Abstract
Objective:
The association between food insecurity and obesity may be partially explained by overeating in response to unpredictable food availability cycles. The aim of this study was to measure objective food intake in food insecure individuals.
Methods:
82 volunteers (53m; BMI 29±7; 38±12y) were admitted to our inpatient Clinical Research Unit and completed the Food Security Short Form (FSSF), Three-Factor Eating Questionnaire and Gormally Binge Eating Scale and body composition assessment (DXA). After 5d of weight maintaining diet, participants self-selected food from an ad libitum vending machine paradigm for 3d. Mean daily intake (kcal), macronutrient intake, and percentage of weight maintaining energy needs (%WMEN) were calculated.
Results:
Based on FSSF cutoffs, food insecure participants (n=46; 56%) had higher body weight (p=.04), FFM (p=.05), disinhibition (p=.008), hunger (p=.02) and binge eating scores (p=.02), but not cognitive restraint (p=.37) compared to food secure individuals. They overate more kcal (p=.001), %WMEN (p=.003), fat (p=.003) and carbohydrates (p=.004) during the vending machine paradigm, continued to increase their hourly rate of kcal (group×time, β=37.7 cumulative kcal/hour, p<.0001) and ate more total kcal across the 72-hours (β=47.09 kcal/hour, p=.003).
Conclusion:
Food insecurity may amplify susceptibility to weight gain via overeating during times of unlimited food access.
Keywords: Binge eating, Obesity, Disordered Eating, Food Intake
Introduction
Food insecurity is a major health problem in the US affecting an estimated 42.4 million people and is associated with increased susceptibility to obesity, type 2 diabetes, mood/anxiety disorders, and disordered eating(1, 2, 3, 4). In 2006 the USDA eliminated hunger from their definition and food insecurity is currently defined as limited or uncertain availability of nutritionally adequate foods or the limited ability to acquire food in socially acceptable ways(1). Historically, food insecurity has been associated with malnutrition and being underweight(5) but rates of both obesity and food insecure households(6) have risen dramatically over the past decade, indirectly indicating a paradox linking obesity and food insecurity(7). Energy density and food costs are inversely associated, supporting the idea that food insecurity promotes dependence on inexpensive, palatable, energy-dense foods to meet caloric needs(8, 9). Furthermore, 1 in 7 Americans are dependent on monthly food assistant programs such as the Supplemental Nutrition Assistance Program (SNAP), the largest food assistant program in the US(10). These individuals tend to be economically dependent on low-cost/energy-dense foods to stretch their budget to ensure adequate food throughout the month(11).
It has been hypothesized that food insecure individuals alternate between times of adequate food availability and food scarcity(5, 6), a chronic cycle that promotes overeating of low-cost/energy-dense foods when food is available and restrictive behaviors when food is scarce, resulting in physiological shifts toward energy efficiency, increased storage of fat and subsequent weight gain(2, 12). The chronic cycle of restriction-overeating may lead to disordered eating behaviors which may increase anxiety and negative emotions towards food, subsequently promoting this vicious cycle(2).
Animal studies also provide insights into the food-insecurity obesity paradox. Mice exposed to random, intermittent fasting, gained more weight and fat mass compared to mice with both predictable food availability and predictable fasting sessions(13). Similarly, rats exposed to repeated food restrictive and binge feeding cycles were heavier compared to rats on a continuous restrictive feeding cycle(14). These rats also displayed reduced sensitivity to sensory/satiety factors which are important regulators of the cessation of eating. In humans, cyclic food restriction is associated with preferences for energy-dense foods and increased body fat(3). Thus, perceived unpredictable access to food, as mirrored in food insecurity, appears to promote hyperphagia of energy-dense foods and subsequent weight gain.
While a growing body of evidence indicates a link between food insecurity, energy intake and obesity, previous studies have only examined intake through self-reported food diaries, which are often biased and inaccurate(15, 16). Thus, the aim of the current study was to investigate differences between food secure and food insecure individuals in measures of adiposity, maladaptive eating behaviors and objectively measured ad libitum energy intake using a reproducible automated vending machine paradigm(17). We hypothesized food insecure individuals would have greater adiposity, maladaptive eating behaviors and would consume more calories compared to food secure individuals.
