Abstract
Background
In Ebola virus (EBOV) infection, the specific neutralizing activity of convalescent plasma against other members of the Ebolavirus genus has not been extensively analyzed.
Methods
We measured the neutralizing activity in plasma from 3 survivors of the recent outbreak due to the Makona variant of EBOV and tested its neutralizing potency against other variants of EBOV (ie, Mayinga and Kikwit) and against Sudan virus (SUDV), Bundibugyo virus (BDBV), and Reston virus (RESTV), using a glycoprotein (GP)–pseudotyped lentiviral system both with full-length GP and in vitro–cleaved GP (GPCL).
Results
Convalescent plasma specimens from survivors of EBOV infection showed low neutralizing activity against full-length GPs of SUDV, BDBV, RESTV, and EBOV variants Mayinga and Kikwit. However, broad and potent neutralizing activity was observed against the GPCL forms of SUDV, BDBV, and RESTV.
Discussion
Removal of the mucin-like domain and glycan cap from the GP of members of the Ebolavirus genus presumably exposes conserved epitopes in or in the vicinity of the receptor binding site and internal fusion loop that are readily amenable to neutralization. These types of broad neutralizing antibodies could be induced by using immunogens mimicking GPCL.
Keywords: Ebola virus, glycoprotein, convalescent patients, neutralization assay
The magnitude of the recent outbreak of Ebola virus disease (EVD) in West Africa has stimulated research in the field of emergent agents with high pathogenicity, and it is clear that a better understanding of the pathogenic mechanisms and the immune response to natural infection will be necessary for the design of preventive and therapeutic interventions to minimize the tremendous impact of these rapidly spreading outbreaks [1, 2]. The specificity and kinetics of the neutralizing antibody (NAb) response in patients with active or convalescent-phase Ebola virus (EBOV) infection are not completely clear. A very limited number of studies have characterized the specific neutralizing activity against other members of the Ebolavirus genus in EVD survivors. Moreover, it is not clear whether survivors are protected against homologous or heterologous ebolavirus. The precise mechanism of EBOV neutralization by Abs is not fully understood. This knowledge is important since the neutralizing mechanism plays a crucial role in predicting long-term protection in both survivors of natural infection and vaccinated individuals.
Ebolavirus exhibits a complex process of cellular interaction and entry before actual fusion is produced in the late endosomal compartment. During the process of ebolavirus entry, the cleavage of the virion-associated glycoprotein (GP) by host cell cathepsins removes the glycan cap and mucin-like domains (MLDs), producing another, functionally distinct form of GP (GPCL). The cleavage of GP is thought to expose the receptor-binding site and, upon interaction with the late endosomal receptor NPC-1 [3, 4], mediates fusion of viral and cellular membranes [5–7]. It has been previously proposed that Abs against MLD and the glycan cap are generally nonneutralizing, most likely because they are removed together with their epitopes from viral particles once endocytosis occurs [8]. On the other hand, a number of NAbs were shown to remain attached during GP enzymatic processing because they were positioned at sites where they could prevent rearrangements necessary for viral fusion [9].
A wide variety of human monoclonal Abs (mAbs) against ebolavirus have recently been characterized. Furuyama et al reported the generation of an ebolavirus GP–specific mAb 6D6 that was directed against the highly conserved internal fusion loop, thereby preventing cell-virus membrane fusion. The 6D6 antibody was shown to successfully prevent cellular entry in vitro by isolates from all Ebolavirus species and to protect against virus infection in a mouse model [10]. Bornholdt et al isolated and characterized 349 GP-specific Abs from peripheral B cells of a convalescent patient from the latest West Africa outbreak. They showed that >77% of the isolated mAbs were able to neutralize live EBOV, but they did not detect broad species cross-reactivity. The most potent NAbs were shown to be directed against the GP1/GP2 interface and the GP stalk region [11]. Howell et al identified a mAb FVM04 that targets the receptor-binding site of ebolavirus GP and blocks interaction with its endosomal receptor, NPC1. FMV04 cross-neutralizes EBOV, Sudan virus (SUDV), and Bundibugyo virus (BDBV) and protects against EBOV and SUDV in mice and guinea pig models [12]. Although it has been previously suggested that the glycan cap and MLD mAbs may not neutralize well because these regions are removed by cathepsins during virus entry [9], Flyak et al observed that a large panel of neutralizing human mAbs directed against BDBV bound to the glycan cap region. mAbs in this study, which were isolated using peripheral blood B cells from convalescent patients from the 2007 BDBV outbreak in Uganda, showed high neutralization potency against multiple ebolaviruses, including EBOV and SUDV [13]. In a recent study by Zhao et al, CA45, a broad NAb targeting a region within the internal fusion loop and the N-terminal part of the ebolavirus GP, was isolated from a macaque immunized with EBOV, SUDV, and Marburg virus (MARV) GP lacking MLD [14]. CA45 potently neutralized EBOV, SUDV, BDBV, and Reston virus (RESTV) and provided full protection against infection in mouse, guinea pig, and ferret models. In this study, memory B cells encoding broad NAbs against ebolavirus were present at very low frequencies (0.06%). Interestingly, it was observed that, although the CA45 germ-line precursor bound poorly to full-length GPs, it exhibited high affinity to GPCL, probably because of the better access to the epitopes on the processed form of GPs [14]. In a different approach to search for broadly NAbs, Wec et al [15] used a library of EBOV-GP mAbs from a convalescent patient [11] and identified 2 mAbs, ADI-15742 and ADI-15878, that potently cross-neutralized EBOV, SUDV, and BDBV. These broadly NAbs recognized preferentially conserved residues in the GP2 internal fusion loop after GP cleavage [15].
