Key Points
Question
What are the indications for a thigh free flap with 2 pedicles in head and neck reconstruction?
Findings
In a retrospective case series, 57 patients received an anterolateral thigh flap with a single pedicle; 18 were reconstructed with a thigh flap with 2 pedicles; and 6 underwent multiple simultaneous thigh flaps.
Meaning
Harvesting a thigh flap with 2 pedicles has the potential to reduce complications and should be considered for divergent and extremely wide or long defects.
This case series study examines the indications and outcomes of a single-pedicle anterolateral thigh flap vs a thigh free flap with 2 pedicles in head and neck reconstruction.
Abstract
Importance
Flap choice and design are crucial to the success of free flap reconstruction of the head and neck. These are dependent on donor and recipient site characteristics.
Objective
To demonstrate indications and outcomes of a single-pedicle anterolateral thigh flap (standard ALT flap) vs a thigh free flap with 2 pedicles in head and neck reconstruction.
Design, Setting, and Participants
A retrospective case series of consecutive patients treated in a tertiary academic care center between October 2011 and June 2017 by a single reconstructive microsurgeon was carried out. Eighty-one patients underwent reconstruction of a cutaneous and/or mucosal defect of the head and neck. Patients with a composite mandibular defect who received both a fibular flap and a thigh flap were excluded. Those with less than 6 months of follow-up were excluded.
Main Outcomes and Measures
Patient characteristics and clinical variables, including age, sex, primary diagnosis/indication for reconstruction, type of flap, dimensions of flap, and number of perforators in the flap, were collected. Optimal cutoff values to quantitate the differences in length and width between the standard ALT and 2-pedicle thigh flaps were determined using receiver operating characteristic (ROC) curve analysis and the Youden Index. The types of flap were compared to determine any difference in flap complications including flap loss, venous congestion, and poor wound healing.
Results
Of the 81 patients (mean [SD] age, 58.2 [15.9] years; 62 [76.5%] men), 57 and 18 patients were reconstructed with a standard ALT flap and a thigh flap with 2 pedicles, respectively. Six patients underwent multiple simultaneous thigh (MST) flaps. Defect size (width ≥12 cm, standard ALT: 95% CI, 7.6-9.7; thigh flap with 2 pedicles: 95% CI, 7.0-17.4; P = .02; length ≥17 cm, standard ALT: 95% CI, 11.9-15.2; thigh flap with 2 pedicles: 95% CI, 13.6-30.0; P = .001), the presence of divergent mucosal defects, and through-and-through oral cavity/pharyngeal defects were associated with the use of 2 pedicles. Within groups of thigh flaps with 2 pedicles and MST flaps, there were no flap complications (ie, partial loss, venous congestion, or wound healing issues from poor perfusion).
Conclusions and Relevance
Harvesting a thigh flap with 2 pedicles has the potential to reduce flap complications and should be considered for divergent and wide or long defects. Width and length measurements respectively of 12 cm and 17 cm are reasonable numbers to initially consider when deciding whether to include a second pedicle.
Level of Evidence
3.
Introduction
The anterolateral thigh (ALT) free flap has become the most widely used fasciocutaneous free flap for head and neck reconstruction.1,2,3 The overall size of an ALT flap is dependent on the number and location of perforators.4,5 Given that the perforators of an ALT flap routinely arise sequentially from the descending branch of the circumflex artery as it descends down the thigh, it is likely that a long flap can be more reliably harvested than a wide flap.6
When the dominant perforator(s) for the flap arise from the descending branch of the lateral circumflex femoral artery (LCFA), 3 main options routinely exist for including a second pedicle (ie, supercharging and augmenting venous drainage). These additional vascular pedicles are the transverse branch of the LCFA sending a perforator through the distal fascia lata, a branch coming directly off the superficial femoral artery (SFA) sending a perforator through the rectus femoris muscle, and a branch originating from the profunda femoris artery (PFA) sending a perforator to the lateral thigh that traverses the vastus lateralis and biceps femoris.7
The purpose of this study was to demonstrate our selection criteria and outcomes of including a second pedicle for a thigh free flap (or harvesting multiple simultaneous thigh [MST] flaps) compared with an ALT flap with a single pedicle, or standard ALT flap.
