Abstract
Marburg virus (MARV; family Filoviridae) causes sporadic outbreaks of Marburg hemorrhagic fever in sub-Saharan Africa with case fatality rates reaching 90%. Wild-type filoviruses, including MARV and the closely related Ebola virus, are unable to suppress the type I interferon response in rodents, and therefore require adaptation of the viruses to cause disease in immunocompetent animals. In the current study, we demonstrate that STAT2 knockout Syrian hamsters are susceptible to infection with different wild-type MARV variants. MARV Musoke causes a robust and systemic infection resulting in lethal disease. Histopathological findings share features similar to those observed in human patients and other animal models of filovirus infection. Reverse-transcription polymerase chain reaction analysis of host transcripts shows a dysregulation of the innate immune response. Our results demonstrate that the STAT2 knockout hamster represents a novel small animal model of severe MARV infection and disease without the requirement for virus adaptation.
Keywords: Marburg virus, STAT2 KO hamster, Filovirus, animal model
Marburg viruses (MARVs) are members of the family Filoviridae, which also includes the related Ebola viruses (EBOVs) and Cuevavirus [1], and are endemic across sub-Saharan Africa in fruit bat reservoir hosts [2]. Patients present initially with flulike symptoms, including fever, chills, headache, and general myalgia. Symptoms progress within several days to a central rash, nausea, and diarrhea and concludes with progression to hemorrhage and multiorgan system failure, known as Marburg hemorrhagic fever (MHF) [3]. With case fatality rates for confirmed cases of up to 90%, MARV presents a significant public health hazard across the region. Survivors of the infection report of long-term complications, such as joint pain, psychosis, and ocular symptoms [4], and it has been reported that MARV can persist in some survivors and be spread via semen [5]. Currently, no licensed therapeutics or vaccines are available to treat MHF. Therefore, MARV is categorized as a National Institute of Allergy and Infectious Diseases category A priority pathogen and a tier 1 select agent, requiring biosafety level (BSL) 4 containment.
The development of vaccines and therapeutics requires extensive testing in animal models. Typically, such testing is performed initially in rodent models, followed by efficacy testing in nonhuman primate (NHP) models [6]. Mice, guinea pig, and hamster models have been developed for both MARV and EBOV, but rodent-adapted viruses are required to establish an infection in immunocompetent animals to reproduce some of the disease features observed in NHP models and human patients [7–12]. Recently, a novel hamster model has been described for hamster-adapted MARV Angola (HA-MARV), which displayed almost all of the clinical features of MHF observed in patients and NHPs [7]. Rodent-adapted filoviruses accumulate mutations over serial passages that increase their pathogenicity in rodents [9, 10, 13, 14]. These adaptations may lead to changes in the virus that less faithfully reproduce human infection and disease and alter the sensitivity of the infection to antivirals or vaccines.
Type I interferon (IFN) responses have been shown to play a key role to resistance of mice to infection with wild-type filoviruses [15]. Mice deficient in type I IFN responses are susceptible to infection with wild-type EBOV and Sudan virus, resulting in high viral load in multiple organs (including liver and spleen) and certain aspects of clinical disease, as described in NHP models and patients, including thrombocytopenia, liver damage, and lymphopenia [10, 15–18]. Although immunocompromised small animal models have limited usefulness for studying correlates of immune response in pathogenesis or protection by vaccine candidates, they can be used to evaluate the efficacy of candidate antiviral therapeutics with clinical wild-type isolates. The abrogation of the STAT2 pathway has been used to examine the pathogenicity of diverse viral infections in the hamster model [19–22]. Thus, we hypothesized that the absence of this pathway would enable productive replication of MARV in hamsters, without the need to modify the virus, and its ability to respond to IFN, by serial passage.
In the present study, we demonstrate that Syrian hamsters deficient in STAT2 signaling (STAT2−/−) are susceptible to infection with multiple wild-type non–rodent-adapted MARV variants, including Musoke, Angola, Voege, and Ravn (RAVV), and subsequently characterize the natural history of disease and immune responses in MARV Musoke-infected hamsters. This new hamster model shares features of MHF in NHPs and humans and will be a valuable resource for studying the molecular mechanisms of MARV-induced pathogenesis.
MATERIALS AND METHODS
Ethics Statement
All animal experiments were approved by the Institutional Animal Care and Use Committee of the University of Texas Medical Branch (UTMB) (protocol 1601002) and performed following the guidelines of the Association for Assessment and Accreditation of Laboratory Animal Care International (AAALAC) by certified staff in an AAALAC-approved facility.
Viruses
MARV isolates RAVV, Musoke, Voege, and Angola were used for this study and provided through the World Reference Center for Emerging Viruses and Arboviruses (UTMB; Thomas Ksiazek). Virus titers were determined by plaque assay on Vero E6 cells (American Type Culture Collection), using a modified protocol as described elsewhere, with incubation times of 6 days for Voege and Angola and 13 days for Musoke and RAVV [23]. All work with infectious MARVs was performed at the Robert E. Shope and Galveston National Laboratory BSL-4 laboratories at UTMB.
Animals
STAT2 knockout (KO) hamsters were developed as described elsewhere [24]. Male and female animals were used in all studies to avoid sex-biased selection in pathological examination or molecular markers of disease.
Susceptibility Study
Groups of 5 STAT2 KO hamsters were inoculated with 105 plaque-forming units (PFUs) of virus via the intraperitoneal route. Animals were monitored daily for development of clinical signs of disease. Changes in body weight were determined daily for the first 10 days post infection (dpi) and then every third day until end of the study. Animals were humanely euthanized if disease progressed to end point requirements or weight loss reached 25% of starting weight.
Serial Dosing Study
Based on the susceptibility study, MARV Musoke was selected for further model development. To determine the mean lethal dose (LD50), 5 groups of 6 STAT2 KO hamsters were infected with 10, 102, 103, 104 or 105 PFUs via the intraperitoneal route. Monitoring was performed as described above.