There is limited information about the breadth of the neutralizing response against other potential variants of ebolavirus after natural infection. We have recently shown that the neutralizing response in convalescent plasma specimens from patients is variant specific and appears to increase up to several months after infection [16]. In this study, we analyzed the neutralizing activity in convalescent plasma specimens from 3 survivors of the recent outbreak due to the Makona variant of EBOV, followed from 2–3 months through 9–18 months after infection, and tested the neutralizing potency of the specimens against other variants of EBOV (ie, Mayinga, Makona, and Kikwit), SUDV, BDBV, and RESTV members of the genus ebolavirus, with both full-length GP and the cleaved form (GPCL).
MATERIALS AND METHODS
Patients
The study was approved by the ethics committee and institutional review board at Hospital Universitario La Paz (Madrid, Spain). Written informed consent was obtained from all participants. Convalescent plasma specimens from 3 patients with EVD were studied. Patients 1 and 2 were black, female missionaries aged 36 and 45 years, respectively, involved in healthcare activity in Liberia and received a diagnosis of EVD in August 2014. Both were admitted to a local Ebola treatment unit and discharged after 15 and 18 days upon clinical recovery. Patient 3 was a female nurse assistant aged 44 years who was infected in Madrid, Spain, in October 2014 while providing healthcare to a patient with EVD who had been evacuated from Sierra Leone. She had a severe form of disease and was discharged from the isolation unit after 34 days. Convalescent patient 3 received supportive care, high-dose favipiravir for 10 days, and 5 units of convalescent plasma obtained from patient 1 (2 units, 200 mL each) and patient 2 (3 units, 200 mL each) 2 months after infection [16, 17]. Patients 1 and 2 received standard supportive treatment in local Ebola treatment units in West Africa. Blood samples were obtained in ethylenediaminetetraacetic acid–lined tubes at the following time points: 2 months after infection (for patients 1 and 2), 3 months after infection (for patients 1–3), 4 months after infection (for patient 1), 9 months after infection (for patient 1) and 18 months after infection (for patient 3).
Enzyme-Linked Immunosorbent Assay (ELISA)–Based Detection of Human Anti-EBOV GP
For total anti–EBOV-GP immunoglobulin G (IgG) detection in convalescent plasma samples, the Recombivirus Human Anti-Zaire Ebola Virus Glycoprotein IgG ELISA kit (Alpha Diagnostic International, San Antonio, TX) was performed according to the manufacturer’s instructions, using a 1:500 dilution of plasma.
Production of Filoviral GP–Pseudotyped Particles
An EBOV-GP–pseudotyped lentiviral system was used to test neutralizing activity. Briefly, human embryonic kidney 293 T cells were plated at a density of 3 × 106 cells per 10-cm diameter tissue culture dish and, after overnight incubation, were transfected with pNL4-3.Luc.R–.E– (kindly provided by Dr Nathaniel Landau via the National Institutes of Health [NIH] AIDS Reagent Program, Division of AIDS, National Institute of Allergy and Infectious Diseases, NIH, Bethesda, MD) [18] and EBOV-GP expression vectors, using a standard calcium chloride transfection protocol (Life Technologies, Carlsbad, CA). Expression plasmids for the GP of EBOV strain Mayinga (GenBank accession no. U23187.1) and RESTV (GenBank accession no. U23152.1) were kindly provided by Anthony Sanchez, Centers for Disease Control and Prevention (Atlanta, GA). EBOV strain Makona GP (GenBank accession no. KM233102.1) [19, 20], EBOV strain Kikwit GP (GenBank accession no. AY354458.1), SUDV (GenBank accession no. NC_006432), and BDBV (GenBank accession no. FJ217161.1) were synthesized and cloned into pcDNA3.1 by GeneArt AG technology (Life Technologies, Regensburg, Germany). Supernatants containing GP-pseudotyped viruses were harvested 48 hours later, centrifuged to remove cell debris, and stored in aliquots at -80°C. Infectious titers were estimated as the number of tissue culture infective doses per milliliter by performing a limiting dilution (1:5 serial dilutions in triplicate) of the lentivirus-containing supernatants on HeLa cells. Luciferase activity was determined by luciferase assay (Luciferase Assay System, Promega, Madison, WI) in a GloMax-Multi+ Detection System (Promega).
