Abstract
Black patients with chronic kidney disease (CKD) receive more cardiopulmonary resuscitation (CPR) than other racial groups, and knowledge of CPR influences preferences for care. As limited health literacy disproportionately affects Blacks and contributes to disparities in end-of-life (EOL) care, we investigated whether health literacy mediates racial disparities in CPR knowledge. Black and White adult patients with advanced CKD completed CPR knowledge surveys. Health literacy was assessed using the Rapid Estimate of Adult Literacy in Medicine. Among 149 patients, Black patients were more likely to have limited health literacy and lower mean CPR knowledge scores than White patients. In adjusted analyses, health literacy mediated racial differences in CPR knowledge. Knowledge of CPR is lower among Black compared with White CKD patients and health literacy is a mediator of this difference. Future CPR educational interventions should target health literacy barriers to improve informed decision-making and decrease racial disparities at the end-of-life.
Keywords: Racial disparities, end of life, chronic kidney disease, CPR knowledge, advance directives, advance care planning
Patients with chronic kidney disease (CKD) are at high risk of developing arrhythmias that lead to sudden cardiac arrest; however, patients with CKD have a much lower rate of survival after cardiopulmonary resuscitation (CPR) compared with other patient populations.1–5 Furthermore, studies of patients with CKD who progress to end-stage renal disease and receive dialysis show that Black patients are more likely to receive CPR compared with White patients—these disparate trends have persisted over time.4, 6, 7 Patients’ decisions about whether they should undergo CPR are a key part of informed decision-making, goals of care discussions, and completion of advance directives. Therefore, understanding racial differences in patient knowledge of CPR may provide insight into differences in patterns of end-of-life (EOL) care between racial groups in this patient population.6, 8
Racial disparities in EOL treatment preferences among patients with CKD have been attributed to differences in communication and knowledge of EOL treatments (e.g., hospice) among Black and White patients.9 However, given the higher incidence of limited health literacy among Black patients, there is evidence that health literacy is a mediator of racial disparities across several parts of care.10–13 Limited health literacy impedes an individual’s capacity to understand basic information to make informed medical decisions and approximately 28–32% of patients with CKD are afflicted.14–16 Patients’ understanding of the risks and benefits of CPR has been shown to be associated with subsequent treatment preferences and more recent studies of general medicine patients have focused on the effect of health literacy on racial disparities in preferences for EOL care and advance care planning.11, 17–21 Still, the role of race and health literacy in EOL treatment knowledge in the CKD population has not been fully explored. We therefore sought to investigate whether health literacy would mediate racial disparities in understanding of CPR among Black and White patients with advanced CKD.
Methods
Setting and study participants.
We performed a cross-sectional study of patients with Stage 4 or 5 CKD (as defined by the Modification of Diet in Renal Diseases estimation of glomerular filtration rate 16 to 29 ml/min/1.73m2 and <15 ml/min/1.73m2 respectively)22 between August 2013 and February 2015. We recruited patients from outpatient nephrology clinics affiliated with two academic centers in Boston, Massachusetts. Patients were included if they were 45 years and older, English-speaking, Black or White race, and were referred by their primary nephrologist. We excluded patients if they were on the waiting list for a kidney transplantation. Patients with a documented history of dementia in the medical record or who could not independently give consent to participate in this study were also excluded. All enrolled patients were also screened with the Short Portable Mental Status Questionnaire23 and excluded if they were found to have severe cognitive deficits (as determined by eight or more errors). This study was approved by the Institutional Review Boards at Partner’s Health Care and Boson Medical Center.
Data collection.
All study personnel underwent training in performing study procedures using interviewer-assisted study questionnaires. All interviews were performed in a quiet and private room in the outpatient clinic during a scheduled routine visit. Study personnel ready survey questionnaires out loud to all patients. Patient demographic information including age, ethnicity, income, and education were self-reported. Health literacy was assessed using the Rapid Estimate of Adult Literacy in Medicine (REALM) survey which has been used in previous studies of patients with advanced and end-stage kidney disease.24–26 Limited health literacy was defined as a total score of ≤ 60. Electronic medical records were reviewed for co-morbidities and this information was used to calculate the Charlson Comorbidity Index for each patient.27 Advance care planning, which was defined as having EOL discussions with their health care providers within the last year as well as completion of advance directives, was assessed for all patients. Patients were asked if they had: 1) any EOL discussion with any health care provider (yes/no), 2) any EOL discussion with their nephrologist (yes/no), 3) a health care proxy form (yes/no), or 4) a Do-Not-Resuscitate form/living will (yes/no). We reviewed electronic medical records to validate each patient’s report of advance directives. If there was no evidence of any advance directives or discordance in documentation, the patient’s spoken response was used in analyses.