Methods
We present a retrospective review of 81 consecutive patients who underwent reconstruction of head and neck cutaneous and/or mucosal defects with a thigh free flap between October 2011 and June 2017 at the University of Colorado Hospital by a single reconstructive microsurgeon (FWBD). Patients with a composite mandibular defect who underwent reconstruction with both a fibular free flap and an ALT free flap were excluded (n = 5). Patient characteristics and clinical variables, including age, sex, primary diagnosis/indication for reconstruction, type of flap (ie, standard ALT flap vs thigh flap with 2 pedicles vs MST flaps), dimensions of flap, and number of perforators in the flap, were collected. Type of free flap was compared to determine any difference in flap complications, in particular, flap loss, venous congestion, or wound healing that could be attributed to poor (ie, marginal) perfusion at the most distal portions of the flap. Approval was obtained from the institutional review board at the University of Colorado.
Defects were classified as (1) cutaneous only, (2) limited to the oral cavity and/or oropharynx, or (3) through-and-through defects (mucosa and skin). The length, width, and area of the cutaneous defects were compared with Student’s t test for patients with standard ALT and thigh flap with 2 pedicles only (given no patient with MST flaps had a cutaneous-only defect), using GraphPad Prism (version 7.0a; GraphPad Software, Inc). Optimal cutoff values to quantitate the differences in length and width between the standard ALT and thigh flap with 2 pedicles were determined using receiver operating characteristic (ROC) curve analysis and the Youden Index.8 The ROC curve plots sensitivity vs 1-specificity and assists, for example, in evaluating a test’s diagnostic ability, or as in this review, optimal cutoff values. It has wide clinical applicability in epidemiology to assess laboratory biomarkers and imaging tests. The method of determining a cutoff value, the Youden Index, was achieved by maximizing sensitivity and specificity across various cutoff points. P < .05 was considered statistically significant.
Results
Fifty-seven (70%) patients underwent a standard ALT free flap. Eighteen (22%) patients underwent a thigh flap with 2 pedicles. Six (8%) patients underwent MST flaps. The most common indication for reconstruction was malignant abnormality (70 [86%]), followed by infection (4 [5%]) and trauma/burn (7 [9%]).
The Table shows patients categorized by type of flap and by defect characterization. Of 35 patients with cutaneous-only defects, 29 underwent a standard ALT flap with mean defect size of 120.9 cm2 (95% CI, 96.5-145.2). In contrast, the 6 patients who underwent a thigh flap with 2 pedicles had mean defect of 265.2 cm2 (95% CI, 111.0-419.4; P < .001). The mean width between the 2 groups differed by 3.6 cm (standard ALT: 95% CI, 7.6-9.7; thigh flap with 2 pedicles: 95% CI, 7.0-17.4; P = .02) whereas mean length differed by 8.2 cm (standard ALT: 95% CI, 11.9-15.2; thigh flap with 2 pedicles: 95% CI, 13.6-30.0; P = .001). Optimal cutoff values based on ROC curve analysis and the Youden Index yielded values of 12 cm and 17 cm for width and length, respectively.
