Abstract
Screening of monoclonal antibodies against ebolaviruses requires small-animal models. Wild-type mice require adaptation of ebolaviruses, whereas immunodeficient mice are still resistant to nonadapted Bundibugyo ebolavirus. Swapping of Ebola virus glycoprotein with that from Bundibugyo virus resulted in a replication-competent chimeric virus, which caused 100% lethal infection in STAT1 knockout mice. Monoclonal antibody BDBV223 isolated from a human survivor of Bundibugyo virus infection protected mice from challenge with the chimeric virus. These data demonstrate the suitability of the approach for in vivo screening of antibodies and suggest the greater contribution of internal Ebola proteins in pathogenesis compared to Bundibugyo virus proteins.
Keywords: Bundibugyo virus, Ebola virus, glycoprotein, mouse model, monoclonal antibodies
The ebolavirus Bundibugyo virus (BDBV) was discovered during the first known outbreak in 2007 in Uganda, with a subsequent outbreak occurring in 2012 in the Democratic Republic of Congo [1]. Cumulatively, these outbreaks resulted in a case-fatality rate of 33.7%, which is comparable to that of Ebola virus (EBOV) infections, including the Western African epidemic of 2013–2016 (41.4%) [2]. This devastating epidemic in nonendemic areas highlights an urgent need for the development of therapeutics against emerging and reemerging filoviruses.
Monoclonal antibodies (mAbs) show great promise for development of effective filovirus antibody treatments [3]. Mouse models have been widely used to screen filovirus mAbs [4–8]. However, wild-type filoviruses do not cause any apparent illness in adult, immunocompetent laboratory mice regardless of dose or route of inoculation [9–11]. To cause a lethal disease, filoviruses must first be adapted to mice. Among ebolaviruses, a mouse-adapted variant has been described only for EBOV [11]. The adaptation of filoviruses to mice, at least in part, is associated with altered interactions with the interferon (IFN) system, which plays a critical role in the resistance of mice to ebolavirus infections [12]. During adaptation, viruses overcome this barrier by accumulating mutations, allowing subversion of the murine immune system. Strains of mice with disrupted IFN response therefore represent an alternative model of filovirus infections that does not require adaptation of virus. Knockout (KO) mice lacking the receptor for IFN-α/β (IFNAR) [13] or the cytoplasmic signal transducer and activator of transcription 1 (STAT1) protein are susceptible to infection by wild-type filoviruses [14]. STAT1 signals the binding of IFN-α/β and IFN-γ to cell-surface receptors and is essential for IFN-mediated transcription of genes triggering antiviral state of the cells [15]. However, inoculation of IFNAR KO mice with wild-type BDBV still does not cause clinical signs of disease, weight loss, or lethality [13]. STAT1-deficient mice are susceptible to wild-type EBOV, Sudan ebolavirus, Reston ebolavirus (RESTV), Marburg virus, and Ravn virus [14].
In a previous study, we used an EBOV reverse genetics system to generate chimeric filoviruses in which the sole envelope glycoprotein (GP) was replaced with the counterparts of heterologous filoviruses, with each resulting virus expressing enhanced green fluorescent protein (eGFP) [16]. We demonstrated that these viruses can be used as tools for screening panels of mAbs specific for multiple filoviruses [5]. In this study, we tested feasibility of using one of these viruses for testing mAb treatment in mice.
METHODS
Viruses
The construction of eGFP-expressing EBOV/BDBV-GP virus was published previously [16]. To generate its derivative not expressing eGFP, the full-length clone was digested with BsiWI restriction endonuclease to remove the eGFP gene, and then re-ligated. The resulting plasmid was used to rescue the chimeric EBOV enveloped with BDBV-GP as previously described [17]. The complete nucleotide sequences of the chimeric virus and the corresponding full-length clone, pEBO_BDBV-GP plasmid, have been deposited in GenBank (accession numbers MH464888 and MH464889, respectively). Wild-type BDBV, strain 200706291 Uganda, which was originally isolated from the serum of a patient during the first known outbreak [18], was passaged 3 times in Vero-E6 cells. Wild-type EBOV, strain Mayinga (GenBank accession number AY142960), was obtained from the US Army Medical Research Institute of Infectious Diseases through Dr Heinz Feldmann (while at the Canadian National Microbiology Laboratory, Winnipeg) and Dr Michael R. Holbrook (while at the University of Texas Medical Branch [UTMB]), and passaged 4 times in Vero-E6 cells.