Outcomes.
The primary outcome was CPR knowledge. The knowledge questionnaire was developed based on a literature review including previously published CPR knowledge surveys and information found on the American Heart Association website.28–31 We aimed to assess the domains of CPR purpose, risk/benefits, and outcomes data. The survey consisted of eight multiple-choice questions that included knowledge about cardiac arrest, cardiopulmonary resuscitation, respiratory failure/intubation and survival post-CPR for hospitalized patients with advanced CKD (see Supplement). Authors (NDE, AEV, and MKP) developed and reviewed the survey items using guidelines for readability and clarity as per recommendations from the Institute of Medicine.16 These questions were piloted among CKD patients using standard cognitive interview techniques and modified to produce the final version.
Statistical analysis.
Patient characteristics were evaluated as proportions for categorical variables or means with standard deviations for continuous variables. We calculated the proportion of patients who had any EOL discussions with their providers as well as possession of health care proxy forms and Do-Not-Resuscitate forms/living wills. We also tabulated the proportion of correct responses for each CPR knowledge question as well as mean summary scores. Chi-square and independent sample t-testing were used to determine differences in demographic, health literacy, advance care planning, and CPR knowledge among Black and White patients.
We used multivariate linear regression to determine unadjusted and adjusted associations of CPR knowledge with race. Statistical significance from univariate analysis determined which demographic variables would be included in multivariable regression models. Three different linear models were estimated: 1) race alone; 2) age, education, and income; and 3) age, education, income, and health literacy. In addition, to assess the impact of advance directives on racial differences in CPR knowledge, we added 1) possession of a Do-Not-Resuscitate form/living will; and, 2) possession of a health care proxy form to the fully adjusted model. We used the R2 statistic to summarize model fit and plots of residuals, residuals versus fitted values, and residual versus quantiles as regression diagnostics to determine the appropriateness of the model. A variance inflation factor of less than 10 was used to indicate the absence of multicollinearity. We used the Baron and Kenny approach to determine whether health literacy mediated the relationship between CPR knowledge and race.32 This approach considered the following questions: 1) Does race significantly predict CPR knowledge? 2) Does race significantly predict health literacy? 3) Does health literacy significantly predict CPR knowledge when controlling for race? All analyses were performed using SAS version 9.4 (SAS Institute, Inc. Cary, NC, USA). Statistical significance was determined by p values < 0.05.
Results
Two hundred and sixty-eight patients were approached to participate in the study. Sixty-one patients declined participation, 54 were ineligible, and one patient stopped the study early. Among the 152 patients who provided informed consent and enrolled in the study, 149 were included in the analysis, as three patients did not complete all variables needed for analyses. The mean age of the entire cohort was 68 (± 11) years; 77% of White patients were aged 65 years or greater compared with 55% of Black patients (p < .01, Table 1). Sixty-one percent of patients were male and 98% had health insurance. Most patients had completed high school; however, 32% of Black patients had not attained a high school diploma compared with 5% of White patients (p < .01). Additionally, more Black patients reported an annual income of less than $30,000 compared with White patients (69% vs. 27%, p < .01). Although the proportion of patients with limited health literacy was 34% among all patients, 63% of Black patients had limited health literacy compared with 14% of White patients (p < .01). There was no racial difference in comorbidity burden.
Table 1.