Table. Head and Neck Defect Characteristics.
| Characteristic | Standard ALT Flap (n = 57) |
Thigh Flap With 2 Pedicles (n = 18) |
MST Flaps (n = 6)a |
P Valueb |
|---|---|---|---|---|
| Cutaneous only | 29 | 6 | NA | NA |
| Defect size, No. (SD), cm2 | 120.9 (64.0) | 265.2 (146.9) | NA | <.001 |
| Mean width, No. (SD), cm | 8.6 (2.8) | 12.2 (5.0) | NA | .02 |
| Mean length, No. (SD), cm | 13.6 (4.4) | 21.8 (7.8) | NA | .001 |
| Perforators captured, mean | 1.7 | 2.8 | NA | NA |
| Limited to oral cavity and/or oropharynx, No. | 23 | 7 | NA | NA |
| Divergent mucosal defect, No. (%) | 0 | 5 (100) | NA | NA |
| Perforators captured, No. | 1.5 | 2.9 | NA | NA |
| Through-and-through (mucosa and skin), No. | 5 | 5 | 6 | NA |
| Oral cavity with skin, No. (%) | 3 (27) | 3 (27) | 5 (45) | NA |
| Perforators, mean | 1.0 | 3.0 | NA | NA |
| Total pharyngectomy with cervical skin, No. (%) | 2 (40) | 2 (40) | 1 (20) | NA |
| Perforators, mean | 2.5 | 2.0 | NA | NA |
Abbreviations: ALT, anterolateral thigh; MST, multiple simultaneous thigh; NA, not applicable.
No patient with a cutaneous-only defect nor defect limited to the oral cavity/oropharynx underwent MST.
The P values are comparing the defect size, mean width, and mean length between the group of patients who underwent a standard ALT flap versus a thigh flap with 2 pedicles.
Most of the patients (23 of 30, 77%) with defects limited to the oral cavity and/or oropharynx were reconstructed with a standard ALT (Table). No patient who received a standard ALT had a defect involving divergent mucosa. The mean number of perforators captured was 1.5. Of the 7 patients who underwent a thigh flap with 2 pedicles, 5 had divergent mucosal defects. A divergent mucosal defect was defined as having 2 noncontiguous areas requiring flap coverage that would necessitate the flap to be partially divided to reconstruct both areas. All divergent defects included a total glossectomy with bilateral exposed tonsillar fossae. An average of 2.9 perforators were captured in these 2-pedicle flaps. Of the 2 patients without a divergent defect, 1 received a 2-pedicle thigh flap owing to aberrant vascular anatomy. This patient had only 1 small distal perforator and the diameter of the descending branch of the LCFA was less than 1 mm at its origin. Therefore, to augment perfusion a second pedicle was harvested, arising posteriorly from the profunda system and contributing a perforator to the lateral thigh. The other patient without a divergent defect underwent a total pharyngectomy with near-total glossectomy. Given the extent of the defect, 2 pedicles were designed—1 perfusing the skin paddle for reconstruction of the tongue and the second perfusing skin forming the neopharynx.
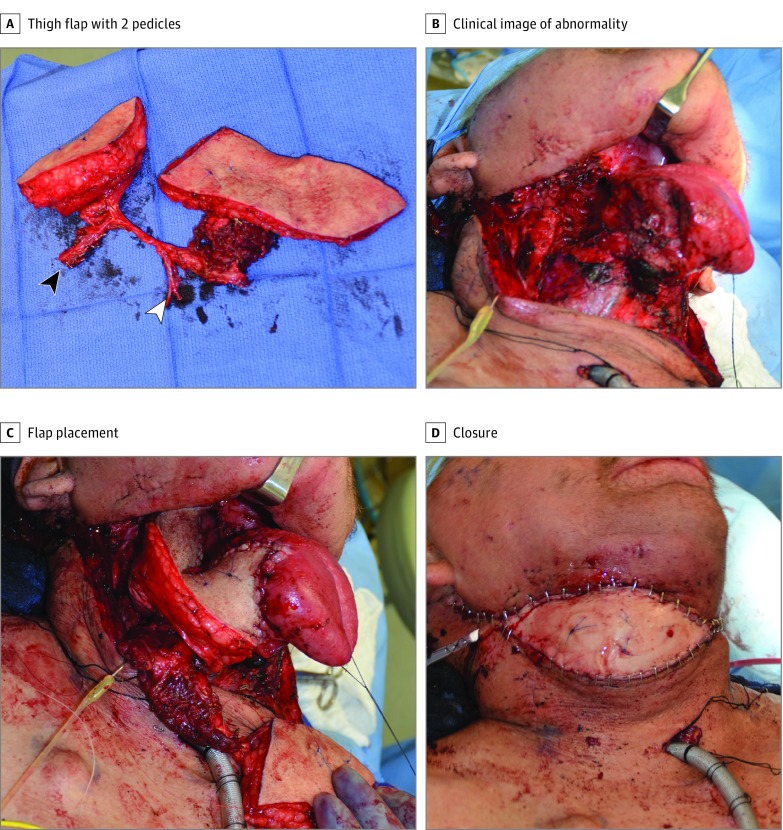
Sixteen patients had through-and-through defects of the oral cavity or pharyngeal mucosa and skin (Table). Five were reconstructed with a standard ALT flap and 5 had a thigh flap with 2 pedicles (Figure 1). In each group, 3 patients had a defect involving the oral cavity with resection of facial or cervical skin whereas 2 had a total pharyngectomy with resection of cervical skin. In patients with MST flaps, 5 had a defect involving the oral cavity with resection of facial or cervical skin whereas 1 patient had a total pharyngectomy with resection of cervical skin.
