Abstract
Background
Inverted sinonasal (Schneiderian) papilloma (ISP) is a locally aggressive neoplasm often associated with sinonasal squamous cell carcinoma (SNSCC). While the etiology of ISP is not well understood, human papillomavirus (HPV) has been detected in a subset of cases. Our group recently identified activating somatic EGFR mutations in the majority of ISP and ISP-associated SNSCC. However, the relationship between EGFR mutations and HPV infection has not been explored.
Patients and methods
We evaluated 58 ISP and 22 ISP-associated SNSCC (including 13 patients with matched ISP/SNSCC samples), as well as 14 SNSCC without clinical or pathologic evidence of an associated ISP. Formalin-fixed, paraffin-embedded samples were evaluated for EGFR mutations using Sanger sequencing and for HPV infection using GP5+/GP6+ PCR. HPV subtyping based on the L1 sequence was done for HPV positive cases including temporally distinct tumors for four patients. Clinicopathologic data including progression free survival was also analyzed.
Results
All ISP and ISP-associated SNSCC demonstrated either an EGFR mutation or HPV infection. HPV and EGFR mutation were mutually exclusive in all cases of ISP-associated SNSCC and all but one ISP; this case was only weakly HPV positive, and analysis of a prior temporally distinct ISP specimen from this patient failed to show HPV infection, suggesting transient infection/incidental colonization. HPV subtypes in ISP and ISP-associated SNSCC were predominantly low-risk, in contrast with SNSCC without ISP association, which showed frequent high-risk HPV. All paired ISP and associated SNSCC samples demonstrated concordant HPV status and EGFR genotypes. ISP progression to SNSCC was significantly associated with the presence of HPV infection and the absence of an EGFR mutation (log-rank = 9.620, P = 0.002).
Conclusions
Collectively our data show that EGFR mutations and HPV infection represent essential, alternative oncogenic mechanisms in ISP and ISP-associated SNSCC.
Keywords: sinonasal (Schneiderian) papilloma, sinonasal squamous cell carcinoma (SNSCC), Sanger sequencing, human papillomavirus (HPV) subtypes, EGFR mutations
Introduction
Inverted sinonasal (Schneiderian) papilloma (ISP) is a benign neoplasm that arises from the respiratory-type (Schneiderian) epithelium of the lateral nasal wall or paranasal sinuses [1–3]. From a clinical standpoint, ISP is important due to its propensity for local recurrence and association with synchronous or metachronous sinonasal squamous cell carcinoma (SNSCC) in 10%–25% of patients [1, 4, 5]. The pathogenesis and etiology of ISP has been the subject of intense debate since before the first large-scale clinicopathologic analysis by Dr Vincent Hyams in 1971 [6], and over the past several decades, a possible role for human papillomavirus (HPV) infection has been explored by a number of independent groups [1, 7]. Recent meta-analyses have found evidence of HPV infection in up to 38% of ISP [7] and ∼33% of SNSCC (although not necessarily ISP-associated SNSCC) [8]. HPV infection in ISP was also found to be associated with an increased risk of progression to SNSCC [9].
Recently, utilizing targeted next-generation and conventional Sanger sequencing, our group identified activating, somatic EGFR exon 19 and 20 mutations in 88% of ISP and 77% of ISP-associated SNSCC [10]. We also demonstrated that matched pairs of ISP and associated SNSCC had concordant EGFR genotypes, providing the first genetic evidence of biological link between ISP and SNSCC. EGFR mutations were not found in exophytic papillomas, oncocytic papillomas or SNSCC without known ISP association, suggesting that ISP and associated SNSCC are biologically distinct from these other sinonasal tumors. We also showed that EGFR mutation status in ISP was an independent prognostic factor for progression to SNSCC. Finally, ISP-associated SNSCC cells showed increased EGFR signaling, which could be blocked using irreversible EGFR inhibitors causing potent growth inhibition.
