Abstract
In this study, we investigated immune responses induced by purified Ebola virus (EBOV) soluble glycoprotein (sGP) subunit vaccines via intradermal immunization with microneedle (MN) patches in comparison with intramuscular (IM) injection in mice. Our results showed that MN delivery of EBOV sGP was superior to IM injection in eliciting higher levels and longer lasting antibody responses against EBOV sGP and GP antigens. Moreover, sGP-specific immune responses induced by MN or IM immunizations were effectively augmented by formulating sGP with a saponin-based adjuvant, and they were shown to confer complete protection of mice against lethal mouse-adapted EBOV (MA-EBOV) challenge. In comparison, mice that received sGP without adjuvant by MN or IM immunizations succumbed to lethal MA-EBOV challenge. These results show that immunization with EBOV sGP subunit vaccines with adjuvant by MN patches, which have been shown to provide improved safety and thermal stability, is a promising approach to protect against EBOV infection.
Keywords: Ebola, microneedle patch, soluble GP, vaccine
Ebola hemorrhagic fevers is a severe disease with high fatality rates ranging from 20% to 90% [1]. The 2013–2016 Ebola virus (EBOV) epidemic in West Africa caused more than 28600 human infections and over 11300 deaths, underscoring the urgent need to develop a safe and effective vaccine strategy against EBOV infection [2]. Significant progress has been made on EBOV vaccine development, and a number of approaches have been shown to confer effective protection against EBOV infection in animal models including nonhuman primates (NHPs) [3]. Most notably, a Phase III clinical trial using a recombinant vesicular stomatitis virus-based EBOV vaccine that expresses the EBOV glycoprotein (GP) was conducted at the end of the 2014–2016 EBOV outbreak, and it was shown to be highly effective for protection against EBOV infection [4], demonstrating that an effective vaccine can contribute to the controlling of an EBOV epidemic.
A number of studies evaluating different EBOV vaccine strategies have shown that protection of NHPs mostly correlated with vaccine-induced serum antibody levels against EBOV GP [5, 6], indicating that induction of such responses is critical for protection against EBOV infection. Of note, EBOV GP is synthesized through a ribonucleic acid (RNA)-editing mechanism during virus infection, through joining 2 reading frames in the viral RNA by a slippage of the viral polymerase at an editing site to generate the GP messenger RNA (mRNA) transcript [7–9]. During the process, only approximately 20% of the mRNA transcripts are edited for the synthesis of GP, whereas 80% of transcripts are not edited and direct the synthesis of a soluble GP (sGP) product, which is efficiently secreted from infected cells at large quantities in the form of homodimers [9]. The function of sGP is not clearly understood. Of note, it has been reported that EBOV quickly mutates to synthesize primarily GP in cell culture, whereas such mutant virus reverts to a primarily sGP-producing phenotype in infected animals [10], suggesting an important role for sGP in virus replication within the host. On the other hand, a more recent study showed that synthesis of sGP by EBOV is not required for its virulence in guinea pigs [11]. We have shown that production of sGP may provide a mechanism of immune evasion by EBOV through stimulating production of antibodies that preferentially react with sGP and thereby enabling sGP to absorb such antibodies [12]. Furthermore, overproduction of EBOV GP was shown to decrease the infectivity of EBOV GP pseudoviruses produced from 293T cells [13]. Thus, it may be possible that EBOV produces sGP to evade the host immune defense and control GP levels for enhanced infectivity to spread among its natural hosts. More studies are necessary to delineate the role of sGP in EBOV infection, transmission, and pathogenesis and virulence in different animal species.
Over the past decade, microneedle (MN) patch-based vaccine delivery systems have been investigated for vaccination against a range of different diseases [14, 15]. This novel vaccination technology offers several advantages over conventional intramuscular (IM) injection by hypodermic needles with respect to vaccine stability, reduced pain during immunization, ease of use, and elimination of sharp needles as biohazardous waste [16–19]. In this study, we investigated the immunogenicity of purified EBOV sGP proteins as a subunit vaccine by intradermal immunization using MN patches and by IM injection, and we evaluated the efficacy of protection against lethal EBOV challenge in the mouse model. The present results show that EBOV sGP vaccines can be efficiently coated onto solid metal MN patches, and that immunization by MN patches induced higher levels and longer lasting antibody responses against EBOV GP than IM injection. Furthermore, immunogenicity of EBOV sGP vaccines on MN patches can be effectively augmented by formulating with a saponin-based adjuvant, as similarly observed in IM injections, and confer complete protection against lethal mouse-adapted EBOV (MA-EBOV) challenge in mice.
METHODS
Virus and Biosafety
Mouse-adapted EBOV stock based on the Mayinga strain was propagated in Vero E6 cells and titered by a plaque assay before use for challenge studies [20, 21]. All experiments involving infectious EBOV were performed at the biosafety level 4 (BSL-4) facility at the Texas Biomedical Research Institute.
Cell Lines, Purified Soluble Glycoprotein, Subunit Vaccines, and Adjuvant
HeLa cells, 293T cells, and JC53 cells were maintained in Dulbecco’s modified Eagle’s medium (Mediatech) supplemented with 10% fetal bovine serum (Hyclone, ThermoFisher) and 1% penicillin/streptomycin. Ebola virus sGP (based on the sequence of EBOV Mayinga strain; GenBank accession number NC_002549) was produced using recombinant vaccinia viruses and purified using a histag protein purification system as described previously [12]. The adjuvant, Matrix-M, is a proprietary adjuvant from Novavax, which is produced by formulating purified saponin with cholesterol and phospholipid [22].
