Abstract
A recombinant vesicular stomatitis virus (rVSV) expressing the Marburg virus (MARV) Musoke variant glycoprotein fully protects macaques against 2 MARV variants and Ravn virus as a preventive vaccine and MARV variant Musoke as a postexposure treatment. To evaluate postexposure efficacy against the most pathogenic MARV variant, Angola, we engineered rVSVs expressing homologous Angola glycoprotein. Macaques were challenged with high or low doses of variant Angola and treated 20–30 minutes after exposure. A total of 25% and 60%–75% of treated macaques survived the high-dose and low-dose challenges, respectively. The more rapid disease progression of variant Angola versus variant Musoke may account for the incomplete protection observed.
Keywords: Marburg virus, Angola, Musoke, filovirus, recombinant vesicular stomatitis virus, vaccine, treatment
Marburg virus (MARV; species Marburg marburgvirus) and Ebola virus (EBOV; species Zaire ebolavirus) are filoviruses endemic to Africa that cause severe viral hemorrhagic fever (VHF) in humans and nonhuman primates (NHPs). Both viruses are National Institute of Allergy and Infectious Diseases Category A Priority Pathogens and Centers for Disease Control and Prevention Tier 1 select agents, owing to their bioweapon potential, high lethality, and the lack of Food and Drug and Administration–approved vaccines and therapeutics. Sporadic, reoccurring outbreaks of MARV infection (including a recent episode in Uganda and Kenya), the unprecedented 2013–2016 outbreak of EBOV infection in West Africa, with >28000 documented cases, as well as imported cases into Europe and the United States, highlight a need for the development of effective vaccines and therapeutics against these pathogens [1]. Ideally, a vaccine could be used both preventively and as an emergency postexposure treatment.
One of the most promising filovirus vaccine candidates uses a recombinant vesicular stomatitis virus (rVSV) platform. Results from phase 2 and 3 human clinical trials for a rVSV expressing the EBOV glycoprotein (rVSV-EBOV) demonstrated good safety and immunogenicity profiles [2]. Further, no cases of EBOV were recorded in individuals ≥10 days after vaccination in a phase 3 ring vaccination trial in Guinea [3]. This study indicates the usefulness of rVSV vectors for emergency interventions and the rapid immunostimulatory properties of the vaccine. A similar ring immunization strategy could be used during MARV outbreaks.
Most rVSV-based vaccination studies for MARV have been conducted in guinea pigs and NHPs. NHPs are considered the most reliable animal model for recapitulating MARV infection in humans [4]. Previously, a rVSV vaccine expressing the Musoke variant glycoprotein of MARV (rVSV∆G/MARV-Musoke-GP) was reported to fully protect cynomolgus macaques against a lethal, high-dose, 1000–plaque-forming unit (PFU) challenge of MARV Musoke. A single intramuscular injection of the vector elicited strong humoral responses in these animals and was cross-protective against MARV Angola, as well as the closely related Ravn virus [5]. The vaccine also protected monkeys against a 1000-PFU MARV Musoke challenge when administered after exposure to the virus, with survival rates of 100% at 30 minutes [6], 83% at 24 hours [7], and 33% at 48 hours [7].
Although results of these vaccination studies are promising, the effectiveness of rVSV postexposure treatment against the most pathogenic variant, Angola, has not been evaluated. MARV Angola was responsible for one of the worst VHF outbreaks, in 2004–2005 (in Uige Province, Angola), resulting in 252 cases and a 90% case-fatality rate [8]. In animal models, a challenge with the Angola variant results in more-rapid onset of clinical signs in outbred guinea pigs as compared to Ravn virus [9] and in NHPs as compared to other MARV variants [4, 10]. Moreover, livers of Angola variant–infected macaques have more-severe reticulation and paler coloration [10]. To determine the postexposure potential of rVSV against MARV Angola, we engineered 2 rVSV vectors expressing the Angola GP of MARV (rVSV∆G/MARV-Angola-GP and rVSVN4CT1-MARV-Angola-GP) and assessed postexposure efficacy in a rhesus monkey model of MARV disease.