Mice Infection With BDBV and EBOV/BDBV-GP Viruses
The animal protocols for experiments with mice were approved by the UTMB Institutional Animal Care and Use Committee (IACUC). The experiments were performed in the Animal Biosafety Level 4 (ABSL-4) facility of the Galveston National Laboratory. Six- to 7 week-old STAT1 KO mice (129S6/SvEv-Stat1tm1Rds, Taconic Biosciences) at 4–5 animals per group were injected intraperitoneally with 1000 plaque-forming units (PFU) of BDBV or EBOV/BDBV-GP and monitored daily for 28 days. After the onset of symptoms, animals were observed twice a day. The extent of disease was scored using the following parameters: dyspnea (possible score, 0–5), recumbence (0–5), unresponsiveness (0–5), and bleeding/hemorrhage (0–5). Moribund mice were euthanized as per the IACUC-approved protocol. On day 28 after challenge, all remaining animals were euthanized.
Analysis of Viremia
Mice were challenged intraperitoneally with 1000 PFU of wild-type EBOV, BDBV, or EBOV/BDBV-GP (n = 4 animals/group), and monitored for 28 days as described above. Serum samples were collected by retroorbital bleeding on days 3, 5, 7, and 9 postinfection. Samples were serially diluted in Minimum Essential Medium (ThermoFisher Scientific) and titrated in Vero-E6 cell monolayers in duplicate as described elsewhere [7].
Testing of BDBV223 mAbs In Vivo
Mice were challenged intraperitoneally with 1000 PFU of EBOV/BDBV-GP and, 24 hours later, injected with 0.2 mg of BDBV223 or the irrelevant dengue virus (DENV) 2D22–specific antibody (n = 5 animals/group), which was used as a control, and monitored for 28 days as described above.
Statistics and Graphs
Statistical analyses and generation of graphs were performed using GraphPad Prism version 6.05 (GraphPad Software). Log-rank (Mantel-Cox) test was used for analysis of survival data. Unpaired t test was used for analysis of viremia data.
RESULTS
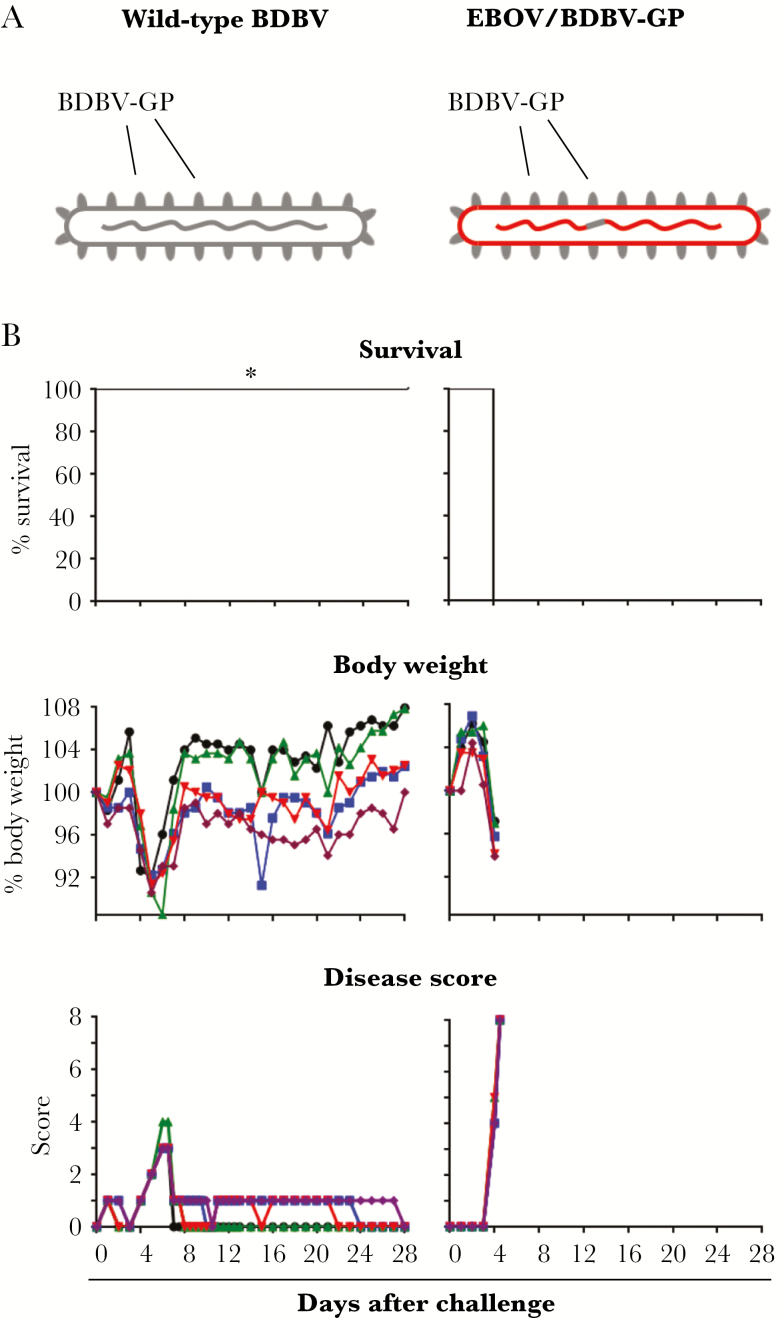