Natural History Study
To investigate disease development of MARV Musoke infection in STAT2 KO hamsters, a total of 44 animals were inoculated with 1000 × LD50 (104 PFUs) via the intraperitoneal route. Negative control animals were inoculated with Dulbecco phosphate-buffered saline (Corning). Health was monitored as described above. Preselected animals were euthanized between 2 and 8 dpi. At time of euthanasia, whole blood was collected by cardiac puncture, and necropsies were performed. Brain, lung, liver, spleen, heart, and kidney samples were collected, as well as inguinal, superficial cervical, deep cervical, mediastinal, mesenteric, and axillary lymph nodes when possible. Subdivided tissues were homogenized for RNA extraction (TRIzol reagent; Thermo Fisher Scientific) and virus titration (Dulbecco phosphate-buffered saline), and fixed in 10% formalin (Thermo Fisher Scientific) for histopathological analysis. Whole lymph nodes were processed for titration. Gross lesions were noted at the time of euthanasia and necropsy. Animals were not perfused before necropsy.
Blood Chemistry
Whole blood samples were analyzed using a Hemavet 950FS system (Drew Scientific) on the day of blood collection. A mouse standard was used. Blood was dispensed into single-use heparinized vials and rotated until use. The following laboratory measurements were analyzed: white and red blood cell counts; counts and percentages for neutrophils, lymphocytes, monocytes, eosinophils, and basophils; hemoglobin level; hematocrit; mean corpuscular volume, mean corpuscular hemoglobin, and mean corpuscular hemoglobin concentration; red blood cell distribution width; and platelet count.
RNA Extraction and Reverse-Transcription Polymerase Chain Reaction
RNA extractions from TRIzol reagent were performed according to the manufacturer’s instructions, with modifications. Samples were mixed with chloroform and spun to clarify before mixing with 1 volume of 100% ethanol and loading onto a DirectZol RNA Miniprep (Zymo) column. deoxyribonuclease digestion was performed in column. RNA samples were converted to complementary DNA using the Ambion High Capacity cDNA Synthesis kit and standard cycling. Primers used for selected hamster genes and MARV Musoke are summarized in Supplementary Table 1 [7, 25]. Bio-Rad iTaq Sybr Green chemistry was used in standard cycling conditions. Samples are calculated normalized to hamster RPL18 and presented as fold change relative to uninfected (mock-infected) samples. There were no significant differences for RPL18 between the mock-infected animals euthanized at 2 and 8 dpi.
Histopathology and Immunohistochemistry
Formalin-fixed organs were preserved immediately after necropsy. Before removal from BSL-4 containment, formalin was exchanged 3 times 24 hours apart and the organs were transferred to a new container before removal, in accordance with standard UTMB protocols. Formalin-fixed paraffin-embedded tissues were sectioned (5–8 µm) and processed for hematoxylin-eosin staining and immunohistochemistry (IHC) for MARV nucleoprotein [26], CD3 (T-cell marker), CD20 (B-cell marker), and ionized calcium binding adaptor molecule 1 (macrophage marker). IHC was performed as described elsewhere [27]. The methods for the IHC stains performed are presented in Supplementary Table 2. For MARV IHC, tissue sections were permeabilized with 0.5% Triton X-100 (Sigma-Aldrich), and the endogenous peroxidase activity was blocked for 15 minutes with 3% hydrogen peroxide. Slides were counterstained with hematoxylin (HHS16; Sigma-Aldrich). After dehydration in ascending grades of ethanol and xylene, the slides were permanently mounted.
Statistics
Statistical analyses were performed using Sigmaplot 14 software (Systat Software, Inc). Data are presented as median values for animals euthanized on the indicated day, with standard deviations.
RESULTS
Susceptibility of STAT2 KO Hamsters to Non–Rodent-Adapted Wild-Type MARV Infection
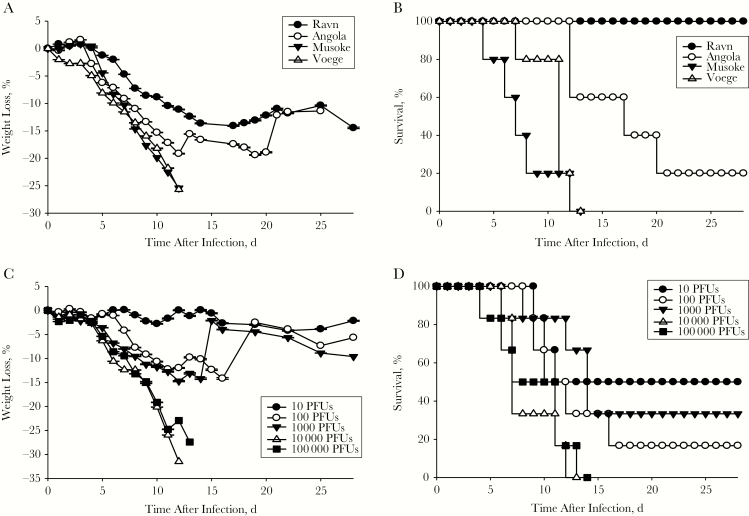
Wild-type Syrian hamsters have been described as refractory to disease development after infection with wild-type MARV Angola [7]. To determine the susceptibility of STAT2 KO hamsters to infection with non–rodent-adapted wild-type MARV, animals were initially infected with 105 PFUs of 1 of the 4 variants, MARV Angola, Musoke, Voege, or RAVV, via the intraperitoneal route. All animals demonstrated weight loss starting between 1 (MARV Voege) and 4 (RAVV, MARV Angola, and Musoke) dpi (Figure 1A).
Figure 1.
