Abstract
People living with HIV/AIDS (PLH) experience high rates of depression and related psychosocial risk factors that vary by gender. This study examines gender differences in depression severity among antiretroviral therapy (ART) patients (n = 362) from a large government ART clinic in Kolkata, India. Hypotheses for multiple linear regression models were guided by an integrated gendered stress process model focusing on variables reflecting social status (age, partner status), stressors (stigma), and resources (income, social support). Depressive symptoms were assessed with the Hospital Anxiety and Depression Scale (HADS); 22% of the sample reached the cutoff for severe depression, 56% moderate, and 13% mild depression. Compared to men, women reported lower income, education (50% no formal education vs. 20% men), availability of emotional and instrumental support, and were less likely to be married or cohabiting (53% women vs. 72% of men). However, more women had partners who were HIV-positive (78% women vs. 46% men). Overall, depression severity was negatively associated with availability of emotional support and self-distraction coping, and positively associated with internalized HIV/AIDS stigma, availability of instrumental support, and behavioral disengagement coping. Interactions for instrumental support by income and partner status by age varied significantly by gender. Analyses stratified by gender indicated that: 1) Frequently seeking instrumental support from others was protective for men at all income levels, but only for high-income women; and 2) having a partner was protective for men as they aged, but not for women. These results suggest that gender disparities in depression severity are created and maintained by women’s lower social status and limited access to resources. The effect of stigma on depression severity did not vary by gender. These findings may inform the tailoring of future interventions to address mental health needs of PLH in India, particularly gender disparities in access to material and social resources for coping with HIV.
Trial Registration: ClinicalTrials.gov registration #NCT02118454, registered April 2014.
Introduction
India has the third largest population of people living with HIV/AIDS (PLH) in the world, estimated at 2.3 million [1]. Depression is one of the most common co-morbidities of HIV worldwide [2]. High prevalence of depression has consistently been documented among PLH in India [3–8]. The few studies that have examined gender differences in depression among PLH in India have found higher prevalence and severity of depression among women than men [9, 10]. However, previous studies on HIV and mental health in India have included small samples of PLH (n < 100), which limit meaningful comparisons between men and women.
No studies to our knowledge have examined whether the relationship between gender and depression among PLH in India is modified by disparities between men and women in social status, exposure to stressors, or access to resources. For example, internalized HIV/AIDS stigma is a common stressor for PLH, and the effect of stigma on depression might vary by gender [11]. Similarly, access to and use of social support resources can modify the relationship between gender and depression [12].
This paper presents results from a cross-sectional analysis of baseline data with a sample of PLH (n = 362) at a large government clinic in Kolkata, India engaged in a randomized controlled trial of mobile phone support for ART adherence and self-management over six months [3]. First, we examined rates of mild, moderate, and severe depressive symptomology. Second, we tested gender differences in associations between depression severity and social status, stigma, and coping resources. We proposed a novel theoretical model, which posits that gender disparities in depression severity among PLH in India are maintained and exacerbated by an unequal distribution of stressors, resources, and social status between men and women.
Theoretical framework: Integrated model of the gendered stress process
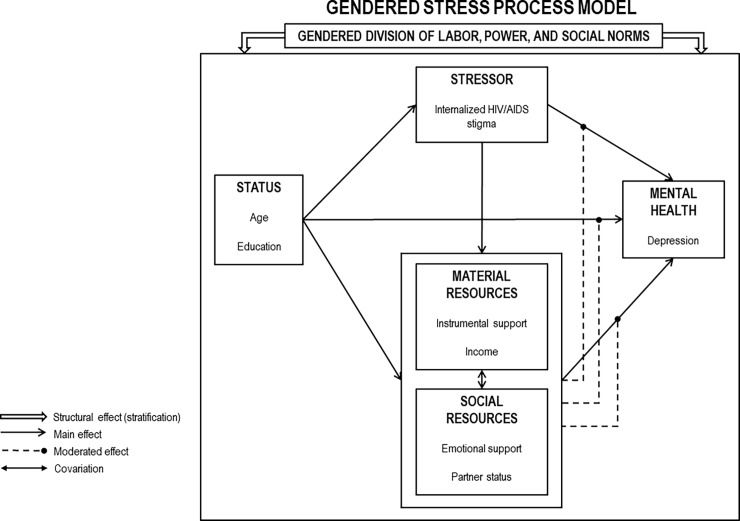
To examine gender differences in depression among PLH, we designed a model integrating the theory of gender and power [13] with the stress process model [14] (Fig 1). The theory of gender and power explains how social and institutional structures contribute to gender imbalances in power [13]. The stress process model explains how mental health disparities are created and maintained by social stratification, such that people at the bottom of the social hierarchy are exposed to more stressors and have access to fewer resources for coping with those stressors [14].
Fig 1. Gendered stress process model.
According to the theory of gender and power, three distinct but overlapping structures simultaneously create gender inequities between men and women: the gendered division of labor, the gendered division of power, and the structure of cathexis, which refers to social norms [15]. The unequal divisions of labor, power, and social norms create gender disparities, such as occupational segregation, less control over resources, and lower expectations for women compared to men in institutions, such as schools and workplaces [13]. In turn, these disparities lead to environmental exposures, interpersonal risks, and biological vulnerabilities that increase women’s susceptibility to disease and violence [16, 17]. The theory of gender and power has been applied to investigate disparities in HIV risk and physical outcomes, but it remains underutilized in the study of HIV and mental health [15, 18].
The stress process model explains how a person’s status within a stratified society influences exposure to stressors and access to resources, which in turn, create and sustain mental health disparities [14]. We theorize that the unequal status of men and women in India and the large gender gap in access to resources make the stress process of receiving an HIV diagnosis and managing ART adherence more detrimental to mental health for women than men.
Study hypotheses
Based on this integrated model of the gendered stress process, we hypothesize that the relationship between gender and depression severity among PLH in India is conditional on social statuses, stressors, and coping resources (See Fig 1). In the model, we conceptualize gender, age, and partner status as social status characteristics, stigma as a stressor, and emotional support, instrumental support, and income as resources. Partner status functions as both a social status and a social resource. Emotional support is a social resource while instrumental support and income are material resources. Hypotheses for the conditional relationships in the model are outlined below:
Conditional effect of social statuses: Age X partner status
H1-A: Age will be positively associated with depression level for both men and women due to accelerated functional decline from HIV with aging.
H1-B: Having a partner will reduce the strength of the relationship between age and depression level more for men than women. We expect that men will benefit more from having a partner as they age because women in India are expected to take on the role of caregiver for their spouses, but men are not [19].
Conditional effect of stressors: Stigma X partner status
H2-A: Internalized HIV/AIDS stigma will be positively associated with depression level for both men and women. In India, women with HIV/AIDS experience stigma due to assumptions about infidelity or engagement in sex work, whereas men experience stigma primarily due to assumptions about being gay, or to a lesser extent, purchasing commercial sex [20–22]. We expect the relationship between stigma and depression level to be stronger for women than men because the stigma experienced by PLH in India is more likely to be accompanied by physical abuse, social ostracism, and loss of economic resources for women than men [23–25].
H2-B: Having a partner will reduce the strength of the relationship between stigma and depression more for men than women. We expect that the positive relationship between stigma and depression level will be dampened more for men with a partner than women with a partner because women in India are expected to provide more emotional and caregiver support for sick spouses than men are [26–28]. Additionally, men living with HIV in India are more likely to be married to their partners than women living with HIV in India and are less likely to experience marital dissolution or have a partner desert them as a result of their diagnosis [29].
Conditional effect of resources: Instrumental support X income
H3-A: Instrumental support will be negatively associated with depression level for both men and women. We expect the protective effect of instrumental support to be stronger for men than women. Although men have access to more material resources than women in India, many studies suggest that women still provide more instrumental support to others than men provide on average, when someone close to them seeks financial or other forms of tangible assistance [30, 31].
H3-B: We expect that the relationship between instrumental support and depression severity will be conditional on income, such that higher income people will experience a stronger protective effect of instrumental support on depression level because they are more likely to be in social networks with other high income people who are capable of providing material support without eroding scarce resources or damaging social ties. In India, men and women have large income disparities, in which women are severely disadvantaged economically, so we expect the protective effect of coping by drawing on instrumental support by income level to be stronger for men than women.
