Abstract
Antibody therapy has been used to treat a variety of diseases and the success of ZMapp and other monoclonal antibody-based therapies during the 2014–2016 West African Ebola outbreak has shown this countermeasure can be a successful therapy for Ebola hemorrhagic fever. This study utilized transchromosomal bovines (TcB) vaccinated with a DNA plasmid encoding Ebola virus glycoprotein sequence to produce human polyclonal antibodies directed against Ebola virus glycoprotein. When administered 1 day postinfection, these TcB polyclonal antibodies provided partial protection and resulted in a 50% survival rate following a lethal challenge of Ebola virus Makona in rhesus macaques.
Keywords: Ebola virus, transchromosomal bovines (TcB), polyclonal antibodies, protection
The passive transfer of plasma collected from convalescent patients who suffered Ebola hemorrhagic fever (EHF) has been used as a therapy for EHF as far back as 1976 [1, 2]. The 2014–2016 Ebola virus outbreak in west Africa saw an expansion of convalescent plasma treatments with clinical trials occurring in Liberia, Sierra Leone, and Guinea, but little success was measured in these studies [3–6]. Monoclonal antibody (mAb) treatments have since come to the forefront in EHF treatments following the experimental and clinical successes of ZMab, ZMapp, and others [7–10]. Although mAb treatments are promising, a potential downside is that escape mutants may render them ineffective; whereas treatment with polyclonal antibodies (pAbs) could greatly reduce the virus’s ability to mutate and escape based on the sheer number of different epitopes the virus would need to evade. The protective effects of pAbs from filoviruses was illustrated previously when purified immunoglobulin (IgG) isolated from Ebola or Marburg-infected rhesus macaques provided full protection to newly infected animals [11]. The study described here uses pAbs produced and isolated from transchromosomal bovines (TcB) that were genetically engineered to produce human heavy and kappa light-chain immunoglobulin from a human artificial chromosome [12, 13]. These TcB were vaccinated with a eukaryotic expression plasmid containing codon-optimized glycoprotein genes of Sudan virus and Ebola virus (EBOV) to generate fully human pAb IgG [14]. These pAbs were first tested in the BALB/c and IFNAR−/− mouse models of EHF, where they showed a significant increase in survival in both models with treatments occurring 1 day postinfection [14]. In the study reported here, the efficacy of the TcB-generated pAbs were assessed in the rhesus macaque model of EHF with 2 different treatment schemes.
All infectious work was performed in the maximum containment laboratory at the Rocky Mountain Laboratories, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Montana, applying standard operating protocols approved by the Institutional Biosafety Committee. All animal work was approved by the Institutional Animal Care and Use Committee (IACUC) and was performed in strict accordance with the Guide for the Care and Use of Laboratory Animals, Office of Laboratory Animal Welfare, National Institutes of Health and the Animal Welfare Act, United States Department of Agriculture. The pAbs were purified and titered as described previously [14]. TcB pAb treatments were designed according to animal weights and previously established titers [14].
Clinical examinations were performed on days 0, 1, 3, 5, 7, 10, 14, 18, 24, and 31 and included blood sampling for virology and clinical pathology. Hematological analysis was performed with fresh ethylenediaminetetraacetic acid blood using a Procyte Dx analyzer (IDEXX Laboratories) and serum biochemistries were analyzed on a Piccolo Xpress instrument (Abaxis). Changes in hematology and the blood chemistries were evaluated as previously described [15]. Presence of viral RNA and infectious virus titers were assessed as previously described [15]. Blood samples from days 7, 17, 24, and 31 were titered in triplicate with 10-fold serial dilutions on Vero cells using 50% tissue culture infective dose (TCID50) methodologies and the Reed-Muench formula [15]. Animals were monitored and scored twice daily using an IACUC-approved scoring methodology for signs of clinical disease. Animals were euthanized when they reached their clinical endpoint and a full necropsy with histopathology was completed.