Methods
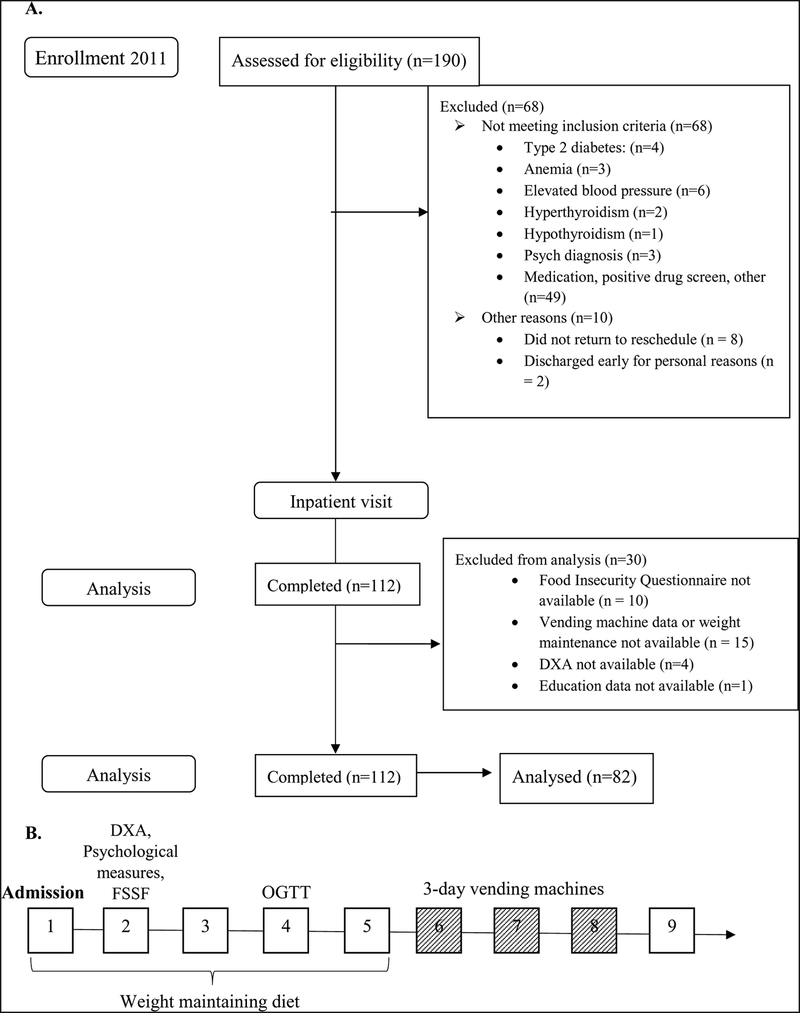
The current study measuring ad libitum food intake has been ongoing since 1999, however assessment of food insecurity was added in 2011. From November 11, 2011-March 3, 2017, 190 adults between the ages of 18–65 were recruited from the Phoenix area via advertisement in newspapers and in various public places such as, libraries, universities, hospitals and health clubs to participate in an ongoing natural history study assessing eating behavior and food preferences as risk factors for obesity using an ad libitum vending machine paradigm (Clinical Trial Identifier: NCT00342732). Of these, 112 met initial inclusion criteria (Fig. 1A.) and were admitted to our clinical research unit for at least 4-days. Screening, eligibility and available data are reported in the CONSORT diagram (Fig. 1A.). Only individuals with available food insecurity status, vending machine and DXA data were included in the current analyses resulting in a total of 82 participants. Prior to participation, all participants were informed of the nature, purpose and risks of the study and provided written informed consent. The protocol was approved by the Institutional Review Board of the NIDDK and is described in detail below (Fig. 1B.). All participants were healthy based on medical history, physical examinations and laboratory tests.
Fig. 1A.
Consort flow diagram.</p>B. Study diagram of the clinical study.</p>Day 1–5: Weight maintaining diet</p>Day 1: Admission and informed consent</p>Day 2: DXA (dual energy X-ray absorptiometry), Psychological measures, FSSF=Food Security Short Form</p>Day 4: OGTT (oral glucose tolerance test)</p>Day 6–7–8: Assessment of ad libitum food intake with vending machine paradigm</p>Day 9: Discharged
Study Design
Upon admission to the Obesity and Diabetes Clinical Research Unit (Phoenix, AZ), participants were placed on a standard weight maintaining diet for 5-days to standardize baseline food intake prior to ad libitum food consumption. Weight maintaining energy needs (WMEN) were calculated for each participant based on weight, sex and BMI(18) and each meal contained a macronutrient composition of 50% carbohydrate, 30% fat and 20% protein. Participants were instructed to consume the entirety of every weight maintaining meal. Within the first 2 days after admission, while participants were weight stable, body composition was determined by Dual-Energy X-Ray Absorptiometry (DPX-L; Lunar Radiation, Madison, WI) and participants completed the psychological questionnaires (described below) approximately 1-hour after eating breakfast. After 4-days of the weight maintaining diet, a 75g oral glucose tolerance test (OGTT) was done to exclude individuals with diabetes mellitus.
Vending Machine paradigm:
Ad libitum food intake was measured using automated vending machines, as previously described(17, 19, 20). Prior studies on our unit have shown high reproducibility (ICC=0.9) in intra-person energy intake pattern during repeated visits(17), demonstrating this method provides a highly accurate assessment of energy intake for persons admitted to our research unit. In brief, participants completed a Food Preferences Questionnaire (FPQ) after the day of admission, which was used to determine food preferences for stocking of vending machines, using a paradigm devised by Geiselman et al.(21). Participants rated their preference for a variety of foods on a 9-point Likert scale. Forty different foods given an intermediate rating were used to stock the vending machines for and were available each of the 3-days along with condiments. Participants were given free access to the machines for 23.5 hours with 30 minutes per day needed to re-stock the machines. The machines are computer operated and require a unique code given to each participant which records the time of day food was accessed. To correct for actual food intake, the metabolic kitchen staff weighed food leftovers returned by participants. These data were then imported into the Food Processor SQL Edition software (version 10.0.0, ESHA Research) which provided calories and macronutrient content of the foods. Energy intake is expressed as total kilocalories eaten per day, intake from macronutrients (kcal) and percent of WMEN consumed per day (%WMEN), calculated by dividing the total average kcal by WMEN.
Demographic Measures
Food Insecurity(22, 23, 24):
Food insecurity over a 12-month reference period was assessed using the validated 6-item Food Security Short Form (FSSF) of the USDA Household Food Security Model. A food security summary score was calculated and used to classify individuals as either food secure (score 0–1) or food insecure (score 2–6).