Microneedle Patch Preparation and Characterization
Microneedle patches were fabricated from stainless steel sheets by lithographic patterning and chemical etching (Tech Etch, Plymouth, MA). Each MN patch contained a single row of 5 MNs, which are measured to be 700-µm tall, with a cross-sectional area of 170 µm by 55 µm at the base and tapering to a sharp tip. Ebola virus sGP with or without the Matrix-M adjuvant were concentrated by Vivaspin 500 filters (Sartorius) of 30K molecular-weight cutoff at a centrifugal force of 15 000 × g for 30 minutes at 5°C. Concentrated sGP with or without the Matrix-M adjuvant was then diluted (1:1) with the excipient solution (30% w/v trehalose and 2% w/v carboxymethyl cellulose sodium in phosphate-buffered saline [PBS]) and used to coat MNs by a dip-coating process [15].
To measure the amount of vaccine on each MN patch, coated MNs were incubated in 200 µL PBS to dissolve the coating. The solution was then concentrated 10-fold using a protein concentrating column, and 1 µg of total protein was analyzed by sodium dodecyl sulfate polyacrylamide gel electrophoresis followed by Western blot in comparison with different amounts of purified sGP. The amount of sGP on MN patches was further determined by a quantitative enzyme-linked immunosorbent assay (ELISA). In brief, vaccine antigens dissolved from MN patches were serially diluted and then used to coat a 96-well microtiter plate. In parallel, serial dilutions of purified sGP with known concentrations were also coated onto microtiter plates for generation of a standard curve. After coating, the wells were blocked by 5% w/v bovine serum albumin (BSA), and the amount of sGP coated on each well of the plate was determined by ELISA using mouse-anti-GP antibodies (pooled sera from mice that had been vaccinated by EBOV-Mayinga GP deoxyribonucleic acid vaccines) as primary antibodies and horseradish peroxidase (HRP)-conjugated goat-antimouse immunoglobulin G (IgG) antibodies as secondary antibodies. The amount of sGP dissolved from MN patches was then calculated based on the standard curve generated using the purified sGP.
Immunization, Blood Sample Collection, and Challenge of Mice
Eight-week-old female BALB/c mice (Charles River Laboratory) were housed at the Emory University animal facility in microisolator cages. All animal studies were carried out in accordance with relevant guidelines and regulations and approved by the Institutional Animal Care and Use Committees (IACUC) of Emory University, Georgia Institute of Technology, and the Texas Biomedical Research Institute.
Each mouse in each immunization group (5 mice per group) was vaccinated with purified sGP protein (5 µg) with or without Matrix-M adjuvant (5 µg) via MN patches or IM injection. For immunization by MN patches, the hair on the abdominal side of the mouse skin was removed before vaccination by application of depilatory cream (Nair, Church & Dwight). Under anesthesia by ketamine and xylazine, the mouse skin was lightly stretched by hand, and MN patches were pressed into the skin and held in position for 2 minutes. For IM immunization, the same amount antigen was dissolved in 50 µL PBS and injected into the hind legs. Mice (groups of 5) receiving IM injection of 50 µL PBS was used as controls.
For evaluating the protective efficacy against EBOV challenge, mice were shipped to the Texas Biomedical Research Institute and challenged by intraperitoneal injection with 1000 plaque-forming units (pfu) of MA-EBOV in an ABSL-4 facility at 8 weeks after the second immunization. After challenge, mice were monitored for weight changes and signs of disease on a daily basis until day 36 postchallenge. Clinical scores were recorded based on observation of for following symptoms: dyspnea (0–12), recumbency (0–12), responsiveness (0–12), appearance (0–3), eye appearance (0–3), nasal discharge (0–2), feed consumption (0–4), stool (0–1), and fluid intake (0–2), with “0” being normal and higher scores being more severe. Mice with combined clinical scores over 12 were sacrificed by cervical dislocation under anesthesia based on IACUC endpoint. All mice that survived the challenge were sacrificed at the end of the study.
Enzyme-Linked Immunosorbent Assay
Ebola virus sGP or GP-specific antibodies in individual mouse serum samples were measured by ELISA using established protocols [12, 20, 23, 24]. In brief, the assays were performed in a 96-well plate coated overnight at 4°C with purified EBOV sGP or GP proteins at concentration of 1 µg /mL and then blocked with 5% w/v BSA. Serial dilutions of serum samples were incubated at room temperature for 2 hours on coated and blocked ELISA plates, and the bound antibodies were detected with HRP-conjugated goat-antimouse IgG secondary antibodies (Southern Biotechnology Associates), followed by addition of tetramethylbenzidine (Sigma), and then by determination of absorbance values at 450 nm by an ELISA reader. A standard curve (1) was constructed by coating each ELISA plate with serial 3-fold dilutions of purified mouse IgG antibodies with known concentrations and (2) used to determine the concentrations of sGP or GP-specific antibodies in serum samples that were expressed as the mass (nanogram) of antigen-specific antibodies per volume (milliliter) of serum sample.
Pseudovirion Neutralization Assay
Neutralizing activity of sera from vaccinated mice was analyzed against pseudoviruses containing EBOV-Mayinga GP based on a human immunodeficiency virus backbone as described in previous studies [12, 23]. In brief, pseudoviruses were preincubated with serial 3-fold dilutions of heat-inactivated serum samples from each individual mouse and supplemented with heat-inactivated naive mouse sera (Innovative Research) so that 5% of the total volume was mouse serum. Pseudovirus-serum mixtures were then added to 50% confluent JC53 cells and incubated for 48 hours. Pseudovirus infection and neutralization was measured by a luciferase reporter assay, and neutralizing activity was expressed as the percentage reduction of luciferase activity in sample wells, compared with luciferase activities in control wells with only naive mouse sera: [(luciferase activity in control well-luciferase activity in sample well)/(luciferase activity in control well)] × 100%.
Statistics
The statistical significance for antibody levels and neutralizing activities between different groups was calculated by a 2-tailed unpaired t test, and P≤.05 was considered significant. Statistical analysis of Kaplan-Meier survival curves was done by log-rank analysis, and P≤.05 was considered significant.