To test if STAT1 KO mice can be used as a model for BDBV infection, we inoculated animals with 1000 PFU of the virus by the intraperitoneal route. However, animals demonstrated only a mild and transient body weight decrease that reached the peak (approximately 10% weight loss) on days 5–6, which was completely restored by days 7–8, with subsequent minor fluctuations (Figure 1B, left panels). This reduction of weight corresponded temporally to the increase in disease score, which did not exceed 4 (mild illness). All animals survived the challenge, suggesting that the deficiency of IFN system in an animal model may be insufficient for the development of lethal infection.
Figure 1.
The chimeric Ebola virus (EBOV) enveloped with Bundibugyo virus (BDBV) glycoprotein (GP), but not wild-type BDBV, causes a uniformly lethal infection in STAT1 knockout mice. A, Schematic representation of BDBV and EBOV/BDBV-GP. The components of BDBV virions are shown in gray, and the components of EBOV virions are shown in red. B, Kaplan–Meier survival curves, body weight, and disease score curves are shown for individual animals (5 animals per group). *Survival difference between groups infected with wild-type BDBV or EBOV/BDBV-GP: P = .0027 (Mantel–Cox test).
As amino acid differences between mouse-adapted and wild-type EBOV include substitutions in VP24 and NP [19], we hypothesized that biological properties of the internal proteins, not the envelope GP, are responsible for the inability of BDBV to cause lethal infection in mice. We therefore made use of the recently described chimeric EBOV-based filovirus enveloped with BDBV-GP [16], which was used successfully for high-throughput screening and characterization of mAbs obtained from the blood of EBOV infection survivors [5]. To avoid a possible interference of an extra gene with virus pathogenicity [20], we removed the reporter eGFP gene from the full-length clone, and used it for the recovery of chimeric EBOV with BDBV-GP envelope EBOV/BDBV-GP (Figure 1A). This chimeric virus was used for the infection of STAT1 KO mice in parallel with wild-type BDBV (Figure 1B, right panels). In contrast to BDBV, EBOV/BDBV-GP caused rapid disease progression, evidenced by soaring of the disease score from 0 on day 3, to scores of 4–5 on day 4, and a score of 8 later on day 4. Reduction of weight also was observed, although the magnitude of the loss did not exceed 6%. All animals succumbed to infection on day 4 (the survival rate difference between wild-type BDBV and EBOV/BDBV-GP: P = .0027, Mantel–Cox test).