Patient Characteristics
| Total (N=149) | Black (N=62) | White (N=87) | P-Value | |
|---|---|---|---|---|
| Age, years1 | 68 (11) | 66 (11) | 70 (10) | 0.01 |
| Age ≥ 65 years (%) | 68 | 55 | 77 | <0.01 |
| Hispanic ethnicity (%) | 2 | 3 | 1 | 0.16 |
| Male (%) | 61 | 52 | 66 | 0.08 |
| Less than high school education (%) | 24 | 32 | 5 | < 0.01 |
| Income less than $30,000 (%) | 44 | 69 | 27 | < 0.01 |
| Health insured (%) | 98 | 97 | 99 | 0.36 |
| Limited health literacy2 | 34 | 63 | 14 | < 0.01 |
| Charlson comorbidity index score1,* | 7 (2) | 7 (2) | 7 (2) | 0.96 |
| Charlson comorbidity index score ≥ 3 (%) | 97 | 95 | 98 | 0.40 |
| Advance care planning | ||||
| Have had any EOL3 discussion with provider | 23 | 24 | 23 | 0.86 |
| Have had any EOL discussion with nephrologist | 8 | 13 | 5 | 0.06 |
| Possession of DNR4 form or living will | 32 | 23 | 39 | 0.03 |
| Possession of HCP5 form | 61 | 48 | 70 | 0.01 |
Presented as mean (± SD);
Limited health literacy =REALM score ≤ 60,
EOL =End-of-Life,
DNR=Do-Not-Resuscitate,
HCP=Healthcare proxy form,
Charlson comorbidity index score is derived from age and comorbidities including myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, dementia, chronic pulmonary disease, connective tissue disease, ulcer disease, mild liver disease, diabetes, hemiplegia, moderate or severe renal disease, solid tumor (non-metastatic), leukemia, lymphoma/multiple myeloma, moderate or severe liver disease, metastatic solid tumor, and AIDS.
Twenty-three percent of patients had not had any EOL discussion with any health care provider and only 8% reported having this discussion with their nephrologist (Table 1). There were no differences between Black and White patients in terms of EOL discussions, however racial differences were observed in self reports of advance care planning. Thirty-two percent of patients had a Do-Not-Resuscitate form/living will with Black patients reporting that they completed these forms less often than White patients (23% vs. 39%, p < .01). Black patients also less commonly possessed health care proxy forms compared with White patients (48% vs. 70%, p = .01).
The proportion of correct responses to CPR knowledge items are displayed in Table 2. Overall, less than half of all patients knew: 1) the correct definition of cardiac arrest (46%), 2) the possibility of traumatic sequelae after receiving CPR (43%), 3) the possibility of respiratory failure after successful CPR (48%), 4) about the inability to speak after initial intubation (44%), and, 5) the chance of post-CPR survival for hospitalized patients with advanced chronic kidney disease (6%). Overall, patients had a mean summary knowledge score of 51 ±20, with Black patients scoring significantly lower than White patients (45 ±19 vs. 56 ±20, p = .01).
Table 2.
Percentage of Correct CPR* Knowledge Items
| Total (N=149) | Black (N=62) | White (N=87) | P-Value | |
|---|---|---|---|---|
| CPR Knowledge Items (%) | ||||
| Knowledge of meaning of “cardiac arrest” | 46 | 39 | 52 | 0.12 |
| Knowledge of CPR purpose | 84 | 77 | 89 | 0.07 |
| Knowledge of CPR causing physical trauma | 43 | 34 | 49 | 0.06 |
| Knowledge of respiratory failure occurring after successful CPR | 48 | 31 | 60 | < 0.01 |
| Knowledge of ventilator purpose | 81 | 77 | 83 | 0.42 |
| Knowledge of ability to speak after initial intubation | 44 | 31 | 54 | < 0.01 |
| Knowledge of post-CPR survival in CKD patients | 6 | 8 | 5 | 0.38 |
| Knowledge of change in ability to perform daily activities post-CPR survival | 60 | 60 | 60 | 0.99 |
| Mean summary score (±SD) | 51 (±20) | 45 (±19) | 56 (±20) | 0.01 |
CPR=Cardiopulmonary resuscitation
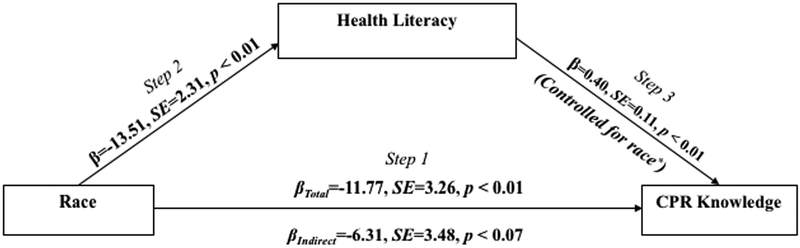
In the unadjusted model predicting the relationship between race and CPR knowledge (Model 1; Table 3) as well as in a multivariate model adjusted for race, age, education and income (Model 2; Table 3), we demonstrated a significant racial difference in CPR knowledge. Patients with limited health literacy also had significantly lower CPR knowledge scores compared with those with adequate health literacy (−8.28 (−16.00, −0.56)). In addition, all three criteria for the Baron Kenny approach to mediation were fulfilled (Figure 1). Specifically, race significantly predicted CPR knowledge (Step 1, p < .01) and health literacy (Step 2, p < .01). Finally, health literacy significantly predicted CPR knowledge while controlling for race (Step 3, p < .01). After the addition of health literacy to Model 2 (Model 3; Table 3), the point estimate for race reduced by 38% (from −8.14 to −5.05) and was no longer significant.