RESULTS
Production of Microneedle Patches Coated With Purified Ebola Virus Soluble Glycoproteins Subunit Vaccines
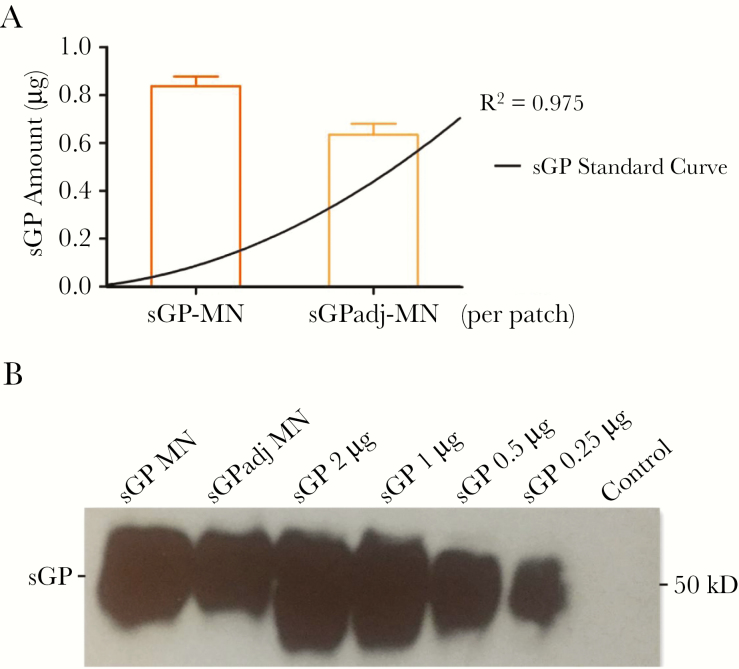
To investigate the immunogenicity of purified EBOV sGP by intradermal immunization, we coated sGP onto solid, stainless steel MN patches, which involves a simple fabrication process and has been shown to be effective for intradermal delivery of influenza vaccines in our previous studies [15]. Two batches of MNs were produced. One batch was coated with purified EBOV sGP alone and designated as sGP-MN. The other batch was coated with purified EBOV sGP in formulation with an adjuvant, Matrix-M, and designated as sGPadj-MN. Matrix-M is a saponin-based immune adjuvant and has been shown to be highly active in augmenting induction of immune responses by an EBOV GP subunit vaccine by IM injection [22]. After fabrication and antigen coating, 5 MN patches were randomly selected, and the quantity of GP coated onto MN patches was determined by a quantitative ELISA. As shown in Figure 1A, sGPadj-MN contained approximately 0.63 µg of sGP per patch, whereas sGP-MN contained approximately 0.82 µg of sGP per patch. The amount of sGP on each MN patch varied by less than 5% for both sGPadj-MN and sGP-MN patches. Furthermore, sGP extracted from sGPadj-MN and sGP-MN patches showed migration patterns in Western blot analysis similar to untreated purified sGP proteins (Figure 1B). These results indicate that sGP subunit vaccines with or without the Matrix-M adjuvant were coated onto MN patches at similar efficiencies without degradation or damage in molecule integrity.
Figure 1.
Characterization of soluble glycoprotein (sGP) vaccines on microneedle (MN) patches. Purified Ebola virus (EBOV) sGP subunit vaccine was coated onto MN patches as described in Materials and Methods. Five patches were randomly selected from the production batch, and sGP proteins were dissolved from MN patches by incubating the MN patches in 200 µL phosphate-buffered saline, to determine the amount of sGP from each MN patch by a quantitative enzyme-linked immunosorbent assay (ELISA) and to examine sGP molecular integrity by Western blot. (A) Quantitative ELISA. Ebola virus sGP proteins dissolved from each GP-MN were serially diluted and coated onto the wells of a 96-well plate in triplicate. Serial dilutions of purified sGP were also coated onto the wells of the 96-well plate at known concentrations to generate a standard curve. The amount of sGP dissolved from sGP-MN and sGPadj-MN was determined by ELISA based on the standard curve generated with purified sGP with known concentrations. (B) Western blot. Ebola virus sGP proteins dissolved from sGP-MN and sGPafj-MN were concentrated, and the protein concentration was determined by a bicinchoninic acid assay. The dissolved sGP proteins (1 µg) were analyzed by sodium dodecyl sulfate polyacrylamide gel electrophoresis and Western blot in comparison with 2, 1, 0.5, and 0.25 µg of purified sGP.