Susceptibility of STAT2 knockout (KO) hamsters to infection with wild-type Marburg virus (MARV). A, B, Weight loss (A) and survival outcome (B) during infection of STAT2 KO hamsters (n = 5) infected intraperitoneally with 105 plaque-forming units (PFUs) of MARV Ravn, Angola, Musoke, and Voege. C, D, Weight loss (C) and survival outcome (D) during serial dosing study for MARV Musoke in STAT2 KO hamsters. Groups of 6 hamsters (3 male, 3 female) were infected with serial dilutions of MARV Musoke via the intraperitoneal route.
Clinical signs of disease, including scruffy coat, lethargy, hunched posture, and weight loss, were detectable by 5 dpi with Musoke, Voege, and Angola infection. RAVV-infected animals began to show similar signs at 13 dpi, but all recovered by 21 dpi. Infection with MARV Musoke and Voege resulted in uniform lethality by 12 dpi (Figure 1B). Hamsters infected with MARV Angola had a delayed onset of disease development and required euthanasia between 12 and 21 dpi, resulting in 80% lethality (Figure 1B). All animals infected with RAVV lost weight but survived the infection (Figure 1A and 1B). Weight loss peaked at 15% on 16 dpi, followed by recovery and weight gain. However, none of the animals had returned to their starting weight by the end of the study, 28 dpi. Based on the results of the susceptibility study, we chose to further characterize MARV Musoke because of the more rapid onset of disease and uniform lethality.
Serial Dosing Study With MARV Musoke in STAT2 KO Hamsters
To determine the LD50 for MARV Musoke, the point at which 50% of animals die of infection, hamsters were challenged intraperitoneally with 10–105 PFUs of virus and monitored for disease development. Doses were confirmed by back titration within acceptable assay variation. Although infection with 10 PFUs resulted in only a transient and minor change in weight, all animals infected with 102–105 PFUs had significant weight loss (Figure 1C). Uniform lethality was achieved with 104 and 105 PFUs between 4 and 14 dpi (Figure 1D). Half of the animals infected with 10 PFUs reached euthanasia criteria between 9 and 11 dpi, representing the LD50.
Natural History and Pathogenicity of MARV Musoke Infection in STAT2 KO Hamsters
To further characterize the pathogenicity of MARV Musoke in STAT2 KO hamsters, a natural history of disease study was performed. To ensure uniform lethality, 36 hamsters were infected intraperitoneally with 104 PFUs, and 8 additional hamsters were mock infected. Predetermined animals were euthanized on 2, 4, 5, 6, 7, and 8 dpi, and mock-infected animals on 2 and 8 dpi. However, to accommodate progression of disease during infection, both scheduled animals and any animals showing sufficient disease to necessitate humane euthanasia were collected. Musoke-infected animals began losing weight at 5 dpi. Starting on 6 dpi, animals showed clinical signs of disease, including scruffy coat, lethargy, hunched posture, irregular breathing, orbital tightening, nasal discharge, abnormal gait, weight loss, hyperreflexia, and head tilt. Mock-infected animals were clinically normal over the course of the study.
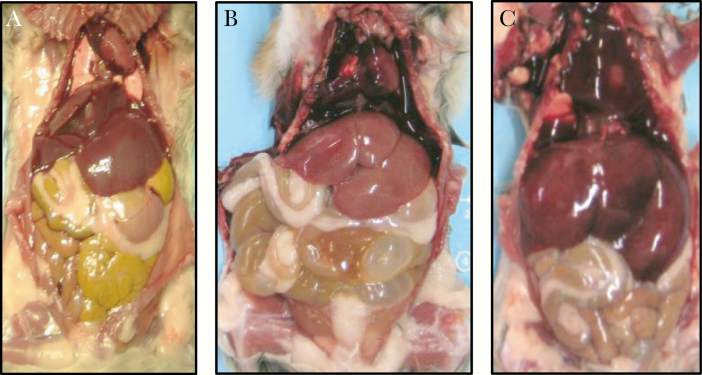
At necropsy at 2 dpi, STAT2 KO hamsters did not show any abnormal gross morphological changes compared with mock-infected animals (Figure 2A). At 8 dpi, pathological changes were observed in infected animals (Figure 2B and 2C). Livers were either diffusely dark red, diffusely pale mahogany, or very finely mottled pale mahogany and tan. Some had rounded edges. On sampling of the liver, excess blood flowed out from the cut surfaces. No maculopapular or petechial rash was detected on any of the animals. Hematological analysis showed no significant differences in analyzed parameters in infected animals. Although nonsignificant, changes were observed for white blood cell counts (Supplementary Figure 1A), lymphocyte counts (Supplementary Figure 1B), and neutrophil counts (Supplementary Figure 1C). No significant changes or trends were observed in platelet counts (Supplementary Figure 1D).
Figure 2.
Gross pathological findings in mock-infected (A) and Marburg virus (MARV)–infected (B, C) STAT2 knockout (KO) hamsters. A, Findings in control (mock-infected) STAT2 KO hamsters at 2 days post infection (dpi). B, C, Findings in STAT2 KO hamsters at 8 dpi, with pale mahogany liver (B) and diffusely dark mahogany-red liver with rounded edges (swollen and congested liver) (C).