Importantly, the pathogenesis of EGFR wild-type ISP and ISP-associated SNSCC remains uncertain and the relationship between EGFR mutations and HPV infection status in these tumors has never been explored. In this study, we sought to evaluate the association and clinical significance of EGFR mutations and HPV infection in a large retrospective cohort of ISP and ISP-associated SNSCC at our institution.
Patients and methods
Case selection
This study was approved by the Institutional Review Board at the University of Michigan Medical School. An unselected cohort of ISP and SNSCC cases was retrospectively identified from pathology records at Michigan Medicine: 58 ISP, 22 ISP-associated SNSCC (including 13 matched ISP/SNSCC pairs), and 14 SNSCC without clinical or pathologic evidence of associated ISP (SNSCC without known ISP association). Four exophytic sinonasal papillomas (ESP) and 27 oncocytic sinonasal papillomas (OSP) were also selected. The majority of the cases in this cohort were reported in two previous studies [10–12]. All diagnoses were confirmed by experienced head and neck pathologists (AMU and JBM).
Tissue extraction and DNA isolation
Representative non-decalcified formalin-fixed paraffin-embedded (FFPE) tissue was obtained for each case, and areas for extraction were designated by experienced head and neck pathologists (AMU and JBM). FFPE tissue was macrodissected from 10-μm sections on glass slides, and DNA was extracted using the Pinpoint Slide DNA Isolation System (Zymo Research, Irvine, CA) according to the manufacturer’s instructions. For ISP and SNSCC cases, areas of extraction were required to contain at least 30% tumor nuclei.
EGFR mutation status
Samples were examined for the presence of EGFR mutations using bi-directional Sanger sequencing and nested primers spanning exons 18, 19, 20, and 21, as described previously [10].
HPV infection status
Samples were examined for the presence of HPV DNA using GP5+/GP6+ consensus primers for L1 (∼150 bp product) [13]. Specimen adequacy was determined using PCO3/KM38 primers for β-globin (167 bp product) [14]. PCR products were evaluated by capillary electrophoresis using an Applied Biosystems 3130 Genetic Analyzer. Samples with a GP5+/6+ PCR product were deemed positive and subsequently evaluated by Sanger sequencing using the same primers. Samples were deemed negative if there was no GP5+/6+ PCR product and there was adequate amplification of β-globin [≥7000 relative fluorescence units (RFU)]. HPV subtypes were determined based on the L1 sequence using the NCBI Basic Local Alignment Search Tool (http://blast.ncbi.nlm.nih.gov/Blast.cgi (15 November 2017, date last acessed)).
Statistical analysis
All statistical analyses were carried out in Excel (Microsoft, Redmond, WA) using the XLSTAT package (Addinsoft SARL, Paris, France). Fisher’s exact and χ2 tests (as indicated) were utilized to examine associations between EGFR mutation and HPV infection status and categorical clinicopathologic parameters (i.e. gender, smoking history, and progression to SNSCC), while the relationship between EGFR mutation and HPV infection status was explored using the Student’s t-test. Progression-free survival analysis was carried out for patients diagnosed with ISP as described previously [10]. One patient without clinical follow-up was excluded from analysis. Given the 100% concordance between EGFR mutation and HPV status in paired ISP and associated SNSCC samples ([10] and see below), metachronous ISP-associated SNSCC without available ISP material included in the survival analysis were assumed to have the same EGFR and HPV status as the corresponding sequenced SNSCC. The Kaplan–Meier (log-rank) method was utilized to examine the association between EGFR mutation and HPV infection status and time to development of SNSCC, and univariate Cox regression analysis was used to estimate hazard ratios (HR) for progression. A P-value <0.05 was considered statistically significant.