Microneedle Patch Delivery of Ebola Virus Soluble Glycoproteins Induces Stronger Antibody Responses Than Intramuscular Injection
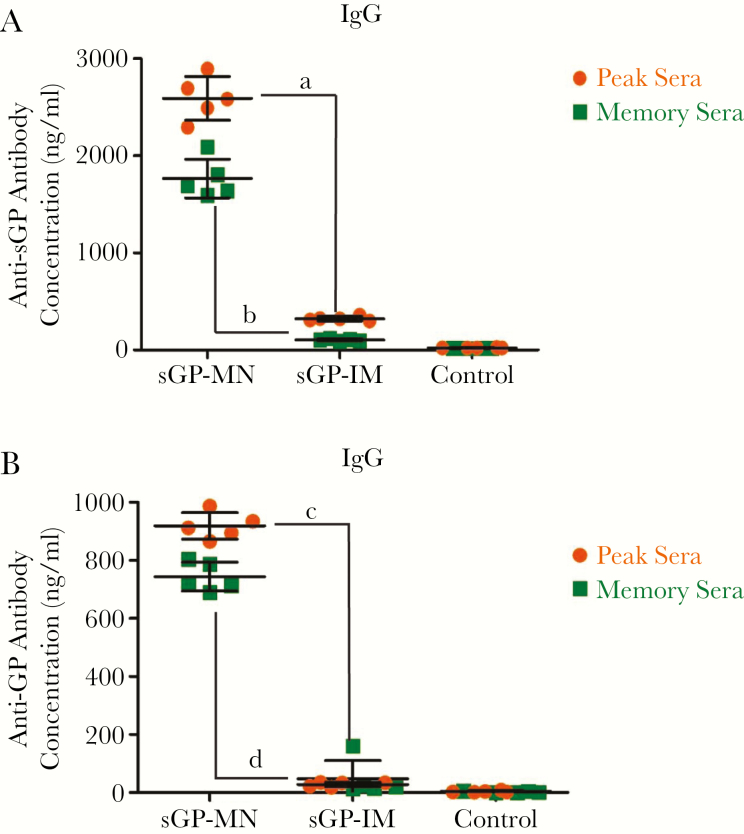
We first investigated the immunogenicity of sGP vaccines coated onto MNs (sGP-MN) in comparison with IM injection of sGP vaccines (sGP-IM) at the same dose. As shown in Figure 2A, immunization by IM injection of sGP (sGP-IM) only induced low levels of antibodies (approximately 300 ng/mL on average) against EBOV sGP 2 weeks after the second immunization. In comparison, intradermal immunization by MNs (sGP-MN) induced approximately 8-fold higher levels of antibodies (approximately 2500 ng/mL on average) against sGP compared with IM injection (P < .01). Moreover, analysis of blood samples collected from vaccinated mice at 16 weeks after the second immunization showed that the level of antibody responses against sGP induced by sGP-MN immunization remained to be higher than sGP-IM immunization at this time point (P < .01). As shown in Figure 2A, antibody levels against sGP in sera from sGP-MN vaccinated mice remained at high levels (approximately 1800 ng/mL on average) in the memory phase (week 16), dropping only by approximately 30% from peak levels (week 6). In comparison, antibody levels against sGP in mice vaccinated by IM injection (sGP-IM) dropped by approximately 3-fold (approximately 100 ng/mL on average) over the same period of time. Similar results were also obtained for antibody responses against EBOV GP (Figure 2B), although the levels of antibody responses against GP were relatively lower compared with the levels of antibody responses against sGP. Of note, sGP-IM immunization only induced very low levels of antibody responses against EBOV GP at 2 weeks after the second immunization (week 6), which remained at low levels at week 16. These results showed that MN delivery of sGP is superior to the conventional IM injection in eliciting higher levels and longer lasting antibody responses against the vaccine antigen sGP as well as the EBOV GP antigen.
Figure 2.
Comparison of antibody responses induced by soluble glycoprotein (sGP)-microneedle (MN) patches and sGP-intramuscular (IM) immunizations. Mice (groups of 5) were vaccinated by MN patch delivery (sGP-MN) or IM injection (sGP-IM) of 5 µg sGP vaccines twice at 4-week intervals. The control group mice received IM injection of 50 µL phosphate-buffered saline. The peak serum samples were collected at 2 weeks after the second immunization, and the memory serum samples were collected at 16 weeks after the second immunization. (A) The levels of sGP-specific immunoglobulin G (IgG) antibodies were determined by enzyme-linked immunosorbent assay (ELISA) using purified sGP as coating antigen. (B) The levels of GP-specific IgG antibodies were determined by ELISA using purified GP as coating antigen. The antibody concentration was determined from a standard curve and expressed as ng/ml. Statistical analysis for differences in antibody responses against sGP and GP between indicated groups (denoted by “a” through “d”) were done by a a 2-tailed unpaired t test. a, sGP-MN vs sGP-IM (peak sera against sGP), P = .0001; b, sGP-MN vs sGP-IM (memory sera against sGP), P = .0001; c, sGP-MN vs sGP-IM (peak sera against GP), P = .0001; d, sGP-MN vs sGP-IM (memory sera against GP), P = .0001.
Microneedle Patch Delivery of Adjuvanted Soluble Glycoproteins Subunit Vaccines Augments Induction of Antibody Responses
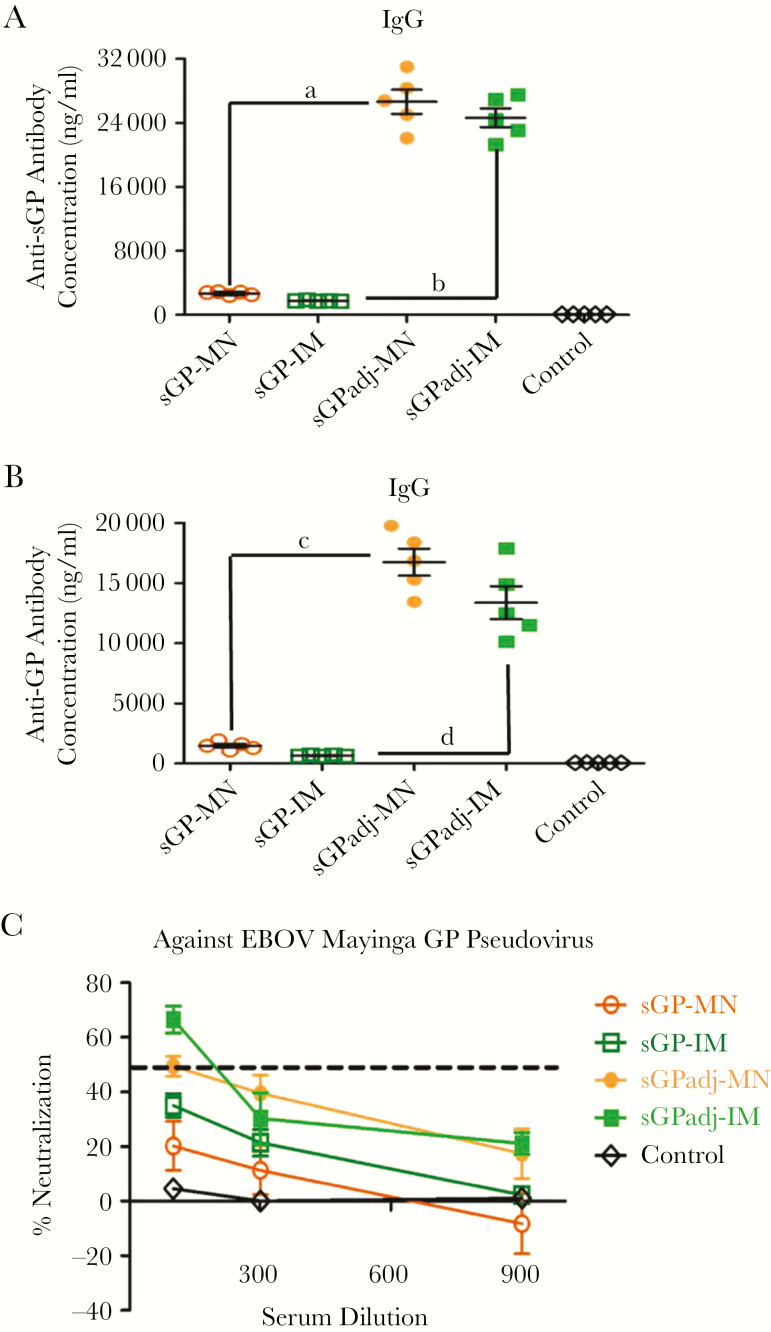