Together, lower social status, higher exposure to stigma, and lower access to social support and economic resources among women compared to men in India will explain gender disparities in depression severity among PLH in India.
Methods
Study recruitment and data collection
Participants were recruited primarily from the Calcutta School of Tropical Medicine (STM) ART clinic, one of the three primary government sponsored ART clinics in Kolkata, India. Secondary recruitment was conducted from the Mamata Care and Treatment Center (MCTC), which is an ancillary support services center serving HIV-positive sex workers and their families. Recruitment was facilitated through verbal introduction scripts to patients in waiting areas of STM and MCTC, followed by the administration of screening questions in private.
Eligibility criteria were: 1) age of 18 years or older; 2) duration on ART of at least six months; 3) on first or second line ART (i.e., not on third line therapy due to prior treatment failures); 4) availability of CD4 counts in the prior two months (conducted routinely at six-month intervals); and 5) self-reported missing at least one ART dose in the past six months. If a prospective participant was eligible based on self-report, eligibility was confirmed by study staff reviewing the participant's “ART Cards” (i.e., a medical record issued by physicians to all ART patients in India). Signed consent forms were stored in a locked file in a locked office. Of 384 patients screened from April to July 2014, 362 were eligible and consented to participate in the study. Interviews were conducted in Bengali (primarily), Hindi, or English based on participants’ language preferences.
Participants were interviewed by a trained research team member administering a face-to-face baseline interview using a mobile phone application to record responses. Participants were queried on depression symptoms, social support, HIV-status disclosures, sexual behaviors, alcohol use, HIV/AIDS stigma, and strategies for coping with HIV/AIDS and ART adherence. Written informed consent was obtained from all individual participants included in the study. The protocol for this study was approved by the Institutional Review Boards of the University of California, Los Angeles and the Durbar Ethical Review Board. All procedures performed involving human participants were in accordance with the ethical standards of the Institutional Review Boards of University of California, Los Angeles and the Durbar Ethical Review Board in West Bengal, India.
Measures
Depression
The Hospital Anxiety and Depression Scale (HADS) was utilized to measure depression through the 8-item depression sub-scale (HADS-D). The HADS instrument has been validated in psychiatric research globally, with good internal validity and external consistency relative to more burdensome diagnostic tools such as ICD-08 and DSM-IV [32–34]. Example questions include, “I still enjoy the things I used to enjoy,” “I feel as if I am slowed down,” and “I have lost interest in my appearance”. Responses on a Likert-scale range from 0 “Not at all” to 3 “Most of the time” and reverse coded for negatively-framed items. The HADS-D has four recommended scoring levels based on the sum of the responses: none (0–7), mild (8–10), moderate (11–14), severe (15+). In this study, the HADS-D score was treated as a continuous variable indicating severity of depressive symptoms for linear regression analyses.
A recent pilot study in Kolkata, India validated the brief HADS measures of depression and anxiety with PLH [35] that was translated in Bengali to reduce confounding from somatization of physical symptoms and functional impairment. A second pilot study with PLH for the current study using this measure found high rates of depression and low rates of anxiety [3]. Therefore, the anxiety subscale was excluded in this study to reduce assessment burden.
Modified medical outcomes study social support (mMOS-SS) brief measures
The mMOS-SS operationalizes the perceived availability of emotional (intangible) support and instrumental (tangible) support. This brief 8-item version demonstrates excellent reliability, sensitivity, and specificity for two higher order factors of emotional support (caring, loving, and empathy) and instrumental support (tangible assistance and material resources provided by others) [36].
Coping with HIV and taking ART: Brief COPE measures
The Brief COPE is a reliable and abbreviated version of the longer COPE inventory, which has been used to assess frequency of behaviors for coping with chronic illnesses [37–39]. For this study, the questions were framed to assess coping specifically with HIV and taking ART. There are 14 sub-scales consisting of two items each with responses ranging from 0 “Not doing this at all” to 3 “Doing this a lot” and summed to a 0–6 score for each sub-scale domain: self-distraction, active coping, denial, substance use, use of emotional support, use of instrumental support, behavioral disengagement, venting, positive reframing, planning, humor, acceptance, religion, and self-blame. For example, self-distraction is assessed with the items: “I've been turning to work or other activities to take my mind off things” and “I've been doing something to think about it less, such as going to movies, watching TV, reading, daydreaming, sleeping, or shopping”.
Stigma
Internalized HIV/AIDS Stigma is a six-item measure of self-effacing and negative self-perceptions endorsed by PLH. The measure has been validated with ART patients in global contexts [40]. Items included: “It is difficult to tell people about my HIV infection,” and “Being HIV positive makes me feel dirty,” with “agree” or “disagree” responses to each item and summed to a 0–6 scale.
Alcohol use
AUDIT-C is an abbreviated 3-item alcohol screening scale, derived from the 10-item AUDIT instrument, and designed to identify hazardous drinkers or individuals with active alcoholism disorders. AUDIT-C is scored on a scale of 0–12 by summing responses to the three items. A higher score is associated with hazardous drinking habits and has been shown to be a reliable, practical, and valid measure to assess heavy drinking and alcohol use [41, 42].
Demographic characteristics
Characteristics of study participants included as control variables or moderators in the analysis were gender, age, income, educational attainment, partner status, HIV status of partner, and number of dependents. Gender is a dichotomous variable with responses 1 “Woman” versus 0 “Man”. Two transgender women were included in the “Woman” category since they identified as women and they mirrored cisgender women in the study on all measured demographic variables and not the cisgender men. Age is a continuous variable measured in years. Income is a continuous variable of individual monthly income categorized in 100 Indian rupee (INR) increments for analyses. Educational attainment is an ordinal categorical variable measured as highest education level completed with responses 0 “No formal education and illiterate”, 1 “No formal education but literate”, 2 “Class 5”, 3 “Class 10”, 4 “Class 12”, 5 “Graduate”, and 6 “Post-graduate”. Partner status is a dichotomous variable with responses 0 “Single and living alone” versus 1 “Married or living with partner”. HIV status of partner is a dichotomous variable with responses 0 “HIV-negative” versus 1 “HIV-positive or not sure”. Number of dependents is a continuous variable for total number of people relying on the respondent’s financial support ranging from zero to ten people.
Statistical data analysis
Baseline descriptive analysis was conducted using simple univariate frequency distribution methods. Bivariate correlation tables were used to inform variable selection and model building for the multiple linear regression analysis. Depression severity was analyzed as a continuous outcome variable ranging from 0–24 using multiple linear regression. Gender was used as the primary independent variable and is the main component of interactions in the multiple linear regression model. All analyses were conducted in Stata 13.1.
A hypothesis-driven approach was utilized to select predictors that had a theoretical basis for inclusion into multiple linear regression models either as a hypothesized predictor from the integrated gendered stress process model or as a control variable for confounding. Next, second-order interactions of gender by age, partner status, stigma, emotional support, and instrumental support were added to the models. Then, third-order interactions for gender by age by partner status and gender by instrumental support by household income were added. Because both third-order interactions were significant, we then stratified the multiple linear regression models by gender and re-tested correlates of depression severity separately for men and women to facilitate interpretation of the interactions.
Following an initial screen for collinearity of variables, two automated regression procedures were utilized as a sensitivity analysis to identify a best fit model using subset regression and score procedures. The subset and score methods resulted in highly concordant models with the same covariates being selected by the hypotheses for both models of the same size. Model fit was assessed in the linear regression models by comparisons of Akaike information criterion (AIC) values and the adjusted R2 value.
There were a small number of missing values for partner status (1 missing value) and income (24 missing values). All other variables had complete data. A sensitivity analysis using multiple imputation was conducted and yielded the same findings as the complete case analysis. For ease of interpretation, we present only the results from the complete case analysis in the tables and graphs of interactions.