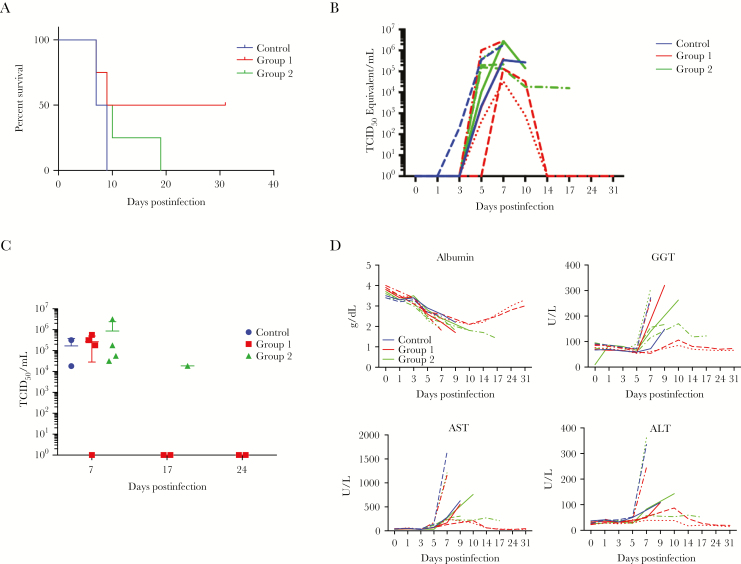
Ten Indian-origin rhesus macaques (Macaca mulatta, ages 2–4 years, weights 3–5 kg) were randomly divided into a control group (n = 2) and 2 treatment groups (n = 4 each). All animals received a lethal dose of 1000 plaque-forming units (pfu) of EBOV Makona (Guinea C07, passage 1). The 2 treatment groups were administered pAb doses composed of 20000 neutralizing antibody units (NAU)/kg intravenously on different days. NAU is defined as the amount of antibody required to neutralize 80% of vesicular stomatitis virus pseudovirions [14].Group 1 received treatments on days 1, 4, 7, and 10 postinfection and group 2 received antibodies on days 2, 5, 8, and 11 days postinfection (Table 1). Control animals received an equivalent amount of unrelated polyclonal antibodies harvested and isolated from the cattle prior to vaccination. One control animal was treated on schedule with group 1 and reached the humane endpoint 9 days postchallenge (Figure 1A). The second control animal was treated on schedule with group 2 and was euthanized on day 7 postchallenge (Figure 1A).
Table 1.
Dosage Groups and Study Design of the 2 Experimental Groups to Treat Ebola Hemorrhagic Fever in Adult Rhesus Macaques
| No. of Animals | Treatment | Schedule, Days | Dosing (NAU/kg) | Survival/Total | |
|---|---|---|---|---|---|
| Group 1 | 1 | Nonspecific TcB pAb | 1,4,7,10 | Equal volume | 0/1 |
| 4 | Anti-EBOV TcB pAb | 1,4,7,10 | 20000 | 2/4 | |
| Group 2 | 1 | Nonspecific TcB pAb | 2,5,8,11 | Equal volume | 0/1 |
| 4 | Anti-EBOV TcB pAb | 2,5,8,11 | 20000 | 0/4 |
All animals were challenged with a previously determined lethal dose of 1000 pfu Ebola virus (strain Makona) via intramuscular injection. Treatments began on day 1 (group 1) or day 2 (group 2) and continued every 3 days until 4 treatments had been administered. Animals were examined daily for clinical signs of disease, and samples were taken for hematology, blood chemistry, and virology analyses at different time points throughout the study beginning on day of virus challenge and ending on day 31 postinfection.
Abbreviations: EBOV, Ebola virus; NAU, neutralizing antibody unit; pfu, plaque-forming unit; TcB pAb, transchromosomal bovine polyclonal antibody.
Figure 1.
The effect of postinfection administration of transchromosomal bovine polyclonal antibodies (TcB pAbs) upon survival in Ebola virus (EBOV)-infected rhesus macaques. Ten rhesus macaques were infected with a lethal dose of EBOV Makona (1000 pfu). One group of 4 animals received treatments on days 1, 4, 7, and 10 postinfection (group 1). A second group of 4 animals received the same treatments of TcB pAbs on days 2, 5, 8, and 11 (group 2). Two animals were used as controls and received nonspecific TcB pAbs on schedule group 1 or group 2. A, Survival of animals in groups 1 and 2, and controls postinfection. B, Viral RNA detected by quantitative polymerase chain reaction from blood samples taken on days 0, 1, 3, 5, 7, 9, 10, 14, 17, 24, and 31 postinfection. The color of each line denotes the treatment group, the style of the line indicates an individual animal within the treatment group. C, Blood samples from all animals analyzed for infectious EBOV titers (50% tissue culture infective dose [TCID50/mL]) on day 7 and from surviving animals on days 17 and 24 postinfection. D, Select blood chemistries from blood samples taken on days 0, 1, 3, 5, 7, 9, 10, 14, 17, 24, and 31 postinfection. The color of each line denotes the treatment group, the style of the line indicates an individual animal within the treatment group. Abbreviations: ALT, alanine transaminase; AST, aspartate transaminase; GGT, γ-glutamyl transferase.