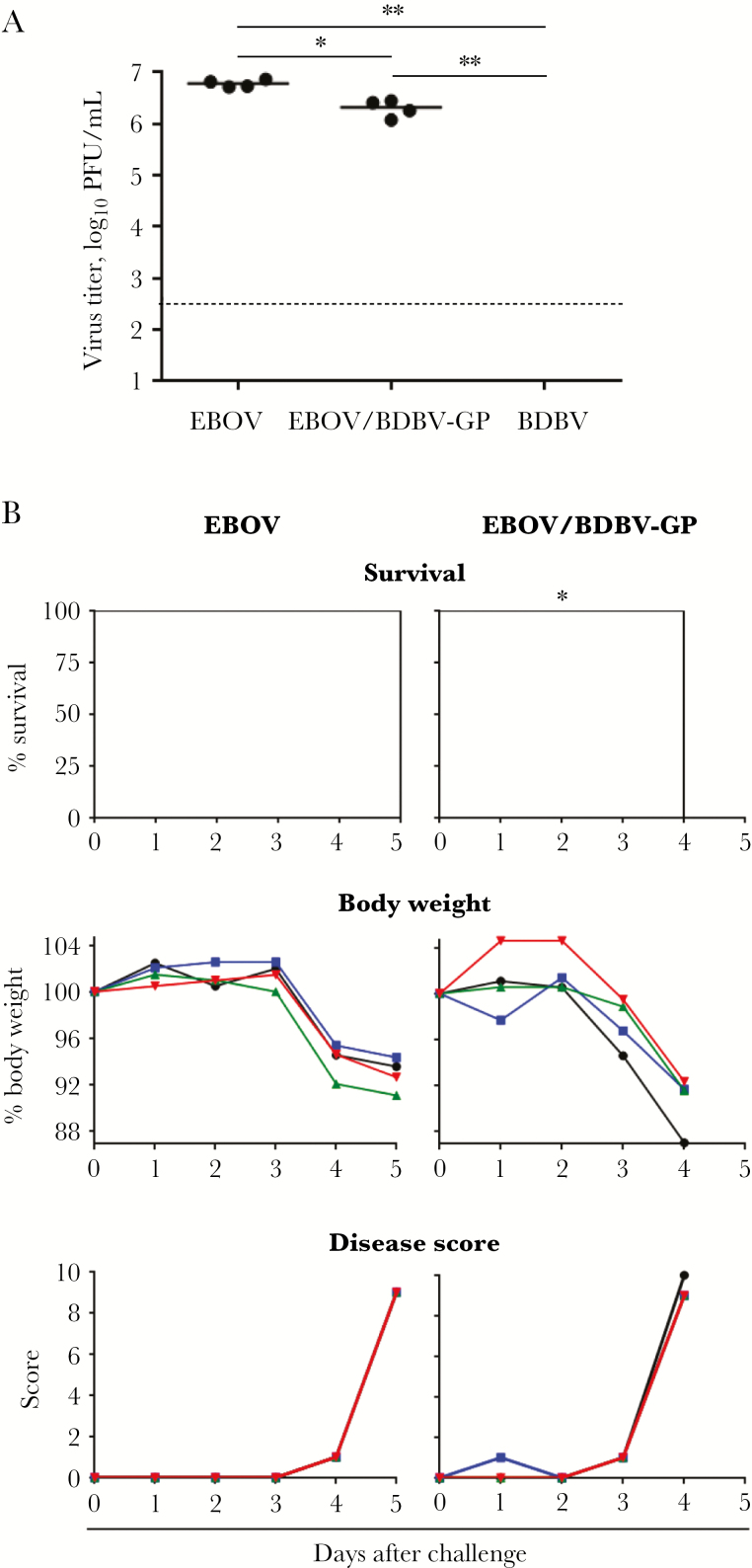
In a separate experiment, the levels of viremia in serum samples of individual STAT1 KO mice infected with EBOV, EBOV/BDBV-GP, or BDBV were analyzed (Figure 2A). On day 3 postinfection, virus titer in the EBOV-infected group was only 2.9-fold higher than those in animals infected with EBOV/BDBV-GP (P = .0019, unpaired t test), with no virus detected in BDBV-infected mice. However, animals infected with EBOV/BDBV-GP succumbed to infection earlier than those infected with EBOV (Figure 2B, day 4 or 5 postinfection, respectively; P = .0082, Mantel–Cox test).