Figure 1. Reconstruction With a Thigh Flap With 2 Pedicles in a Patient With Recurrent Tonsillar Fossa Carcinoma.
A, Design of a thigh flap with 2 pedicles with the skin bridge divided for reconstruction of oral cavity defect and cervical skin. One pedicle arises from the transverse branch of the LCFA (black arrowhead); 1 from the descending branch of the LCFA (white arrowhead). There is an intervening branch connecting the 2 pedicles. B, Defect following resection of base of tongue, lateral pharyngectomy, and cervical skin resection. C, Flap inset at base of tongue and lateral pharynx. Second skin island for cervical skin reconstruction pictured at bottom right of panel. D, Flap inset and closure of cervical skin defect.
In patients with a standard ALT flap, the pedicle source was the descending branch of the LCFA in 48 of 57 (84%), compared with the transverse branch in 9 of 57 (16%). In patients with a thigh flap with 2 pedicles, the primary pedicle was from the descending and transverse branch of the LCFA in 13 of 18 (72%) and 5 of 18 (28%) patients, respectively. The source of the additional pedicle was the transverse branch of the LCFA in 10 of 18 (56%) patients, the SFA in 6 of 18 (33%) patients, the ascending branch of the LCFA in 1 of 18 (6%), and a posterior branch from the PFA in 1 of 18 (6%). All 6 patients who had MST flaps had at least 1 flap where the primary pedicle was from the descending branch of the LCFA.
Six patients in the series experienced flap complications. Of patients with a cutaneous-only defect who underwent a standard ALT flap, 1 had flap failure; 2 had issues with wound healing at the inset site; and 1 developed acute venous congestion.
The flap loss occurred in a woman in her 20s with osteomyelitis of the skull following trauma and scalp loss. Intraoperatively, acute coagulopathy of the arterial system was noted as early as harvest of the flap, as well as during and after anastomosis. Multiple maneuvers throughout treatment were attempted to restore flap perfusion, but were unsuccessful. She was found on hematologic work-up to have factor V Leiden thrombophilia, with multiple deep vein thromboses in the upper extremities during her hospitalization, in addition to the flap loss. She was treated with 2 scalp flaps and split-thickness skin grafting.
Two patients with cutaneous defects reconstructed with a standard ALT flap experienced wound healing issues at the inset site. A man in his 70s with a medical history of chronic lymphocytic leukemia and recurrent periorbital carcinoma experienced partial flap dehiscence following orbital exenteration and forehead skin resection. This was attributed to recurrent disease and extensive radiation history. The second patient, a man in his 60s with occipital basal cell carcinoma developed an infection deep to the flap requiring incision and drainage. This gentleman had poorly controlled insulin-dependent diabetes and was an active smoker. The flap went on to heal well with local wound care.