MacArthur Scale of Subjective Social Status (SSS)(25, 26):
was presented in a 10-step ladder format and used to assess subjective socioeconomic status (SSS). Participants were asked to place a cross on the level which they considered representative of their place in US society. Step 10 represents people who are best off, relative to the rest of the US (e.g., people perceive they have more money, higher educational achievements and better respected jobs). Step 1 represents people who perceive themselves as worse off, relative to the rest of the US (e.g. people have less money, lower education achievements and less respected jobs).
Psychological Measures
Three Factor Eating Questionnaire (TFEQ)(27):
is a 51-item questionnaire which classifies eating behavior into 3 factors: cognitive restraint, disinhibition, and susceptibility to hunger cues. Cognitive restraint reflects the intent to restrict food intake to control body weight, disinhibition is the self-reported overconsumption of food in response to various stimuli, hunger cues is associated with loss of control of eating in the presence of food related stimuli. Scores range from 0–21 (cognitive restraint), 0–16 (disinhibition) and from 0–14 (hunger cues), higher scores indicate greater disordered eating behaviors.
Gormally Binge Eating Scale (BES)(28):
is a 16-item self-report questionnaire that assesses the severity of binge eating behavior. Each item contains 3–4 response options reflecting a range of severity. The BES is designed to describe both behavioral and cognitive aspects of binge eating episodes and provides an overall severity score. Scores range from 0–46 and scores >27 are indicative of severe binge eating behaviors.
Statistical Analyses
Statistical analyses were done using SAS (Version 9.3) and SPSS (version 25). Alpha was set at 0.05 for all analyses besides the multivariate linear models in which a Bonferroni correction was used to correct for multiple analyses conducted on the sample and alpha was set at 0.008, 2-sided p-values were reported. Normally distributed data are presented as means±standard deviations. Because there were no significant differences in food intake between the 3-days by one-way ANOVA, all outcome variables are expressed as the average per day over the 3-days. Differences between food insecure and secure individuals were analyzed using Student’s t-tests. Differences between categorical variables were analyzed using chi-squared tests. There were no differences between Native Americans of Southwestern heritage (n=21, 26%), Other (i.e. individuals with a mixture of minority background; n=15, 18%), Hispanics (n=9, 11%) or Blacks (n=9, 11%) on anthropometric measures, psychological measures, or food insecurity status and these groups were combined into a mixed minority group (n=54, 66%) and were compared to non-Hispanic whites (n=28, 34%).
Multivariate analysis of variance (MANOVA) was used to assess group differences on the three TFEQ subscales and BES. Multivariate analysis of covariance (MANCOVA) was used to assess group differences while adjusting for age, sex, race/ethnicity and SSS. If the overall analysis was significant, univariate tests were examined. A series of multivariate linear analyses were used to assess differences in energy intake between food insecure and secure individuals, adjusting for age, sex, race/ethnicity, SSS and FFM. Least squared means with 95% confidence intervals were generated from these multivariate models. Repeated-measures mixed models were performed to compare the hourly food intake trajectories of the two groups over 72-hours using a first-order autoregressive covariance structure adjusted for age, sex, race/ethnicity, SSS and FFM. A group×time interaction term was also included to assess whether the trajectories of cumulative food intake were different between the two groups.
Results
Baseline Characteristics
Participants ranged in age from 18–65 years (M=38, SD±12) and ranged in BMI from 17–47kg/m2 (M=29, SD±7) (Table S1 in Supplement). Forty-six (56%) individuals were characterized as food insecure and thirty-six (44%) were characterized as food secure. Consistent with a physically and psychologically healthy cohort, the scores of psychological measures were not within clinical range. Food insecure individuals had lower SSS (t=2.39, p=.02) and higher body weight (t=−2.06, p=.04) and had nearly significant higher BMI (t=−1.74, p=.08) and FFM (t=−1.98, p=.05) compared to the food secure group. Age, years of education, height(m) and FM did not differ between groups. There were no significant sex (χ2=2.31, p=.13) or racial differences (χ2=.02, p=.90) between participants with and without food insecurity. Mean scores and correlations across all variables are shown in the in the Supplement (Table S2).
Eating Behavior Questionnaires
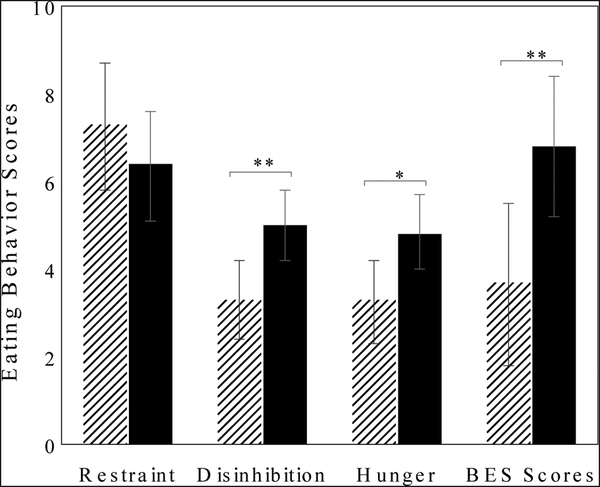
A MANOVA revealed group differences on the TFEQ and BES (Wilks’s Fs[4, 77]=3.13, p=.02, η2=.14). Univariate results indicated food insecure individuals had higher scores on disinhibition (F=7.29, p=.008; partial η2=.08), hunger cues (F=6.3, p=.01, partial η2=.07) and BES (F=7.2, p=.009, η2=.08), but not cognitive restraint (F=1.76, p=.19, η2=.02), even after adjusting for age, sex, race/ethnicity and SSS (Fig. 2.).
