To the Editor—We read with interest the recent article by Chamilos et al regarding the risk of invasive fungal infection (IFI) associated with small molecule kinase inhibitors (SMKIs) [1]. In heeding the authors’ call for publication of such cases, we briefly present the case of a patient recently evaluated by our transplant infectious diseases service with invasive fungal sinusitis due to Mucorales.
Our patient was a 79-year-old man with chronic lymphocytic leukemia (CLL), well-controlled diabetes mellitus (hemoglobin A1c 6.9%), and coronary artery disease who presented with 3 weeks of progressive right maxillary sinus pain and fever. He was diagnosed with CLL 5 years prior and had intermittently required transfusions of red blood cells and platelets until initiating ibrutinib 17 months prior to presentation. He was hospitalized for community-acquired pneumonia once within the last 5 years but had no other history of severe or unusual infections. Computed tomography of his sinuses showed near-complete opacification of the right maxillary, ethmoid, and sphenoid sinuses. There was a small subperiosteal abscess extending through the inferior orbital wall adjoining an inferior orbital abscess. He was taken emergently to the operating room by otolaryngology and ophthalmology. He underwent right maxillary antrostomy, maxillectomy, and infratemporal fossa resection. All frozen sections showed angioinvasive fungal disease. A small length of tubing from an external ventricular drain device was tunneled inferolaterally into the orbit to instill intraorbital antifungal therapy. He was started on intravenous liposomal amphotericin B and isavuconazole along with amphotericin-soaked packing and twice-daily intraorbital infusion of amphotericin. Cultures from the sinus tissue yielded growth of a fluffy white mold within 72 hours (Figure 1A). Microscopic evaluation of a tease preparation of the mold revealed aseptate nonpigmented hyphae, eventually identified as mucor species (Figure 1B). Intravenous amphotericin was discontinued after 7 days of dual systemic antifungal therapy.
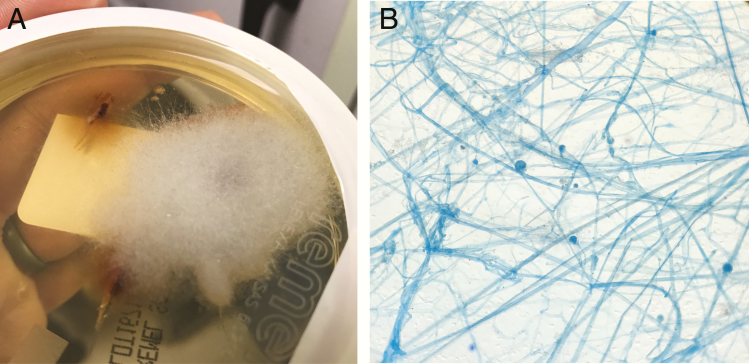
Figure 1.
A, Fungal culture at 30°C after approximately 72 hours. B, Tease preparation of the mold using lactophenol cotton blue stain.
His ibrutinib was discontinued at the time of admission out of concern for its contribution to his infection. His complete blood count was notable for pancytopenia along with absolute neutropenia and lymphocytopenia with nadirs of 520 cells/µL and 320 cells/µL, respectively, for which he was given granulocyte colony-stimulating factor. His total immunoglobulin G level was 207 mg/dL (normal range, 694–1618 mg/dL) for which he received intravenous immunoglobulin. He was discharged in stable condition after 17 days. At 2-month follow-up in clinic, he continues to improve with mild residual sinus pain and persistent cytopenias. We plan for an extended course of isavuconazole followed by indefinite mold prophylaxis if he restarts an SMKI.
After review of case reports of IFI related to ibrutinib, we believe this represents the first reported case of invasive fungal sinusitis with biopsy-proven Mucorales related to an SMKI. As noted in the viewpoint, IFI related to SMKIs will likely become more widespread as their use and indications expand. As infectious disease physicians, we must expand our differential diagnoses in patients on SMKIs to include opportunistic infections classically associated with more significant levels of immunosuppression.
Notes
Disclaimer. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Financial support. D.P.S. is supported by the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH) under Award Number UL1TR002378 and TL1TR002382.
Potential conflicts of interest. All authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Reference
- 1. Chamilos G, Lionakis MS, Kontoyiannis DP. Call for action: invasive fungal infections associated with ibrutinib and other small molecule kinase inhibitors targeting immune signaling pathways [manuscript published online ahead of print 27 September 2017]. Clin Infect Dis 2018; 66:140–148. [DOI] [PMC free article] [PubMed] [Google Scholar]