In Vitro Cleavage of EBOV-GP Particles
Cleavage of EBOV-GP–pseudotyped particles was performed by incubating the virus with 200 µg/mL of thermolysin (Sigma) for 1 hour at 37°C. After incubation, the reaction was stopped by adding 1 mM phosphoramidon (Sigma) and incubating the specimens on ice for 20 minutes. For infectivity studies, native and cleaved particles were then added to 2 × 104 HeLa cells/well in 96-well plates, and infection was measured 48 hours later.
EBOV-GP Neutralizing Assays
Convalescent plasma samples from patients and a plasma specimen from a healthy blood donor were heat inactivated at 56°C for 30 minutes and tested in duplicate or triplicate in at least 3 independent assays. Virus-containing supernatants from transfection plates were normalized for infectivity and an inoculum equivalent to a multiplicity of infection (MOI) of 0.05 was used in the neutralizing experiments. Full-length GPs and in vitro–processed, GPCL-pseudotyped lentiviral particles were incubated with diluted plasma samples at 37°C for 1 hour in 96-well plates. After incubation, 2 × 104 HeLa cells were seeded onto the virus-plasma mixture and incubated in a total volume of 100 µL per well. At 48 hours after infection, cells were lysed and assayed for luciferase expression as described above. The 50% inhibitory concentration (IC50) and IC90 were estimated by testing samples in triplicate along a range of 2-fold dilutions, from 1:100 to 1:6400, and using a nonlinear regression model fit with settings for log inhibitor versus normalized response curves, in GraphPad Prism, version 6.
RESULTS
Anti–EBOV-GP IgG Detection in Convalescent Plasma Specimens
Levels of EBOV-GP–specific IgG detected by a commercial ELISA were high at all time points in plasma samples collected from patients 2–18 months after infection (Supplementary Figure 1).
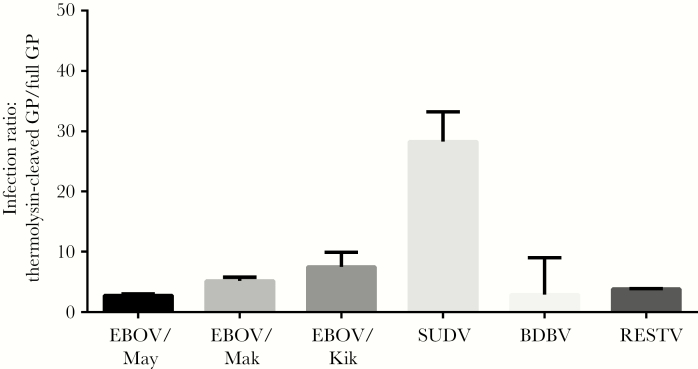
Infectivity of GP-Pseudotyped Particles Cleaved In Vitro
After in vitro cleavage of GP-pseudotyped viral particles, increased infectivity of GPCL as compared to full-length GPs was observed for EBOV, SUDV, BDBV, and RESTV, with a 2.7-fold increase for EBOV Mayinga GPCL, a 4.9-fold increase for EBOV Makona GPCL, a 3.9-fold increase for EBOV Kikwit GPCL, a 28.4-fold increase for SUDV GPCL, a 2.8-fold increase for BDBV GPCL, and a 3.4-fold increase for RESTV GPCL (Figure 1).
Figure 1.
Increased infectivity of filovirus glycoprotein (GP)–pseudotyped particles after thermolysin treatment. Bars represent infection ratios, expressed as relative infection for cleaved filovirus GP in relation to the native form (GPCL/GP). Data are mean values from triplicate analyses in 3 independent experiments. Error bars correspond to standard errors of the mean. Abbreviations: BDBV, Bundibugyo virus; EBOV/Kik, Ebola virus Kikwit; EBOV/Mak, Ebola virus Makona; EBOV/May, Ebola virus Mayinga; RESTV, Reston virus; SUDV, Sudan virus.