Fig. 2.
Mean eating behavior scores between food secure and food insecure individuals. Error bars represent the mean with 95% confidence interval.</p>* p<.05, ** p<.01, p-values adjusted for age, sex, race/ethnicity and subjective socioeconomic status.
Energy Intake
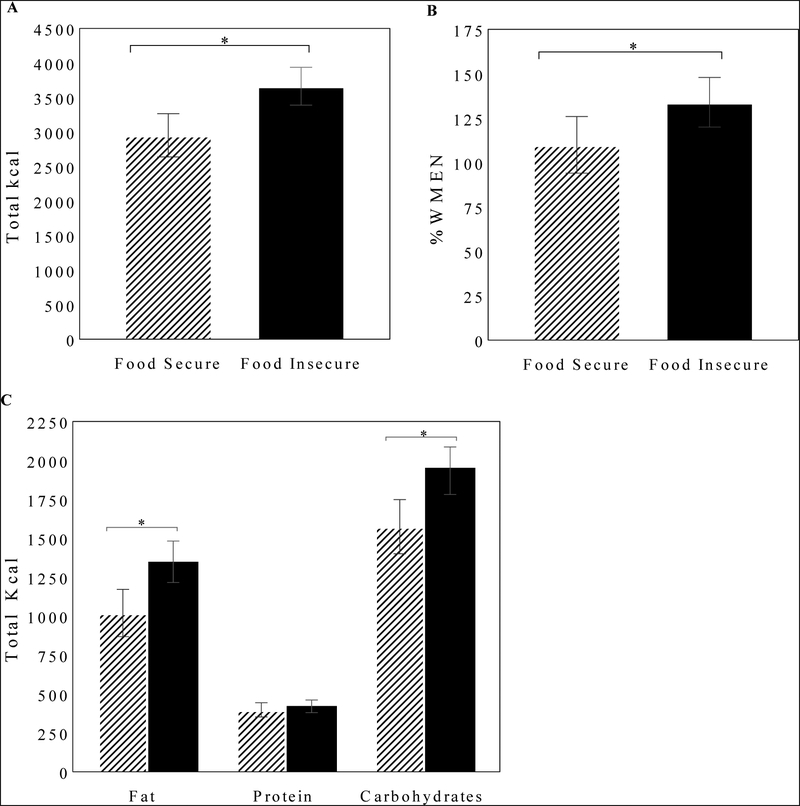
To examine whether food insecurity status predicted ad libitum energy intake during the vending machine paradigm, 5 separate multivariate linear models adjusted for age, sex, race/ethnicity, SSS and FFM were conducted. FFM, as we have previously reported(29), was positively associated with all food intake measures (Table S2 in Supplement). Food insecure individuals consumed significantly more total kcal (β=+710 kcal/day, p=.002, Table 1), %WMEN (β=+25% kcal/day, p=.004, Table 1), kcal from fat (β=+329 kcal/day, p=.003) and carbohydrates (β=+360 kcal/day, p=.004), but not protein (p=.47) compared to the food secure group. Least squares means and 95% confidence intervals are shown in Fig. 3.
Table 1.
Multivariate Linear Models
| Total Kcal | %WMEN | |||||
|---|---|---|---|---|---|---|
| Variables | B | CI | p-value | B | CI | p-value |
| Intercept | 1294.91 | −210.19, 2800.00 | .09 | 88.9 | 32.24, 145.68 | .003 |
| Age (Years) | 10.24 | −7.73, 28.21 | .26 | 0.33 | −0.35, 1.00 | .34 |
| Race/Ethnicity | −257.68 | −706.37, 191.01 | .26 | −8.9 | −25.87, 7.95 | .29 |
| (non-Hispanic White) | ||||||
| Sex (Male) | 767.53 | 188.61, 1346.46 | .01 | 28.33 | 6.51, 50.1 | .01 |
| SSS | −8.90 | −129.49, 111.7 | .88 | 0.13 | −4.41, 4.68 | .95 |
| FFM | 15.57 | −7.63, 38.77 | .18 | −0.13 | −1.00, 0.74 | .76 |
| Food Insecure | 710.35 | 277.93, 1142.78 | .002 | 24.50 | 8.21, 40.80 | .004 |
| R2=.38; F=7.55; p<.0001 | R2=.25; F=4.27; p=.0009 | |||||
β-Coefficients are reported with 95% CIs and p-values. Total intake=mean kcal/day; %WMEN=percent weight maintaining diet; SSS=subjective socioeconomic status; FFM=fat-free mass; Food Insecure=food insecure group
Fig. 3A.
Mean of 3-day energy intake (kcal/day) between food secure and food insecure individuals. B. Mean of 3-day energy intake, expressed as the percentage of their WMEN. C. Mean of 3-day macronutrient energy intake between food secure and food insecure individuals: fat (kcal/day), protein (kcal/day) and carbohydrates (kcal/day). Error bars represent the mean with 95% confidence interval.</p>* p<.05, p-values adjusted for age, sex, race/ethnicity, subjective socioeconomic status and fat-free mass.