METHODS
Generation of rVSV Vectors
rVSVs were produced from infectious clones as described previously [5, 11]. An expression cassette encoding the full-length Angola GP (MARV-Angola-GP; accession number DQ447653) was cloned into rVSV∆G/MARV-Angola-GP and rVSVN4CT1-MARV-Angola-GP vectors at the native VSV glycoprotein (G) site for rVSV∆G/MARV-Angola-GP and at the first position of the rVSVN4CT1-MARV-Angola-GP genome. rVSVN4CT1-MARV-Angola-GP was attenuated by translocating the VSV nucleoprotein (N) gene from the first to the fourth (N4) genomic position and truncating the VSV G cytoplasmic tail (CT1). The rVSVN4CT1–human immunodeficiency virus (HIV) gag vector similarly expressed an HIV gag gene in the first position. See Supplementary Figure 1 for further clarification. Rescued viruses were purified from infected BHK-21 (CCL-10; ATCC) supernatants by centrifugation on a sucrose-TN cushion. The virus pellets were then suspended in a phosphate-buffered saline solution containing a sucrose phosphate stabilizer, snap frozen in an ethanol/dry ice bath, and stored at −80°C until challenge.
Challenge Virus
The MARV Angola seed stock originated from human serum isolated from an 8-month-old female patient in Uige during the 2005 outbreak (isolate 200501379). Study challenge material is the second Vero E6 cell passage of isolate 200501379, and the titer on Vero E6 is 1.5 × 107 PFU/mL. No mycoplasma was detectable in stocks following polymerase chain reaction (PCR) testing. Endotoxin content was <0.5 EU/mL.
Animal Study Design
Eighteen rhesus monkey (Macaca mulatta) adults (10 females and 8 males), weighing approximately 3.6–7.2 kg, were randomly assigned to 2 experiments. For the high-dose experiment, 5 macaques were challenged by intramuscular injection with a target dose of 1000 PFU of MARV Angola; of these, 4 were treated with rVSV∆G/MARV-Angola-GP, and 1 served as an untreated control. Two historical untreated controls were used to assess the statistical significance of survival for the high-dose challenge group. Thirteen macaques in the low-dose experiment were challenged intramuscularly with a uniformly lethal target dose of 50 PFU of MARV Angola, of which 4 received rVSV∆G/MARV-Angola-GP treatment, 5 received rVSVN4CT1-MARV-Angola-GP treatment, 1 received a nonspecific vector control (rVSVN4CT1-HIVgag), and 3 were left untreated. Treated macaques received a single intramuscular dose of approximately 10 million PFU of a rVSV vector in the left quadriceps near the virus injection site and also in the right quadriceps (the dose was divided equally between the 2 sites) 20–30 minutes after MARV Angola exposure. Actual MARV Angola doses were determined to be 1237 PFU for the high-dose experiment and 51 PFU for the low-dose experiment. Animals were monitored daily for signs of disease according to an internal scoring protocol that measured posture/activity level, behavior, appetite, respiration, and signs of hemorrhagic disease. A clinical score of ≥9 warranted euthanasia. Blood specimens were collected at the time of challenge, at the time of death, and, for surviving animals, 3, 6, 10, 14, 21, and 28 days after challenge. The study end point for surviving animals was day 28 after infection. Tissue specimens were collected at terminal time points for immunohistochemical analysis. The animal studies were performed at the Galveston National Laboratory, University of Texas Medical Branch at Galveston, and were approved by the University of Texas Medical Branch Institutional Animal Care and Use Committee.
Hematologic and Serum Biochemical Analyses
Total white blood cell counts, white blood cell differentials, red blood cell counts, platelet counts, hematocrit values, total hemoglobin concentrations, mean cell volumes, mean corpuscular volumes, and mean corpuscular hemoglobin concentrations were analyzed in blood specimens collected in tubes containing ethylenediaminetetraacetic acid, using a laser based hematologic analyzer (Beckman Coulter). Serum samples were tested for concentrations of albumin, amylase, alanine aminotransferase, aspartate aminotransferase, alkaline phosphatase, gamma-glutamyltransferase, glucose, cholesterol, total protein, blood urea nitrogen, creatinine, uric acid, and C-reactive protein by using a Piccolo point-of-care analyzer and Biochemistry Panel Plus analyzer discs (Abaxis).
