Abstract
Background
We sought to study gender differences and differences over time with respect to demographics, relation to recipient, donor motives, and experiences of live kidney donation.
Material/Methods
In all, 455 consecutive live kidney donors, representing all of the donors at our center between 1974 and 2008 were considered for this study. There were 28 deceased donors and 14 donors who had moved abroad, leaving 413 donors; 387 (94%) agreed to participate in this study. A questionnaire was sent and the answers was analyzed for gender differences and, where relevant, for changes over time.
Results
In all sub-periods, female donors made up the majority (55–62%), except for sibling donors (45%) and child-to-parent donors (40%). No significant gender differences were seen in perceived information given before donation. For males, it was more common that the recipient took the initiative to donate. For females, the motivation for donating was more frequently to help the recipient and because others wanted them to donate. For males, it was more common to feel a moral obligation. Post-operatively, females more frequently felt sad and experienced nausea, and more frequently felt that the donation had a positive impact on their lifes. With the introduction of minimally invasive surgical techniques, donors experienced fewer problems from the operation, with no gender difference.
Conclusions
Females donate more frequently than males, a difference that did not change over time. Only a few gender differences were seen in donor motives and the donation experience; however, these differences may be relevant to address the gender imbalance in kidney donations.
MeSH Keywords: Attitude, Follow-Up Studies, Kidney Transplantation, Living Donors
Background
Transplantation of kidneys from live donors has been increasing but in recent years the rate has in some countries stagnated or declined [1,2]. Live donation constitutes an important source of donor kidneys since it increases the donor pool and reduces organ shortage. It has, in addition, been shown to provide better results in terms of both patient and organ survival independent of the donor’s relation to the recipient [3]. Many observations have consistently reported that live kidney donors are predominately female and more males are kidney transplant recipients. The higher incidence of end-stage-renal disease (ESRD) in men and the marginally higher proportion of women in the population have been suggested to explain this gender difference [4,5]. There are, however, many other possible explanations for this imbalance, such as: women being more altruistic, less able to resist pressure, and having less cardiovascular disease than men. Socioeconomic reasons, including the health and welfare environment, may also play a role [5,6]. In Iran, the only country with government-regulated kidney donation, 85% of unrelated live kidney donors are men, indicating that other factors may also be important, such as cultural or religious factors [7].
Female kidneys are in general smaller and have fewer nephrons than those of men [8], and studies have shown inferior graft function in female to male transplantation [4]. This effect of donor gender is due not only to relative nephron under dosing, but may also be related to hormonal and immunological differences between the sexes [6,9]. From both an ethical and socioeconomic perspective, and a medical standpoint, a more equal gender distribution is desired.
In the selection of live kidney donors, it is important to maintain transparent protocols and procedures to minimize the risk of selection based on discriminatory factors such as gender. We have previously reported the results from physical examination of this same cohort, which showed well-preserved long-term kidney function in both male and female donors. At follow-up, the mean MDRD was 69±13 and 65±12 mL/min/1.73 m2 for male and female donors, respectively. The gender difference was significant (p<0.01). No case of ESRD was identified in the follow-up cohort and the lowest reported eGFR was 31 mL/min/1.73 m2 at 25 years after donation [10]. To further address the gender imbalance in live kidney donation, in this study we analyzed gender differences in attitudes, motives, experiences, and follow-up after live kidney donation. Over the time of the study period, knowledge of the long-term effects of kidney donation, the informed consent process, and the surgical techniques have changed. We therefore also set out to study whether there were any changes in the aspects studied over time.
Material and Methods
Study population
At the University Hospital in Uppsala, Sweden, the first live kidney donation was performed in 1974. From that time to the end of our study period, September 2008, a total of 455 live kidney donations were performed. Using donor social security numbers, we could identify all donors, and their current addresses were retrieved from the Swedish population registry. A total of 28 donors were deceased and 14 donors had moved abroad, leaving 413 individuals available to participate in the study. These individuals were sent a survey questionnaire by mail and, if it was not returned, one reminder followed, also by mail. If still not returned, we tried to reach the individuals by phone, retrieving their numbers from online directories. Of the 413 live kidney donors living in Sweden, 387 returned the questionnaire, giving a response rate of 94%.