Results
Table 1 provides a summary of sample characteristics overall and stratified by gender. The majority of participants were men with an average age of 39 years. Men in the sample had significantly higher social status across several demographic variables compared with women, consistent with gender disparities in the Indian general population. Men had higher income and educational attainment, were older, had more dependents, were more likely to be married or living with a partner, and were less likely to have a partner who was also living with HIV than women (all p<0.001). Approximately three-quarters of men in the sample were married or cohabiting compared with only half of the women. Nearly 80% of women in the sample had a partner who was also HIV-positive compared with less than half of men. Half of the women had no formal education compared with 20% of the men. Mean income was 5,184 Rs/month, with men reporting more than double the income of women, on average (6,459 Rs vs. 2,541 Rs, p < .001).
Table 1. Sample characteristics of people living with HIV in India, stratified by gender (N = 362).
| Women (n = 124) | Men (n = 238) | Total (N = 362) | P-value | ||||
|---|---|---|---|---|---|---|---|
| Freq. \ Mean | % \ SD | Freq. \ Mean | % \ SD | Freq. \ Mean | % \ SD | ||
| Dependent Variable | |||||||
| Depression Severity (HADS-D) [0–24] (Mean, SD) | 13.0 | 2.9 | 12.3 | 3.7 | 12.5 | 3.5 | 0.076† |
| None (0–7) | 5 | 4.1 | 28 | 11.8 | 33 | 9.1 | |
| Mild (8–10) | 15 | 12.3 | 30 | 12.6 | 46 | 12.7 | |
| Moderate (11–14) | 73 | 59.8 | 130 | 54.6 | 204 | 56.4 | |
| Severe (15–24) | 29 | 23.8 | 50 | 21.0 | 79 | 21.8 | |
| Independent Variable | |||||||
| Gender (%) | 124 | 34.3 | 238 | 65.7 | 362 | 100 | n.a. |
| Moderator Variables | |||||||
| Status | |||||||
| Age in Years [22–65] (Mean, SD) | 36.7 | 8.0 | 40.6 | 8.7 | 39.2 | 8.6 | < .001*** |
| Stressor | |||||||
| Internalized HIV/AIDS Stigma [0–6] (Mean, SD) | 2.6 | 1.5 | 2.6 | 1.8 | 2.6 | 1.7 | 0.975 |
| Resources | |||||||
| Married or Living with Partner (%) | 64 | 52.5 | 171 | 71.5 | 234 | 64.8 | < .001*** |
| Monthly Income in Indian Rupees [0–60,000] (Mean, SD) | 2540.9 | 3054.0 | 6458.8 | 7395.0 | 5184.0 | 6575.0 | < .001*** |
| Frequency of Instrumental Support (Brief-COPE) [0–6) (Mean, SD) | 2.2 | 1.3 | 2.4 | 1.3 | 2.4 | 1.3 | 0.135 |
| Control Variables | |||||||
| Educational Attainment by Highest Grade [0–6] (Mean, SD) | 1.5 | 1.3 | 2.4 | 1.4 | 2.1 | 1.4 | < .001*** |
| No Formal Education, Illiterate (0) | 36 | 29.5 | 26 | 10.9 | 62 | 17.1 | |
| No Formal Education, Literate (1) | 29 | 23.8 | 20 | 8.4 | 49 | 13.5 | |
| Class 5 (2) | 28 | 23.0 | 91 | 38.2 | 119 | 32.9 | |
| Class 10 (3) | 22 | 18.0 | 64 | 26.9 | 86 | 23.8 | |
| Class 12 (4) | 6 | 4.9 | 18 | 7.6 | 25 | 6.9 | |
| Graduate (5) | 1 | 0.8 | 14 | 5.9 | 16 | 4.4 | |
| Post Graduate (6) | 0 | 0.0 | 5 | 2.1 | 5 | 1.4 | |
| Has an HIV+ Partner (%) | 50 | 78.1 | 79 | 46.2 | 129 | 55.1 | < .001*** |
| Number of Dependents (Mean, SD) | 1.4 | 1.6 | 2.7 | 1.8 | 2.2 | 1.9 | < .001*** |
| Alcoholism (AUDIT-C) [0–12] (Mean, SD) | 0.3 | 1.0 | 0.5 | 1.3 | 0.4 | 1.2 | 0.072† |
| Availability of Social Support (mMOS-SS) [0–100] (Mean, SD) | |||||||
| Instrumental Support | 38.4 | 34.2 | 58.5 | 36.1 | 51.6 | 37.0 | < .001*** |
| Emotional Support | 30.3 | 26.0 | 42.5 | 26.7 | 38.3 | 27.0 | < .001*** |
| Frequency of Coping Responses (Brief-COPE) [0–6] (Mean, SD) | |||||||
| Behavioral Disengagement | 1.0 | 1.3 | 1.8 | 1.5 | 1.5 | 1.5 | 0.000*** |
| Active Coping | 2.6 | 1.1 | 3.1 | 1.3 | 2.9 | 1.2 | 0.000*** |
| Self-Blame | 0.8 | 1.0 | 1.2 | 1.3 | 1.1 | 1.2 | 0.003** |
| Planning | 2.1 | 1.1 | 2.5 | 1.1 | 2.4 | 1.1 | 0.004** |
| Venting | 1.3 | 1.3 | 1.8 | 1.5 | 1.6 | 1.5 | 0.005** |
| Acceptance | 3.3 | 1.7 | 3.8 | 1.7 | 3.7 | 1.7 | 0.006** |
| Humor | 0.6 | 0.9 | 0.4 | 0.8 | 0.4 | 0.8 | 0.005** |
| Substance Abuse | 0.1 | 0.3 | 0.3 | 0.8 | 0.2 | 0.7 | 0.021** |
| Denial | 0.8 | 0.9 | 1.1 | 1.3 | 1.0 | 1.2 | 0.016* |
| Positive Reframing | 2.5 | 1.2 | 2.7 | 1.3 | 2.7 | 1.3 | 0.043† |
| Self-Distraction | 2.5 | 1.3 | 2.8 | 1.5 | 2.7 | 1.4 | 0.059† |
| Emotional Support | 2.3 | 1.3 | 2.4 | 1.4 | 2.4 | 1.3 | 0.511 |
| Religion | 1.6 | 1.5 | 1.4 | 1.6 | 1.5 | 1.5 | 0.266 |
Notes: Significance level
† = p<0.10
* = p<0.05
** = p<0.01
*** = p<0.001
All scales ordered low to high
Monthly income is per 100 Indian Rupees
HADS-D is a subscale of the Hospital Anxiety and Depression Scale used to determine level of depression severity Brief-COPE is an abbreviated version of the COPE Inventory used to assess frequency of coping responses
AUDIT-C is an alcohol screening tool to identify hazardous drinkers or active alcohol use disorders.
mMOS-SS is the modified Medical Outcomes Study Social Support Survey used to measure availability of emotional and instrumental support.
Prevalence of depressive symptoms was high overall, with 56% of respondents scoring in the moderate range and 22% in the severe range. There was a marginal trend for gender differences in depression level (p = 0.08) but not a significant difference in the unadjusted bivariate comparison. AUDIT-C scores were low overall with mean score of 0.4 on a scale of 0–12. Internalized HIV/AIDS stigma scores were moderate overall with mean score of 2.6 on a 0–6 scale.
Overall, perceived availability of instrumental support was higher compared to perceived availability of emotional support (mean mMOS-SS score of 52 vs. 38 on 0–100 scale), and women reported lower availability of social support than men for both subscales (p < .001). The most common coping strategies used for dealing with HIV/AIDS and ART adherence were acceptance, active coping, self-distraction, positive reframing, planning, and drawing on emotional and instrumental support. Compared to women, men reported higher frequency of using active coping, acceptance, self-blame, substance abuse, denial, behavioral disengagement, venting, and planning. Men used humor to cope less frequently than women.
Multiple linear regression for predictors of depression severity
Table 2 presents the unstratified multiple linear regression model for predictors of depression severity as a continuous outcome. The model explained 52% of the variance in depression severity. Overall, depression severity was negatively associated with availability of emotional support from others (B = -0.06, 95% CI: -0.08 –-0.04) and frequency of using self-distraction as a coping strategy (B = -1.08, 95% CI: -1.34 –-0.82). Depression level was positively associated with internalized HIV/AIDS stigma (B = 0.61, 95% CI: 0.12–1.11), availability of instrumental support from others (B = 0.03, 95% CI: 0.01–0.04), and frequency of using behavioral disengagement as a coping strategy (B = 0.43, 95% CI: 0.22–0.65).