One patient with a standard ALT flap, measuring 15 cm by 10 cm, developed acute congestion of the flap within 12 hours (Figure 2). The patient was brought emergently back to the operating room. The 2 venous anastomoses that had been performed with a 2-mm coupler and a 3-mm coupler were without obstruction, and the patient was brought back to the intensive care unit without any further intervention. The congestion cleared within 48 hours.
Figure 2. Acute Venous Congestion in a Standard Anterolateral Thigh Flap.
A, Venous congestion of a 15-cm by 10-cm standard ALT flap in a man with recurrent squamous cell carcinoma. B, Resolution of venous congestion, Image taken 5 days postoperatively.
No patient with a cutaneous-only defect reconstructed with a 2-pedicle thigh flap experienced flap loss or wound-healing issues. Among patients with defects limited to the oral cavity and/or oropharynx, 1 patient with a standard ALT flap had a deep neck infection requiring neck exploration and drainage, and 1 patient with a thigh flap with 2 pedicles developed an oral-cutaneous fistula. The patient with standard ALT flap was a woman in her 60s with recurrent oral cancer previously treated with radiation therapy who underwent a lateral pharyngectomy and near-total tongue resection.
At the time of neck exploration and drainage there was no evidence of a fistula, and she was treated successfully with antibiotics. The patient with the 2-pedicle thigh flap was a woman in her 60s with recurrent squamous cell carcinoma who underwent a total glossectomy and bilateral lateral pharyngectomies with exposure of the carotid arteries in the tonsillar fossae. Her medical history of extreme radiation therapy and poor dentition likely contributed to dehiscence at the suture line along a partially necrotic mandible. At reoperation, she was found to have a tract from the anterior floor of the mouth to the midline neck. Repair was accomplished with extraction of carious teeth, marginal mandibulectomy, and flap advancement.
No patient with a through-and-through defect of any flap type experienced any postoperative complications.
The mean (SD) operative time in minutes for a standard ALT flap, 2-pedicle thigh flap, and MST flaps were 600.8 (118.0) (95% CI, 569.2-632.4), 815.0 (97.8) (95% CI, 764.7-865.3), and 982.3 (83.4) (95% CI, 894.8-1070.0), respectively (P < .001).
Of the standard ALT patients, 47 of 57 (82%) had their donor site in the leg closed primarily, compared with 14 of 18 (78%) double-pedicle ALT flap patients, and 4 of 6 (67%) MST flaps patients.
Discussion
The results of this study suggest that harvesting a thigh flap with 2 pedicles has the potential to reduce flap complications and should be considered for divergent and wide or long defects. Based on ROC curve analysis and the Youden Index, the optimal cutoff values for width and length were respectively 12 cm and 17 cm. Although ALT flaps larger than 12 cm by 17 cm have been harvested without flap loss, our practice has been to incorporate a second pedicle to improve perfusion. These values help quantify our decision making and are reasonable starting points to consider in addition to factors like number, quality, and location of perforators.
With these data, we suggest guidelines for determining flap choice and pedicle design based on defect classification and size.