Results
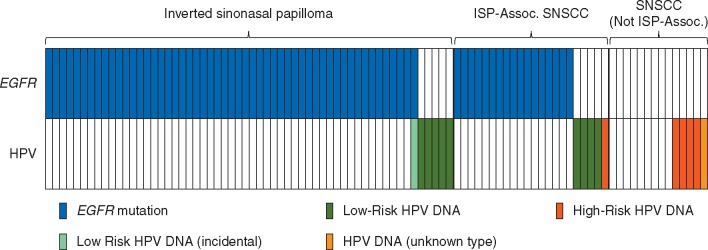
We previously identified EGFR mutations in 44 (88.0%) of the 50 ISP and 17 (77.3%) of the 22 ISP-associated SNSCC; no EGFR mutations were identified in any of the 20 SNSCC without known ISP association [10]. Forty-seven (94.0%) ISP, 21 (95.5%) ISP-associated SNSCC, and 13 (65.0%) SNSCC without known ISP association from this previous cohort were available for assessment of HPV status and included in this study. Eleven additional ISP cases were also included in this study, and nine (81.8%) were found to harbor an EGFR mutation; one additional ISP-associated SNSCC and one additional SNSCC without known ISP association were also included, and neither had an EGFR mutation. Therefore, in the current cohort, EGFR mutations were identified in 53 (91.4%) of 58 ISP and 17 (77.3%) of 22 ISP-associated SNSCC, while no EGFR mutations were identified in any of the 14 SNSCC without known ISP association (Tables 1 and 2; supplementary Table S1, available at Annals of Oncology online). HPV DNA was detected in 6 (10.3%) of 58 ISP, 5 (22.7%) of 22 ISP-associated SNSCC, and 5 (35.7%) of 14 SNSCC without known ISP association (Figure 1); all 4 (100.0%) ESP but none (0.0%) of the 27 OSP harbored HPV DNA. Importantly, all ISP and ISP-associated SNSCC harbored either an EGFR mutation or HPV DNA. In addition, EGFR mutations and HPV infection were mutually exclusive in ISP-associated SNSCC and showed a strong negative correlation in both ISP (P < 0.0001) and ISP-associated SNSCC (P < 0.0001).
Table 1.
Clinicopathologic characteristics of inverted sinonasal (Schneiderian) papillomas, stratified by EGFR mutation and HPV infection status
| Clinicopathologic parameter | EGFRmut/HPVneg (n = 53) | EGFRwt/HPVpos (n = 5) | P-value | |
|---|---|---|---|---|
| Age at initial diagnosis (years) | Mean | 50.8 | 46.2 | 0.515 |
| Median | 50 | 47 | ||
| Min | 26 | 24 | ||
| Max | 84 | 62 | ||
| Gender | Female | 9 (17.0%) | 2 (40.0%) | 0.209 |
| Male | 44 (83.0%) | 3 (60.0%) | ||
| Smoking history | Current/Former | 33 (62.3%) | 4 (80.0%) | 0.678 |
| Never | 19 (35.8%) | 1 (20.0%) | ||
| Unknown | 1 (1.9%) | 0 (0.0%) | ||
| Associated sinonasal squamous cell carcinoma | Yes | 11 (20.8%) | 3 (60.0%) | 0.050 |
| No | 42 (79.2%) | 2 (40.0%) | ||
| Human papillomavirus (HPV) status | Positive | 0 (0.0%) | 5 (100.0%) | <0.0001 |
| Negative | 53 (100.0%) | 0 (0.0%) |
Mut, mutant; wt, wild-type; pos, positive; neg, negative. Statistically significant P-value in bold.
Table 2.