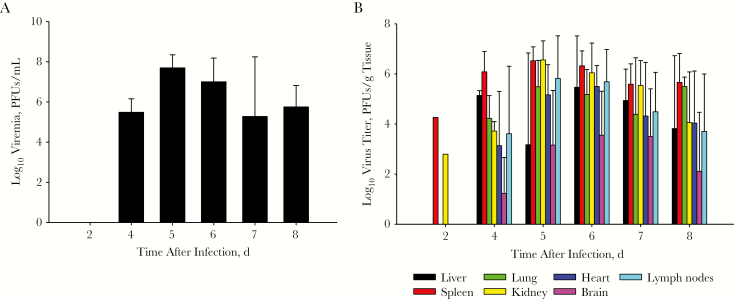
Severe Systemic Infection Caused by MARV Musoke in STAT2 KO Hamsters
Serum and tissue samples collected during the natural history study were analyzed for the presence of infectious MARV Musoke. Viremia was not detected at 2 dpi but spiked at 4 dpi (Figure 3A). Because no blood samples were collected at 3 dpi, the onset of viremia before 4 dpi might have been missed. Peak titers in blood were reached by 5 dpi (108 PFUs/mL), and titers remained elevated through the final day of euthanasia. Infectious virus was detected for 1 animal each in the spleen and kidney, at 2 dpi. However, widespread infection in STAT2 KO hamsters was detected between 4 and 8 dpi in all analyzed tissues (Figure 3B). The highest levels of infectious virus were detected in the liver (105 PFUs/mL), spleen (106 PFUs/mL), lung (105 PFUs/mL), heart (105 PFUs/mL), and kidney (106 PFUs/mL). Moderate titers were detected in the brain (103–104 PFUs/mL). Infectious virus was also detected in lymph nodes (104–106 PFUs/mL), represented here as the average of titers determined in mediastinal, axillary, mesenteric, superficial cervical, deep cervical, and inguinal nodes.
Figure 3.
Marburg virus (MARV) replication kinetics in STAT2 knockout hamsters, shown as MARV Musoke titers in serum (A) and selected organs (B); titers were determined by means of plaque assay. Abbreviation: PFUs, plaque-forming units.
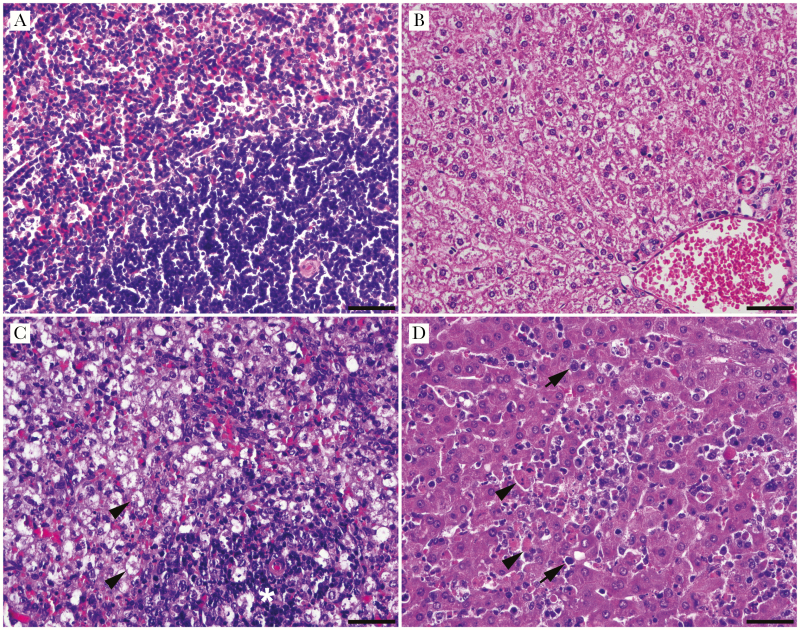
Histopathology in MARV Musoke-Infected STAT2 KO Hamsters
Histological analysis revealed splenitis and hepatitis in infected hamsters starting at 6 dpi (Figure 4A and 4D). The severity of hepatitis and splenitis lesions varied from mild to severe, with a trend to increased severity from 6 to 8 dpi. Necrotic splenitis was characterized by diffuse necrosis of lymphocytes, infiltration by activated macrophages, and small to moderate numbers of neutrophils in both the red and white pulp (Figure 4C). Necrotic hepatitis was characterized by multiple random foci of hepatocellular necrosis infiltrated by small to moderate numbers of mononuclear cells and fewer neutrophils. Moderate individual hepatocellular necrosis and a moderate number of mononuclear inflammatory cells within the sinusoids were present. Multifocal infiltration of a small to moderate number of mononuclear cells and a few neutrophils was also observed in the periportal areas (Figure 4D). At 8 dpi, 1 of 7 hamsters had mild to moderate multifocal, mononuclear, and neutrophilic meningitis (data not shown). Cumulative scoring of liver and splenic lesions is presented in Supplementary Figure 2. These inflammatory mononuclear cells in the liver were immunoreactive for binding adaptor molecule 1 and identified as macrophages (Supplementary Figure 3). Rare circulating cells in the liver sinusoids were immunoreactive for CD3 or CD20.
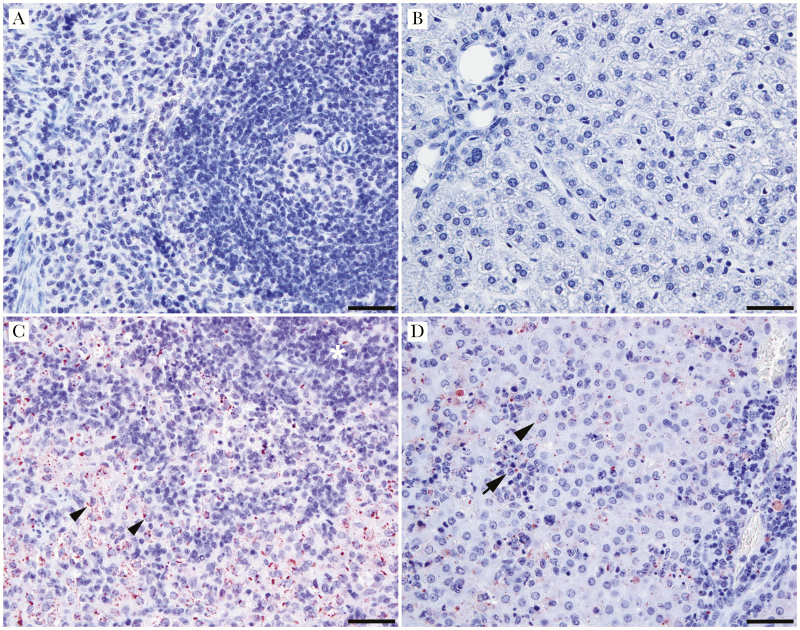
Figure 4.
