S30. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Billing Codes Used to Define Data Elements