Anti-MARV GP Immunoglobulin M (IgM) and Immunoglobulin G (IgG) Enzyme-Linked Immunosorbent Assays (ELISAs)
Sera collected at the indicated time points were tested for MARV Angola GP–specific IgM and IgG antibodies by ELISAs. Flat-bottomed, clear, 96-well plates were coated overnight with 15 ng/well of recombinant MARV Angola GP∆TM (Integrated Biotherapeutics, Gaithersburg, MD) in a sodium carbonate/bicarbonate solution (pH 9.6). Antigen-absorbed wells were subsequently blocked with 4% bovine serum antigen. Sera were initially diluted 1:100, and then 2-fold serial dilutions were performed in antigen-coated wells until a dilution of 1:12800 was achieved. After incubation for 1 hour, wells were washed 6 times and incubated for an hour with a 1:2500 dilution of horseradish peroxidase–conjugated anti-monkey IgM or IgG antibody (Fitzgerald Industries International, Acton, MA). SigmaFast O-phenylenediamine substrate (P9187, Sigma, St. Louis, MO) was added to the wells after 6 additional washes, to develop the colorimetric reaction. The reaction was stopped by adding 3 M sulfuric acid, and absorbances were measured at a wavelength of 492 nm on a spectrophotometer (Molecular Devices Emax system, Sunnyvale, CA). Absorbances were normalized by subtracting values for uncoated wells from values for antigen-coated wells at the corresponding serum dilution. End-point titers were defined as the reciprocal of the last adjusted serum dilution with a value of ≥0.2.
Virus Titration
MARV viremia levels were titrated by a plaque assay on Vero E6 cells, as outlined previously [12].
Quantitative Reverse Transcription PCR (RT-qPCR)
To detect MARV RNA, we targeted the MARV N gene with primer pairs and a 6-carboxyfluorescein–5′-CCCATAAGGT CACCCTCTT-3′–6 carboxytetramethylrhodamine probe as previously reported [12].
Immunohistochemical Analysis
Major organs from macaques were collected during necropsy for immunohistochemical analysis. Tissues were fixed by immersion in 10% neutral buffered formalin, processed, and stained, as described elsewhere [10, 12] .
Serum Neutralization Assay
Neutralization titers were calculated by determining the dilution of serum that reduced 50% of plaques. We incubated a standard 100-PFU amount of MARV with 2-fold serial dilutions of serum samples for 1 hour. The virus-serum mixture was then used to inoculate Vero E6 cells for 60 minutes. Cells were overlaid with a mixture of Eagle’s minimum essential medium and agar and incubated for 6 days, and plaques were counted after 24 hours of staining with 5% neutral red.
Statistical Analyses
Log-rank tests were used to compare survival between treated and control groups (GraphPad Prism software, version 7.0).
RESULTS AND DISCUSSION
Despite the limited amino acid divergence among the glycoproteins of various MARV variants (<7%–8%) [8], we thought the use of a homologous vector would more likely elicit protection against the highly pathogenic MARV Angola. Therefore, we cloned Angola GP into our rVSV vectors (Supplemental Figure 1). Postexposure treatment efficacy was evaluated against high- and low-dose MARV Angola challenges.