Methods
The questionnaire contained questions relating to general background information and then three blocks of questions relating to 1) the period before donation, 2) the perioperative period, and 3) the long-term impact of donation. The first of these addressed the donor’s relation to the recipient, motives for donating a kidney, who took the initiative, and information received about the operation and the short- and long-term risks. The second block of questions dealt with the perioperative course and early recuperation. The last set of questions related to the long-term physical effects of the operation, the donor’s relation to the recipient, and overall outcomes. Most survey questions were answered by checking a box, others were answered on continuous visual analogue scales (one with endpoints “unimportant” and “important”, and another with endpoints “not true at all” and ‘entirely true”). For some questions, space was also provided for the respondents to add more detailed written answers, but these responses have not been included in this analysis.
The Regional Ethics Committee in Gothenburg approved the study and participants gave written informed consent.
Statistical methods
The data are presented as mean values (SD) or percentages. Analyses were carried out using Statistical Package for the Social Sciences software (SPSS, version 23). Differences between groups were calculated using the chi-square test and differences between mean values using the Student’s t-test. A p value < 0.05 was considered statistically significant.
Results
Demographic data
The mean age of donors at donation was 49±10 years (range 21–73 years), and 60±11 years (range 24–97 years) at follow-up. The mean time since donation was 11±7 years (range 1–33 years). In total, there were significantly more female donors (262/193 (F/M), 59%, p≤0.001). This imbalance remained stable over time, ranging from 52–65% (Figure 1). Regarding the donor-recipient relation, females made up the majority in partner (69%), parental (69%), anonymous (67%), other relative (65%) and friend (58%) donations, but not in sibling (45%) or child-to-parent donations (40%).
Figure 1.
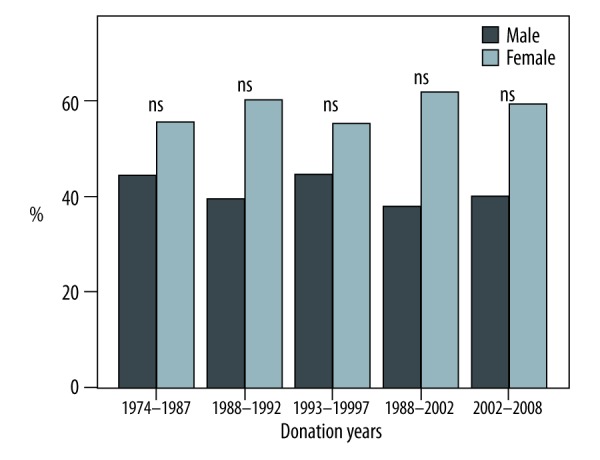
In all sub-periods, female donors (light bars) were more predominant than male donors (dark bars). In total, there were significantly more female donors (262/193 (F/M), 59%, p≤0.001). This imbalance remained stable over time, ranging from 52–65%.
Donation initiative
For both males (69%) and females (77%), it was the donor himself or herself who took the initiative to donate a kidney. The second most frequent initiative-taker for females was the physician (11%), whereas for males it was the recipient (13%), which was significantly more frequent than recipient-initiated donations for female donors (p < 0.04). For both male and female donors, the initiative came from the family in 4% of cases (Figure 2).
Figure 2.
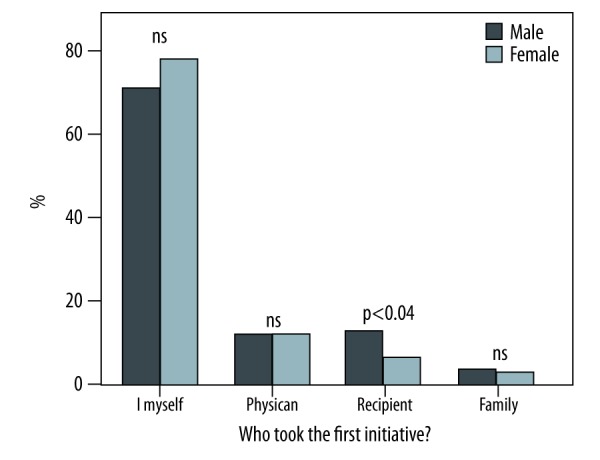
Breakdown of who took the initiative to donate for male (dark bars) and female (light bars) donors. In both males (69%) and females (77%), most of the donors themselves took the initiative to donate a kidney (ns).