None of the animals from group 2 survived, with 2 animals reaching humane endpoint at day 7, 1 at day 10, and 1 at day 19 postchallenge (Figure 1A). In comparison, 2 animals in group 1 survived EHF; the remaining 2 animals reached the humane endpoint on days 7 and 9 postinfection (Figure 1A).
Viral RNA was detected in all animals beginning on day 5 postinfection and peaked at day 7 when the first animals required euthanasia (Figure 1B). Viral RNA levels were decreased on day 10 in the remaining surviving animals in group 1 and RNA was no longer detectable in either survivor by day 24 postchallenge. The animal in group 2 that survived to day 19 had steady levels of viral RNA on days 10, 14, and 17 before succumbing on day 19 (data not shown). Infectious titers measured on day 7 revealed that all animals had similar levels of viremia except 1, which was 1 of 2 surviving animals from group 1 (Figure 1C). While this animal had detectable levels of viral RNA on day 7, it was approximately a log less than the second survivor and infectious virus was not recovered from the blood. The discrepancy between detectable RNA but lack of infectious virus is likely due to the lower level of virus in this animal as determined by polymerase chain reaction (PCR) and the presence of neutralizing pAbs in the blood. Samples taken on day 17 revealed that both surviving animals from group 1 were no longer viremic but the remaining animal from group 2 maintained a level of viremia greater than 104 TCID50/mL of blood.
Corresponding to the decreasing viremia, blood chemistries measured in both surviving animals from group 1 revealed mild elevation in liver enzymes that occurred later in the disease course (Figure 1D). Total protein and albumin were mildly decreased in all animals at day 3 with more severe decreases in animals that ultimately succumbed. Liver enzymes began returning to baseline levels on day 10 in the 2 surviving animals and by day 14 aspartate transaminase, alanine transaminase, albumin, γ-glutamyl transferase, and blood urea nitrogen levels had all nearly recovered to preinfection levels (Figure 1D and Supplementary Figure 1). Several pAb treated animals exhibited a delay in most parameters measured as compared to the controls but ultimately succumbed to disease. Hematologically, thrombocytopenia was noted among all the animals (Supplementary Figure 1). Similar to the liver enzymes in the 2 surviving animals, the thrombocytopenia improved by day 10 and fully recovered by day 14 (Supplementary Figure 1).
Animals that were euthanized for clinical disease showed typical gross and histopathological lesions of EHF, including hepatic and splenic necrosis, fibrin thrombi within the liver and spleen, and multifocal lymphocytolysis in lymph nodes (Supplementary Table 1). Of note, the prolonged survivor in the second treatment group had orchitis and epididymitis and immunohistochemistry positivity within the testicle, retinal epithelium, and sclera (data not shown).
Although the treatment regimen did not improve the outcome in the second group, the pAbs increased survival from 0% to 50% in the first treatment group, despite a high level of viremia and clinical signs of disease. Disease and viremia resolved quickly following the third treatment (day 7) of pAbs in the surviving animals, with blood parameters returning to baseline within a few days. These results, coupled with those from a similar study that resulted in complete protection from EHF in rhesus macaques when treated with purified pAbs [11], suggest that modifications of the treatment scheme to adjust timing, number of doses, or increasing the amount of pAbs administered could make this a viable therapeutic for EHF.
Antibody therapy through passive transfer of pAbs in serum or produced and purified mAbs have successfully been used to treat several different viral diseases both experimentally and clinically. The list of recent experimental successes includes the Middle East respiratory syndrome and Zika viruses; while human cytomegalovirus, influenza, respiratory syncytial virus, rabies, and Ebola viruses all have antibody therapies in clinical trials [16]. Treatment of EHF with either convalescent plasma or monoclonal antibodies has shown promise both experimentally and clinically but problems persist. Production of convalescent plasma is dependent upon the presence and willingness of an EHF survivor to provide plasma. Antibody therapy as a viable option for the treatment of EHF has been proven by the recent successes of ZMAb and then ZMapp. Both ZMAb and ZMapp are a purified and defined cocktail of 3 EBOV-specific mAbs that were selected on the basis of protection in small animal models. This is in stark contrast to the relatively undefined TcB-generated pAbs used in this study. The nature of the mAb cocktails are advantageous as a defined dose can be administered to a patient. However, there are concerns with mAb therapies as well as they are currently limited by production means and the potential of generating escape mutants could eliminate its effectiveness. TcB-generated pAbs have several advantages over convalescent plasma or monoclonal therapies. Large quantities can be produced relatively easily and pAbs would contain several nonneutralizing and neutralizing antibodies that greatly reduce the potential for escape mutants. The upside of the TcB pAbs and the promising results established in the first treatment group in these studies merits additional studies to further characterize and optimize this potentially lifesaving treatment of EHF.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Financial support. This work was supported by the Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health.