Histopathological appearance of lesions in Marburg virus (MARV) Musoke-infected STAT2 knockout (KO) hamsters. A, B, Spleen (A) and liver (B) of a mock-infected control animal at 2 days post infection (dpi). C, MARV-infected spleen at 6 dpi, demonstrating neutrophilic splenitis with activation of the red pulp macrophages (arrowheads) and lymphoid depletion of the white pulp (asterisk). D, MARV-infected liver at 6 dpi shows hepatitis characterized by coagulative necrosis of individual or a small group of hepatocytes (arrowheads), infiltration of inflammatory cells, mostly macrophages (arrows) and a few neutrophils, and Kupffer cell activation. (Scale bars represent 50 μm; hematoxylin-eosin stain, original magnification ×400.)
Replicate tissue sections from animals selected based on detection of infectious virus particles and histopathological review underwent IHC staining for MARV (Figure 5A–5D). MARV-specific antigen was detected in the spleen and liver of infected hamsters beginning at 5 dpi. No antigen was detected in the brain tissue from the same animals (data not shown). MARV antigens were present in mononuclear cells, mostly located in the splenic red pulp (Figure 5C), and in hepatocytes, Kupffer cells/macrophages, and a few endothelial cells in the liver (Figure 5D).
Figure 5.
Marburg virus (MARV) immunohistochemistry in MARV Musoke–infected STAT2 knockout (KO) hamsters. A, B, Spleen (A) and liver (B) of mock-infected control animal at 2 days post infection (dpi). C, MARV-infected spleen at 5 dpi showing immunoreactivity in mononuclear cells (arrowheads) in the splenic white (asterisk) and red pulps. D, MARV-infected liver at 5 dpi with immunoreactivity in hepatocytes (arrowhead), mononuclear inflammatory cells (arrow) and endothelial cells. Inset: higher magnification showing immunoreactivity in hepatocytes (arrowhead). (Scale bars denote 50 μm; hematoxylin-eosin stain, original magnification ×400; inset, ×100 magnification.)
Cytokine Response to MARV Musoke Infection in STAT2 KO Hamsters
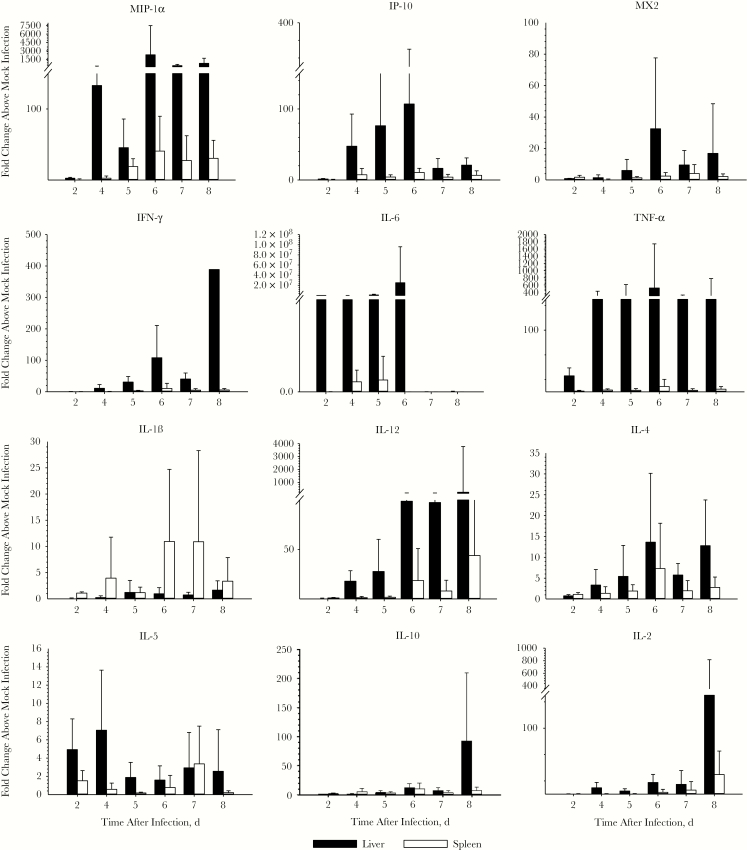
To characterize the innate immune responses of STAT2 KO hamster, levels of a panel of hamster cytokine and chemokine messenger RNAs (Supplementary Table 1) were determined in MARV Musoke–infected hamsters during the course of infection (Figure 6). In the livers and spleens of infected hamsters, an overall strong response could be detected throughout the course of the infection, especially in the liver (Figure 6). Levels of the proinflammatory chemokines macrophage inflammatory protein (MIP) 1α and IFN-inducible protein (IP) 10 increased in the livers over time, reaching a peak at 6 dpi. A similar trend could be observed for myxovirus resistance 2 (Mx2), representative of type I IFN responses. Transcript levels of the type II IFN cytokine IFN-γ peaked at 6 and 8 dpi, with a temporary decrease at 7 dpi.
Figure 6.
Levels of messenger RNA transcripts in Marburg virus (MARV) Musoke-infected STAT2 knockout (KO) hamsters. Reverse-transcription polymerase chain reaction analysis of transcripts isolated from livers and spleens of infected hamsters at the indicated day after infection. Up-regulation of chemokines, proinflammatory, and anti-inflammatory cytokines is evident. Liver is a primary target of MARV infection, and the activation of immune cells strongly affects the spleen during replication. Abbreviations: IFN, interferon; IL-1β, IL-2, IL-4, IL-5, IL-6, IL-10, and IL-12, interleukin 1β, 2, 4, 5, 6, 10, and 12; IP-10, IFN-inducible protein 10; MIP-1α, macrophage inflammatory protein 1α; MX2, myxovirus resistance 2; TNF-α, tumor necrosis factor-α.