Table 2. Unstandardized multiple linear regression coefficients and 95% confidence intervals for correlates of depression severity among people living with HIV in India (n = 337).
| Depression Severity | B | 95% CI | |
|---|---|---|---|
| Constant | 13.992 | 10.584 | 17.401 |
| Gender | -0.462 | -4.843 | 3.919 |
| Age | -0.026 | -0.100 | 0.047 |
| Married or Living with Partner | -4.348† | -9.178 | 0.482 |
| Income (per 100 INR) | 0.022 | -0.006 | 0.050 |
| Internalized HIV/AIDS Stigma (0–6) | 0.612* | 0.120 | 1.105 |
| Availability of Emotional Support (0–100) | -0.062*** | -0.084 | -0.039 |
| Availability of Instrumental Support (0–100) | 0.029*** | 0.012 | 0.044 |
| Frequency of Instrumental Support (0–6) | 0.731** | 0.207 | 1.254 |
| Frequency of Disengagement (0–6) | 0.433*** | 0.220 | 0.646 |
| Frequency of Self-Distraction (0–6) | -1.081*** | -1.343 | -0.819 |
| Gender X Frequency of Instrumental Support | -1.343*** | -1.933 | -0.753 |
| Gender X Income | -0.035* | -0.065 | -0.005 |
| Frequency of Instrumental Support X Income | -0.015* | -0.029 | -0.002 |
| Gender X Frequency of Instrumental Support X Income | 0.019** | 0.005 | 0.032 |
| Gender X Age | 0.078 | -0.021 | 0.176 |
| Gender X Married or Living with Partner | 8.571** | 2.686 | 14.457 |
| Married or Living with Partner X Age | 0.134* | 0.008 | 0.260 |
| Gender X Married or Living with Partner X Age | -0.217** | -0.365 | -0.068 |
| F-test | F(21, 315) | 17.91*** | |
| Adjusted R-squared | 0.51 | ||
Notes: Significance level
† = p<0.10
* = p<0.05
** = p<0.01
*** = p<0.001
B = Regression coefficient
CI = Confidence interval
Among the coping strategies, self-distraction was associated with lower depression levels and behavioral disengagement was associated with higher depression levels. Specifically, for every one-unit increase on the COPE self-distraction scale (range 0–6), depression level decreased by 1.08 points, whereas for every one-unit increase on the COPE behavioral disengagement scale (range 0–6), depression level increased by 0.43 points. For every one-unit increase in internalized HIV/AIDS stigma, depression level increased by 0.61 points. For every 10-point increase in perceived availability of emotional support (range 0–100), depression level decreased by 0.06 points, and for every 10-point increase in perceived availability of instrumental support, depression level increased by 0.03 points.
Two of the three hypothesized interactions based on the gendered stress process model were significantly associated with depression level. The significant interactions were gender X frequency of coping by drawing on instrumental support X income (B = 0.02, 95% CI: 0.01–0.03) and gender X partner status X age (B = -0.22, 95% CI: -0.37 –-0.07). The interaction of gender X partner status X internalized HIV/AIDS stigma was tested but was not significantly associated with depression level (B = 0.01, 95% CI: -0.74–0.77, p = 0.973), so it was not included in Tables 2 and 3. These results support the hypotheses that gender disparities in depression are created and maintained by women’s lower social status and access to resources, but not the hypothesis regarding gender differences in exposure to stigma as a stressor.
Table 3. Unstandardized multiple linear regression coefficients and 95% confidence intervals for correlates of depression severity among people living with HIV in India, stratified by gender (n = 337).
| Women (n = 109) | Men (n = 228) | |||||
|---|---|---|---|---|---|---|
| Depression level | B | 95% CI | B | 95% CI | ||
| Constant | 13.989*** | 10.825 | 17.154 | 13.584*** | 10.793 | 16.375 |
| Age | -0.023 | -0.092 | 0.046 | 0.052 | -0.016 | 0.120 |
| Married or living with partner | -4.374* | -8.641 | -0.107 | 4.178* | 0.934 | 7.421 |
| Income (per 100 INR) | 0.021 | -0.005 | 0.047 | -0.013* | -0.023 | -0.003 |
| Internalized HIV/AIDS stigma (0–6) | 0.587*** | 0.288 | 0.886 | 0.399*** | 0.207 | 0.591 |
| Availability of emotional support (0–100) | -0.081*** | -0.118 | -0.045 | -0.051*** | -0.080 | -0.023 |
| Availability of instrumental support (0–100) | 0.049*** | 0.022 | 0.077 | 0.019† | -0.001 | 0.039 |
| Frequency of instrumental support (0–6) | 0.720* | 0.170 | 1.270 | -0.645** | -1.050 | -0.240 |
| Frequency of disengagement (0–6) | 0.405† | -0.051 | 0.860 | 0.443*** | 0.199 | 0.688 |
| Frequency of self-distraction (0–6) | -1.187*** | -1.700 | -0.675 | -1.051*** | -1.358 | -0.744 |
| Frequency of instrumental support X Income | -0.015* | -0.027 | -0.002 | 0.003† | -0.001 | 0.007 |
| Married or living with partner X Age | 0.133* | 0.015 | 0.251 | -0.084* | -0.166 | -0.003 |
| F-test | F (12, 96) | 7.78*** | F(12, 215) | 22.420*** | ||
| Adjusted R-squared | 0.429 | 0.532 | ||||
Notes: Significance level
† = p<0.10
* = p<0.05
** = p<0.01
*** = p<0.001
B = Regression coefficient
CI = Confidence interval
Multiple linear regression for predictors of depression severity stratified by gender
Table 3 presents the multiple linear regression coefficients and 95% confidence intervals for covariates of depression severity, stratified by gender. The model for women explained 43% of the variance in depression severity among women. The model for men explained 53% of the variance in depression severity among men. Among women, depression severity was negatively associated with availability of emotional support (B = -0.08, 95% CI: -0.12 –-0.05) and frequency of coping by self-distraction (B = -1.19, 95% CI: -1.70 –-0.68) and positively associated with internalized HIV/AIDS stigma (B = 0.59, 95% CI: 0.29–0.89) and availability of instrumental support (B = 0.05, 95% CI: 0.02–0.08). Like women, depression severity among men was negatively associated with availability of emotional support (B = -0.05, 95% CI: -0.08 –-0.02) and frequency of coping by self-distraction (B = -1.05, 95% CI: -1.36 –-0.74) and positively associated with internalized HIV/AIDS stigma (B = 0.40, 95% CI: 0.21–0.59). In contrast to women, depression severity among men was negatively associated with frequency of drawing on instrumental support (B = -0.65, 95% CI: -1.05 –-0.24) and positively associated with frequency of coping by behavioral disengagement (B = 0.44, 95% CI: 0.20–0.69).
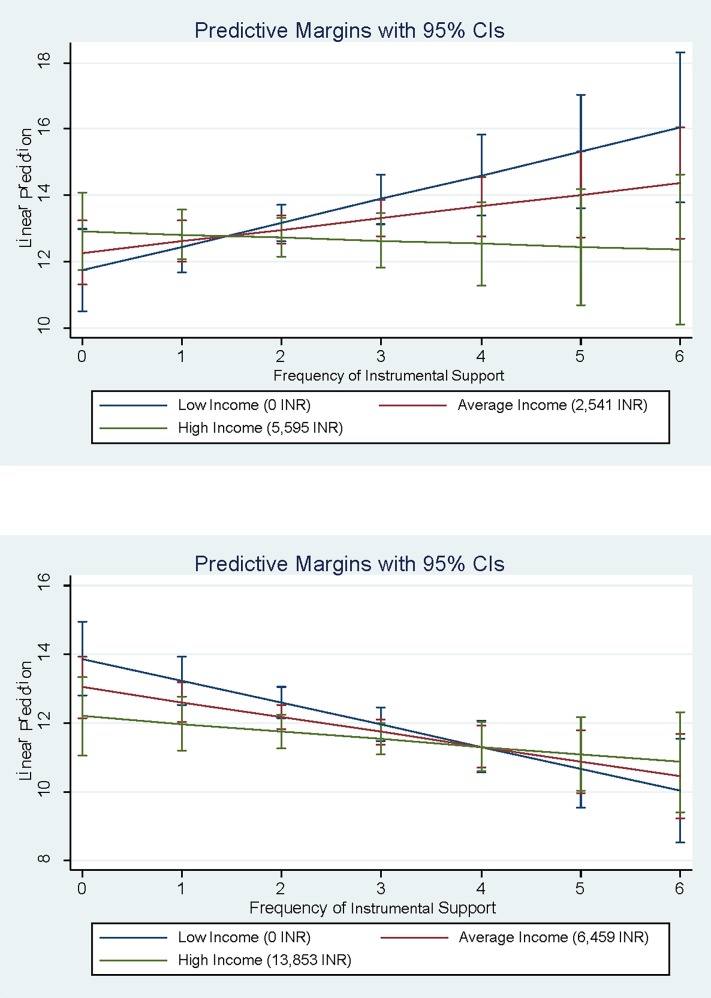
The interaction of frequency of coping by drawing on instrumental support X income was significantly associated with depression severity for women but not for men (see Fig 2A and 2B). For men of all income levels, frequency of drawing on instrumental support to cope with HIV was associated with lower severity of depression. However, this association was observed only for high-income women. Instrumental support was associated with higher severity of depression for women low-income women.