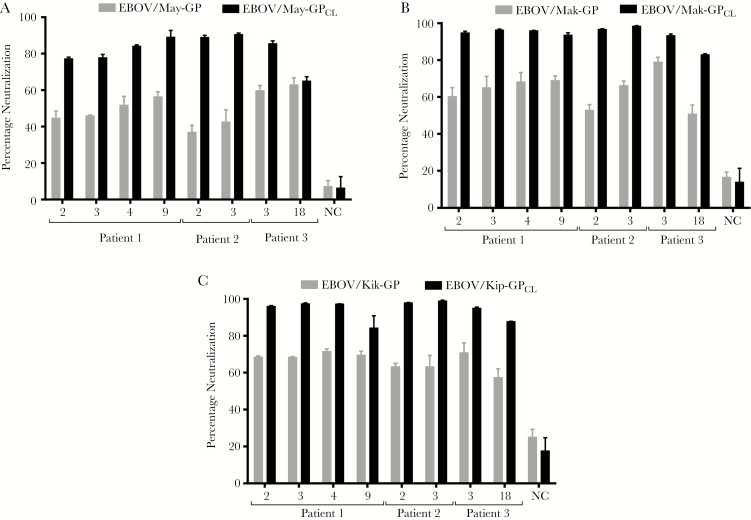
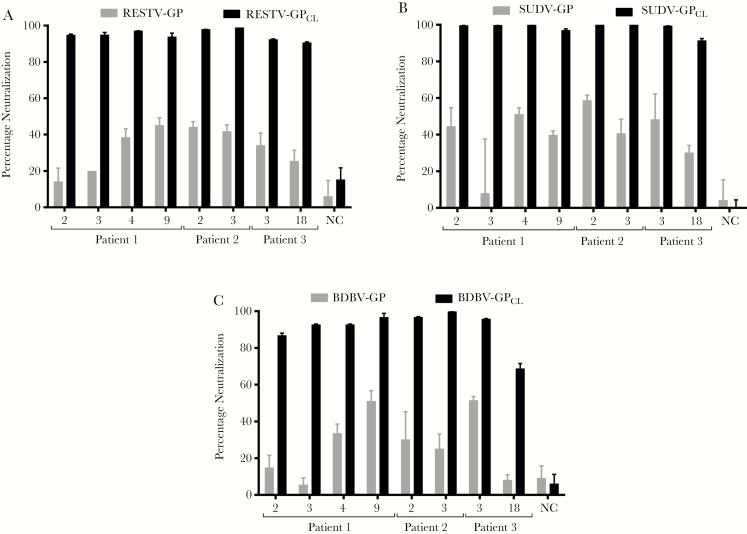
Neutralizing Activity Against GPs and GPCL of EBOV Mayinga, EBOV Makona, EBOV Kikwit, SUDV, BDBV, and RESTV Among Convalescent Plasma Specimens
Neutralizing activity was first measured in plasma specimens diluted to 1:200 after heat inactivation at 56°C for 30 minutes (Figures 2 and 3). The EBOV GP–specific neutralizing titer was higher against both EBOV Makona and Kikwit variants as compared to that against EBOV Mayinga at most time points tested. The GP-specific neutralizing titer increased from 2 to 9 months after infection and decreased thereafter for the single individual (patient 3) from whom plasma was collected 18 months after infection (Figure 2). Lower neutralizing activity against RESTV, SUDV, and BDBV GPs was detected, with the highest neutralization level reaching 40%–50% at the 1:200 plasma dilution. After thermolysin treatment, the neutralization potency increased considerably against EBOV GPCL and especially against RESTV, SUDV, and BDBV GPCL, which were neutralized 90%–100% by plasma at 1:200 dilutions (Figure 3).
Figure 2.
Neutralizing activity against full-length glycoprotein (GP)– and cleaved GP (GPCL)–pseudotyped Ebola virus particles in convalescent plasma specimens from patients with Ebola virus disease. Bars represent neutralization activity of plasma in an infection assay, expressed as the percentage neutralization (expressed as mean values [±standard errors of the mean] from triplicate analyses) as compared to the infectivity obtained without addition of any plasma sample (y-axis). Convalescent plasma samples from 3 patients were heat inactivated and tested at a dilution of 1:200. Abbreviations: EBOV/Kik, Ebola virus Kikwit; EBOV/Mak, Ebola virus Makona; EBOV/May, Ebola virus Mayinga; NC, noninfected control.
Figure 3.