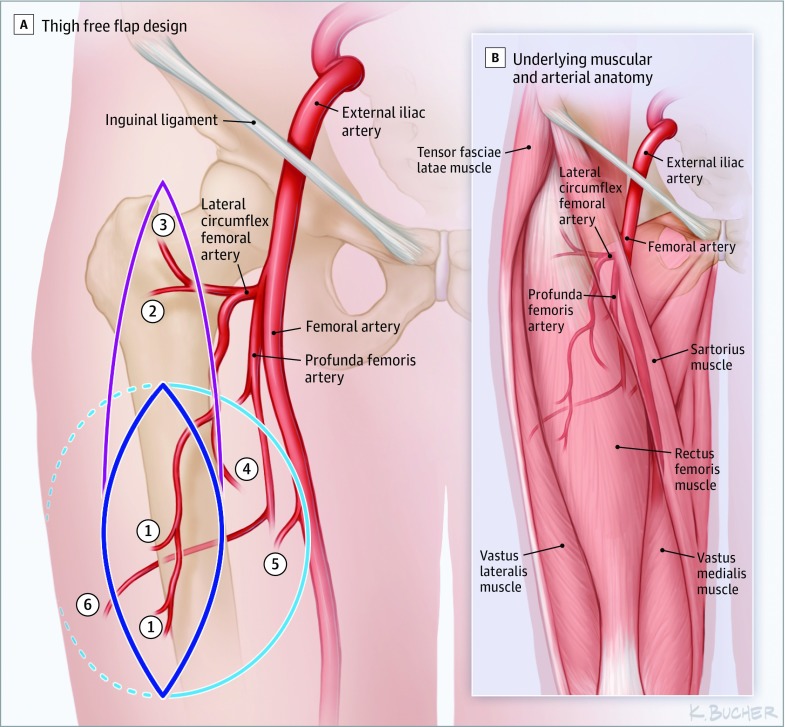
Defects with a narrow width (<12 cm) and a short length (<17 cm) can routinely be reconstructed with a standard ALT flap based on the descending branch of the LCFA (Figure 3).9 If the transverse branch of the LCFA provides the dominant perforator to the lateral thigh, this pedicle should be considered.2 This occurred in 16% of these cases. For very wide flaps (>12 cm) with a length shorter than 17 cm, one should consider including a second pedicle providing medial or lateral perforators. This second pedicle will likely originate medially, directly off the SFA sending a perforator through the rectus femoris or laterally originate from the PFA sending a perforator to the lateral thigh that traverses the vastus lateralis and biceps femoris. On the other hand, defects that are very long (length >17 cm), but narrow (width <12 cm) may require a supercharged/venous-augmented flap with a second pedicle based on the transverse or ascending branch of the LCFA to account for the longer length. This may be particularly useful in a thigh flap that has only a single perforator. The ALT flaps that are both extremely wide and long may benefit from being supercharged with whatever second pedicle seems available. Often a separate pedicle from the transverse branch of the circumflex artery or from medial thigh (ie, SFA) can easily be harvested.
Figure 3. Thigh Free Flap Design.
Labeled pedicles are the same for main figure and inset. A, possible skin islands; the inset shows underlying musculature and vascular anatomy. The solid dark-blue line indicates a standard ALT flap based off perforator from 1, descending branch of LCFA. The solid purple line indicates an extremely long flap (greater than 17-cm length) based on additional perforator from 2, transverse branch of LCFA or 3, ascending branch of LCFA. The solid light-blue line indicates an extremely wide flap (greater than 12-cm width) based on additional perforator from 4, rectus femoris branch of the descending branch of LCFA or 5, superficial femoral artery. Dashed light-blue line indicates extremely wide flap (greater than 12-cm width) based on additional perforator from 6, profunda femoris. B, Underlying muscular and arterial anatomy.
In the group of patients with cutaneous-only defects, 1 patient developed wound dehiscence around the margins of the flap. This failure of healing at the inset site was attributed to poor healing caused by radiation to the skin surrounding the defect. One advantage of a 2-pedicle thigh flap is undoubtedly the larger size that can be harvested because additional perforators are included. In cutaneous defects where the surrounding remaining skin has been radiated, we now routinely resect this skin to reach margins outside the radiation fields. Having the option of including a second pedicle with a thigh flap can enable successful reconstruction of these much larger defects.