Fig 2.
a)Interaction of Instrumental Support by Income for Women b) Interaction of Instrumental Support by Income for Men.
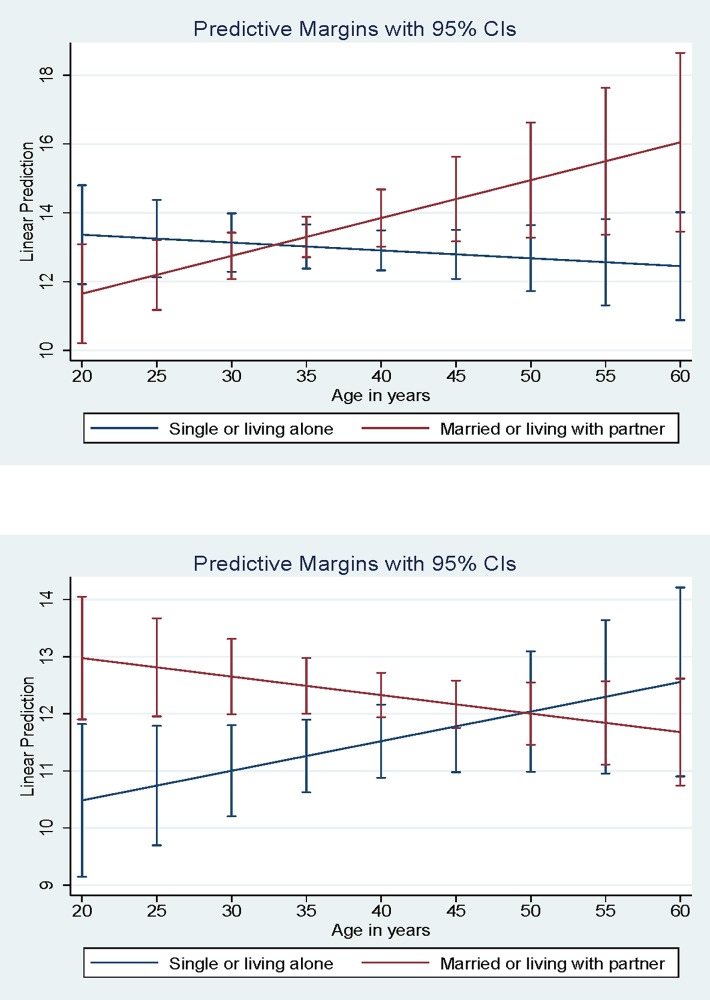
The interaction of partner status X age was significantly associated with depression severity for both women (B = 0.13, 95% CI: 0.02–0.25) and men (B = -0.08, 95% CI: -0.17 –-0.00), but the direction of the association was opposite for women versus men. As men age, having a partner is associated with lower depression severity, but as women age, having a partner is associated with high depression severity (Fig 3A and 3B).
Fig 3.
a) Interaction of Partner Status by Age for Women. Average Income = mean monthly income per respondent. Low Income = 1 standard deviation below the mean or 0 if negative. High Income = 1 standard deviation above the mean. b) Interaction of Partner Status by Age for Men.
Discussion
This study demonstrates high rates of depression among a sample of 362 PLH at government sponsored ART clinics in Kolkata, India. Over 75% of the sample met the threshold for moderate or severe depression based on the HADS-D instrument. Previous studies found a depression prevalence ranging from 12% –40% among PLH in India [6, 43], and a 12% prevalence of major depression and 13% prevalence of other depression symptoms among PLH in the United States [44]. The depression rate in this study is likely higher than most previous India and United States samples because the sample in this study is very low income. As a result, the participants in this study may have many structural risk factors for depression beyond their HIV diagnosis and ART adherence challenges. This study is the first to our knowledge to investigate gender disparities in depression, internal HIV/AIDS stigma, social support, and illness coping strategies among ART patients in India. The findings also provide support for the gendered stress process model proposed.
Gender disparities in depression severity among PLH in India are created and maintained by systems of social stratification that disadvantages women compared to men. This study’s results suggest that women’s lower social status and limited access to resources contribute to higher severity of depression. These findings are consistent with a study conducted in Kolkata, India that found 38.3% of female sex workers suffered from depression, with 27.3% having moderate to severe depression [45]. Existing literature has shown that female sex workers’ depression may be associated with family- and partner-related burdens and lack of support from husbands [46, 47]. Expectations regarding caregiving roles based on gender likely exacerbate these disparities. For example, we would expect that marriage or cohabitation would provide protective effects that reduce the severity of depression for PLH as they age because partnered individuals have more ready access to social and emotional support within the household and potentially to additional income. It is documented in different contexts that the positive influence of adequate emotional support can reduce depression among women living with HIV [48, 49]. However, because women living with HIV in India are more likely to have an HIV-positive spouse than men living with HIV, women take on additional burdens and receive less support from partners.
Previous research has found the need for instrumental support is greater among men than women [50]. This relationship was substantiated by our finding that coping by drawing on instrumental support was protective for men at all income levels, but only protective for high-income women. For low-income women and women with no individual income, attempting to cope by frequently drawing on instrumental support increased the severity of depression. This effect is likely due to low-income women being embedded within resource-poor social networks that have very little support to readily provide. Frequently seeking instrumental support can deplete the few scarce resources available to low-income women for coping with all types of stressors, eroding both material and social support, as our proposed gendered stress process model suggests.
The results also suggest that as men age, having a partner reduces the severity of depression, but as women age, having a partner increases the severity of depression. The likely explanation is that women are providing care to their partners as they age but are not receiving sufficient care from their partners. One factor that may be contributing to this pattern is that the women in the sample are significantly more likely to have HIV-positive partners than the men in the sample. This is reflective of trends in HIV transmission in India, generally, because most women living with HIV who are not sex workers contract HIV from their husbands/intimate partners [51, 52], whereas men are more likely to contract HIV from someone other than their wives/intimate partners [53].
Internalized HIV/AIDS stigma was a strong predictor of depression severity in this sample. In line with our hypothesis, internalized HIV/AIDS was positively associated with depression level for both men and women. Although we hypothesized that exposure to stigma as a stressor would be higher among women and thus contributing to these disparities, we did not find support for this hypothesis. Our findings are consistent with the hypotheses that the conditional effects of lower social status and fewer access to resources for women leads to disparities in depression severity between women and men even though to the effect of stigma is similar for both women and men.