Neutralizing activity against full-length glycoprotein (GP)– and cleaved GP (GPCL)–pseudotyped Reston virus (RESTV), Sudan virus (SUDV), and Bundibugyo virus (BDBV) particles in convalescent plasma specimens from patients with Ebola virus disease. Bars represent the percentage neutralization (expressed as mean values [±standard errors of the mean] from duplicate analyses) in an infection assay as compared to the infectivity obtained in the absence of any plasma sample (y-axis). Plasma samples from 3 convalescent patients were heat inactivated and tested at a dilution of 1:200. Abbreviation: NC, noninfected control.
Since there was probable saturation of neutralizing activity against GPCL by plasma diluted 1:200, a 500-fold dilution was tested against EBOV Makona, using convalescent plasma samples from patient 1. At a 1:500 dilution, the neutralizing activity against the full-length EBOV Makona GP was greatly reduced, but the neutralizing capacity against the GPCL form was very effective as early as 2 months after infection (Supplementary Figure 2).
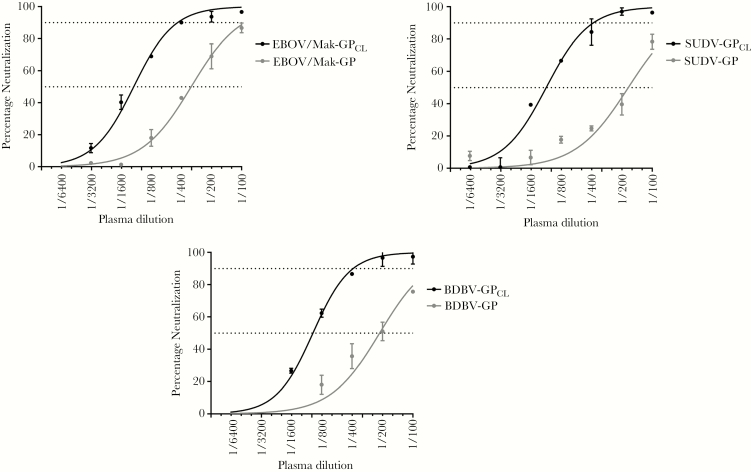
Additionally, IC50 and IC90 were estimated for EBOV Makona, SUDV, and BDBV GP and GPCL in the plasma sample collected from patient 1 nine months after infection (Figure 4 and Table 1).
Figure 4.
Neutralizing activity against full-length glycoprotein (GP)– and cleaved GP (GPCL)–pseudotyped Ebola virus Makona (EBOV/Mak), Sudan virus (SUDV), and Bundibugyo virus (BDBV) in a convalescent plasma specimen from patient 1. Values represent mean values (±standard errors of the mean) of triplicate analyses. Curves were obtained using a nonlinear regression model fit with settings for log inhibitor versus normalized response curves, in GraphPad Prism, version 6.
Table 1.
Neutralizing Activity Against Full-Length Glycoprotein (GP)– and Cleaved GP (GPCL)–Pseudotyped Ebola Virus Makona, Sudan Virus (SUDV), and Bundibugyo Virus (BDBV) in Convalescent Plasma Specimens From Patient 1
| Variable | EBOV Makona, Dilution (95% CI) | SUDV, Dilution (95% CI) | BDBV, Dilution (95% CI) | |||
|---|---|---|---|---|---|---|
| GP | GPCL | GP | GPCL | GP | GPCL | |
| IC 50 | 1/319 (1/386 to 1/263) |
1/1196 (1/1433 to 1/998) |
1/172 (1/231 to 1/129) |
1/1122 (1/1236 to 1/1019) |
1/213 (1/306 to 1/149) |
1/974 (1/1058 to 1/897) |
| IC 90 | 1/92 (1/112 to 1/76) |
1/435 (1/625 to 1/308) |
1/46 (1/61 to 1/34) |
1/382 (1/467 to 1/315) |
1/62 (1/89 to 1/43) |
1/389 (1/463 to 1/329) |
Neutralizing activity was estimated in triplicate by an infection assay along a range of dilutions (from 1:100 to 1:6400), using GraphPad Prism, version 6.
Abbreviations: CI, confidence interval; IC50, 50% inhibitory concentration; IC90, 90% inhibitory concentration.
DISCUSSION
Cathepsin L and cathepsin B cleave GP1, removing the regions containing the glycan cap and MLD. It was previously demonstrated that in vitro cleavage of particles with thermolysin functionally mimics the cleavage due to the combination of cathepsin L and cathepsin B. The MLD was shown to be dispensable for the infection in cell culture, and particles lacking this region were fully competent for entry and infection [7, 21]. It has also been shown that virions treated with cathepsin L and thermolysin exhibit higher infectivity and greater cell binding activity as compared to untreated virions [5, 21, 22]. As expected, this increased infectivity of GPCL forms has been confirmed in our study and extended to SUDV, BDBV, and RESTV (Figure 1).