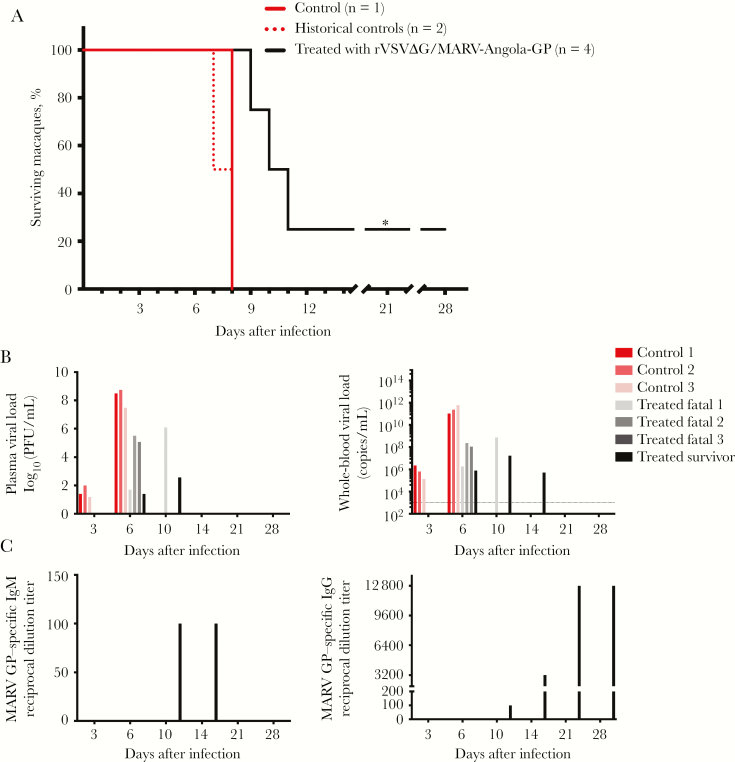
For the high-dose experiment, 7 rhesus macaques (including 2 historical controls) were inoculated intramuscularly with 1000 PFU of MARV Angola. Approximately 20–30 minutes later, 4 of 7 subjects received a single dose of rVSV∆G/MARV-Angola-GP treatment, and 3 were left untreated. Treatment resulted in incomplete protection of monkeys (25% survival; Figure 1A). Untreated controls died on days 7–8, whereas treated animals that did not survive died on days 9–11. Time to death was associated with viral load. For the untreated controls, circulating infectious MARV was detectable 3 days before treated animals (Figure 1B). Terminally, controls had approximately 8 logs of infectious virus in plasma and >1011 MARV RNA copies/mL in whole-blood specimens. In contrast, the viral load was approximately 2–7 logs less in treated animals at this time point. Viremia in the sole survivor cleared by day 21 or was below the detection limit of our plaque and RT-qPCR assays. Only the treated survivor developed MARV GP–specific IgM and IgG, with both immunoglobulin classes appearing at day 10 (Figure 1C). The low anti-MARV IgM titer (1:100) in this animal declined after day 14, conjointly with increased titers (1:12800) of anti-MARV IgG. Only low levels of neutralizing antibody (1:20) were detected in this animal (Supplemental Table 2).
Figure 1.
Postexposure treatment of macaques with a recombinant vesicular stomatitis virus vector expressing the Angola glycoprotein of Marburg virus (rVSV∆G/MARV-Angola-GP) was incompletely protective against a 1000–plaque-forming unit (PFU), high-dose challenge of MARV variant Angola. A, Kaplan-Meier survival curves of treated subjects (solid black line), compared with untreated historical controls (segmented red line) and an untreated control (solid red line). *P ≤ .05 for the difference between the treated group (n = 4) and the control group (n = 3). B, MARV viremia 3, 6, 10, 14, 21, and 28 days after challenge, assessed by plaque assay (left) and quantitative reverse transcription polymerase chain reaction (RT-qPCR) analysis (right). Red and pink bars represent each of the 3 controls, and gray and black bars denote individually treated macaques. The limits of detection are 25 PFU/mL for the plaque assay and 1000 copies/mL for the RT-qPCR assay (dotted line). C, Reciprocal end point dilution titers of anti-MARV GP immunoglobulin M (IgM; left) and immunoglobulin G (IgG; right) in serum specimens obtained from control and treated subjects 3, 6, 10, 14, 21, and 28 days after challenge. Nonsurvivors were serologically negative; therefore, only the treated survivor (black bar) is depicted. Abbreviation: ∆G, VSV in which the native GP is absent.