Table 3.
Unadjusted and Adjusted Analyses for Mean CPR* Knowledge Score by Race
| MODEL 1: Unadjusted | MODEL 2: Multivariable, no health literacy | MODEL 3: Multivariable + health literacy | |
|---|---|---|---|
| B (95% CI) | B (95% CI) | B (95% CI) | |
| Intercept | 56.32 (52.17, 60.47) | 57.02 (52.29, 61.75) | 57.86 (53.12, 62.60) |
| Race: Black vs. White | −11.77 (−18.20, −5.33) | −8.14 (−15.44, −0.83) | −5.05 (−12.82, 2.72) |
| Age, years: < 65 vs. ≥ 65 | −7.34 (0.57, 14.13) | 7.51 (0.81, 14.20) | |
| Education < HS** vs. ≥ HS | −9.77 (−18.82, −0.73) | −7.00 (−16.31, 2.31) | |
| Income: < 30K vs. ≥ 30K | −6.47 (−13.15, 0.20) | −6.02 (−12.63, 0.58) | |
| Health literacy: Limited vs. Adequate | −8.28 (−16.00, −0.56) | ||
| Model R2 | 0.08 | 0.16 | 0.19 |
CPR=Cardiopulmonary resuscitation;
HS = High school
Figure 1.
Racial Differences in CPR Knowledge Mediated by Helth Literacy1,2
1CPR=Cardiopulmonary resuscitation; 2White patients serve as the reference group for this analysis; βTotal = Point estimate for race in Step 1; βIndirect = Point estimate for race in Step 3
After the addition of Do-Not-Resuscitate form/living wills (Model 4, Table 4) and after the addition of health care proxy forms (Model 5, Table 4) to the fully adjusted model (Model 3, Table 3), patients with limited health literacy continued to have significantly lower CPR knowledge than those with adequate health literacy.
Table 4.
Adjusted Analyses Including Advance Directives for Mean CPR1 Knowledge Score by Race
| MODEL 4: Multivariable + DNR form/living will | MODEL 5: Multivariable + HCP form | |
|---|---|---|
| B (95% CI) | B (95% CI) | |
| Intercept | 61.46 (55.54, 67.37) | 58.93 (54.08, 63.78) |
| Race: Black vs. White | −4.56 (−12.28, 3.15) | −4.69 (−12.42, 3.03) |
| Age, years: < 65 vs. ≥ 65 | 9.55 (2.61, 16.49) | 8.94 (2.11, 15.77) |
| Education < HS vs. > HS | −6.65 (−15.88, 2.56) | −7.23 (−16.47, 2.01) |
| Income: < 30K vs. ≥ 30K | −5.90 (−12.45, 0.64) | −4.93 (−11.60, 1.74) |
| Possession of DNR2 form or living will: No vs. Yes | −6.78 (−13.57, 0.02) | _ |
| Possession of HCP3 form: No vs. Yes | _ | −5.98 (−12.59, 0.63) |
| Health literacy: Limited vs. Adequate | −8.21 (−15.85, −0.56) | −7.76 (−15.44, −0.07) |
| Model R2 | 0.21 | 0.21 |
CPR=Cardiopulmonary resuscitation,
DNR=Do-Not-Resuscitate,
HCP=Healthcare proxy form
Discussion
In this study of Black and White patients with advanced CKD, we found a higher proportion of Black patients had limited health literacy, less advance directives and lower knowledge of CPR compared with White patients. However, health literacy significantly mediated racial differences in CPR knowledge. Additionally, after accounting for possession of advance directives, health literacy continued to remain a significant predictor of CPR knowledge.