Clinicopathologic characteristics of sinonasal squamous cell carcinoma (SNSCC), stratified by inverted sinonasal (Schneiderian) papilloma (ISP) association
| Clinicopathologic parameter | ISP-associated SNSCC (n = 22) | SNSCC without known ISP association (n = 14) | P-value | |
|---|---|---|---|---|
| Age at initial diagnosis (years) | Mean | 53.8 | 61.9 | 0.006 |
| Median | 54 | 65 | ||
| Min | 34 | 28 | ||
| Max | 72 | 76 | ||
| Gender | Female | 8 (36.4%) | 5 (35.7%) | 0.968 |
| Male | 14 (63.6%) | 9 (64.3%) | ||
| Smoking history | Current/Former | 18 (81.8%) | 12 (85.7%) | 1.000 |
| Never | 3 (13.6%) | 2 (14.3%) | ||
| Unknown | 1 (4.6%) | 0 (0.0%) | ||
| EGFR mutation status | Mutant | 17 (77.3%) | 0 (0.0%) | <0.0001 |
| Wild type | 5 (22.7%) | 14 (100.0%) | ||
| Human papillomavirus (HPV) status | Positive | 5 (22.7%) | 5 (35.7%) | 0.396 |
| Negative | 17 (77.3%) | 9 (64.3%) | ||
| Low-risk HPV subtype status | Positive | 4 (18.2%) | 0 (0.0%) | 0.118 |
| Negative | 18 (81.8%) | 13 (92.9%) | ||
| Unknown | 0 (0.0%) | 1 (7.1%) | ||
| High-risk HPV subtype status | Positive | 1 (4.5%) | 4 (28.6%) | 0.024 |
| Negative | 21 (95.5%) | 9 (64.3%) | ||
| Unknown | 0 (0.0%) | 1 (7.1%) |
Statistically significant P-value in bold.
Figure 1.
EGFR mutations and HPV infection are essential, mutually exclusive oncogenic events in inverted sinonasal papillomas and associated sinonasal squamous cell carcinomas. Frequency of EGFR mutations (blue), low-risk HPV DNA (green), and high-risk HPV DNA (red) in inverted sinonasal papilloma (ISP), ISP-associated sinonasal squamous cell carcinoma (ISP-Assoc. SNSCC) and sinonasal squamous cell carcinoma without a known ISP associated [SNSCC (Not ISP-Assoc.)]. A single case of ISP demonstrated both an EGFR mutation and transient, low-level HPV DNA that likely reflects incidental HPV colonization (light green). HPV subtype was unknown for one SNSCC (Not ISP-Assoc.; yellow).
Only a single case of ISP was found to have both an EGFR mutation (P772_H773insTNR) and evidence of HPV DNA. However, the HPV product in this sample was low-level (870 RFU) in spite of a strong β-globin product (8070 RFU), nearly 100% neoplastic cells in the extracted sample, and an EGFR variant allele frequency of ∼50%. The observed HPV positivity was also significantly lower than other positive samples (all ≥6000 RFU). Sample contamination was excluded by re-extracting this sample and confirming low-level HPV positivity (1120 RFU). To determine whether the low-level HPV positivity in this sample reflected transient infection/incidental colonization, a separate ISP sample from this patient collected 5 years prior was evaluated. This sample was negative for HPV in spite of a high percentage of neoplastic cells in the extracted sample and a high β-globin product (7854 RFU). In contrast, high-level HPV positivity was detected in temporally distinct samples from three EGFRwt/HPVpos cases (two ISP-associated SNSCC and one ISP) separated by 1, 8, and 9 years, respectively.
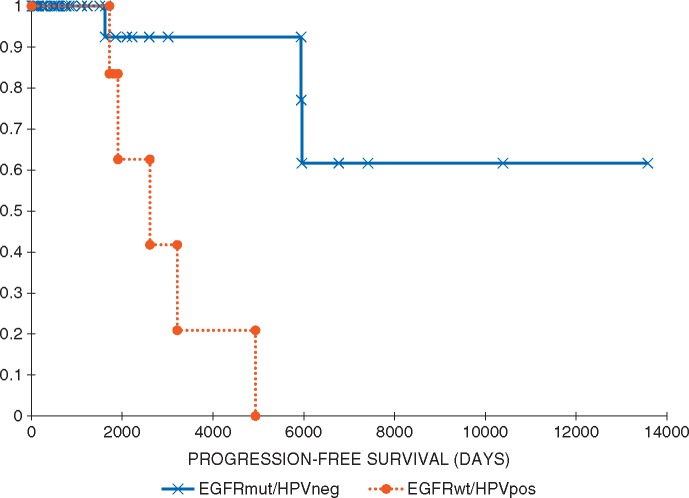
HPV-associated ISP were more frequently associated with synchronous or metachronous SNSCC (P = 0.05), although there were no significant differences in gender, age at initial diagnosis, or smoking history in patients with EGFR-mutant or HPV-associated ISP (Table 1). Progression to SNSCC was significantly associated with the presence of HPV infection and the absence of an EGFR mutation [log-rank = 9.620, P = 0.002; univariate HR = 14.358 (95% confidence interval = 1.631–126.429); P = 0.016]. Patients with ISP-associated SNSCC presented at an earlier age than those with SNSCC without known ISP association (median age at diagnosis 54 versus 65 years, respectively; P = 0.003). There were no significant differences in gender or smoking history (Table 2).