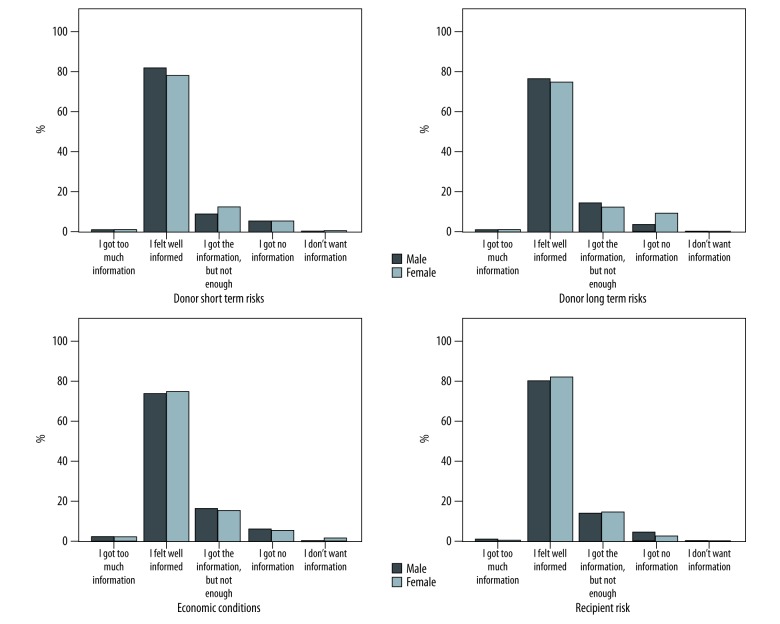
Pre-donation information
Questions relating to information given before donation regarding economic factors, short- and long-term risks for the donor, as well as risks to the recipient, are shown in Figure 3. The responses of males and females were similar for these questions, with a small number of donors stating they had received too much information (1.1% and 2.4%, respectively), the majority felt that they had been well-informed (74.4% and 80.5%, respectively), a small minority felt that they had not received enough information (11.6% and 15.8%, respectively), and others stated that they had received no information (3.6 and 7.7%, respectively), or had not wanted information (0.5–1.8%) (Figure 3). These perceptions of the information received did not change over time.
Figure 3.
Male (dark bars) and female (light bars) donor responses regarding information received about short- and long-term risks of kidney donation, economic factors, and risks to the recipient. No significant gender differences.
Pre-donation motive
Answers to the question “What was the main reason that you donated a kidney?” showed no major differences between male or female donors (Table 1). However, females were significantly more motivated by wanting to help a kidney patient (p≤0.01) and by others wanting them to donate (p≤0.02), whereas men were significantly more motivated by a moral obligation to donate (p≤0.03).
Table 1.
Answers to the Question: “What was the main reason that you donated a kidney?” Using a Visual Analogue Scale, where 0=“unimportant” and 100=“important”.
| Total | Male | Female | p | |
|---|---|---|---|---|
| I wanted to help the kidney patient | 90±6 | 90±6 | 92±6 | 0.008 |
| My religious beliefs say that it was the right thing to do | 16±25 | 15±23 | 17±26 | ns |
| I knew that you could donate a kidney and live a normal life | 82±28 | 80±37 | 83±20 | ns |
| Others wanted me to donate | 13±18 | 15±21 | 11±15 | 0.020 |
| I wanted to improve my relationship with the kidney patient | 16±22 | 18±23 | 15±22 | ns |
| I wanted to feel like a better person | 15±19 | 16±19 | 14±18 | ns |
| The waiting time from a deceased donor was too long | 55±36 | 51±36 | 58±37 | ns |
| I was worried about how it would go without a transplant | 87±15 | 85±16 | 88±14 | ns |
| I felt a moral obligation to donate a kidney | 38±35 | 42±35 | 34±35 | 0.028 |
| I wanted others to see me as a better person | 10±11 | 11±13 | 9±9 | ns |
| It could just as easily have been me who was sick | 60±36 | 56±35 | 62±36 | ns |
| I saw no other option than to donate a kidney | 55±36 | 52±35 | 56±37 | ns |
| My quality of life would be improved | 49±38 | 44±37 | 52±38 | ns |
| The entire family’s quality of life would be improved | 67±32 | 65±32 | 69±32 | ns |
Post-donation attitudes and experiences
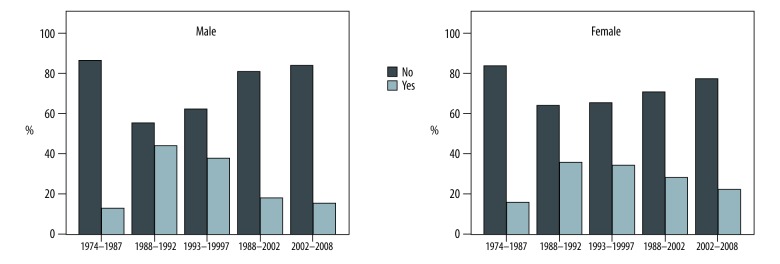
In post-operative week 1, significantly more females experienced nausea/vomiting and more felt sadness (p≤0.0001 and p≤0.006, respectively). Apart from these two areas, there was no gender differences (Table 2). For the later post-operative period, there was no difference between the genders regarding how long it took to recuperate and both male and female donors showed a similar trend toward fewer continuing problems (Figure 4). There was a significant reduction in discomfort from the operation/scar after 1998 when minimally invasive surgical techniques were introduced at the institution (p≤0.009).