We further investigated whether immune responses induced by sGP subunit vaccines via MN delivery or IM injection can be augmented by an adjuvant, Matrix-M, a saponin-based ISCOMATRIX adjuvant [22]. Mice (groups of 5) were vaccinated by sGPadj-MN and sGP-MN vaccines or by IM injection of sGP vaccines with (sGPadj-IM) or without (sGP-IM) the Matrix-M adjuvant twice at 4-week intervals. Blood samples were collected at 2 weeks after the second immunization and analyzed for antibody responses against EBOV sGP and GP antigens. As shown in Figure 3A, immunization with adjuvanted sGP vaccines by MN (sGPadj-MN) or IM (sGPadj-IM) greatly augmented induction of antibodies against the sGP antigen, to levels over 25 000 ng/mL on average. In comparison, immunization with unadjuvanted sGP vaccines by MN (sGP-MN) or IM (sGP-IM) induced approximately 2000 and 1000 ng/mL antibodies against sGP on average, which are 10- to 20-fold lower compared with the antibody levels induced by sGPadj-MN and sGPadj-IM immunizations, respectively (P < .01). Analysis of antibody responses against EBOV GP produced similar results. As shown in Figure 3B, immunization with sGPadj-MN or sGPadj-IM induced approximately 17 000 and 13 000 ng/mL antibodies on average against GP, respectively, which are significantly higher than the levels of antibodies against GP induced by immunization with sGP-MN or sGP-IM (P < .01).
Figure 3.
Analysis of antibody responses induced by microneedle (MN) patch or intramuscular (IM) delivery of soluble glycoprotein (sGP) with or without Matrix-M adjuvant. Mice (groups of 5) were vaccinated twice at 4-week intervals by MN patch delivery (sGPadj-MN) or IM injection (sGPadj-IM) of sGP in formulation with Matrix-M or by MN patch delivery (sGP-MN) or IM injection (sGP-IM) of the same amount (5 µg) unadjuvanted sGP. The control group received IM injection of 50 µL phosphate-buffered saline. Serum samples were collected at 2 weeks after the second immunization. (A) The levels of sGP-specific immunoglobulin G (IgG) antibodies were determined by enzyme-linked immunosorbent assay (ELISA) using purified sGP as coating antigen. (B) The levels of GP-specific IgG antibodies were determined by ELISA using purified GP as coating antigen. The antibody concentration was determined from a standard curve and expressed as ng/ml. Statistical analysis for differences in antibody responses against sGP and GP between indicated groups (denoted by “a” through “d”) were done by a a 2-tailed unpaired t test. a, sGPadj-MN vs sGP-MN (against sGP), P = .0001; b, sGPadj-IM vs sGP-IM (against sGP), P = .0001; c, sGPadj-MN vs sGP-MN (against GP), P = .0001; d, sGPadj-IM vs sGP-IM (against GP), P = .0001. (C) Neutralizing activity of sera was determined by incubating 500 plaque-forming units of Mayinga Ebola virus GP pseudoviruses with serial 3-fold dilutions of serum samples from each vaccinated mouse. Neutralization was measured as percentage decrease in luciferase expression compared with virus-naive mouse sera controls.
Serum samples from vaccinated mice were further analyzed for their neutralizing activity against EBOV GP pseudoviruses. As shown in Figure 3C, sera from mice immunized with adjuvanted sGP vaccines by MN (sGPadj-MN) or IM (sGPadj-IM) neutralized approximately 50% or 65% of EBOV GP pseudoviruses, respectively, at 1:100 serum dilution. In comparison, sera from mice immunized with unadjuvanted sGP vaccines by sGP-MN or sGP-IM failed to neutralize over 50% of EBOV GP pseudoviruses at 1:100 serum dilution. These results showed that formulation with the Matrix-M adjuvant also augmented induction of neutralizing antibodies by sGP vaccines, but only to low levels.