All ISP with detectable HPV DNA harbored low-risk subtypes (two subtype 6 and four subtype 11). Four (80.0%) of the 5 ISP-associated SNSCC with detectable HPV DNA harbored low-risk subtypes (two subtype 6 and two subtype 11), while high-risk HPV subtype 16 was detected in only one ISP-associated SNSCC. By comparison, four HPV+ SNSCC without any known ISP association harbored high-risk subtypes (two subtype 16, one subtype 18, and one subtype 33); L1 Sanger sequencing failed in one tumor. Altogether, high-risk HPV DNA was significantly more likely to be detected in SNSCC without known ISP association than in ISP-associated SNSCC (P = 0.024), while low-risk HPV DNA was more common in ISP-associated SNSCC (P = 0.118). Finally, paired ISP and associated SNSCC samples were available from 13 patients (2 metachronous, 9 synchronous, and 2 synchronous and metachronous), and importantly, all patients showed concordant EGFR genotypes, HPV status, and (if positive) HPV subtype (Table 3).
Table 3.
EGFR genotype and HPV status for matched pairs of inverted sinonasal papilloma with synchronous or metachronous sinonasal squamous cell carcinoma
| Patient | Synchronous/metachronous | Inverted sinonasal papilloma |
Sinonasal squamous cell carcinoma |
||
|---|---|---|---|---|---|
| EGFR genotype | HPV subtype | EGFR genotype | HPV subtype | ||
| 1 | Both | WT | HPV 11 | WT | HPV 11 |
| 2 | Synchronous | D770_N771insGL | Negative | D770_N771insGL | Negative |
| 3 | Synchronous | D770_N771insSVE | Negative | D770_N771insSVE | Negative |
| 4 | Metachronous | N771_H773dup | Negative | N771_H773dup | Negative |
| 5 | Synchronous | S768_D770dup | Negative | S768_D770dup | Negative |
| 6 | Synchronous | D770_N771insGD | Negative | D770_N771insGD | Negative |
| 7 | Both | WT | HPV 6 | WT | HPV 6 |
| 8 | Synchronous | N771_P772insV | Negative | N771_P772insV | Negative |
| 9 | Synchronous | S768_D770dup | Negative | S768_D770dup | Negative |
| 10 | Synchronous | N771_H773dup | Negative | N771_H773dup | Negative |
| 11 | Metachronous | S768_D770dup | Negative | S768_D770dup | Negative |
| 12 | Synchronous | N771delinsGF | Negative | N771delinsGF | Negative |
| 13 | Synchronous | S768_D770dup | Negative | S768_D770dup | Negative |
Discussion
This is the first study to examine the relationship between EGFR mutations and HPV infection status in ISP and SNSCC. The importance of EGFR and HPV is highlighted by the fact that all ISP and ISP-associated SNSCC harbored either an activating EGFR mutation or high-level HPV DNA positivity. In addition, we found that EGFR mutations and HPV infection are strongly and negatively correlated in both ISP and ISP-associated SNSCC (P < 0.0001). We identified only a single ISP patient (<2% of the cohort) that harbored both an EGFR mutation (P772_H773insTNR) and HPV infection (low-risk subtype 11). However, previous studies have detected HPV colonization in 4% and 7% of inflammatory nasal polyps and normal sinonasal mucosa, respectively [7]. Given the reported incidence of HPV colonization, a single case of incidental HPV colonization in a cohort of 68 patients with ISP/ISP-associated SNSCC is not an unexpected finding. While HPV PCR positivity was confirmed in multiple extractions from this sample, HPV DNA was detected at an extremely low level—significantly lower than that of every other HPV positive samples in spite of a high neoplastic content and a high-level EGFR variant allele frequency. In addition, an ISP specimen collected 5 years prior from the same patient was negative for HPV DNA while other HPV positive cases showed durable, high-level positivity over as long as nine years. These collective findings suggest that this case does indeed reflect transient incidental HPV colonization in an ISP driven by an oncogenic EGFR mutation and that EGFR mutations and true oncogenic HPV infection are mutually exclusive. Regardless, our results strongly suggest that activating EGFR mutations and HPV infection are alternative oncogenic mechanisms for the development of ISP [15].