Table 2.
Answers to the question: “How did you experience the first week after donation?” Using a Visual Analogue Scale, where 0=“Not true at all” and 100=“entirely true”.
| Total | Male | Female | p | |
|---|---|---|---|---|
| I had a lot of pain | 58±31 | 59±30 | 57±32 | ns |
| I felt nauseous and vomited | 39±34 | 29±29 | 47±34 | <0.0001 |
| I felt good | 53±31 | 53±31 | 52±31 | ns |
| I was constipated | 38±32 | 35±31 | 40±32 | ns |
| I felt refreshed | 49±30 | 50±29 | 48±30 | ns |
| I was very tired | 54±30 | 51±31 | 56±30 | ns |
| I felt sadness | 26±24 | 22±21 | 28±26 | 0.006 |
| I felt happy and lucky | 68±26 | 67±26 | 69±26 | ns |
| I don’t remember | 21±21 | 18±17 | 23±24 | ns |
Figure 4.
Both male and female donors showed a similar trend toward fewer continuing problems, with no major gender differences. Donor responses (dark bars – “No” and light bars – “Yes”) to the question about whether they had continuing problems after donation, by sub-period.
From an overall perspective, the vast majority felt the donation had had a positive influence on their lives, and this was significantly more frequent among females (70% versus 56%, p≤0.02). A small minority felt that it had had a negative impact, a feeling that was significantly more frequent in males (3% versus 1%, p≤0.02). No difference was observed between the genders in how the relationship to the recipient had developed and no change over time. To the question about donating again (“If it were possible, would you donate again?”), 82% answered “Yes”, 6% “No”, and 11% “Maybe” or “Don’t know”. Regarding regrets (“Do you regret that you were donor?”), 97% stated they did not regret having been a donor. There were no significant differences between the genders for either of these questions.
Follow-up
A majority of the donors had regular check-ups, with no difference between the genders (females 83% and males 81%) (Figure 5).
Figure 5.
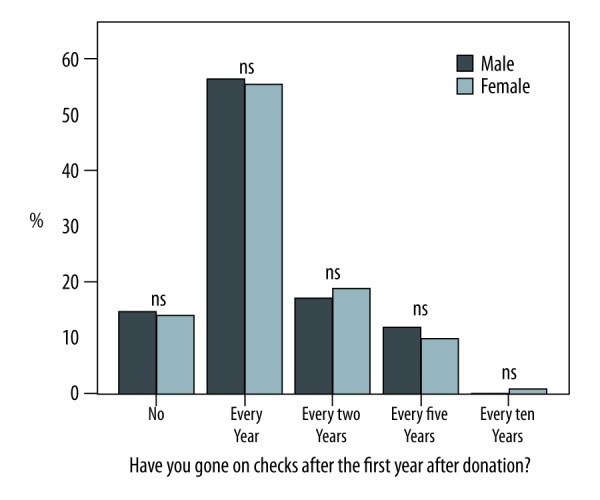
Breakdown of frequency of check-ups for male (dark bars) and female (light bars) donors. A majority of the donors had regular check-ups, with no difference between the genders (females 83% and males 81%).