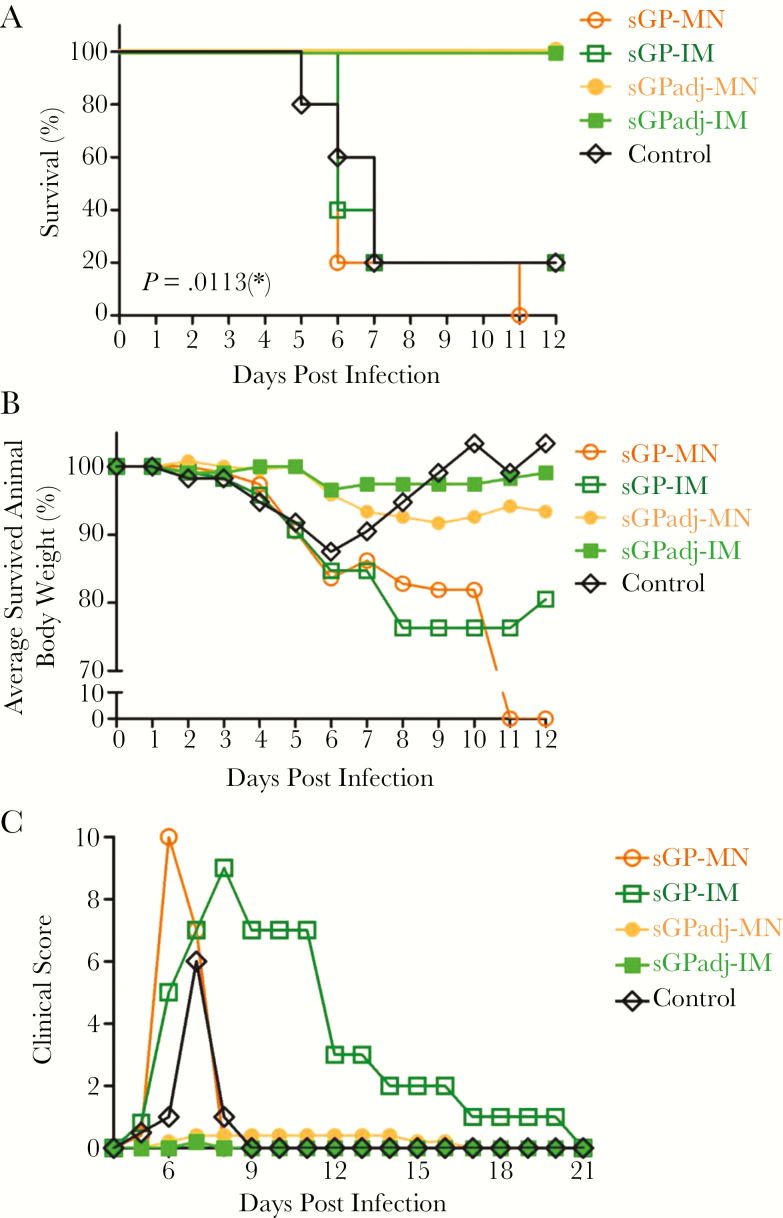
Immunization With Adjuvanted Soluble Glycoproteins Vaccines by Microneedle Patches or Intramuscular Injection Confers Effective Protection Against Lethal Mouse-Adapted Ebola Virus Challenge
To compare the protective efficacy of different immunization approaches against EBOV infection, vaccinated mice were challenged at 8 weeks after the second immunization with 1000 pfu of MA-EBOV and monitored daily for 36 days after challenge to record weight changes, disease symptoms, and survival rates. As shown in Figure 4A, only 1 of 5 mice in the sGP-IM group survived the challenge, similar to the control group that received IM injection of PBS, and none of the 5 mice in the sGP-MN group survived the challenge. On the other hand, all mice in the sGPadj-MN group and the sGPadj-IM group that were vaccinated with adjuvanted sGP vaccines survived the challenge. Log-rank analysis of the survival curves showed that the differences in survival rates between these groups are statistically significant (P = .0013). Furthermore, a progressive loss in average body weight of surviving mice was observed for the control, the sGP-MN, and the sGP-IM groups, correlating with the timing of animal deaths in each group (Figure 4B). In comparison, no significant body weight change was detected for the sGPadj-MN and sGPadj-IM groups. Moreover, as shown in Figure 4C, the clinical scores for the control group, the sGP-MN group, and the sGP-IM group increased drastically on day 5 after challenge. In comparison, the clinical scores remained at baseline levels throughout the duration of the challenge in the sGPadj-MN and sGP-adj-IM groups. These results show that immunization with sGP vaccines in formulation with the Matrix-M adjuvant by MNs or by IM injection was able to confer complete protection against death and disease caused by MA-EBOV infection.
Figure 4.
Protective efficacy against lethal mouse-adapted Ebola virus (MA-EBOV) challenge. Mice (groups of 5) were vaccinated twice at 4-week intervals by microneedle (MN) patch delivery (sGPadj-MN) or intramuscular (IM) injection (sGPadj-IM) of soluble glycoprotein (sGP) in formulation with Matrix-M or by MN patch delivery (sGP-MN) or IM injection (sGP-IM) of the same amount (5 µg) unadjuvanted sGP. The control mice received IM injection of phosphate-buffered saline. At 8 weeks after the second immunization, mice were challenged by intraperitoneal injection with 1000 plaque-forming units of MA-EBOV and monitored daily for survival, body weight changes, and disease symptoms. (A) Daily survival rate of mice in each group postchallenge. Statistical analysis of the Kaplan-Meier survival curves after challenge was conducted by log-rank analysis (P = .0113). (B) Average body weight of surviving mice in each group were determined daily postchallenge and expressed as the percentage of the average body weight of the same group of mice on day 0 of challenge. (C) Average daily clinical scores of surviving mice in each group postchallenge. Clinical scores were recorded as described in Methods.
DISCUSSION
The present results show that intradermal immunization by MN patch delivery of purified EBOV sGP subunit vaccines was able to induce higher levels of antibody responses against EBOV sGP as well as GP antigens than the conventional IM immunization approach. Moreover, the immune responses induced by MN vaccination were found to be substantially augmented by formulating sGP vaccines with an adjuvant and confer highly effective protection against lethal MA-EBOV challenge, as also observed in IM immunization of sGP with adjuvant.