Figure 2.
Ebola virus (EBOV)/Bundibugyo virus (BDBV) glycoprotein (GP) causes faster disease progression than EBOV in STAT1 knockout mice (4 animals per group). A, The levels (plaque-forming units [PFU]) of viremia of individual animals on day 3 after challenge. No virus was detected for BDBV on day 3 or for any virus on days 5, 7, and 9. The limit of detection (2.6 log10) is indicated by the dotted line. The horizontal lines indicate the mean values for each group. *P = .0019, **P < .0001 (unpaired t test). B, Kaplan–Meier survival curves, body weight, and disease score curves are shown for individual animals. *Survival difference between EBOV and EBOV/BDBV-GP groups: P = .0082 (Mantel–Cox test).
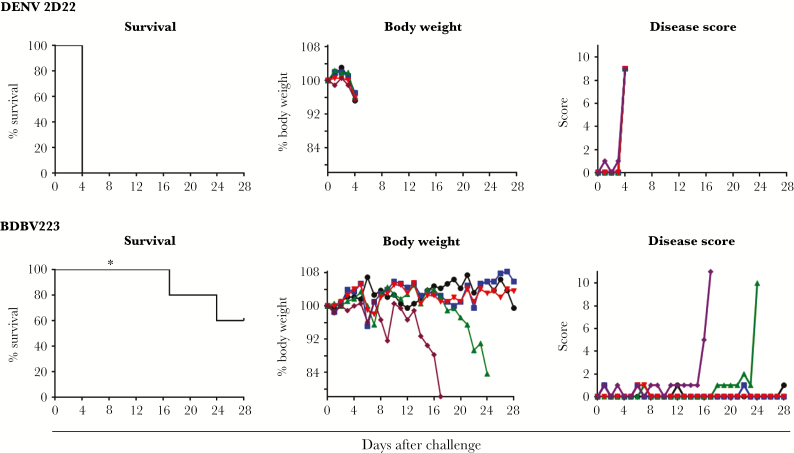
We next tested if STAT1 KO mice can be protected from infection with the chimeric virus by an mAb recognizing its envelope. For this experiment, we used the broadly reactive human mAb BDBV223, which was previously demonstrated to protect immunocompetent BALB/c mice from EBOV infection [5]. Consistent with Figure 1 data, the control animals treated with irrelevant 2D22 antibody specific for DENV at 24 hours after challenge showed signs of rapid disease progression (Figure 3, top row), with all mice succumbing to infection on day 4. In contrast, 3 of 5 animals (60%) treated with mAb BDBV223 survived the infection (Figure 3, bottom row), while the other 2 animals succumbed to infection on days 17 and 22 (the survival rate difference between BDBV223 and 2D22: P = .0027, Mantel–Cox test). Our data suggest that STAT1 KO mouse model of infection with chimeric virus can be used for in vivo screening of protective antibodies targeting BDBV GP.
Figure 3.
Monoclonal antibody (mAb) BDBV223 targeting the Bundibugyo virus (BDBV) glycoprotein (GP) protects STAT1 KO mice from the lethal infection caused by Ebola virus/BDBV-GP. Kaplan–Meier survival curves, body weight, and disease score curves are shown for individual animals (5 animals per group). *Survival difference between the dengue virus (DENV) mAb 2D22 and BDBV223 recipients: P = .0027 (Mantel–Cox test).
DISCUSSION
Ebolaviruses can induce a highly lethal hemorrhagic fever, creating a serious health concern in sub-Saharan Africa. BDBV is one of the ebolavirus species pathogenic for humans and nonhuman primates. Despite the fact that BDBV was discovered >10 years ago, there is still no small-animal model for this infection, which complicates development and screening of antiviral mAbs and drugs. Here, we demonstrate that the chimeric EBOV enveloped with BDBV-GP (EBOV/BDBV-GP), unlike wild-type BDBV, causes a lethal disease in STAT1 KO mice, and that this model can be used for in vivo screening of mAbs targeting BDBV-GP.