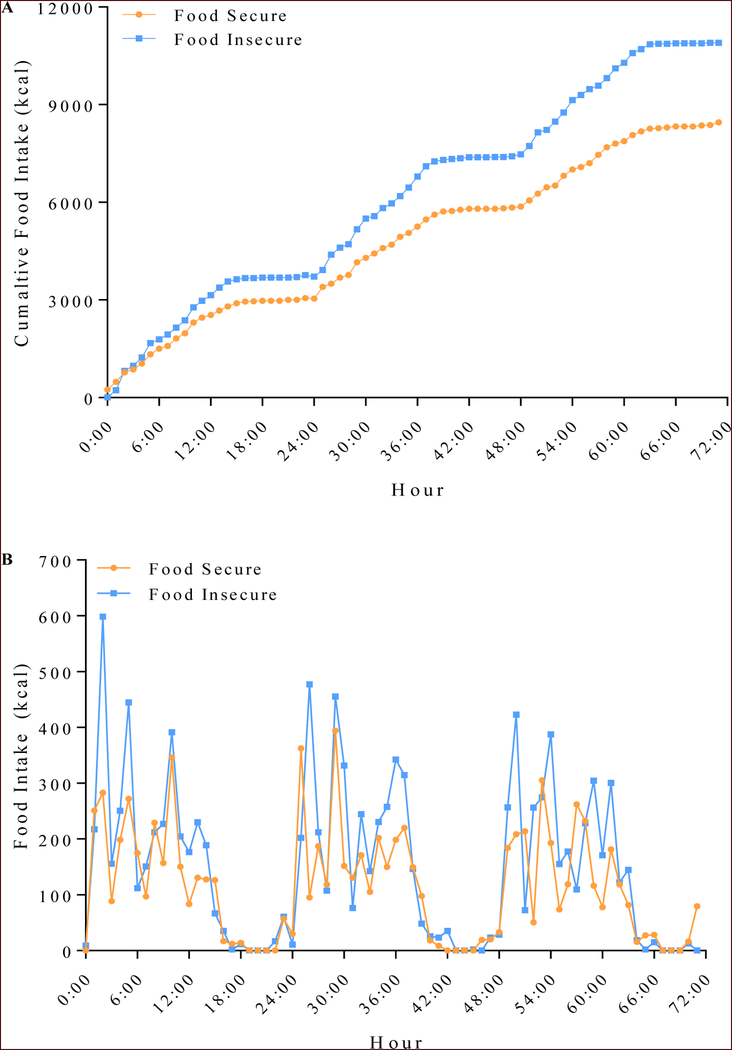
Repeated measures analysis of cumulative food intake over the 72-hours revealed that compared to the food secure group, the food insecure group had a greater hourly rate of cumulative food intake (interaction term group×time, β=37.7 cumulative kcal/hour, p<.0001, Fig. 4A.) and consistently ate significantly more total kcal across the 72-hours (β=47.09 kcal/hour, p=.003, Fig. 4B.).
Fig. 4A.
Cumalative food intake (kcal) and B. food intake per hour between food insecure and food secure individuals during a 72-hour ad libitum vending machine paradigm. Values are presented from hour 0:00 (6:00 AM) through hour 72:00 (6am day 3). (A) The hourly food intake of the food insecure group, shown in light blue, continued to increase over that of the food secure group, shown in orange, (interaction term group×time, β=37.7 cumulative kcal/hour, p<.0001) and (B) the food insecure group consistently ate more total kcal across the 72-hours (β=47.09 kcal/hour, p=.003).
Discussion
We have shown, that individuals who rate themselves as food insecure ingested greater total kcal and greater kcal relative to their WMEN over a 3-day period as measured by a highly reproducible ad libitum food intake paradigm in a controlled setting(17, 21). Food insecure individuals also had greater body weight and higher scores on indices of disordered eating behavior (i.e. disinhibition, hunger cues and binge eating) supporting the hypothesized vicious cycle that repeated patterns of restriction and overeating may contribute to disordered eating behavior. To our knowledge, there are no previous reports in the literature comparing food insecure and secure individuals on objectively measured food intake.
The utilization of an objective measure of food intake broadens the existing knowledge of the association between food insecurity with overeating(11, 12, 30). The ad libitum vending machine system employed in our study has been shown to be valid and highly reliable(17) as compared to less reliable measures such as 24-hour food recall questionnaires and self-report food diaries(8, 31, 32). Self-report measures are associated with underreporting of food intake and biased reports of high fat, palatable and energy-dense foods(15, 31, 33), most notably in those with obesity(16) and binge eating disorder(34). Furthermore, participants were on a weight maintaining diet for 5-days prior to the ad libitum vending machine paradigm and thus were not in a state of nutrient or caloric deficiency prior to the vending machine paradigm. This indicates that food insecurity may be an engrained construct resulting in overeating even when food is readily available without constraints.