Limitations
We acknowledge several limitations inherent to this study. First, the HADS-D is not a diagnostic measure of depression, but it is a reliable, brief assessment tool that is widely used in medical settings globally [54, 55], is highly correlated with diagnostic measures (i.e., has good concurrent validity), and has been translated in Bengali and validated for use in this context [35]. Second, depression was far higher than other samples. More than 90% of our sample reached the cutoff for at least mild depression based on the adapted HADS-D subscale. Two studies utilizing the HADS-D screening tool to measure depression among PLH found a depression prevalence ranging between 15%-30% [56, 57]. Several recent studies have found higher depression rates are associated with ART nonadherence compared to PLH who are adherent to their medication [58–60]. This may provide insight into the higher rates of depression among our sample of ART patients compared to other samples of PLH which may include people who are adherent to their ART regimens. We acknowledge this may not be a representative sample and results may not be generalizable to all PLH in India. Third, the cross-sectional nature of the analysis does not allow for causal inferences on temporality of variables examined. Therefore, it is important to be aware of the predictive limitations of the results. Since all variables are simultaneously assessed, it is difficult to infer temporal association between depression and psychosocial factors. In particular, the associations between behavioral disengagement and higher depression levels may be interpreted as the onset of depression preceded using behavioral disengagement to cope. Alternatively, PLH who report behavioral disengagement—or “giving up” attempts to cope with HIV and taking ART—may be at higher risk for developing depression over time [38]. Similarly, the findings surrounding self-distraction coping warrant further research. The observed association between self-distraction and lower depression severity may be interpreted that those with lower depression severity are able to take interest in things that distract from their HIV diagnosis, while those with more severe depression tend to lose interest in pleasurable activities. Previous literature has found self-distraction to be a maladaptive coping strategy resulting from depression [38, 61]. However, other studies found the use of self-distraction is associated with higher quality of life and lower levels of depression [62, 63]. The findings suggest the need for future longitudinal studies to better understand causal flow and/or bidirectional relationships of depression and psychosocial factors among PLH in India. The results of this cross sectional study may inform the hypotheses for a more complex, longitudinal cohort study.
Conclusion
This study demonstrates high rates of depression among ART patients in Kolkata, India and identifies psychosocial factors associated with depression that may be targets of future interventions, including internalized HIV/AIDS stigma, social support, and important coping and self-management strategies, which vary by gender. The findings identify a significant need among PLH in India for programs or services targeting mental health, tailored by gender, age, and partner status. India’s National AIDS Control Organization (NACO) previously supported PLH through a comprehensive program that addressed positive living, psychosocial support, counseling, referrals, and linkage to needs-based services [64]. This effort was part of the national response to meet the needs of PLH, specifically those from high-risk groups, women, and children [64]. However, in a massive cleanup of corruption and inadequate staffing, NACO discontinued its support for these services in 2008 [65]. Social support programs should be reinstated as part of non-medical services for PLH in resource-poor settings, particularly to facilitate additional support systems for women infected with HIV [66]. There is a critical lack of mental health services globally, particularly in low and middle income countries [8]. Mental health services may not only improve quality of life and daily functioning, but also support ART adherence and retention. These findings can inform enhanced strategies in future interventions to address mental health, access to material and social resources, and ART adherence. Gender-specific tailoring of interventions will likely be needed to optimize intervention effects.
Acknowledgments
This research was supported by collaborative funding from the National Institute of Allergy and Infectious Diseases (R21AI094666, Swendeman P.I.) and the Indian Council of Medical Research (INDO-US/86/9/20 1O ECD-II), Jana P.I.). Additional institutional support was provided by; the UCLA Center for HIV Identification, Prevention and Treatment Services (P30MH58107); the UCLA Center for AIDS Research (P30AI028697); the UCLA Clinical and Translational Science Institute (UL1TR000124). Dr. Fehrenbacher is also supported by the National Institute of Mental Health (T32MH109205). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or other funders. We would like to acknowledge the participants in this study, the field staff responsible for recruitment and assessment (Madhushree Das, Mousimi Chowdhury, Subharanjan Sinha), the study’s data manager (Aaron Scheffler), and Dimagi Inc. for electronic data collection tools. We also acknowledge the University of California Global Health Institute’s Center of Expertise in Women’s Health, Gender, and Empowerment for supporting the intellectual environment related to this work.
Data Availability
The ART Adherence Behaviour and Practices Among HIV Positives in Kolkata, India dataset that supports the findings of this study are publicly available in Data Archiving and Networking Services (DANS) repository with the identifier https://doi.org/10.17026/dans-zk9-azdj.
Funding Statement
This research was supported by collaborative funding from the National Institute of Allergy and Infectious Diseases (R21AI094666, Swendeman P.I.) and the Indian Council of Medical Research (INDO-US/86/9/20 1O ECD-II), Jana P.I.). Additional institutional support was provided by; the UCLA Center for HIV Identification, Prevention and Treatment Services (P30MH58107); the UCLA Center for AIDS Research (P30AI028697); the UCLA Clinical and Translational Science Institute (UL1TR000124). Dr. Fehrenbacher is also supported by the National Institute of Mental Health (T32MH109205).
References
- 1.Indian Council of Medical Resarch, UNAIDS. Technical report, India—HIV estimates 2012: UNAIDS; 2012. Available from: http://www.unaids.org/en/media/unaids/contentassets/documents/data-and-analysis/tools/spectrum/India2012report.pdf.
- 2.Simoni JM, Safren SA, Manhart LE, Lyda K, Grossman CI, Rao D, et al. Challenges in Addressing Depression in HIV Research: Assessment, Cultural Context, and Methods. AIDS and Behavior. 2011;15(2):376–88. 10.1007/s10461-010-9836-3 PubMed PMID: ISI:000286932800014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Swendeman D, Jana S, Ray P, Mindry D, Das M, Bhakta B. Development and Pilot Testing of Daily Interactive Voice Response (IVR) Calls to Support Antiretroviral Adherence in India: A Mixed-Methods Pilot Study. Aids and Behavior. 2015;19:S142–S55. 10.1007/s10461-014-0983-9 PubMed PMID: WOS:000357646800009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kermode M, Devine A, Chandra P, Dzuvichu B, Gilbert T, Herrman H. Some peace of mind: assessing a pilot intervention to promote mental health among widows of injecting drug users in north-east India. Bmc Public Health. 2008;8:294 10.1186/1471-2458-8-294 ; PubMed Central PMCID: PMCPMC2533322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chandra PS, Deepthivarma S, Carey MP, Carey KB, Shalinianant MP. A cry from the darkness: women with severe mental illness in India reveal their experiences with sexual coercion. Psychiatry. 2003;66(4):323–34. ; PubMed Central PMCID: PMCPMC2430935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chandra PS, Ravi V, Desai A, Subbakrishna DK. Anxiety and depression among HIV-infected heterosexuals—a report from India. J Psychosom Res. 1998;45(5):401–9. . [DOI] [PubMed] [Google Scholar]