Potential conflicts of interest. E. S., H. W., and J. J. are employees of SAB Biotherapeutics, the company that owns the transchromosomal bovines. All other authors report no potential conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Emond RT, Evans B, Bowen ET, Lloyd G. A case of Ebola virus infection. Br Med J 1977; 2:541–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mupapa K, Massamba M, Kibadi K, et al. Treatment of Ebola hemorrhagic fever with blood transfusions from convalescent patients. International Scientific and Technical Committee. J Infect Dis 1999; 179(Suppl 1):S18–23. [DOI] [PubMed] [Google Scholar]
- 3. Edwards T, Semple MG, De Weggheleire A, et al. ; Ebola_Tx Consortium Design and analysis considerations in the Ebola_Tx trial evaluating convalescent plasma in the treatment of Ebola virus disease in Guinea during the 2014-2015 outbreak. Clin Trials 2016; 13:13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mire CE, Geisbert JB, Agans KN, et al. Passive immunotherapy: assessment of convalescent serum against Ebola virus Makona infection in nonhuman primates. J Infect Dis 2016; 214:367–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. van Griensven J, De Weiggheleire A, Delamou A, et al. The use of Ebola convalescent plasma to treat Ebola virus disease in resource-constrained settings: a perspective from the field. Clin Infect Dis 2016; 62:69–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. van Griensven J, Edwards T, de Lamballerie X, et al. ; Ebola-Tx Consortium Evaluation of convalescent plasma for Ebola virus disease in Guinea. N Engl J Med 2016; 374:33–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Marzi A, Yoshida R, Miyamoto H, et al. Protective efficacy of neutralizing monoclonal antibodies in a nonhuman primate model of Ebola hemorrhagic fever. PLoS One 2012; 7:e36192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Qiu X, Wong G, Audet J, et al. Reversion of advanced Ebola virus disease in nonhuman primates with ZMapp. Nature 2014; 514:47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Qiu X, Audet J, Wong G, et al. Successful treatment of Ebola virus-infected cynomolgus macaques with monoclonal antibodies. Sci Transl Med 2012; 4:138ra81. [DOI] [PubMed] [Google Scholar]
- 10. Olinger GG Jr, Pettitt J, Kim D, et al. Delayed treatment of Ebola virus infection with plant-derived monoclonal antibodies provides protection in rhesus macaques. Proc Natl Acad Sci U S A 2012; 109:18030–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dye JM, Herbert AS, Kuehne AI, et al. Postexposure antibody prophylaxis protects nonhuman primates from filovirus disease. Proc Natl Acad Sci U S A 2012; 109:5034–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sano A, Matsushita H, Wu H, et al. Physiological level production of antigen-specific human immunoglobulin in cloned transchromosomic cattle. PLoS One 2013; 8:e78119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Matsushita H, Sano A, Wu H, et al. Triple immunoglobulin gene knockout transchromosomic cattle: bovine lambda cluster deletion and its effect on fully human polyclonal antibody production. PLoS One 2014; 9:e90383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bounds CE, Kwilas SA, Kuehne AI, et al. Human polyclonal antibodies produced through DNA vaccination of transchromosomal cattle provide mice with post-exposure protection against Lethal Zaire and Sudan Ebolaviruses. PLoS One 2015; 10:e0137786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Marzi A, Hanley PW, Haddock E, Martellaro C, Kobinger G, Feldmann H. Efficacy of vesicular stomatitis virus-Ebola virus postexposure treatment in rhesus macaques infected with Ebola virus Makona. J Infect Dis 2016; 214:360–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Salazar G, Zhang N, Fu TM, An Z. Antibody therapies for the prevention and treatment of viral infections. NPJ Vaccines 2017; 2:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.