The proinflammatory cytokines interleukin 6 (IL-6) and tumor necrosis factor (TNF) α peaked by 2 and 4 dpi, respectively. Interleukin 1β (IL-1β) transcript levels, on the other hand, peaked later during the infection, at 6 dpi, and this was the only proinflammatory cytokine that was markedly increased in the spleen. The T-helper (Th) 1 cytokine interleukin 12 (IL-12) and Th2 cytokine interleukin 4 (IL-4) steadily increased with progressing infection in the liver and peaked at 6 dpi, whereas the Th2 cytokine interleukin 5 (IL-5) was only moderately elevated early and decreased on 5 dpi for the remainder of the course of infection. Elevated transcript levels for interleukin 2 and 10 (IL-2 and IL-10) were measured only at the end of the study, at 8 dpi.
In the lung, kidney, heart, and brain, responses for the proinflammatory chemokines MIP-1α and IP-10 followed a trend similar to that observed in liver and spleen, with peak levels observed late during infection, starting at 6 dpi (Supplementary Figure 3). Type I (myxovirus resistance 2) and type II (IFN-γ) IFN responses were strongest in the kidney, lung, and heart. Whereas IL-6 peaked early after infection (4 dpi) in the heart and kidney, TNF-α transcript levels were most strongly up-regulated at 7 dpi. In contrast to the spleen, IL-1β levels were strongly increased in the lung and brain starting at 2 dpi, whereas maximum levels in the kidney were reached later during the infection. The Th1 cytokine IL-12 and the Th2 cytokine interleukin 4 sharply increased at 6 dpi in the lung. Up-regulation of interleukin 5 was detected in the heart mostly at 4 and 6 dpi. IL-10 and IL-2 were already increased by 6 dpi in hearts and brains for IL-10, and in lungs and hearts for IL-2 (Supplementary Figure 4).
DISCUSSION
Type I IFN responses are critical for establishing an antiviral state in the host and are crucial for subsequent activation of adaptive immune responses. Filoviruses encode several viral proteins (VP35, VP24, and VP40), which are known to target type I IFN responses [28]. This suppression of the innate immune response is important for viral replication and ultimately pathogenesis. Previously, mouse models deficient in the type I IFN response, including STAT1 KO mice, have been successfully developed and characterized, allowing the use of non–rodent-adapted wild-type filoviruses [15, 29]. STAT1 KO mice are susceptible to infection with wild-type EBOVs and MARV, but with slower disease onset than mouse-adapted EBOV (MA-EBOV) [29]. Infection in these mice mirrors the overall gross liver pathological changes of filovirus infection.
Recently, a novel STAT2 KO Syrian hamster model has been developed and demonstrated to support replication of divergent viruses [19–22]. Because STAT2 is a potent activator of type I and type II IFN, we hypothesized that the abrogation of this pathway will favor wild-type MARV replication in these animals [30]. In the current study, we found that STAT2 KO hamsters were susceptible to infection with MARV Musoke, Angola, RAVV, and Voege. However, RAVV was the only MARV that failed to cause severe disease. RAVV is significantly divergent from other MARVs [31], which may contribute to the differential pathogenicity observed. Whereas MARV Angola has been reported to be the most pathogenic MARV in humans and NHPs [32–36], we observed a delayed onset of disease development in the STAT2 KO hamsters.
To better define factors contributing to this observation, future efforts will need to examine the pathological changes and innate immune responses associated with MARV Angola in this hamster model. Because STAT2 is an important modulator and inducer of the IFN-I pathway, it is likely to be intimately involved in the nuances of pathogenic differences between model systems. Selecting MARV Musoke for further model characterization, we demonstrated that challenge with as low a dose as 10 PFUs could result in severe infection. In the natural history study, we found that infection with 1000 × LD50 of MARV Musoke resulted in systemic spread. MARV was found at high titers in the blood, liver, spleen, kidneys, and other major organs. While hematological changes were not significant, trends suggest that MARV Musoke infection resulted in neutrophilia, which probably was the main contributor to leukocytosis observed toward the end of the study. In contrast to the HA-MARV hamster and NHP models, as well as patient data, no maculopapular or petechial rash was detected on any of the STAT2 KO hamsters [7, 32, 33, 37]. We did not analyze blood of infected hamsters for the presence of coagulation abnormalities or serum biochemistry parameters, and such analyses need to be performed in future studies.
In the spleen, necrotic splenitis was primarily characterized by infiltration of activated macrophages and diffuse necrosis of lymphocytes. In the liver, necrotic hepatitis was characterized by small to moderate numbers of infiltrating macrophages and fewer neutrophils. These findings are consistent with reports of MA-EBOV infections in wild-type hamsters [11] and the recently described HA-MARV hamster model [7]. Compared with the findings of Marzi et al [7], onset of hepatitis was delayed by 3 days, whereas the onsets of splenitis were closer, arising 1 day earlier in the study by Marzi et al (5 vs 6 dpi). Similarly, both studies indicated loss of lymphocytes in splenic pulp and the subsequent infiltration of macrophages into the pulp. Interestingly, in both our study and that of Marzi et al [7], infectious virus and viral genome were both readily isolated from the brain, but viral antigen was not detectable by IHC, even though meningitis had developed in 1 of 7 hamsters euthanized at 8 dpi. A more detailed analysis of specific regions of the brain potentially harboring filovirus neural replication may be necessary.