Currently, vaccinations are commonly administered via IM or subcutaneous injection of vaccines, which are prepared in solution and need to be stored under frozen or refrigerated conditions to maintain their stability. In comparison, MN patches deliver vaccines intradermally in a dry form, and they have been shown to offer improved vaccine thermal stability in previous studies [25]. We and others have previously demonstrated that intradermal delivery of influenza vaccines using solid metal MNs or dissolving MNs have the ability to (1) generate potent and effective immune responses equivalent or superior to IM injection and (2) protect vaccinated animals against lethal challenge by influenza viruses [18, 19]. More recently, results from a Phase I clinical trial of influenza vaccines showed that MN immunization was able to induce robust immune responses in humans that are at least equivalent to IM immunization and exhibited an excellent safety profile [26]. Moreover, the influenza vaccines in MN patches were shown to retain their antigenicity and potency after storage at elevated temperatures for up to 12 months, demonstrating the potential to eliminate the cold-chain requirement for vaccine storage and transportation by this technology.
We also observed that sGP subunit vaccines in formulation with an adjuvant, Matrix-M, can also be efficiently coated onto solid metal MN patches at levels comparable to sGP alone. Matrix-M is a saponin-based adjuvant that exerts its adjuvant activity through activation of dendritic cells and macrophages and recruitment of these cells to the draining lymph nodes [27], and it has been shown to be highly effective for augmenting induction of immune responses by various subunit vaccines via IM injection in both animal models and human clinical trials [28, 29]. Furthermore, the Matrix-M adjuvant has been shown to effectively augment immune responses induced by IM immunization with an EBOV GP nanoparticle vaccine [22]. We found that Matrix-M retains its adjuvant activity when coated on MN patches, and it is as effective to augment induction of antibodies in MN immunization as in IM immunization. Moreover, our results showed that mice vaccinated with adjuvanted sGP vaccines by either MN vaccination or IM injection were effectively protected against both morbidity and mortality after MA-EBOV challenge.
CONCLUSIONS
Current EBOV vaccines mostly target the viral GP antigen. Of particular note, recent studies have shown that subunit vaccines based on the whole GP or the entire extracellular domain of GP were able to protect vaccinated mice against lethal EBOV challenge [22, 30]. Our results in this study show that immunization by sGP subunit vaccines could also confer effective protection against lethal EBOV challenge of mice. Compared with the whole EBOV GP, the sGP is devoid of the entire mucin-like domain and the GP2 subunit, and thus missing some of the targets in GP for antibody responses. On the other hand, antibody responses induced by sGP vaccines may be more effectively boosted by the large amount of sGP produced and secreted during virus infection [12] and thereby contribute to more effective control of virus replication. Furthermore, its shared sequence with GP encompasses the putative receptor binding domain that binds to NPC-1 for mediating interactions between viral and cellular membranes during virus infection [31], and it is relatively more conserved amongst different Ebolavirus species than the mucin-like domain in GP. Moreover, EBOV sGP is efficiently secreted from cells after synthesis, and thus it is easy to produce and purify at large quantities. Taken together, MN patch delivery of sGP subunit vaccines may represent an attractive approach for EBOV vaccine development, offering enhanced immunogenicity and the potential to overcome the cold-chain requirement for vaccine storage and distribution. Further optimization of this novel vaccine delivery platform with respect to vaccine-adjuvant formulation and MN production will provide a novel approach to develop a safe, effective, and thermally stable vaccine against EBOV as well as other filoviruses.
Notes
Financial support. This work was supported in part by funding from the National Institute of Allergy and Infectious Diseases (grant AI093406) and the China Scholarship Council (to Y. L.).
Potential conflicts of interest. M. R. P. is an inventor of patents licensed to companies developing microneedle-based products, a paid advisor to companies developing microneedle-based products, and a founder/shareholder of companies developing microneedle-based products (Micron Biomedical). This potential conflict of interest has been disclosed and is managed by Georgia Tech and Emory University. Authors from Novavax, Inc. (D. F., G. G., and G. S.) are current or past employees of for-profit organizations and own stock or hold stock options. G. S. has submitted a pending patent applications related to the work. These interests do not alter the author’s adherence to policies on sharing data and materials. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Presented in part: 9th International Symposium on Filoviruses, September 13–17, 2017, Marburg, Germany.