Discussion
At our center, women make up in the majority of live kidney donors, which is consistent with most studies in other countries. This imbalance was not seen in all subgroups, however, the exceptions being sibling-to-sibling and child-to-parent donations. There are many possible explanations for why fewer men than women become live kidney donors, and the reasons are likely a combination of medical, psychological, and economic factors. Some studies have shown that men are more reluctant to register as donors, and others have shown that it is more common for men to have cardiovascular barriers to donation, such as hypertension, which excludes them from being donors [11]. It has been reported that the introduction of laparoscopic nephrectomy, with shorter hospitalizations, less post-operative pain, less sick leave, and smaller scars was associated with a decrease in the gender difference in kidney donation |12]. This current study shows that the female predominance in live kidney donation did not decrease after the introduction of laparoscopic nephrectomy at our center, which occurred in 1998 [13]. The largest gender difference observed in our study was in the partner-to-partner group, where approximately only a third of donors were male. This difference is likely explained by the fact that ESRD is more common among men. In Sweden, this figure has been about 66% of men for the study period in question [14]. In the cohort studied, 66% of partner-to-partner donations were a female donor donating to a spouse, which matches the expected frequency in heterosexual relationships, which is the case in this cohort. During pregnancy, female recipients may also have become sensitized and developed HLA antibodies to their children’s fathers, thereby excluding, to a larger degree, their male partners from becoming donors [15]. Another possible reason for why fewer males donate to their partners may be that, in addition to a higher frequency of ESRD, they are often also older and thus more likely to have other contraindications for donation, such as cardiovascular disease. Given the results of this study where there were more male donors in sibling-to-sibling and child-to-parent donations and the frequency of male donors in spousal donations was as expected, research and interventions to address the gender imbalance should be focused on the remaining relation groups.
In the recruitment of potential donors, healthcare professionals must act to the benefit of both donor and recipient, and this process involves medical and ethical aspects, including information about the risks and exploration of the motives for donation [16]. In both male and female donors in our study, it was the donors themselves who took the first initiative. Although there were no major differences in the main reasons men and women gave for becoming donors, there were nevertheless a number of important significant differences. Females more frequently stated that they wanted to help the recipient and that others wanted them to donate, whereas men more frequently stated that they saw it as their moral obligation to donate. These differences could also be the focus of further research and interventions to address the gender imbalance. A third (and the largest subgroup) of the donors were siblings. As stated above, in this group there were more male than female donors. Another Scandinavian study showed the strongest motives for donors to be a desire to help, self-benefit, and identification with the recipient. Siblings had a stronger sense of identification with the recipient [17].
The only significant change over time was less discomfort from the operation/scar in more recent years. This coincides with the introduction of minimally invasive surgical techniques and was not unexpected. It was, however, less expected to see how many donors still had discomfort a very long time after the donation. This somewhat surprising finding could reflect the fact that surgical literature has focused on reporting objective findings, such as hernia, and not self-reported experiences. It could also be related to the fact that this is a population of donors that have no therapeutic benefit of the surgery and may therefore have somewhat different expectations and reference points when it comes to what is acceptable as a result of surgery. Based on the self-reported findings, however, it was reassuring that the vast majority felt that the donation had had a positive influence on their lives and, also, that more females perceived it as positive, especially considering the gender imbalance.
The strengths of this study are the very high response rate and that it reflects more than three decades of live kidney donation. The limitations of the study are that it is based on a single center in Sweden and can therefore not be directly generalized to other countries. A further limitation is the retrospective design with long follow-up may have had an impact on participants’ memory and recollection, going back as far as 30 years ago. A live donation is, however, a unique, once-in-a-lifetime event that is likely to produce long-lasting memories. In the questionnaires, the donors were also given the option to state that they did not remember.
Conclusions
In conclusion, we found that females remained the most common donors over time, but found no major gender differences in attitudes or regarding the information given/received before donation, experiences after donation, or frequency of follow-up. The only area of gender difference identified were differences in one’s motivation to become a donor, where females were slightly more driven by wanting to “do good” and felt that others wanted them to donate, whereas males more frequently felt a “moral obligation.” These differences could also be the focus of further research and interventions to address the gender imbalance. Based on the outcomes of this study, the focus of such activities should be on relations other than sibling-to-sibling, child-to-parent and spouse-to-spouse donations, as there was no apparent gender imbalance in these relations.
Acknowledgements
We would like to thank all the donors for their contribution to this study and, ultimately, to the kidney recipients, as well as all of the nurses and physicians who helped us with the physical examinations at the donors’ local nephrology departments.