To gain insight into the immune response to MARV infection in STAT2 KO hamsters, we performed a real-time reverse-transcription polymerase chain reaction cytokine profiling analysis on all major organs. Similar to findings in studies characterizing MA-EBOV and HA-MARV infection in hamsters, we also detected an overzealous immune response, as indicated by the expression of certain cytokine/chemokine genes (including IP-10, IL-6, TNF-α, IL-1β, and IL-10) [7, 11, 25]. In general, the replication of wild-type MARV Musoke seems to correlate with patterns of cytokine and chemokine expression in infected hamster organs. This could imply that the innate immune response to infection was not capable of inducing a protective immune response, which ultimately could contribute to disease development.
Levels of IL-1β messenger RNAs increase over the course of MARV infection in the spleens of infected animals, peaking at 7 dpi (Figure 6). Interestingly, combined with the proinflammatory presence of IL-1β in the brain (Supplementary Figure 3), IL-10, a suppressor of inflammatory activity, is also up-regulated during MARV Musoke infection in the liver (Figure 6). IL-1β has been previously shown to be up-regulated in models of EBOV disease, and increased levels of circulating IL-1β have been detected in the serum of infected humans and rhesus macaques [38]. This may suggest that the immune system is struggling to balance the demands of proinflammatory and antiviral responses to infection. Furthermore, elevated IFN-γ levels have been described in EBOV- and MARV-infected NHPs and human patients and may have an antiviral role in vivo [39]. These increased levels might be regulated by an increase in IL-12, which can stimulate transcription of IFN-γ [40]. The infiltration of macrophages into the liver, which are activated by IFN-γ, can also be detected in the current study [40, 41]. Late activation (6, 7, and 8 dpi) of macrophages produced MIP-1α tracks, with the increase in neutrophils to their highest level at 6 dpi, in addition to splenic macrophage activation and hepatic infiltration.
In conclusion, the current study assessed a novel small animal model for wild-type MARV using STAT2 KO hamsters, in which viral replication rapidly progresses to multiorgan infection and extensive viremia. Hepatic and splenic inflammation, leukocytosis with neutrophilia, and general up-regulation of proinflammatory mediators are clinical features of MHF in patients and NHPs. Future studies will need to characterize the levels of adaptive immune responses to support evaluation of MARV vaccine candidates. Thus, this model will provide a new resource for studying molecular mechanisms of MARV-induced pathogenesis, as well as for testing antiviral countermeasures against clinical MARV isolates.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Acknowledgments. We thank Thomas Ksiazek (UTMB, Galveston) for providing MARVs, James M. Robl (Auratus Bio, Canton, South Dakota) for providing the STAT2 KO hamsters, and Ayato Takada (Hokkaido University, Sapporo, Japan) for providing the anti-MARV nucleoprotein antibody.
Financial support. This work was supported by the National Institutes of Health (grant R41OD021979 to B. B. G., Z. W., and A. N. F) through Auratus Bio.
Potential conflicts of interest. Z. W. has financial interests in Auratus Bio, a biotech startup specialized in developing genetically engineered animal models of human disease. All other authors report no potential conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Presented in part: Ninth International Filovirus Symposium, Marburg, Germany, 13–16 September 2017. Abstract P102.
References
- 1. Jun SR, Leuze MR, Nookaew I, et al. Ebolavirus comparative genomics. FEMS Microbiol Rev 2015; 39:764–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Towner JS, Amman BR, Sealy TK, et al. Isolation of genetically diverse Marburg viruses from Egyptian fruit bats. PLoS Pathog 2009; 5:e1000536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nyakarahuka L, Ojwang J, Tumusiime A, et al. Isolated case of Marburg virus disease, Kampala, Uganda, 2014. Emerg Infect Dis 2017; 23:1001–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mehedi M, Groseth A, Feldmann H, Ebihara H. Clinical aspects of Marburg hemorrhagic fever. Future Virol 2011; 6:1091–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brainard J, Pond K, Hooper L, Edmunds K, Hunter P. Presence and persistence of Ebola or Marburg virus in patients and survivors: a rapid systematic review. PLoS Negl Trop Dis 2016; 10:e0004475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nakayama E, Saijo M. Animal models for Ebola and Marburg virus infections. Front Microbiol 2013; 4:267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Marzi A, Banadyga L, Haddock E, et al. A hamster model for Marburg virus infection accurately recapitulates Marburg hemorrhagic fever. Sci Rep 2016; 6:39214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Qiu X, Wong G, Audet J, et al. Establishment and characterization of a lethal mouse model for the Angola strain of Marburg virus. J Virol 2014; 88:12703–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cross RW, Fenton KA, Geisbert JB, Ebihara H, Mire CE, Geisbert TW. Comparison of the pathogenesis of the Angola and Ravn strains of Marburg virus in the outbred guinea pig model. J Infect Dis 2015; 212(suppl 2):S258–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bray M, Hatfill S, Hensley L, Huggins JW. Haematological, biochemical and coagulation changes in mice, guinea-pigs and monkeys infected with a mouse-adapted variant of Ebola Zaire virus. J Comp Pathol 2001; 125:243–53. [DOI] [PubMed] [Google Scholar]
- 11. Ebihara H, Zivcec M, Gardner D, et al. A Syrian golden hamster model recapitulating Ebola hemorrhagic fever. J Infect Dis 2013; 207:306–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bray M, Davis K, Geisbert T, Schmaljohn C, Huggins J. A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J Infect Dis 1999; 179(suppl 1):S248–58. [DOI] [PubMed] [Google Scholar]