One patient with a standard ALT flap developed acute venous congestion (Figure 2). The congestion was attributed to insufficient outflow even though both venous anastomoses (to the paired venae comitantes) were found to be flowing at time of exploration. Both veins were without torsion. An operative intervention was necessary to make this diagnosis, and the flap likely suffered some fat necrosis. Of note, this ALT flap had only 1 perforator and was relatively thick (approximately 25 mm). Though this is a single case, it does underscore the value of including multiple outflow channels (ie, multiple perforators served by a single pedicle or 2 pedicles) when harvesting relatively large (and thick) flaps.6,10,11
For patients with defects limited to the oral cavity/oropharynx, decision making is based on whether the defect involves divergent mucosa. If there is not a divergent mucosal defect, a standard ALT flap with a single-pedicle is appropriate. If a thicker flap is necessary (ie, for a total glossectomy rather than a partial anterior glossectomy), greater volume can be provided by designing a flap based on a more proximal perforator. On the other hand, if the defect contains areas of divergent mucosa, a 2-pedicle thigh flap based on both the descending and the transverse branch of the LCFA is an effective approach. For example, in patients with defects that include a total glossectomy with bilateral carotid exposure in the tonsillar fossae, any problems with wound or flap healing could leave the carotid arteries exposed with catastrophic results. If a standard ALT flap was partially divided to allow the flap to wrap around the pharynx and to be extended anteriorly for tongue reconstruction, division of the flap could be associated with poorer perfusion in the rotated limb. By placing a perforator in both limbs (either by including a second pedicle or by dividing the flap between 2 perforators from the same pedicle), perfusion is improved. Using this approach, there were no complications of wound breakdown in our series.
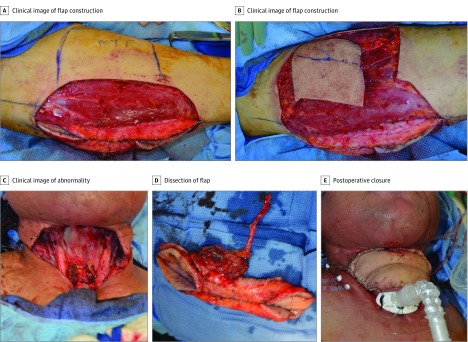
Reconstruction of through-and-through defects (ie, oral cavity with submental or facial skin; total pharyngectomy with cervical skin) is dependent on whether a separate perforator from the main pedicle can be placed in the cutaneous paddle. If so, deepithelialization between the 2 perforators allows the flap to be turned over for cervical or facial skin replacement. If a separate perforator from the main pedicle cannot be placed in the cutaneous paddle, we designed the flap with the goal of harvesting a second pedicle with a perforator in each paddle. Of note, ALT flaps can be successfully deepithelialized to create 2 skin paddles without necessarily incorporating a perforator into each paddle. However, a strategy to include a perforator in each paddle will likely lead to more reliable perfusion. If none of these strategies can be employed, MST flaps are the next option In our series, indications for MST flaps were noncontinguous, simultaneous skin defects (ie, 2 different sites on the head and neck) and noncontinguous, skin and mucosal defects where a single flap or supercharged flap could not be turned over, rotated, or just partially divided to reconstruct both defects (Figure 4).
Figure 4. Reconstruction Following Total Pharyngectomy and Cervical Skin Resection in a Man in His 40s.
A, Design of multiple simultaneous thigh free flaps. Top (A and B) shows design for medial thigh flap for coverage of cervical skin defect. Bottom shows lateral thigh flap tubed in situ for pharyngeal reconstruction. B, Harvest of medial thigh flap. C, Defect following cervical skin resection and total pharyngectomy. D, Dissection of lateral thigh flap, tubed for pharyngeal reconstruction. E, Medial thigh flap inset and closure of cervical defect.
Mean (SD) operative times in minutes were longer for 2-pedicle flaps (815.0 [97.8]; 95% CI, 764.7-865.3) compared with standard ALT flaps (600.8 [118.0]; 95% CI, 569.2-632.4) (P < .001). This increase in time was mainly attributed to the longer times for extirpation because in general these tumors were more extensive. All flaps were routinely raised and ready for inset prior to the completion of the tumor resection and neck dissections. Closure of the donor site defect, either primarily or with skin grafting, was done at the same time as flap inset.