- 7.Ahuja AS, Parkar SR, Yeolekar ME. Psychosocial aspects of seropositive HIV patients. J Assoc Physicians India. 1998;46(3):277–80. . [PubMed] [Google Scholar]
- 8.Patel V, Prince M. Global Mental Health A New Global Health Field Comes of Age. Jama-J Am Med Assoc. 2010;303(19):1976–7. 10.1001/jama.2010.616 PubMed PMID: WOS:000277764500027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Talukdar A, Parmar V, Bhattacharya R, Khanra D, Verma S, Talukdar P, et al. HIV Infected Elderly Women: From Rhetoric to Reality—Experience from Eastern India. World Journal of AIDS. 2014;4(1):1. [Google Scholar]
- 10.Short WE, Vissandjée B. Women Living with HIV in India: Looking up from a Place of Stigma, Identifying Nexus Sites for Change. Diversity and Equality in Health Care. 2017;14(3):159–66. [Google Scholar]
- 11.Simbayi LC, Kalichman S, Strebel A, Cloete A, Henda N, Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Social Science & Medicine. 2007;64(9):1823–31. 10.1016/j.socscimed.2007.01.006 PubMed PMID: WOS:000246786300004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vyavaharkar M, Moneyham L, Corwin S, Saunders R, Annang L, Tavakoli A. Relationships Between Stigma, Social Support, and Depression in HIV-Infected African American Women Living in the Rural Southeastern United States. J Assoc Nurse Aids C. 2010;21(2):144–52. 10.1016/j.jana.2009.07.008 PubMed PMID: WOS:000278339500007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Connell RW. Gender and Power. Polity. 1987:279–304. [Google Scholar]
- 14.Pearlin LI, Menaghan EG, Lieberman MA, Mullan JT. The stress process. Journal of Health and Social Behavior. 1981:337–56. [PubMed] [Google Scholar]
- 15.Wingood GM, DiClemente RJ. Application of the theory of gender and power to examine HIV-related exposures, risk factors, and effective interventions for women. Health Educ Behav. 2000;27(5):539–65. 10.1177/109019810002700502 PubMed PMID: WOS:000089417900001. [DOI] [PubMed] [Google Scholar]
- 16.Pulerwitz J, Gortmaker SL, DeJong W. Measuring sexual relationship power in HIV/STD research. Sex Roles. 2000;42(7–8):637–60. 10.1023/A:1007051506972 PubMed PMID: WOS:000088504400007. [Google Scholar]
- 17.Wingood GM, Diclemente RJ. The Role of Gender Relations in Hiv Prevention Research for Women. Am J Public Health. 1995;85(4):592–. 10.2105/Ajph.85.4.592 PubMed PMID: WOS:A1995QR24400031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lennon CA, Huedo-Medina TB, Gerwien DP, Johnson BT. A role for depression in sexual risk reduction for women? A meta-analysis of HIV prevention trials with depression outcomes. Soc Sci Med. 2012;75(4):688–98. 10.1016/j.socscimed.2012.01.016 ; PubMed Central PMCID: PMCPMC3383381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Joseph EB, Bhatti RS. Psychosocial problems and coping patterns of HIV seropositive wives of men with HIV/AIDS. Soc Work Health Care. 2004;39(1–2):29–47. 10.1300/J010v39n01_04 PubMed PMID: WOS:000226868400004. [DOI] [PubMed] [Google Scholar]
- 20.Steward WT, Herek GM, Ramakrishna J, Bharat S, Chandy S, Wrubel J, et al. HIV-related stigma: Adapting a theoretical framework for use in India. Social Science & Medicine. 2008;67(8):1225–35. 10.1016/j.socscimed.2008.05.032 PubMed PMID: WOS:000260200800004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thomas BE, Rehman F, Suryanarayanan D, Josephine K, Dilip M, Dorairaj VS, et al. How stigmatizing is Stigma in the life of people living with HIV: A study on HIV positive individuals from Chennai, South India. Aids Care. 2005;17(7):795–801. 10.1080/09540120500099936 PubMed PMID: WOS:000231429100002. [DOI] [PubMed] [Google Scholar]
- 22.Asthana S, Oostvogels R. The social construction of male 'homosexuality' in India: implications for HIV transmission and prevention. Social Science & Medicine. 2001;52(5):707–21. 10.1016/S0277-9536(00)00167-2 PubMed PMID: WOS:000166784100005. [DOI] [PubMed] [Google Scholar]
- 23.Chandra PS, Deepthivarma S, Manjula V. Disclosure of HIV infection in South India: patterns, reasons and reactions. Aids Care. 2003;15(2):207–15. 10.1080/0954012031000068353 PubMed PMID: WOS:000182470800007. [DOI] [PubMed] [Google Scholar]
- 24.Mawar N, Saha S, Pandit A, Mahajan U. The third phase of HIV pandemic: social consequences of HIV/AIDS stigma & discrimination & future needs. Indian J Med Res. 2005;122(6):471–84. . [PubMed] [Google Scholar]
- 25.Genberg BL, Hlavka Z, Konda KA, Maman S, Chariyalertsak S, Chingono A, et al. A comparison of HIV/AIDS-related stigma in four countries: Negative attitudes and perceived acts of discrimination towards people living with HIV/AIDS. Social Science & Medicine. 2009;68(12):2279–87. 10.1016/j.socscimed.2009.04.005 PubMed PMID: WOS:000268128700023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.D'Cruz P. The Family Context of Care in HIV/AIDS: A Study from Mumbai, India. The Qualitative Report. 2004;9(3):413–34. [Google Scholar]
- 27.Tarakeshwar N, Krishnan AK, Johnson S, Solomon S, Sikkema K, Merson M. Living with HIV infection: Perceptions of patients with access to care at a non-governmental organization in Chennai, India. Cult Health Sex. 2006;8(5):407–21. 10.1080/13691050600859609 PubMed PMID: WOS:000240654300003. [DOI] [PubMed] [Google Scholar]
- 28.Gupta RN, Swaminathan S, Wyatt GE, Rewari BB, Locke TF, Ranganath V, et al. Correlates of Relationship, Psychological, and Sexual Behavioral Factors for HIV Risk Among Indian Women. Cult Divers Ethn Min. 2008;14(3):256–65. 10.1037/1099-9809.14.3.256 PubMed PMID: WOS:000261640000010. [DOI] [PubMed] [Google Scholar]
- 29.Solomon S, Venkatesh KK, Brown L, Verma P, Cecelia AJ, Daly C, et al. Gender-Related Differences in Quality of Life Domains of Persons Living with HIV/AIDS in South India in the Era Prior to Greater Access to Antiretroviral Therapy. Aids Patient Care St. 2008;22(12):999–1005. 10.1089/apc.2008.0040 PubMed PMID: WOS:000261578700009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Helgeson VS. Social support and quality of life. Quality of Life Research. 2003;12:25–31. 10.1023/A:1023509117524 PubMed PMID: WOS:000183279000004. [DOI] [PubMed] [Google Scholar]
- 31.Valk R, Srinivasan V. Work–family balance of Indian women software professionals: A qualitative study. IMB Management Review. 2011;23(1):39–50. [Google Scholar]
- 32.Spinhoven P, Ormel J, Sloekers PPA, Kempen GIJM, Speckens AEM, VanHemert AM. A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychological Medicine. 1997;27(2):363–70. 10.1017/S0033291796004382 PubMed PMID: WOS:A1997WT61200012. [DOI] [PubMed] [Google Scholar]
- 33.Crawford JR, Henry JD, Crombie C, Taylor EP. Normative data for the HADS from a large non-clinical sample. Brit J Clin Psychol. 2001;40:429–34. 10.1348/014466501163904 PubMed PMID: WOS:000172345200007. [DOI] [PubMed] [Google Scholar]
- 34.Herrero MJ, Blanch J, Peri JM, De Pablo J, Pintor L, Bulbena A. A validation study of the hospital anxiety and depression scale (HADS) in a Spanish population. Gen Hosp Psychiat. 2003;25(4):277–83. 10.1016/S0163-8343(03)00043-4 PubMed PMID: WOS:000184201800009. [DOI] [PubMed] [Google Scholar]
- 35.Ghose T, Chowdhury A, Solomon P, Ali S. Depression and anxiety among HIV-positive sex workers in Kolkata, India: Testing and modifying the Hospital Anxiety Depression Scale. Int Soc Work. 2015;58(2):211–22. 10.1177/0020872813497381 PubMed PMID: WOS:000350481200002. [Google Scholar]
- 36.Moser A, Stuck AE, Silliman RA, Ganz PA, Clough-Gorr KM. The eight-item modified Medical Outcomes Study Social Support Survey: psychometric evaluation showed excellent performance. J Clin Epidemiol. 2012;65(10):1107–16. 10.1016/j.jclinepi.2012.04.007 PubMed PMID: WOS:000308118000010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Su XY, Lau JTF, Mak WWS, Choi KC, Feng TJ, Chen X, et al. A preliminary validation of the Brief COPE instrument for assessing coping strategies among people living with HIV in China. Infect Dis Poverty. 2015;4. doi: ARTN 41. 10.1186/s40249-015-0074-9 PubMed PMID: WOS:000367171800001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Carver CS. You want to measure coping but your protocol's too long: Consider the brief COPE. Int J Behav Med. 1997;4(1):92–100. 10.1207/s15327558ijbm0401_6 PubMed PMID: WOS:A1997XM28700006. [DOI] [PubMed] [Google Scholar]