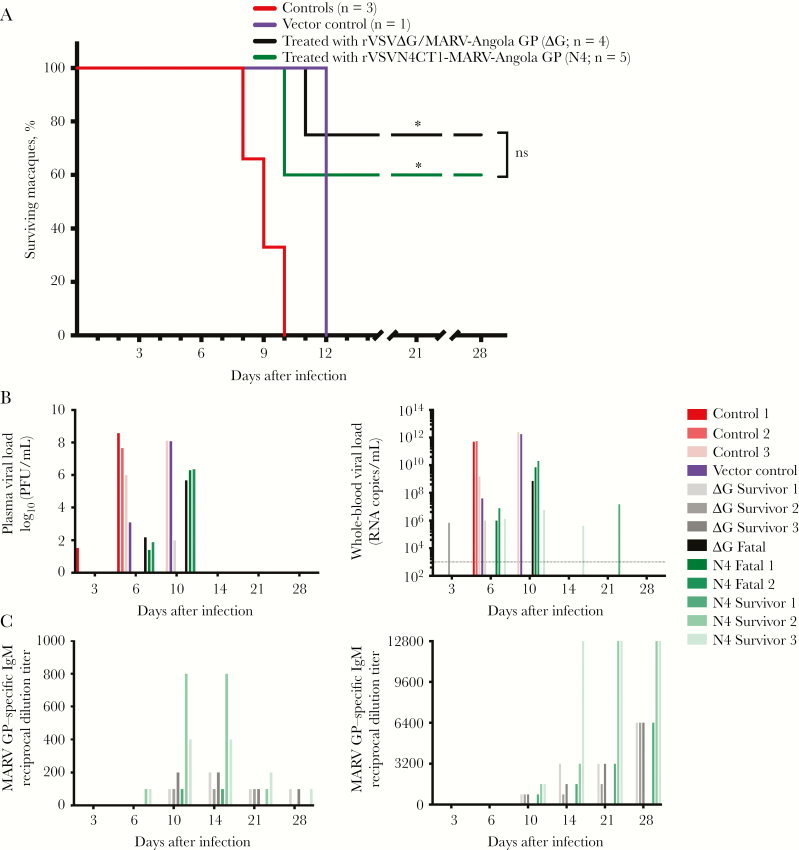
The low-dose experiment involved 13 macaques that were challenged with 50 PFU of MARV Angola and similarly treated as described for the high-dose study. However, in the low-dose experiment, 5 animals received rVSVN4CT1-MARV-Angola-GP (N4), and 4 received rVSV∆G/MARV-Angola-GP (∆G), to assess the effect of vector attenuation on postexposure protection. Additionally, a vector control receiving rVSVN4CT1-HIV gag was included to account for irrelevant, nonspecific effects. The untreated control animals died on days 8–10 and the vector control died on day 12 after virus challenge (Figure 2A). Survival rates were 75% for rVSV∆G/MARV-Angola-GP–treated macaques and 60% for those receiving rVSVN4CT1-MARV-Angola-GP treatment (P = nonsignificant). Similar to the high-dose study, survival correlated with lower viremia levels (Figure 2B) and formation of MARV GP–specific IgM and IgG within 6–10 days after treatment (Figure 2C). Survivors had fewer clinical signs (Supplemental Table 1) and low levels of neutralizing antibody titers (Supplemental Table 2), suggesting antibody-dependent cell-mediated cytotoxicity or complement-mediated lysis involvement. Necropsy findings among nonsurvivors, in conjunction with histopathologic and immunohistochemical findings, were consistent with disease caused by MARV. Antigen was absent in tissue specimens obtained from treated survivors at the study end point (Supplemental Figure 2).
Figure 2.