Limitations
This study has a number of limitations. Because it was not a randomized clinical trial we were unable to know definitively whether complications and partial flap loss would have occurred with only a single pedicle. The inclusion of a second pedicle was done to improve perfusion, especially in those defects most challenging (ie, divergent mucosal, through-and-through, and extremely large defects). Such a strategy seems worthwhile, especially because even a partial flap loss in the oral cavity or oropharynx can lead to devastating complications in the head and neck. The ROC analysis performed to estimate cutoff values for width and length is only 1 method for performing such calculations; however, given its broad clinical uses, we felt that it was the most appropriate for our study. These width and length cutoffs will obviously be affected by the size of the perforators and the number and positions of the perforators relative to each other and the edges of the skin paddle. However, we believe that these are reasonable numbers to initially consider when deciding whether to include a second pedicle.
Conclusions
Harvesting a thigh flap with 2 pedicles has the potential to reduce flap complications and should be considered for divergent and extremely wide or long defects. The proposed design options of this review will help guide flap choice when designing a thigh free flap for a cutaneous and/or mucosal defect of the head and neck.
References
- 1.Song YG, Chen GZ, Song YL. The free thigh flap: a new free flap concept based on the septocutaneous artery. Br J Plast Surg. 1984;37(2):149-159. [DOI] [PubMed] [Google Scholar]
- 2.Xu Z, Zhao XP, Yan TL, et al. A 10-year retrospective study of free anterolateral thigh flap application in 872 head and neck tumour cases. Int J Oral Maxillofac Surg. 2015;44(9):1088-1094. [DOI] [PubMed] [Google Scholar]
- 3.Wei FC, Jain V, Celik N, Chen HC, Chuang DCC, Lin CH. Have we found an ideal soft-tissue flap? An experience with 672 anterolateral thigh flaps. Plast Reconstr Surg. 2002;109(7):2219-2226. [DOI] [PubMed] [Google Scholar]
- 4.Landuyt KV. The anterolateral thigh flap for lower extremity reconstruction. Semin Plast Surg. 2006;2(20):127-132. [Google Scholar]
- 5.Mosahebi A, Disa JJ, Pusic AL, Cordeiro PG, Mehrara BJ. The use of the extended anterolateral thigh flap for reconstruction of massive oncologic defects. Plast Reconstr Surg. 2008;122(2):492-496. [DOI] [PubMed] [Google Scholar]
- 6.Sokoya M, Deleyiannis FW. A triple pedicle, near-total thigh flap supercharged with the flow-through technique. Eplasty. 2016;16:e4. [PMC free article] [PubMed] [Google Scholar]
- 7.Deleyiannis FW, Badeau AM, Leem TH, Song JI. Supercharging and augmenting venous drainage of an anterolateral thigh free flap: options and indications. Plast Reconstr Surg Glob Open. 2014;2(4):e135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hajian-Tilaki K. Receiver operating characteristic (ROC) curve analysis for medical diagnostic test evaluation. Caspian J Intern Med. 2013;4(2):627-635. [PMC free article] [PubMed] [Google Scholar]
- 9.Di Candia M, Lie K, Kumiponjera D, Simcock J, Cormack GC, Malata CM. Versatility of the anterolateral thigh free flap: the four seasons flap. Eplasty. 2012;12:e21. [PMC free article] [PubMed] [Google Scholar]
- 10.Jiang C, Guo F, Li N, et al. Multipaddled anterolateral thigh chimeric flap for reconstruction of complex defects in head and neck. PLoS One. 2014;9(9):e106326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Numajiri T, Morita D, Tsujiko S, et al. Dual vascular free anterolateral thigh flap. Plast Reconstr Surg Glob Open. 2017;5(8):e1448. [DOI] [PMC free article] [PubMed] [Google Scholar]