The recent observation of broad NAbs whose germ-line precursors bound poorly to full-length GPs but were able to efficiently neutralize GPCL [14, 15] encouraged us to study the neutralizing potency against both forms of GP among convalescent plasma specimens from patients in the recent EVD outbreak. Treatment based on passive transfer of Abs has been tested in a very limited number of studies, and the specificity and kinetics of the neutralizing response in infected and convalescent patients have not been completely described yet [16, 23, 24]. In our study, the specific neutralizing titer of convalescent plasma from patients with EVD in the 2013–2016 West African outbreak was significantly higher against EBOV Makona and EBOV Kikwit GPs as compared to other ebolaviruses, including the EBOV Mayinga GP variant. Although EBOV Mayinga GP was neutralized less efficiently in comparison to EBOV Makona and EBOV Kikwit GPs, it was still much better neutralized than other members of the Ebolavirus genus [16]. There was an increasing trend in the GP-specific neutralizing titer between 2 and up to 9 months after infection when tested against EBOV Mayinga and EBOV Makona GPs, although it was not seen for EBOV Kikwit GP under these assay conditions (Figure 2). There was no appreciable neutralizing activity detected against RESTV and BDBV GPs. The neutralization potency against SUDV GP was fairly better than against RESTV and BDBV, but there was no apparent increase in the neutralizing titer over time after clinical recovery (Figure 3).
This neutralizing titer increased significantly upon GP cleavage by thermolysin treatment, and the breadth of the activity expanded to other members of the Ebolavirus genus, such as SUDV, BDBV, and RESTV (Figures 2 and 3). The significant increase in the neutralizing potency against GPCL-pseudotyped particles was found in all convalescent samples at each time point tested, including the earliest months after infection. Interestingly, poor neutralization against GPs from SUDV, BDBV, and RESTV in convalescent plasma specimens reached 90%–100% against GPCL forms at 1:200 dilutions (Figure 3).
Convalescent plasma samples obtained 2, 3, 4, and 9 months after infection from patient 1 were tested for neutralizing activity against EBOV Makona at a 1:500 dilution. Neutralizing potency against GPCL was remarkable as early as 2 months after infection (approximately 80% neutralization), with a slightly increasing trend in the GPCL-specific neutralizing titer up to 9 months after infection (Supplementary Figure 2). The vulnerability of the GPCL forms to NAbs was further highlighted by determining specific neutralizing end points for the specimen obtained 9 months after infection from patient 1, with IC50 and IC90 titers 6- and 8-fold greater, respectively, for SUDV GPCL and 4- and 6-fold greater, respectively, for BDBV GPCL (Figure 4 and Table 1)
In addition to EBOV VP24 and VP35, viral proteins that act as strong inhibitors of interferon production and signaling and thus interfere with the early innate host response [25], GP is considered a major determinant of pathogenicity [26, 27] and the main target of NAbs [9, 28]. Access to important domains in GP is masked by the heavily N- and O-glycosylated MLD. The O-linked glycosylation found on the EBOV GP MLD were proposed to adopt an extended conformation that acts as a shield to protect GP from NAbs [29]. A glycan shield model has also been previously suggested as a mechanism to evade host immune recognition in the case of human immunodeficiency virus GPs [30]. Since the majority of EBOV-specific Abs reported so far recognize continuous epitopes in the MLD [31], the cleavage of the GP by host cell cathepsins was suggested to uncover critical NAb binding sites within conserved domains of the RBD [32]. Three main neutralization mechanisms for ebolaviruses have been described. The first mechanism was based on inhibition of cathepsin-mediated cleavage. The second involved blocking of NPC1 binding and the last targeted mechanical interference that prevents GP2 structural rearrangements required for GP fusion [33]. Before the recent outbreak, several neutralizing mAbs against ebolavirus GPs were shown to be protective in animal models, but they were only effective against specific EBOV variants [34, 35]. Therefore, there is a need for cross-reacting mAbs against different Ebolavirus species that could be used as universal EVD therapy [10]. A number of recent studies have characterized potent broad NAbs directed against these neutralizing epitopes [12, 13]. Of importance, these studies identified broad NAbs that target the conserved epitopes in the receptor-binding site and internal fusion loop domains that are difficult to access in the native conformation of the GP [14, 15].