STAT1 KO mice lack the key component of the classical JAK-STAT pathway of the IFN system, which renders them deficient in both type I and II IFN responses and susceptible to infection by many, but not all, ebolaviruses [14]. At the same time, several STAT1-independent pathways, such as PI3K, p38, and MEK-ERK, can participate in transduction of IFN signaling [15]. In particular, it was shown that EBOV VP24 can interfere with the p38 MAP kinase pathway by preventing IFN-β–mediated phosphorylation of the alpha isoform of p38, which blocks the downstream cascade of phosphorylation of transcription factors participating in IFN response [21]. However, the role of this inhibitory mechanism in EBOV pathogenesis in vivo remains unclear. The observed differences in virulence of BDBV and EBOV/BDBV-GP suggest that the internal proteins of EBOV are more efficient compared to that of BDBV in suppression of these alternative pathways. These data are consistent with previous studies demonstrating that BDBV replicates in peripheral blood mononuclear cells more slowly than EBOV, produces lower levels of cytokines, and exhibits a significant delay in macrophage apoptosis [22]. Using chimeric EBOV and RESTV with the swapped GPs, Groseth et al showed that, although GP is important for EBOV virulence in vivo, other filovirus proteins also contribute to it [23]. Clearly, the difference in pathogenesis of various ebolaviruses is associated with multiple proteins.
Recently, the ferret model of BDBV infection was described [24, 25]. It was shown that intramuscular or intranasal inoculation of wild-type BDBV causes lethal infection in these animals. However, the use of ferrets for routine in vivo screening of large numbers of BDBV mAbs is not likely to be feasible, given that a high number of these inbred animals per group will be required to generate statistically significant data. Furthermore, the ferret model requires much larger amounts of mAbs and also has a higher cost of housing as compared to mice.
In this study, we demonstrated that the difference in virulence between EBOV and BDBV in STAT1 KO mice is associated with internal viral proteins. Moreover, we developed the first uniformly lethal filovirus model suitable for testing of BDBV-specific antibodies in mice, which does not require adaptation of the virus to mice. The BDBV GP differs approximately 35% from EBOV GP at the amino acid level. As EBOV can tolerate replacement of GP with counterparts of each of the known filovirus [16], the approach we used here is likely to be suitable for rapid development of mouse models for any new filovirus that may emerge in the future using GP sequence even without virus isolation.
Notes
Author contributions. P. A. I. and A. B. conceived the experiments, analyzed data, and wrote the manuscript. P. A. I., J. G., N. K., and K. H. performed experiments. T. G. K. and J. E. C. provided critical resources. J. E. C. and A. B. provided supervision. A. B. conceived of the project.
Acknowledgments. We thank Drs J. Towner and S. Nichol (Centers for Disease Control and Prevention) for providing the EBOV-eGFP full-length clone, and Drs Y. Kawaoka (University of Wisconsin) and H. Feldmann (National Institutes of Health) for providing the EBOV NP, VP35, L, VP30, and T7 polymerase plasmids. We thank the UTMB Animal Resource Center veterinary staff for their excellent technical support of mouse experiments in ABSL-4. This study was supported by the Defense Threat Reduction Agency (grant number HDTRA1-13-1-0034 to J. E. C. and A. B.) and the National Institute of Allergy and Infectious Diseases (grant number U19 AI109711 to J. E. C. and A. B.).
Potential conflicts of interest. All authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Centers for Disease Control and Prevention. Outbreaks chronology: Ebola virus disease Available at: http://www.cdc.gov/vhf/ebola/outbreaks/history/chronology.html. Accessed June 20, 2018.