- 13. Valmas C, Basler CF. Marburg virus VP40 antagonizes interferon signaling in a species-specific manner. J Virol 2011; 85:4309–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Warfield KL, Bradfute SB, Wells J, et al. Development and characterization of a mouse model for Marburg hemorrhagic fever. J Virol 2009; 83:6404–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Brannan JM, Froude JW, Prugar LI, et al. Interferon α/β receptor-deficient mice as a model for Ebola virus disease. J Infect Dis 2015; 212(suppl 2):S282–94. [DOI] [PubMed] [Google Scholar]
- 16. Bradfute SB, Braun DR, Shamblin JD, et al. Lymphocyte death in a mouse model of Ebola virus infection. J Infect Dis 2007; 196(suppl 2):S296–304. [DOI] [PubMed] [Google Scholar]
- 17. Bradfute SB, Swanson PE, Smith MA, et al. Mechanisms and consequences of Ebolavirus-induced lymphocyte apoptosis. J Immunol 2010; 184:327–35. [DOI] [PubMed] [Google Scholar]
- 18. Shurtleff AC, Bavari S. Animal models for ebolavirus countermeasures discovery: what defines a useful model?Expert Opin Drug Discov 2015; 10:685–702. [DOI] [PubMed] [Google Scholar]
- 19. Gowen BB, Westover JB, Miao J, et al. Modeling severe fever with thrombocytopenia syndrome virus infection in golden Syrian hamsters: importance of STAT2 in preventing disease and effective treatment with favipiravir. J Virol 2017; 91:e01942-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Siddharthan V, Van Wettere AJ, Li R, et al. Zika virus infection of adult and fetal STAT2 knock-out hamsters. Virology 2017; 507:89–95. [DOI] [PubMed] [Google Scholar]
- 21. Toth K, Lee SR, Ying B, et al. STAT2 knockout Syrian hamsters support enhanced replication and pathogenicity of human adenovirus, revealing an important role of type I interferon response in viral control. PLoS Pathog 2015; 11:e1005084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Westover JB, Rigas JD, Van Wettere AJ, et al. Heartland virus infection in hamsters deficient in type I interferon signaling: protracted disease course ameliorated by favipiravir. Virology 2017; 511:175–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bharaj P, Atkins C, Luthra P, et al. The host E3-ubiquitin ligase TRIM6 ubiquitinates the Ebola virus VP35 protein and promotes virus replication. J Virol 2017; 91:e00833-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fan Z, Li W, Lee SR, et al. Efficient gene targeting in golden Syrian hamsters by the CRISPR/Cas9 system. PLoS One 2014; 9:e109755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Zivcec M, Safronetz D, Haddock E, Feldmann H, Ebihara H. Validation of assays to monitor immune responses in the Syrian golden hamster (Mesocricetus auratus). J Immunol Methods 2011; 368:24–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kajihara M, Marzi A, Nakayama E, et al. Inhibition of Marburg virus budding by nonneutralizing antibodies to the envelope glycoprotein. J Virol 2012; 86:13467–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ramos-Vara JA. Technical aspects of immunohistochemistry. Vet Pathol 2005; 42:405–26. [DOI] [PubMed] [Google Scholar]
- 28. Ramanan P, Shabman RS, Brown CS, Amarasinghe GK, Basler CF, Leung DW. Filoviral immune evasion mechanisms. Viruses 2011; 3:1634–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Raymond J, Bradfute S, Bray M. Filovirus infection of STAT-1 knockout mice. J Infect Dis 2011; 204(suppl 3):S986–90. [DOI] [PubMed] [Google Scholar]
- 30. Hambleton S, Goodbourn S, Young DF, et al. STAT2 deficiency and susceptibility to viral illness in humans. Proc Natl Acad Sci U S A 2013; 110:3053–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Barrette RW, Xu L, Rowland JM, McIntosh MT. Current perspectives on the phylogeny of Filoviridae. Infect Genet Evol 2011; 11:1514–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Alves DA, Glynn AR, Steele KE, et al. Aerosol exposure to the Angola strain of Marburg virus causes lethal viral hemorrhagic fever in cynomolgus macaques. Vet Pathol 2010; 47:831–51. [DOI] [PubMed] [Google Scholar]
- 33. Johnston SC, Lin KL, Twenhafel NA, et al. Dose response of MARV/Angola infection in cynomolgus macaques following IM or aerosol exposure. PLoS One 2015; 10:e0138843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Fernando L, Qiu X, Melito PL, et al. Immune response to Marburg virus Angola infection in nonhuman primates. J Infect Dis 2015; 212(suppl 2):S234–41. [DOI] [PubMed] [Google Scholar]
- 35. Geisbert TW, Daddario-DiCaprio KM, Geisbert JB, et al. Marburg virus Angola infection of rhesus macaques: pathogenesis and treatment with recombinant nematode anticoagulant protein c2. J Infect Dis 2007; 196(suppl 2):S372–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lin KL, Twenhafel NA, Connor JH, et al. Temporal characterization of Marburg virus Angola infection following aerosol challenge in rhesus macaques. J Virol 2015; 89:9875–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bausch DG, Nichol ST, Muyembe-Tamfum JJ, et al. ; International Scientific and Technical Committee for Marburg Hemorrhagic Fever Control in the Democratic Republic of the Congo Marburg hemorrhagic fever associated with multiple genetic lineages of virus. N Engl J Med 2006; 355:909–19. [DOI] [PubMed] [Google Scholar]
- 38. Connor JH, Yen J, Caballero IS, et al. Transcriptional profiling of the immune response to Marburg virus infection. J Virol 2015; 89:9865–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rhein BA, Powers LS, Rogers K, et al. Interferon-γ inhibits Ebola virus infection. PLoS Pathog 2015; 11:e1005263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Darwich L, Coma G, Peña R, et al. Secretion of interferon-gamma by human macrophages demonstrated at the single-cell level after costimulation with interleukin (IL)-12 plus IL-18. Immunology 2009; 126:386–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Held TK, Weihua X, Yuan L, Kalvakolanu DV, Cross AS. Gamma interferon augments macrophage activation by lipopolysaccharide by two distinct mechanisms, at the signal transduction level and via an autocrine mechanism involving tumor necrosis factor alpha and interleukin-1. Infect Immun 1999; 67:206–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.