- 39.Muller L, Spitz E. Multidimensional assessment of coping: validation of the Brief COPE among french population. Encephale. 2003;29(6):507–18. PubMed PMID: WOS:000189080800005. [PubMed] [Google Scholar]
- 40.Kalichman SC, Simbayi LC, Cloete A, Mthembu PP, Mkhonta RN, Ginindza T. Measuring AIDS stigmas in people living with HIV/AIDS: the Internalized AIDS-Related Stigma Scale. Aids Care. 2009;21(1):87–93. doi: Pii 906575058. 10.1080/09540120802032627 PubMed PMID: WOS:000261659000012. [DOI] [PubMed] [Google Scholar]
- 41.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA, Project ACQI. The AUDIT alcohol consumption questions (AUDIT-C)—An effective brief screening test for problem drinking. Arch Intern Med. 1998;158(16):1789–95. 10.1001/archinte.158.16.1789 PubMed PMID: WOS:000075829200007. [DOI] [PubMed] [Google Scholar]
- 42.Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin Exp Res. 2007;31(7):1208–17. 10.1111/j.1530-0277.2007.00403.x PubMed PMID: WOS:000247318400014. [DOI] [PubMed] [Google Scholar]
- 43.Charles B, Jeyaseelan L, Pandian AK, Sam AE, Thenmozhi M, Jayaseelan V. Association between stigma, depression and quality of life of people living with HIV/AIDS (PLHA) in South India–a community based cross sectional study. Bmc Public Health. 2012;12(1):463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Do AN, Rosenberg ES, Sullivan PS, Beer L, Strine TW, Schulden JD, et al. Excess Burden of Depression among HIV-Infected Persons Receiving Medical Care in the United States: Data from the Medical Monitoring Project and the Behavioral Risk Factor Surveillance System. Plos One. 2014;9(3). doi: ARTN e92842 10.1371/journal.pone.0092842 PubMed PMID: WOS:000333459900124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jana S, Ray P, Roy S, Piduttia J, Ghose T, Jana S. Depression and Its Relation with HIV Risk and Social Well-Being among the Brothel-Based Female Sex Workers in Kolkata, India. HSOA Journal of Community Medicine and Public Health Care. 2017;4(25). [Google Scholar]
- 46.Suresh G, Furr LA, Srikrishnan AK. An assessment of the mental health of street-based sex workers in Chennai, India. Journal of Contemporary Criminal Justice. 2009;25(2):186–201. [Google Scholar]
- 47.Ngugi EN, Wilson D, Sebstad J, Plummer FA, Moses S. Focused peer-mediated educational programs among female sex workers to reduce sexually transmitted disease and human immunodeficiency virus transmission in Kenya and Zimbabwe. Journal of Infectious Diseases. 1996;174:S240–S7. PubMed PMID: WOS:A1996VK50200013. [DOI] [PubMed] [Google Scholar]
- 48.Serovich JM, Kimberly JA, Mosack KE, Lewis TL. The role of family and friend social support in reducing emotional distress among HIV-positive women. Aids Care. 2001;13(3):335–41. 10.1080/09540120120043982 PubMed PMID: WOS:000169361300007. [DOI] [PubMed] [Google Scholar]
- 49.Musliner KL, Singer JB. Emotional support and adult depression in survivors of childhood sexual abuse. Child Abuse Neglect. 2014;38(8):1331–40. 10.1016/j.chiabu.2014.01.016 PubMed PMID: WOS:000339863000006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Grav S, Hellzen O, Romild U, Stordal E. Association between social support and depression in the general population: the HUNT study, a cross-sectional survey. J Clin Nurs. 2012;21(1–2):111–20. 10.1111/j.1365-2702.2011.03868.x PubMed PMID: WOS:000297953700013. [DOI] [PubMed] [Google Scholar]
- 51.Jacob SM, Sivasangeetha K, Anitha D, Dhavamani G. Use of Contraception among Women Living with HIV in Chennai, South India. International Journal of Pharma Research and Health Sciences. 2017;5(4):1785–88. [Google Scholar]
- 52.Silverman JG, Decker MR, Saggurti N, Balaiah D, Raj A. Intimate partner violence and HIV infection among married Indian women. Jama-J Am Med Assoc. 2008;300(6):703–10. 10.1001/jama.300.6.703 PubMed PMID: WOS:000258374500022. [DOI] [PubMed] [Google Scholar]
- 53.UNAIDS. HIV transmission in intimate partner relationships in India. New Delhi, India: Joint United Nations Programme on HIV/AIDS: 2009. [Google Scholar]
- 54.Montazeri A, Vahdaninia M, Ebrahimi M, Jarvandi S. The Hospital Anxiety and Depression Scale (HADS): translation and validation study of the Iranian version. Health and Quality of Life Outcomes. 2003;1(14). 10.1186/1477-7525-1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dahl AA, Haaland CF, Mykletun A, Bremnes R, Dahl C, Klepp O, et al. Study of anxiety disorder and depression in long-term survivors of testicular cancer. J Clin Oncol. 2005;23(10):2389–95. 10.1200/JCO.2005.05.061 PubMed PMID: WOS:000228260200034. [DOI] [PubMed] [Google Scholar]
- 56.Robertson K, Bayon C, Molina JM, McNamara P, Resch C, Munoz-Moreno JA, et al. Screening for neurocognitive impairment, depression, and anxiety in HIV-infected patients in Western Europe and Canada. Aids Care. 2014;26(12):1555–61. 10.1080/09540121.2014.936813 PubMed PMID: WOS:000343417200016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pappin M, Wouters E, Booysen FLR. Anxiety and depression amongst patients enrolled in a public sector antiretroviral treatment programme in South Africa: a cross-sectional study. Bmc Public Health. 2012;12. doi: Artn 244 10.1186/1471-2458-12-244 PubMed PMID: WOS:000305433000001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Uthman OA, Magidson JF, Safren SA, Nachega JB. Depression and Adherence to Antiretroviral Therapy in Low-, Middle- and High-Income Countries: A Systematic Review and Meta-Analysis. Curr Hiv-Aids Rep. 2014;11(3):291–307. 10.1007/s11904-014-0220-1 PubMed PMID: WOS:000340368500011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Blashill AJ, Bedoya CA, Mayer KH, O'Cleirigh C, Pinkston MM, Remmert JE, et al. Psychosocial Syndemics are Additively Associated with Worse ART Adherence in HIV-Infected Individuals. Aids and Behavior. 2015;19(6):981–6. 10.1007/s10461-014-0925-6 PubMed PMID: WOS:000356519600005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Magidson JF, Saal W, Nel A, Remmert JE, Kagee A. Relationship between depressive symptoms, alcohol use, and antiretroviral therapy adherence among HIV-infected, clinic-attending patients in South Africa. J Health Psychol. 2017;22(11):1426–33. 10.1177/1359105316628743 PubMed PMID: WOS:000408530400007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Carels RA, Musher-Eizenman D, Cacciapaglia H, Perez-Benitez CI, Christie S, O'Brien W. Psychosocial functioning and physical symptoms in heart failure patients—A within-individual approach. Journal of Psychosomatic Research. 2004;56(1):95–101. 10.1016/S0022-3999(03)00041-2 PubMed PMID: WOS:000220078500014. [DOI] [PubMed] [Google Scholar]
- 62.Kuehner C, Buerger C. Determinants of subjective quality of life in depressed patients: The role of self-esteem, response styles, and social support. J Affect Disorders. 2005;86(2–3):205–13. 10.1016/j.jad.2005.01.014 PubMed PMID: WOS:000229879400011. [DOI] [PubMed] [Google Scholar]
- 63.Lam D, Schuck N, Smith N, Farmer A, Checkley S. Response style, interpersonal difficulties and social functioning in major depressive disorder. J Affect Disorders. 2003;75(3):279–83. 10.1016/S0165-0327(02)00058-7 PubMed PMID: WOS:000184635700007. [DOI] [PubMed] [Google Scholar]
- 64.National AIDS Control Organization. Care amd Support Centres Ministry of Health & Family Welfare2015. Available from: http://naco.gov.in/care-and-support-centres-0.
- 65.Padma TV. India continues crackdown, dismissing hundreds of AIDS groups. Nature Medicine. 2008;14(3). [DOI] [PubMed] [Google Scholar]
- 66.National AIDS Control Organization. NACP-IV Components: Ministry of Health & Family Welfare; 2015. Available from: http://naco.gov.in/nacp-iv-components.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The ART Adherence Behaviour and Practices Among HIV Positives in Kolkata, India dataset that supports the findings of this study are publicly available in Data Archiving and Networking Services (DANS) repository with the identifier https://doi.org/10.17026/dans-zk9-azdj.