Postexposure treatment of macaques with recombinant vesicular stomatitis virus vectors expressing the Angola glycoprotein of Marburg virus (rVSV∆G/MARV-Angola-GP or rVSVN4CT1-MARV-Angola-GP) was partially effective against a 50–plaque-forming unit (PFU), low-dose challenge with MARV variant Angola. A, Kaplan-Meier survival curves of the rVSV∆G/MARV-Angola-GP group (black line; n = 4), rVSVN4CT1-MARV-Angola-GP (green line; n = 5), untreated control group (red line; N = 3), and vector control treated with rVSVN4CT1-HIV gag (purple line; n = 1). *P ≤ .05 for the difference between the groups treated with rVSV vectors expressing Angola GP and the untreated control group. Statistical significance was not calculated for the vector control, owing to a lack of biological replicates. B, Plasma and whole blood MARV viral loads on days 3, 6, 10, 14, 21, and 28 days after challenge determined via plaque assay (left panel) and RT-qPCR (right panel), respectively. Individual untreated (red and pink bars), rVSV∆G/MARV-Angola-GP–treated (∆G; gray and black bars), and rVSVN4CT1-MARV-Angola-GP–treated (N4; green bars) subjects, as well as the single vector control (purple bar), are shown. The limits of detection are 25 PFU/mL for the plaque assay and 1000 copies/mL for the RT-qPCR assay (dotted line). C, Reciprocal end point dilution titers of anti-MARV GP immunoglobulin M (IgM; left) and immunoglobulin G (IgG; right) in the serum of individual control (red gradient), vector control (purple), and treated (black and green gradient) subjects. Serological titers were evaluated 3, 6, 10, 14, 21, and 28 days after challenge. The untreated controls, vector control, and treated animals that died were serologically negative for MARV GP–specific IgM and IgG; therefore, only treated survivors are depicted. Abbreviations: CT1, native rVSV GP with a truncated cytoplasmic tail; ∆G, VSV in which the native GP is absent; N4, rVSV nucleoprotein at position 4 in the genome.
Although rVSV vectors remain potent components in prophylactic vaccines, postexposure treatment was only partially (60%–75%) effective against a low-dose, 50-PFU challenge with MARV Angola. Only limited protection (25%) was observed against a high-dose, 1000-PFU challenge in rhesus macaques. The rapid disease course of the Angola variant as compared to the Musoke variant in NHPs may account for our failure to achieve protection against the high-dose challenge. In the rhesus macaque model, the terminal stage of disease for a 1000-PFU intramuscular challenge with MARV Musoke is 10–12 days, compared with 7–9 days for MARV Angola [4, 10]. Lower challenge doses of MARV Angola are known to prolong the disease course in macaques by 1–4 days, depending on the dose and route [13]. For this study, it is possible the combined effect of rVSV treatment and the lower, 50-PFU challenge dose delayed the disease course sufficiently for surviving animals to mount a protective humoral response. This hypothesis is supported by the fact that treated survivors produce MARV GP–specific antibodies, whereas in fatal cases they do not [6, 7]. However, we did not detect a statistically significant difference in times to death between untreated control and rVSV-treated groups with the limited number of animals in this study. Monkeys treated with a nonspecific vector in this and past studies [6, 7] did not survive; therefore, viral interference or stimulation of innate immunity alone might not confer protection. On the contrary, rhesus macaques given 2 doses of a rVSV-based MARV vaccine 1 and 24 hours after infection demonstrated partial protection against a lethal EBOV Makona challenge, suggesting a nonspecific response drives postexposure protection [14]. The number of doses (ie, 2) might explain this difference. Alternatively, these animals may have survived without treatment as EBOV is not uniformly lethal in the rhesus macaque model [4, 15]. A larger vector control group in the future will provide more-meaningful data. More studies are needed to unravel the mechanisms by which rVSV vectors mediate protective immune responses, particularly in the postexposure context.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Acknowledgments. We thank Natalie Dobias, for assistance with tissue preparations, and the University of Texas Medical Branch Animal Resource Center, for husbandry support.
C. B. W, C. E. M., J. H. E., and T. W. G. designed the research; C. B. W., J. B. G., D. M., K. N. A., V. B., R. W. C., D. J. D., K. A. F., C. E. M., and T. W. G. performed the research; C. B. W., J. B. G., D. M., K. N. A., V. B., R. W. C., D. J. D., K. A. F., C. E. M., J. H. E., and T. W. G. analyzed the data; and C. B. W., C. E. M., and T. W. G. wrote the manuscript.
Disclaimer. The opinions, interpretations, conclusions, and recommendations contained herein are those of the authors and are not necessarily reflected by the University of Texas Medical Branch.