- 2. Burk R, Bollinger L, Johnson JC, et al. Neglected filoviruses. FEMS Microbiol Rev 2016; 40:494–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mire CE, Geisbert TW. Neutralizing the threat: pan-Ebolavirus antibodies close the loop. Trends Mol Med 2017; 23:669–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Keck ZY, Enterlein SG, Howell KA, et al. Macaque monoclonal antibodies targeting novel conserved epitopes within filovirus glycoprotein. J Virol 2016; 90:279–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Flyak AI, Shen X, Murin CD, et al. Cross-reactive and potent neutralizing antibody responses in human survivors of natural ebolavirus infection. Cell 2016; 164:392–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Holtsberg FW, Shulenin S, Vu H, et al. Pan-ebolavirus and pan-filovirus mouse monoclonal antibodies: protection against Ebola and Sudan viruses. J Virol 2016; 90:266–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Flyak AI, Kuzmina N, Murin CD, et al. Broadly neutralizing antibodies from human survivors target a conserved site in the Ebola virus glycoprotein HR2-MPER region. Nat Microbiol 2018; 3:670–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Flyak AI, Ilinykh PA, Murin CD, et al. Mechanism of human antibody-mediated neutralization of Marburg virus. Cell 2015; 160:893–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bray M. The role of the type I interferon response in the resistance of mice to filovirus infection. J Gen Virol 2001; 82:1365–73. [DOI] [PubMed] [Google Scholar]
- 10. Warfield KL, Bradfute SB, Wells J, et al. Development and characterization of a mouse model for Marburg hemorrhagic fever. J Virol 2009; 83:6404–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bray M, Davis K, Geisbert T, Schmaljohn C, Huggins J. A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J Infect Dis 1998; 178:651–61. [DOI] [PubMed] [Google Scholar]
- 12. Banadyga L, Dolan MA, Ebihara H. Rodent-adapted filoviruses and the molecular basis of pathogenesis. J Mol Biol 2016; 428:3449–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Brannan JM, Froude JW, Prugar LI, et al. Interferon α/β receptor-deficient mice as a model for Ebola virus disease. J Infect Dis 2015; 212(Suppl 2):S282–94. [DOI] [PubMed] [Google Scholar]
- 14. Raymond J, Bradfute S, Bray M. Filovirus infection of STAT-1 knockout mice. J Infect Dis 2011; 204(Suppl 3):S986–90. [DOI] [PubMed] [Google Scholar]
- 15. Platanias LC. Mechanisms of type-I- and type-II-interferon-mediated signalling. Nat Rev Immunol 2005; 5:375–86. [DOI] [PubMed] [Google Scholar]
- 16. Ilinykh PA, Shen X, Flyak AI, et al. Chimeric filoviruses for identification and characterization of monoclonal antibodies. J Virol 2016; 90:3890–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lubaki NM, Ilinykh P, Pietzsch C, et al. The lack of maturation of Ebola virus-infected dendritic cells results from the cooperative effect of at least two viral domains. J Virol 2013; 87:7471–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Towner JS, Sealy TK, Khristova ML, et al. Newly discovered ebola virus associated with hemorrhagic fever outbreak in Uganda. PLoS Pathog 2008; 4:e1000212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ebihara H, Takada A, Kobasa D, et al. Molecular determinants of Ebola virus virulence in mice. PLoS Pathog 2006; 2:e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ebihara H, Theriault S, Neumann G, et al. In vitro and in vivo characterization of recombinant Ebola viruses expressing enhanced green fluorescent protein. J Infect Dis 2007; 196(Suppl 2):S313–22. [DOI] [PubMed] [Google Scholar]
- 21. Halfmann P, Neumann G, Kawaoka Y. The ebolavirus VP24 protein blocks phosphorylation of p38 mitogen-activated protein kinase. J Infect Dis 2011; 204(Suppl 3):S953–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gupta M, Goldsmith CS, Metcalfe MG, Spiropoulou CF, Spipopoulou CF, Rollin PE. Reduced virus replication, proinflammatory cytokine production, and delayed macrophage cell death in human PBMCs infected with the newly discovered Bundibugyo ebolavirus relative to Zaire ebolavirus. Virology 2010; 402:203–8. [DOI] [PubMed] [Google Scholar]
- 23. Groseth A, Marzi A, Hoenen T, et al. The Ebola virus glycoprotein contributes to but is not sufficient for virulence in vivo. PLoS Pathog 2012; 8:e1002847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kozak R, He S, Kroeker A, et al. Ferrets infected with Bundibugyo virus or Ebola virus recapitulate important aspects of human filovirus disease. J Virol 2016; 90:9209–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cross RW, Mire CE, Borisevich V, Geisbert JB, Fenton KA, Geisbert TW. The domestic ferret (Mustela putorius furo) as a lethal infection model for 3 species of ebolavirus. J Infect Dis 2016; 214:565–9. [DOI] [PMC free article] [PubMed] [Google Scholar]