Our results confirm a recent study by Becker and colleagues(4) who reported that severity of food insecurity in individuals seeking food from food pantries was associated with increased eating disorder pathology, weight self-stigma and worry. Similarly, a recent study randomized individuals to a high subjective social position or low subjective social position in a rigged game of Monopoly and assessed acute ad libitum food intake during a buffet meal(35). Results indicated that the individuals randomized to the low subjective social position ate significantly more during the ad libitum buffet meal, possibly due to their decreased feelings of pride and powerlessness. Our study extends these findings to a diverse group of individuals recruited from the general population and confirms reports of overeating with objectively measured food intake. The differences observed between food insecure and secure individuals in disinhibition, hunger cues and binge eating scores, but not cognitive restraint, indicates that overeating/binge eating behaviors may be of particular concern in this population. Furthermore, overeating in this population may be attributable to increased worry, powerlessness and pride which are associated with lower social status(4, 35).
Energy balance is defined as the interaction between energy intake and energy expenditure and eating in excess of metabolic needs results in a positive energy balance(36), which leads to ongoing weight gain. In the current study, food insecure individuals consistently overate during a 3-day period even after being on a weight maintaining diet for 5 consecutive days. Thus, food insecurity may result in a pattern of overeating whenever food is available, promoting positive energy balance, and in turn, subsequent weight gain and obesity(37, 38). Since food insecure adults are often trapped in cyclic food patterns moving from available food to food scarcity, they may be in a transient state of negative energy during restrictive times, such as when food stamp assistance runs out at the end of the month(5, 10). But when they do have access to food, such as during the beginning of the month, they may overeat, resulting in positive energy balance and increased risk of obesity(39). Thus, both poor diet quality over time and engagement in maladaptive eating behaviors such as those reported herein, may further exacerbate the documented health consequences observed in food insecure populations(40).
Despite previous reports (41, 42), SSS alone does not explain the important mechanism observed here between maladaptive eating behaviors and greater body weight in food insecure individuals. In the current study, food insecurity was a better predictor of overeating, above and beyond the effects of SSS. Food insecurity may indeed be better predictor of obesity because the chronic food insecurity cycle is a likely contributor to the chronic maladaptive eating patterns often linked to weight gain. This was evident in our data as measures of overeating were still significant after adjustment for SSS.
This study has several limitations. First, the ad libitum vending machine paradigm is an artificial environment with no barriers to food intake, which promotes overeating. However, this paradigm has shown high reliability, which is not true for self-reported food intake measures(17, 21, 43). Secondly, our longitudinal data of follow-up weight was limited and consisted of only 36% (n=30) of the total 82 participants. Thus, we were unable to examine the longitudinal effects of the overeating behaviors observed on our clinical unit. Third, follow-up measurements were not obtained for other variables which limited our ability to assess whether change in food insecurity status could improve the observed maladaptive eating behaviors. However, change in food insecurity status is relatively rare and would require much larger samples(44). Fourth, we did not utilize an objective measure of socioeconomic status. However, previous studies have found that SSS is more predictive of health outcomes(45). Lastly, participants were not from a clinical population and therefore scores on the BES were below the clinical range. However, we believe this is actually a strength, as we found that food insecure individuals scored higher on the BES, even within a normative range, which is likely more representative of the general population. Future research should focus on longitudinal measurements to determine whether maladaptive eating behaviors and increased food intake in food insecure individuals leads to weight gain over time.
Conclusion
We observed, that food insecurity, a significant public health issue, is associated with increased ad libitum food intake over a 3-day period using a direct and objective measure of food intake. The chronic cycle between food availability and food scarcity may be associated with the maladaptive eating behaviors observed in our study, amplifying susceptibility to overeating during times of unlimited access to food and thus predisposing food insecure individuals to obesity and weight gain. Replication and follow-up studies are needed to determine whether these observed relationships predict future weight gain and if changes in the food insecurity cycle can reverse eating behaviors specifically, overeating. Advocacy and policy initiatives to address the adverse health effects of food insecurity are critical to address the obesity epidemic and improve the health and livelihood of the 42.2 million individuals suffering from food insecurity.
Supplementary Material
Study Important Questions.
What is already known about this subject?
Food insecurity is a major health problem in the US affecting 42.4 million people and is associated with increased risk of obesity, type 2 diabetes and mood/anxiety disorders.
Individuals with food insecurity tend to alternate between periods of adequate food availability and food scarcity which promotes overeating of low-cost/energy-dense foods when food is available and restrictive behaviors when food is scarce, resulting in physiological shifts towards increased fat storage and weight gain.
What does this study add?
Food insecure individuals had greater body weights and higher scores on indices of disordered eating behavior.
The current study demonstrated that individuals who rate themselves as food insecure ingested greater total kcal, greater total kcal relative to their weight maintaining energy needs and consumed more kcal from fat and carbohydrates over a 3-day period as measured by a reproducible ad libitum food intake paradigm in a controlled setting.
Food insecure individuals continued to increase their hourly rate of food intake and consistently ate more total kcal across the 3-days as compared to food secure individuals.
Acknowledgements
The authors thank the volunteers who participated in our studies. They also thank the clinical staff of the Phoenix Epidemiology and Clinical Research Branch for conducting the examinations. The authors have nothing to disclose.