Our results indicate that cross-reactive potent NAbs are present in convalescent plasma samples even at early times after clinical recovery. The presence of the dense glycan shield on ebolavirus GPs precludes access to their neutralizing epitopes presumably in the conserved receptor-binding site and internal fusion loop domain, as has been demonstrated for the broad NAbs CA45, ADI-15742, and ADI-15978 [14, 15]. Further studies are necessary to characterize the site of recognition of these NAbs. These findings, together with characterization of the new broad NAbs, could be used to improve the design of broadly protective immunogens through the removal of GP immunodominant domains such as MLD and the glycan cap and, thus, enhance presentation of conserved epitopes in the receptor-binding site and internal fusion loop [14, 15]
Our study is limited by the small number of individuals analyzed and by the infection model used, in which GP-pseudotyped lentiviral particles, although largely used in pathogenic and drug-discovery studies involving EBOV [16, 36, 37], might not completely reproduce the complexities of viral entry of a different viral particle. Nevertheless, these preliminary observations support the concept that potent broad NAbs are present in convalescent blood specimens from patients with EVD. Whether the production of these Abs after natural infection can be enhanced by vaccines containing immunogens that resemble the conserved domains of GPCL deserves further investigation.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Financial support. This work was supported by Instituto de Investigación Carlos III (grants FIS PI 1400708 and DTS 1500171) and by the European Union Commission VIRUSCAN Future and Emerging Technologies Proactive 2016, under the 731868-Horizon 2020 Framework Programme by the European Union Commission Horizon 2020 Framework Programme: Project VIRUSCAN FETPROACT-2016: 731868.
Potential conflicts of interest. All authors: No reported conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Muñoz-Fontela C, McElroy AK. Ebola virus disease in humans: pathophysiology and immunity. Curr Top Microbiol Immunol 2017; 411:141–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Team WER. After Ebola in West Africa — unpredictable risks, preventable epidemics. N Engl J Med 2016; 375:587–96. [DOI] [PubMed] [Google Scholar]
- 3. Côté M, Misasi J, Ren T, et al. Small molecule inhibitors reveal Niemann-Pick C1 is essential for Ebola virus infection. Nature 2011; 477:344–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Carette JE, Raaben M, Wong AC, et al. Ebola virus entry requires the cholesterol transporter Niemann-Pick C1. Nature 2011; 477:340–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chandran K, Sullivan NJ, Felbor U, Whelan SP, Cunningham JM. Endosomal proteolysis of the Ebola virus glycoprotein is necessary for infection. Science 2005; 308:1643–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Schornberg K, Matsuyama S, Kabsch K, Delos S, Bouton A, White J. Role of endosomal cathepsins in entry mediated by the Ebola virus glycoprotein. J Virol 2006; 80:4174–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dube D, Brecher MB, Delos SE, et al. The primed ebolavirus glycoprotein (19-kilodalton GP1,2): sequence and residues critical for host cell binding. J Virol 2009; 83:2883–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Martinez O, Tantral L, Mulherkar N, Chandran K, Basler CF. Impact of Ebola mucin-like domain on antiglycoprotein antibody responses induced by Ebola virus-like particles. J Infect Dis 2011; 204(Suppl 3):S825–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Murin CD, Fusco ML, Bornholdt ZA, et al. Structures of protective antibodies reveal sites of vulnerability on Ebola virus. Proc Natl Acad Sci U S A 2014; 111:17182–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Furuyama W, Marzi A, Nanbo A, et al. Discovery of an antibody for pan-ebolavirus therapy. Sci Rep 2016; 6:20514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bornholdt ZA, Turner HL, Murin CD, et al. Isolation of potent neutralizing antibodies from a survivor of the 2014 Ebola virus outbreak. Science 2016; 351:1078–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Howell KA, Qiu X, Brannan JM, et al. Antibody treatment of ebola and sudan virus infection via a uniquely exposed epitope within the glycoprotein receptor-binding site. Cell Rep 2016; 15:1514–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Flyak AI, Shen X, Murin CD, et al. Cross-reactive and potent neutralizing antibody responses in human survivors of natural Ebolavirus infection. Cell 2016; 164:392–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zhao X, Howell KA, He S, et al. Immunization-elicited broadly protective antibody reveals ebolavirus fusion loop as a site of vulnerability. Cell 2017; 169:891–904 e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wec AZ, Herbert AS, Murin CD, et al. Antibodies from a human survivor define sites of vulnerability for broad protection against ebolaviruses. Cell 2017; 169:878–90 e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Luczkowiak J, Arribas JR, Gómez S, et al. Specific neutralizing response in plasma from convalescent patients of Ebola virus disease against the West Africa Makona variant of Ebola virus. Virus Res 2016; 213:224–9. [DOI] [PubMed] [Google Scholar]