Financial support. This work was supported by the National Institutes of Health (grant U19 AI109711 to T. W. G. and J. H. E.).
Potential conflicts of interest. The N4 rVSV vectors described in this manuscript are the subjects of patents licensed to Profectus BioSciences. J. H. E. and T. W. G. claim intellectual property regarding recombinant VSV-based vaccines for the prevention and treatment of filovirus infections. All other authors report no potential conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Presented in part: Keystone Symposia on Hemorrhagic Fever Viruses, Santa Fe, New Mexico, December 2016.
References
- 1. Cross RW, Mire CE, Feldmann H, Geisbert TW. Post-exposure treatments for Ebola and Marburg virus infections. Nat Rev Drug Discov 2018; doi: 10.1038/nrd.2017.251. [DOI] [PubMed] [Google Scholar]
- 2. Kennedy SB, Bolay F, Kieh M, et al. ; PREVAIL I Study Group Phase 2 Placebo-controlled trial of two vaccines to prevent Ebola in Liberia. N Engl J Med 2017; 377:1438–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Henao-Restrepo AM, Camacho A, Longini IM, et al. Efficacy and effectiveness of an rVSV-vectored vaccine in preventing Ebola virus disease: final results from the Guinea ring vaccination, open-label, cluster-randomised trial (Ebola Ça Suffit!). Lancet 2017; 389:505–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Geisbert TW, Strong JE, Feldmann H. Considerations in the use of nonhuman primate models of Ebola virus and Marburg virus infection. J Infect Dis 2015; 212(Suppl 2):S91–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Daddario-DiCaprio KM, Geisbert TW, Geisbert JB, et al. Cross-protection against Marburg virus strains by using a live, attenuated recombinant vaccine. J Virol 2006; 80:9659–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Daddario-DiCaprio KM, Geisbert TW, Ströher U, et al. Postexposure protection against Marburg haemorrhagic fever with recombinant vesicular stomatitis virus vectors in non-human primates: an efficacy assessment. Lancet 2006; 367:1399–404. [DOI] [PubMed] [Google Scholar]
- 7. Geisbert TW, Hensley LE, Geisbert JB, et al. Postexposure treatment of Marburg virus infection. Emerg Infect Dis 2010; 16:1119–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Towner JS, Khristova ML, Sealy TK, et al. Marburgvirus genomics and association with a large hemorrhagic fever outbreak in Angola. J Virol 2006; 80:6497–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cross RW, Fenton KA, Geisbert JB, Ebihara H, Mire CE, Geisbert TW. Comparison of the pathogenesis of the Angola and Ravn strains of Marburg virus in the outbred guinea pig model. J Infect Dis 2015; 212(Suppl 2):S258–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Geisbert TW, Daddario-DiCaprio KM, Geisbert JB, et al. Marburg virus Angola infection of rhesus macaques: pathogenesis and treatment with recombinant nematode anticoagulant protein c2. J Infect Dis 2007; 196(Suppl 2):S372–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Matassov D, Mire CE, Latham T, et al. Single dose trivalent vesiculovax vaccine protects macaques from lethal Ebolavirus and Marburgvirus challenge. J Virol 2017; JVI.01190-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mire CE, Geisbert JB, Borisevich V, et al. Therapeutic treatment of Marburg and Ravn virus infection in nonhuman primates with a human monoclonal antibody. Sci Transl Med 2017; 9:doi: 10.1126/scitranslmed.aai8711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Johnston SC, Lin KL, Twenhafel NA, et al. Dose response of MARV/Angola infection in cynomolgus macaques following IM or aerosol exposure. PLoS One 2015; 10:e0138843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Marzi A, Hanley PW, Haddock E, Martellaro C, Kobinger G, Feldmann H. Efficacy of vesicular Stomatitis virus-Ebola virus postexposure treatment in rhesus macaques infected with Ebola virus makona. J Infect Dis 2016; 214:360–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wong G, Qiu X, de La Vega MA, et al. Pathogenicity comparison between the Kikwit and Makona Ebola virus variants in rhesus macaques. J Infect Dis 2016; 214:281–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.