Sources of support
This study was funded by the Intramural Research Program of the National Institutes of Health (NIH) and the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Abbreviations:
- FFM
fat-free mass
- FM
fat mass
- DXA
Dual-Energy X-Ray Absorptiometry
- WMEN
Weight maintaining energy needs
- FSSF
Food Security Short Form
- TFEQ
Three-Factor Eating Questionnaire
- BES
Gormally Binge Eating Scale
- SSS
Subjective socioeconomic status
- NIH:
National Institute of Health
Footnotes
Clinical Trial Registration Number (clinicaltrials.gov): NCT00342732
Conflict of Interest
No conflict
References
- 1.Coleman-Jensen A, Rabbitt PM, Gregory AC, Singh A. Household food security in the United States in 2015. In: ERR-215 USDoA, Econimic Research Service (ed). September, 2016. [Google Scholar]
- 2.Laraia BA. Food insecurity and chronic disease. Advances in nutrition (Bethesda, Md) 2013;4: 203–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seligman HK, Schillinger D. Hunger and socioeconomic disparities in chronic disease. The New England journal of medicine 2010;363: 6–9. [DOI] [PubMed] [Google Scholar]
- 4.Becker CB, Middlemass K, Taylor B, Johnson C, Gomez F. Food insecurity and eating disorder pathology. The International journal of eating disorders 2017;50: 1031–1040. [DOI] [PubMed] [Google Scholar]
- 5.Ludwig DS, Blumenthal SJ, Willett WC. Opportunities to reduce childhood hunger and obesity: restructuring the Supplemental Nutrition Assistance Program (the Food Stamp Program). Jama 2012;308: 2567–2568. [DOI] [PubMed] [Google Scholar]
- 6.Dinour LM, Bergen D, Yeh MC. The food insecurity7obesity paradox: a review of the literature and the role food stamps may play. Journal of the American Dietetic Association 2007;107: 1952–1961. [DOI] [PubMed] [Google Scholar]
- 7.Crawford PB, Webb KL. Unraveling the paradox of concurrent food insecurity and obesity. American journal of preventive medicine 2011;40: 274–275. [DOI] [PubMed] [Google Scholar]
- 8.Leung CW, Epel ES, Ritchie LD, Crawford PB, Laraia BA. Food insecurity is inversely associated with diet quality of lower-income adults. Journal of the Academy of Nutrition and Dietetics 2014;114: 1943–1953.e1942. [DOI] [PubMed] [Google Scholar]
- 9.Widome R, Neumark-Sztainer D, Hannan PJ, Haines J, Story M. Eating when there is not enough to eat: eating behaviors and perceptions of food among food-insecure youths . American journal of public health 2009;99: 822–828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leung CW, Epel ES, Willett WC, Rimm EB, Laraia BA. Household food insecurity is positively associated with depression among low-income supplemental nutrition assistance program participants and income-eligible nonparticipants. The Journal of nutrition 2015;145: 622–627. [DOI] [PubMed] [Google Scholar]
- 11.Laraia B, Vinikoor-Imler LC, Siega-Riz AM. Food insecurity during pregnancy leads to stress, disordered eating, and greater postpartum weight among overweight women. Obesity (Silver Spring, Md) 2015;23: 1303–1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Finney Rutten LJ, Yaroch AL, Colón-Ramos U, Johnson-Askew W, Story M. Poverty, food insecurity, and obesity: a conceptual framework for research, practice, and policy. Journal of Hunger & Environmental Nutrition 2010;5: 403–415. [Google Scholar]
- 13.Zhang L- N, Mitchell SE, Hambly C, Morgan DG, Clapham JC, Speakman JR. Physiological and behavioral responses to intermittent starvation in C57BL/6J mice. Physiology & behavior 2012;105: 376–387. [DOI] [PubMed] [Google Scholar]
- 14.Ahn S, Phillips AG. Repeated cycles of restricted food intake and binge feeding disrupt sensory-specific satiety in the rat. Behavioural Brain Research 2012;231: 279–285. [DOI] [PubMed] [Google Scholar]
- 15.Arab L, Tseng CH, Ang A, Jardack P. Validity of a multipass, web-based, 24-hour self-administered recall for assessment of total energy intake in blacks and whites. American journal of epidemiology 2011;174: 1256–1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bailey RL, Mitchell DC, Miller C, Smiciklas-Wright H. Assessing the effect of underreporting energy intake on dietary patterns and weight status. Journal of the American Dietetic Association 2007;107: 64–71. [DOI] [PubMed] [Google Scholar]
- 17.Venti CA, Votruba SB, Franks PW, Krakoff J, Salbe AD. Reproducibility of ad libitum energy intake with the use of a computerized vending machine system. The American journal of clinical nutrition 2010;91: 343–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ferraro R, Boyce VL, Swinburn B, De Gregorio M, Ravussin E. Energy cost of physical activity on a metabolic ward in relationship to obesity. The American journal of clinical nutrition 1991;53: 1368–1371. [DOI] [PubMed] [Google Scholar]
- 19.Salbe AD, Tschop MH, DelParigi A, Venti CA, Tataranni PA. Negative relationship between fasting plasma ghrelin concentrations and ad libitum food intake. The Journal of clinical endocrinology and metabolism 2004;89: 2951–2956. [DOI] [PubMed] [Google Scholar]
- 20.Rising R, Alger S, Boyce V, Seagle H, Ferraro R, Fontvieille AM, et al. Food intake measured by an automated food-selection system: relationship to energy expenditure. The American journal of clinical nutrition 1992;55: 343–349. [DOI] [PubMed] [Google Scholar]
- 21.Geiselman PJ, Anderson AM, Dowdy ML, West DB, Redmann SM, Smith SR. Reliability and Validity of a Macronutrient Self-Selection Paradigm and a Food Preference Questionnaire 1. Physiology & behavior 1998;63: 919–928. [DOI] [PubMed] [Google Scholar]