In this study, HPV DNA was detected in 10.3% of ISP and 22.7% of ISP-associated SNSCC. While the frequency of HPV in SNSCC without an ISP association (35.7%) is similar to frequencies reported in SNSCC as a whole [8], the frequency of HPV-associated ISP in this study appears to be significantly lower than the frequency reported in a recent meta-analysis (38%) [7]. The reason for this discrepancy is uncertain. However, there appears to be tremendous variability in the reported HPV positivity rate in various studies. This may reflect HPV detection methodology differences such as limit of detection or comprehensiveness for various HPV subtypes. Indeed, the incidence of apparent incidental colonization in this study is lower than that reported in some other studies. However, geographic differences in the incidence of HPV as a whole may also explain the observed variability in ISP HPV positivity. These environmental factors may also affect the relative proportions of ISP patients with EGFR mutations versus HPV infection, as well as the local incidence of ISP and SNSCC.
Our evaluation of patients with paired ISP and associated SNSCC samples not only demonstrated concordant EGFR genotypes as previously described [10], but also concordant HPV status and (when positive) HPV subtyping (see Table 3). These findings add further support to the notion that ISP and SNSCC are clonally related and that ISP can be a precursor for SNSCC.
Similar to previous studies, our results show that HPV-associated ISP and ISP-associated SNSCC predominantly carry low-risk subtypes [7, 12], in contrast to SNSCC without known ISP association, which frequently harbor high-risk subtypes [16]. Along with the absence of EGFR mutations in SNSCC without an associated ISP, these findings provide further evidence that ISP/ISP-associated SNSCC are biologically distinct from other sinonasal squamous neoplasms. In addition, our findings suggest that papillary sinonasal tumors that harbor high-risk HPV subtypes are only rarely ISP or ISP-associated SNSCC, and thus, cases of high-risk HPV-associated ‘ISP with dysplasia’ should be examined carefully by pathologists to find convincing morphologic evidence of conventional ISP.
While high-risk HPV subtypes typically promote oncogenic transformation through the actions of E6 and E7 oncoproteins on the p53 and RB pathways, respectively, low-risk HPV subtypes generally lack strong E6 and E7 oncoprotein function [17]. In tumors harboring low-risk HPV subtypes, the E5 oncoprotein is thought play an important role in oncogenic transformation, and one of the major effects of the E5 oncoprotein is enhanced endogenous EGFR pathway signaling via inhibition of EGFR degradation, alteration of endosomal EGFR trafficking, and activation of downstream proteins (including MAPK and ERK1/2) [18]. Interestingly, our group has previously shown that EGFR protein expression is significantly higher in HPV-associated ISP compared with ISP without HPV infection [12]. Given the universal presence of either an EGFR mutation or HPV DNA in our cohort, EGFR pathway activation appears to play an essential role in the pathogenesis of ISP and associated SNSCC. We previously showed that treatment of EGFR-mutated ISP-associated SNSCC cells with irreversible tyrosine kinase inhibitors results in inactivation of EGFR signaling and growth inhibition [10]. Further studies are needed to determine whether EGFR pathway activation can be targeted in HPV-driven ISP/SNSCC and if EGFR targeted therapies can be successfully applied clinically. Our data provide a rational basis for exploring such therapies in ISP patients with locally aggressive, unresectable disease and in ISP-associated SNSCC.