- 17. Mora-Rillo M, Arsuaga M, Ramírez-Olivencia G, et al. ; La Paz-Carlos III University Hospital Isolation Unit Acute respiratory distress syndrome after convalescent plasma use: treatment of a patient with Ebola virus disease contracted in Madrid, Spain. Lancet Respir Med 2015; 3:554–62. [DOI] [PubMed] [Google Scholar]
- 18. Connor RI, Chen BK, Choe S, Landau NR. Vpr is required for efficient replication of human immunodeficiency virus type-1 in mononuclear phagocytes. Virology 1995; 206:935–44. [DOI] [PubMed] [Google Scholar]
- 19. Gire SK, Goba A, Andersen KG, et al. Genomic surveillance elucidates Ebola virus origin and transmission during the 2014 outbreak. Science 2014; 345:1369–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kuhn JH, Andersen KG, Baize S, et al. Nomenclature- and database-compatible names for the two Ebola virus variants that emerged in Guinea and the Democratic Republic of the Congo in 2014. Viruses 2014; 6:4760–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kaletsky RL, Simmons G, Bates P. Proteolysis of the Ebola virus glycoproteins enhances virus binding and infectivity. J Virol 2007; 81:13378–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jeffers SA, Sanders DA, Sanchez A. Covalent modifications of the ebola virus glycoprotein. J Virol 2002; 76:12463–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. van Griensven J, De Weiggheleire A, Delamou A, et al. The use of Ebola convalescent plasma to treat Ebola virus disease in resource-constrained settings: a perspective from the field. Clin Infect Dis 2016; 62:69–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mire CE, Geisbert JB, Agans KN, et al. Passive immunotherapy: assessment of convalescent serum against Ebola virus makona infection in nonhuman primates. J Infect Dis 2016; 214:367–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Basler CF. Innate immune evasion by filoviruses. Virology 2015; 479-480:122–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Yang Z, Delgado R, Xu L, et al. Distinct cellular interactions of secreted and transmembrane Ebola virus glycoproteins. Science 1998; 279:1034–7. [DOI] [PubMed] [Google Scholar]
- 27. Yang ZY, Duckers HJ, Sullivan NJ, Sanchez A, Nabel EG, Nabel GJ. Identification of the Ebola virus glycoprotein as the main viral determinant of vascular cell cytotoxicity and injury. Nat Med 2000; 6:886–9. [DOI] [PubMed] [Google Scholar]
- 28. Wong G, Kobinger GP, Qiu X. Characterization of host immune responses in Ebola virus infections. Expert Rev Clin Immunol 2014; 10:781–90. [DOI] [PubMed] [Google Scholar]
- 29. Jentoft N. Why are proteins O-glycosylated?Trends Biochem Sci 1990; 15:291–4. [DOI] [PubMed] [Google Scholar]
- 30. Wei X, Decker JM, Wang S, et al. Antibody neutralization and escape by HIV-1. Nature 2003; 422:307–12. [DOI] [PubMed] [Google Scholar]
- 31. Wilson JA, Hevey M, Bakken R, et al. Epitopes involved in antibody-mediated protection from Ebola virus. Science 2000; 287:1664–6. [DOI] [PubMed] [Google Scholar]
- 32. Shedlock DJ, Bailey MA, Popernack PM, Cunningham JM, Burton DR, Sullivan NJ. Antibody-mediated neutralization of Ebola virus can occur by two distinct mechanisms. Virology 2010; 401:228–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Saphire EO, Aman MJ. Feverish quest for Ebola immunotherapy: straight or cocktail?Trends Microbiol 2016; 24:684–6. [DOI] [PubMed] [Google Scholar]
- 34. Qiu X, Audet J, Wong G, et al. Successful treatment of ebola virus–infected cynomolgus macaques with monoclonal antibodies. Sci Transl Med 2012; 4:138ra81. [DOI] [PubMed] [Google Scholar]
- 35. Qiu X, Wong G, Audet J, et al. Reversion of advanced Ebola virus disease in nonhuman primates with ZMapp. Nature 2014; 514:47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Marzi A, Akhavan A, Simmons G, et al. The signal peptide of the ebolavirus glycoprotein influences interaction with the cellular lectins DC-SIGN and DC-SIGNR. J Virol 2006; 80:6305–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Barrientos LG, Lasala F, Otero JR, Sanchez A, Delgado R. In vitro evaluation of cyanovirin-N antiviral activity, by use of lentiviral vectors pseudotyped with filovirus envelope glycoproteins. J Infect Dis 2004; 189:1440–3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.