- 22.Blumberg SJ, Bialostosky K, Hamilton WL, Briefel RR. The effectiveness of a short form of the Household Food Security Scale. American journal of public health 1999;89: 1231–1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bengle R, Sinnett S, Johnson T, Johnson MA, Brown A, Lee JS. Food insecurity is associated with cost-related medication non-adherence in community-dwelling, low-income older adults in Georgia. J Nutr Elder 2010;29: 170–191. [DOI] [PubMed] [Google Scholar]
- 24.Goldberg SL, Mawn BE. Predictors of Food Insecurity among Older Adults in the United States. Public health nursing (Boston, Mass) 2015;32: 397–407. [DOI] [PubMed] [Google Scholar]
- 25.Adler NE, Epel ES, Castellazzo G, Ickovics JR. Relationship of subjective and objective social status with psychological and physiological functioning: preliminary data in healthy white women. Health psychology : official journal of the Division of Health Psychology, American Psychological Association 2000;19: 586–592. [DOI] [PubMed] [Google Scholar]
- 26.Goodman E, Adler NE, Kawachi I, Frazier AL, Huang B, Colditz GA. Adolescents’ perceptions of social status: development and evaluation of a new indicator. Pediatrics 2001;108: E31. [DOI] [PubMed] [Google Scholar]
- 27.Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. Journal of psychosomatic research 1985;29: 71–83. [DOI] [PubMed] [Google Scholar]
- 28.Gormally J, Black S, Daston S, Rardin D. The assessment of binge eating severity among obese persons. Addictive behaviors 1982;7: 47–55. [DOI] [PubMed] [Google Scholar]
- 29.Weise CM, Hohenadel MG, Krakoff J, Votruba SB. Body composition and energy expenditure predict ad-libitum food and macronutrient intake in humans. International journal of obesity (2005) 2014;38: 243–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Darmon N, Drewnowski A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutrition reviews 2015;73: 643–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kirkpatrick SI, Tarasuk V. Food insecurity is associated with nutrient inadequacies among Canadian adults and adolescents. The Journal of nutrition 2008;138: 604–612. [DOI] [PubMed] [Google Scholar]
- 32.Kharmats AY, Jones-Smith JC, Cheah YS, Budd N, Flamm L, Cuccia A, et al. Relation between the Supplemental Nutritional Assistance Program cycle and dietary quality in low-income African Americans in Baltimore, Maryland. The American journal of clinical nutrition 2014;99: 1006–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McKenzie DC, Johnson RK, Harvey-Berino J, Gold BC. Impact of interviewer’s body mass index on underreporting energy intake in overweight and obese women. Obesity research 2002;10: 471–477. [DOI] [PubMed] [Google Scholar]
- 34.Bartholome LT, Peterson RE, Raatz SK, Raymond NC. A comparison of the accuracy of self-reported intake with measured intake of a laboratory overeating episode in overweight and obese women with and without binge eating disorder. European journal of nutrition 2013;52: 193–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cardel MI, Johnson SL, Beck J, Dhurandhar E, Keita AD, Tomczik AC, et al. The effects of experimentally manipulated social status on acute eating behavior: A randomized, crossover pilot study. Physiology & behavior 2016;162: 93–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Blundell JE, Caudwell P, Gibbons C, Hopkins M, Naslund E, King N, et al. Role of resting metabolic rate and energy expenditure in hunger and appetite control: a new formulation. Disease models & mechanisms 2012;5: 608–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Caudwell P, Finlayson G, Gibbons C, Hopkins M, King N, Naslund E, et al. Resting metabolic rate is associated with hunger, self-determined meal size, and daily energy intake and may represent a marker for appetite. The American journal of clinical nutrition 2013;97: 7–14. [DOI] [PubMed] [Google Scholar]
- 38.Piaggi P, Thearle MS, Bogardus C, Krakoff J. Lower energy expenditure predicts long-term increases in weight and fat mass. The Journal of clinical endocrinology and metabolism 2013;98: E703-707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Grummon AH, Taillie LS. Nutritional profile of Supplemental Nutrition Assistance Program household food and beverage purchases. The American journal of clinical nutrition 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tarasuk V, Cheng J, de Oliveira C, Dachner N, Gundersen C, Kurdyak P. Association between household food insecurity and annual health care costs. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne 2015;187: E429-436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Drewnowski A, Moudon AV, Jiao J, Aggarwal A, Charreire H, Chaix B. Food environment and socioeconomic status influence obesity rates in Seattle and in Paris. International journal of obesity (2005) 2014;38: 306–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gallo LC, Fortmann AL, de Los Monteros KE, Mills PJ, Barrett-Connor E, Roesch SC, et al. Individual and neighborhood socioeconomic status and inflammation in Mexican American women: what is the role of obesity? Psychosomatic medicine 2012;74: 535–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pfrimer K, Vilela M, Resende CM, Scagliusi FB, Marchini JS, Lima NK, et al. Under-reporting of food intake and body fatness in independent older people: a doubly labelled water study. Age and ageing 2015;44: 103–108. [DOI] [PubMed] [Google Scholar]
- 44.Nettle D, Andrews C, Bateson M. Food insecurity as a driver of obesity in humans: The insurance hypothesis. The Behavioral and brain sciences 2016: 1–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Operario D, Adler NE, Williams DR. Subjective social status: Reliability and predictive utility for global health. Psychology & Health 2004;19: 237–246. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.