Clinicopathologic risk factors and the molecular pathogenesis of ISP progression to SNSCC is not currently well understood [19]. In our previous study, we reported that EGFR mutation status was a prognostic risk factor for ISP malignant transformation, with EGFR mutated tumors being significantly less likely to progress to SNSCC [10]. This negative association of EGFR mutation with progression to SNSCC was also observed in the current study, while correspondingly, HPV positivity was associated with progression (Figure 2). HPV infection and genomic integration has previously been implicated as a risk factor for ISP malignant transformation in a number of studies [1, 12, 20]. A recent meta-analysis demonstrated that HPV infection is a significant risk factor for ISP progression to SNSCC, with a pooled odds ratio of 2.16 [9]. Therefore, the apparent negative association of EGFR mutations and progression may reflect the mutual exclusivity of EGFR mutations and oncogenic HPV infection. Additional molecular analysis of paired ISP and associated SNSCC are needed to determine the mechanisms of malignant transformation in both HPV-associated tumors and those without HPV infection.
Figure 2.
EGFR wild-type, HPV positive inverted sinonasal papillomas are associated with increased progression to sinonasal squamous cell carcinoma. Progression-free survival (in days) for EGFR mutated, HPV negative (EGFRmut/HPVneg) and EGFR wild type, HPV positive (EGFRwt/HPVpos) ISP using the Kaplan–Meier method [log-rank = 9.620, P = 0.002; univariate HR = 14.358 (95% confidence interval = 1.631–126.429); P = 0.016]. The single case of EGFR mutated, weakly HPV positive ISP was assumed to represent incidental HPV colonization and was allocated to the EGFRmut/HPVneg category.
We have shown that EGFR mutations and HPV infection represent alternate oncogenic mechanisms in all evaluated cases of ISP and ISP-associated SNSCC. These early etiologic events may have important prognostic and potential targeted therapeutic implications for the clinical management of the ISP/ISP-associated SNSCC disease spectrum, which could be explicitly explored in future studies.
Funding
Department of Pathology, Divisions of Anatomic Pathology and Clinical Pathology, of the University of Michigan Medical School, the University of Michigan Head and Neck Specialized Program of Research Excellence (SPORE; NCI P50 CA97248).
Key Message
In this study, we report that HPV infection and somatic EGFR mutations are essential, mutually exclusive oncogenic mechanisms for inverted sinonasal papillomas and associated sinonasal squamous cell carcinomas. These early etiologic events may have important prognostic and potential targeted therapeutic implications for the clinical management of the ISP/ISP-associated SNSCC disease spectrum.
Disclosure
The authors have declared no conflicts of interest.