References
- 1. Towner JS, Sealy TK, Khristova ML et al. . Newly discovered ebola virus associated with hemorrhagic fever outbreak in Uganda. PLoS Pathog 2008; 4:e1000212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lambe T, Bowyer G, Ewer KJ. A review of Phase I trials of Ebola virus vaccines: what can we learn from the race to develop novel vaccines?Philos Trans R Soc Lond B Biol Sci 2017; 372: pii:20160295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Keshwara R, Johnson RF, Schnell MJ. Toward an effective Ebola virus vaccine. Annu Rev Med 2017; 68:371–86. [DOI] [PubMed] [Google Scholar]
- 4. Henao-Restrepo AM, Longini IM, Egger M et al. . Efficacy and effectiveness of an rVSV-vectored vaccine expressing Ebola surface glycoprotein: interim results from the Guinea ring vaccination cluster-randomised trial. Lancet 2015; 386:857–66. [DOI] [PubMed] [Google Scholar]
- 5. Marzi A, Engelmann F, Feldmann F et al. . Antibodies are necessary for rVSV/ZEBOV-GP-mediated protection against lethal Ebola virus challenge in nonhuman primates. Proc Natl Acad Sci U S A 2013; 110:1893–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wong G, Richardson JS, Pillet S et al. . Immune parameters correlate with protection against ebola virus infection in rodents and nonhuman primates. Sci Transl Med 2012; 4:158ra46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sanchez A, Trappier SG, Mahy BW, Peters CJ, Nichol ST. The virion glycoproteins of Ebola viruses are encoded in two reading frames and are expressed through transcriptional editing. Proc Natl Acad Sci U S A 1996; 93:3602–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Volchkov VE, Becker S, Volchkova VA et al. . GP mRNA of Ebola virus is edited by the Ebola virus polymerase and by T7 and vaccinia virus polymerases. Virology 1995; 214:421–30. [DOI] [PubMed] [Google Scholar]
- 9. Volchkov VE, Volchkova VA, Slenczka W, Klenk HD, Feldmann H. Release of viral glycoproteins during Ebola virus infection. Virology 1998; 245:110–9. [DOI] [PubMed] [Google Scholar]
- 10. Volchkova VA, Dolnik O, Martinez MJ, Reynard O, Volchkov VE. Genomic RNA editing and its impact on Ebola virus adaptation during serial passages in cell culture and infection of Guinea pigs. J Infect Dis 2011; 204:S941–6. [DOI] [PubMed] [Google Scholar]
- 11. Hoenen T, Marzi A, Scott DP et al. . Soluble glycoprotein is not required for Ebola virus virulence in Guinea pigs. J Infect Dis 2015; 212:S242–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mohan GS, Li W, Ye L, Compans RW, Yang C. Antigenic subversion: a novel mechanism of host immune evasion by Ebola virus. PLoS Pathog 2012; 8:e1003065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mohan GS, Ye L, Li W et al. . Less is more: Ebola virus surface glycoprotein expression levels regulate virus production and infectivity. J Virol 2015; 89:1205–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Matsuo K, Okamoto H, Kawai Y et al. . Vaccine efficacy of transcutaneous immunization with amyloid β using a dissolving microneedle array in a mouse model of Alzheimer’s disease. J Neuroimmunol 2014; 266:1–11. [DOI] [PubMed] [Google Scholar]
- 15. Zhu Q, Zarnitsyn VG, Ye L et al. . Immunization by vaccine-coated microneedle arrays protects against lethal influenza virus challenge. Proc Natl Acad Sci U S A 2009; 106:7968–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Prausnitz MR. Engineering microneedle patches for vaccination and drug delivery to skin. Annu Rev Chem Biomol Eng 2017; 8:177–200. [DOI] [PubMed] [Google Scholar]
- 17. Shin CI, Jeong SD, Rejinold NS, Kim YC. Microneedles for vaccine delivery: challenges and future perspectives. Ther Deliv 2017; 8:447–60. [DOI] [PubMed] [Google Scholar]
- 18. Leone M, Mönkäre J, Bouwstra JA, Kersten G. Dissolving microneedle patches for dermal vaccination. Pharm Res 2017; 34:2223–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Marshall S, Sahm LJ, Moore AC. The success of microneedle-mediated vaccine delivery into skin. Hum Vaccin Immunother 2016; 12:2975–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sun Y, Carrion R Jr, Ye L et al. . Protection against lethal challenge by Ebola virus-like particles produced in insect cells. Virology 2009; 383:12–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bray M, Davis K, Geisbert T, Schmaljohn C, Huggins J. A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J Infect Dis 1999; 179:S248–58. [DOI] [PubMed] [Google Scholar]
- 22. Bengtsson KL, Song H, Stertman L et al. . Matrix-M adjuvant enhances antibody, cellular and protective immune responses of a Zaire Ebola/Makona virus glycoprotein (GP) nanoparticle vaccine in mice. Vaccine 2016; 34:1927–35. [DOI] [PubMed] [Google Scholar]
- 23. Ye L, Lin J, Sun Y et al. . Ebola virus-like particles produced in insect cells exhibit dendritic cell stimulating activity and induce neutralizing antibodies. Virology 2006; 351:260–70. [DOI] [PubMed] [Google Scholar]
- 24. Li W, Ye L, Carrion R Jr et al. . Characterization of immune responses induced by Ebola virus glycoprotein (GP) and truncated GP isoform DNA vaccines and protection against lethal Ebola virus challenge in mice. J Infect Dis 2015; 212:S398–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chu LY, Ye L, Dong K, Compans RW, Yang C, Prausnitz MR. Enhanced stability of inactivated influenza vaccine encapsulated in dissolving microneedle patches. Pharm Res 2016; 33:868–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rouphael NG, Paine M, Mosley R et al. . The safety, immunogenicity, and acceptability of inactivated influenza vaccine delivered by microneedle patch (TIV-MNP 2015): a randomised, partly blinded, placebo-controlled, phase 1 trial. Lancet 2017; 390:649–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Magnusson SE, Reimer JM, Karlsson KH, Lilja L, Bengtsson KL, Stertman L. Immune enhancing properties of the novel Matrix-M™ adjuvant leads to potentiated immune responses to an influenza vaccine in mice. Vaccine 2013; 31:1725–33. [DOI] [PubMed] [Google Scholar]
- 28. Morelli AB, Becher D, Koernig S, Silva A, Drane D, Maraskovsky E. ISCOMATRIX: a novel adjuvant for use in prophylactic and therapeutic vaccines against infectious diseases. J Med Microbiol 2012; 61:935–43. [DOI] [PubMed] [Google Scholar]
- 29. Drane D, Gittleson C, Boyle J, Maraskovsky E. ISCOMATRIX adjuvant for prophylactic and therapeutic vaccines. Expert Rev Vaccines 2007; 6:761–72. [DOI] [PubMed] [Google Scholar]
- 30. Lehrer AT, Wong TS, Lieberman MM et al. . Recombinant proteins of Zaire ebolavirus induce potent humoral and cellular immune responses and protect against live virus infection in mice. Vaccine 2018; 36:3090–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Miller EH, Obernosterer G, Raaben M et al. . Ebola virus entry requires the host-programmed recognition of an intracellular receptor. EMBO J 2012; 31:1947–60. [DOI] [PMC free article] [PubMed] [Google Scholar]