Abbreviations
- BMI
body mass index
- MDRD
modification of diet in renal disease formula
- ESRD
end-stage renal disease
Footnotes
Source of support: Departmental sources
Conflict of interest statement
None declared
References
- 1.Allen MB, Reese PP. Transforming living kidney donation with a comprehensive strategy. PLoS Med. 2016;13(2):e1001948. doi: 10.1371/journal.pmed.1001948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rodrigue JR, Kazley AS, Mandelbrot DA, et al. Living donor kidney transplantation: Overcoming disparities in live kidney donation in the US – Recommendations from a Consensus Conference. Clin J Am Soc Nephrol. 2015;10(9):1687–95. doi: 10.2215/CJN.00700115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matas AJ, Smith JM, Skeans MA, et al. OPTN/SRTR 2012 annual data report: Kidney. Am J Transplant. 2014;14(Suppl 1):11–44. doi: 10.1111/ajt.12579. [DOI] [PubMed] [Google Scholar]
- 4.Puoti F, Ricci A, Nanni-Costa A, et al. Organ transplantation and gender differences: a paradigmatic example of intertwining between biological and sociocultural determinants. Biol Sex Differ. 2016;7:35. doi: 10.1186/s13293-016-0088-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khalifeh N, Horl WH. Gender and living donor kidney transplantation. Wien Med Wochenschr. 2011;161(5–6):124–27. doi: 10.1007/s10354-011-0895-5. [DOI] [PubMed] [Google Scholar]
- 6.Csete M. Gender issues in transplantation. Anesth Analg. 2008;107(1):232–38. doi: 10.1213/ane.0b013e318163feaf. [DOI] [PubMed] [Google Scholar]
- 7.Malakoutian T, Hakemi MS, Nassiri AA, et al. Socioeconomic status of Iranian living unrelated kidney donors: A multicenter study. Transplant Proc. 2007;39(4):824–25. doi: 10.1016/j.transproceed.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 8.Denic A, Mathew J, Lerman LO, et al. Single-nephron glomerular filtration rate in healthy adults. N Engl J Med. 2017;376(24):2349–57. doi: 10.1056/NEJMoa1614329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zeier M, Dohler B, Opelz G, Ritz E. The effect of donor gender on graft survival. J Am Soc Nephrol. 2002;13(10):2570–76. doi: 10.1097/01.asn.0000030078.74889.69. [DOI] [PubMed] [Google Scholar]
- 10.von Zur-Mühlen B, Berglund D, Yamamoto S, Wadström J. Single-centre long-term follow-up of live kidney donors demonstrates preserved kidney function but the necessity of a structured lifelong follow-up. Ups J Med Sci. 2014;119(3):236–41. doi: 10.3109/03009734.2014.899654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lam NN, Lentine KL, Garg AX. Renal and cardiac assessment of living kidney donor candidates. Nat Rev Nephrol. 2017;13(7):420–28. doi: 10.1038/nrneph.2017.43. [DOI] [PubMed] [Google Scholar]
- 12.Tuohy KA, Johnson S, Khwaja K, Pavlakis M. Gender disparities in the live kidney donor evaluation process. Transplantation. 2006;82(11):1402–7. doi: 10.1097/01.tp.0000248953.64931.15. [DOI] [PubMed] [Google Scholar]
- 13.Wadström J. Laparoscopic donor nephrectomy technique. Transplant Proc. 2003;35(3):939–40. doi: 10.1016/s0041-1345(03)00171-4. [DOI] [PubMed] [Google Scholar]
- 14.Swedish Renal Registry. 2009. Available at: http://www.medscinet.net/snr/rapporterdocs/Publikation2009.pdf.
- 15.Bromberger B, Spragan D, Hashmi S, et al. Pregnancy-induced sensitization promotes sex disparity in living donor kidney transplantation. J Am Soc Nephrol. :2017. doi: 10.1681/ASN.2016101059. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mazaris EM, Warrens AN, Smith G, et al. Live kidney donation: Attitudes towards donor approach, motives and factors promoting donation. Nephrol Dial Transplant. 2012;27(6):2517–25. doi: 10.1093/ndt/gfr642. [DOI] [PubMed] [Google Scholar]
- 17.Lennerling A, Forsberg A, Meyer K, Nyberg G. Motives for becoming a living kidney donor. Nephrol Dial Transplant. 2004;19(6):1600–5. doi: 10.1093/ndt/gfh138. [DOI] [PubMed] [Google Scholar]