Supplementary Material
References
- 1. Barnes L. Schneiderian papillomas and nonsalivary glandular neoplasms of the head and neck. Mod Pathol 2002; 15(3): 279–297. [DOI] [PubMed] [Google Scholar]
- 2. Bishop JA. OSPs and ESPs and ISPs, Oh My! An update on sinonasal (Schneiderian) papillomas. Head Neck Pathol 2017. March 20 [Epub ahead of print], doi:10.1007/s12105-017-0799-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Udager AM, McHugh JB.. Human papillomavirus-associated neoplasms of the head and neck. Surg Pathol Clin 2017; 10(1): 35–55. [DOI] [PubMed] [Google Scholar]
- 4. Lesperance MM, Esclamado RM.. Squamous cell carcinoma arising in inverted papilloma. Laryngoscope 1995; 105(2): 178–183. [DOI] [PubMed] [Google Scholar]
- 5. Tanvetyanon T, Qin D, Padhya T. et al. Survival outcomes of squamous cell carcinoma arising from sinonasal inverted papilloma: report of 6 cases with systematic review and pooled analysis. Am J Otolaryngol 2009; 30(1): 38–43. [DOI] [PubMed] [Google Scholar]
- 6. Hyams VJ. Papillomas of the nasal cavity and paranasal sinuses. A clinicopathological study of 315 cases. Ann Otol Rhinol Laryngol 1971; 80(2): 192–206. [DOI] [PubMed] [Google Scholar]
- 7. Syrjanen K, Syrjanen S.. Detection of human papillomavirus in sinonasal papillomas: systematic review and meta-analysis. Laryngoscope 2013; 123(1): 181–192. [DOI] [PubMed] [Google Scholar]
- 8. Syrjanen K, Syrjanen S.. Detection of human papillomavirus in sinonasal carcinoma: systematic review and meta-analysis. Hum Pathol 2013; 44(6): 983–991. [DOI] [PubMed] [Google Scholar]
- 9. Zhao RW, Guo ZQ, Zhang RX.. Human papillomavirus infection and the malignant transformation of sinonasal inverted papilloma: a meta-analysis. J Clin Virol 2016; 79: 36–43. [DOI] [PubMed] [Google Scholar]
- 10. Udager AM, Rolland DC, McHugh JB. et al. High-frequency targetable EGFR mutations in sinonasal squamous cell carcinomas arising from inverted sinonasal papilloma. Cancer Res 2015; 75(13): 2600–2606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Udager AM, McHugh JB, Betz BL. et al. Activating KRAS mutations are characteristic of oncocytic sinonasal papilloma and associated sinonasal squamous cell carcinoma. J Pathol 2016; 239(4): 394–398. [DOI] [PubMed] [Google Scholar]
- 12. Scheel A, Lin GC, McHugh JB. et al. Human papillomavirus infection and biomarkers in sinonasal inverted papillomas: clinical significance and molecular mechanisms. Int Forum Allergy Rhinol 2015; 5: 701–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cannavo I, Loubatier C, Chevallier A, Giordanengo V.. Improvement of DNA extraction for human papillomavirus genotyping from formalin-fixed paraffin-embedded tissues. Biores Open Access 2012; 1(6): 333–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Das D, Shah RB, Imperiale MJ.. Detection and expression of human BK virus sequences in neoplastic prostate tissues. Oncogene 2004; 23(42): 7031–7046. [DOI] [PubMed] [Google Scholar]
- 15. Udager AM, McHugh JB, Elenitoba-Johnson KS, Brown NA.. EGFR mutations in sinonasal squamous tumors: oncogenic and therapeutic implications. Oncoscience 2015; 2: 908–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rooper LM, Bishop JA, Westra WH.. Transcriptionally active high-risk human papillomavirus is not a common etiologic agent in the malignant transformation of inverted Schneiderian papillomas. Head Neck Pathol 2017. February 8 [Epub ahead of print], doi:10.1007/s12105-017-0779-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Doorbar J, Egawa N, Griffin H. et al. Human papillomavirus molecular biology and disease association. Rev Med Virol 2015; 25: 2–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Venuti A, Paolini F, Nasir L. et al. Papillomavirus E5: the smallest oncoprotein with many functions. Mol Cancer 2011; 10: 140.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Re M, Gioacchini FM, Bajraktari A. et al. Malignant transformation of sinonasal inverted papilloma and related genetic alterations: a systematic review. Eur Arch Otorhinolaryngol 2017; 274(8): 2991–3000. [DOI] [PubMed] [Google Scholar]
- 20. McKay SP, Gregoire L, Lonardo F. et al. Human papillomavirus (HPV) transcripts in malignant inverted papilloma are from integrated HPV DNA. Laryngoscope 2005; 115(8): 1428–1431. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.