Discussing the risks and benefits of life-sustaining treatments such as CPR, mechanical ventilation, and feeding tubes is fundamental to promoting effective informed decision-making in the event of critical illnesses. Advance care planning, which encompasses communication and documentation of goals of care at the end of life between health care providers, patients, and their families, occurs infrequently among patients with CKD and ESRD.33, 34 Importantly, studies have shown that knowledge of what CPR entails and perceptions of one’s survival affects preferences and subsequent decision-making about this treatment.20, 21, 30, 31 One study of older inpatients with end-stage cancer showed that only 11% of patients could describe more than two components of CPR and that less than 3% correctly knew that the success rate of CPR was less than 10%.31 We found similar results and although patients knew the overall purposes of CPR and mechanical ventilation, most were not aware of the bodily trauma, inability to speak initially after intubation or chances of survival after receiving CPR. Additionally, patients who have limited health literacy may have poor insight into these aspects of care and our findings showed health literacy remained a significant predictor of CPR knowledge after controlling for several demographic variables. These findings remained consistent even after controlling for possession of advance directives. This is consistent with previous work that show the completion of EOL documentation is not always associated with improved knowledge of life-sustaining therapies.30 Patients with CKD have high rates of limited health literacy and experience frequent complications and poor survival during hospitalizations when they receive CPR.2, 35 Therefore, it is imperative that providers delineate the risks of this therapy and confirm understanding with patients and their loved ones during advance care planning discussions. To our knowledge, there have not been any studies that have investigated the impact of health literacy-sensitive interventions to improve EOL treatment knowledge within nephrology. However, advance directives and video decision-aids that have been developed to address the needs of patients with limited health literacy have been particularly useful in improving advance care planning and EOL decision-making outcomes in other medical disciplines.36–39
Although we demonstrated differences in CPR knowledge and possession of advance directives between Black and White patients, we did not find racial differences with regard to frequency of EOL discussions with health care providers and this was consistent with other studies.9, 33 Patients may feel more inclined to have discussions with their providers whom they feel comfortable with however, relationships with health care providers may have less of an impact on subsequent treatment decision-making among minority racial patients. For instance, Smith et al. showed that although the quality of the physician-patient relationship (e.g., perceived respect, listening, help in navigating the medical system) was lower among Black patients compared with White patients, this did not influence advance care planning or preferences for life-sustaining treatments.40 Factors such as relationships with families and communities, negative beliefs regarding advance care planning, and limited health literacy have been proven to impact EOL care preferences especially among Black patients.41 Health care teams should therefore tailor advance care planning conversations to account for these cultural, educational and social support differences to effectively engage minority populations in the advance care planning process.42 For example, Song et al. randomized an advance care planning intervention among Black and White hemodialysis patients and their surrogates.43 Specifically, the intervention aimed to discern the emotional and spiritual beliefs that patients and family members had in relation to the illness. This intervention led to significantly improved congruence on goals of care (between patients and surrogates) as well as surrogate decision-making confidence for Black patients compared with White patients who also received the intervention. Furthermore, surrogates of Black patients had less bereavement depressive symptoms compared with surrogates of White patients. Similarly, Perry et al. used a peer-mentoring program to improve end-of-life planning among hemodialysis patients.44 The peer mentors were specifically trained in addressing facts, myths, and barriers to completing advance directives. Among Black patients, the program had a larger impact on completion and comfort with discussion of advance directives compared with White patients. Although racial differences in health literacy were not accounted for in the aforementioned studies, interventional approaches that specifically focus on understanding of health statuses and EOL care options appear to be effective in decreasing racial disparities in advance care planning. These results, along with the findings of the current study, indicate that addressing health literacy barriers (e.g., expectations, understanding) as well as belief systems during advanced care planning is a promising approach to decreasing racial disparities in care received at the end of life.
Our study has a few limitations. The limited racial diversity and language capability among the study cohort may limit generalizability to other study populations. We did not specifically explore reasons for lower health literacy in Black versus White patients living in the Boston area and acknowledge these findings may differ among patients from the same racial groups who live in other US regions. Additionally, we aimed to confirm advance directives with chart review, however only 37% (n=55) had documentation of a health care proxy form and 9% (n=13) had documentation of a Do-Not-Resuscitate form/living will. However, of these, 87% (n = 48) and 92% (n = 12) were respectively concordant with what patients reported to us regarding health care proxy forms and Do-Not-Resuscitate form/living wills in their surveys. We also did not include patient EOL preferences in this study, which prevents us from assessing the impact of CPR knowledge on preferences. Although patients were provided the option of stopping the study early or skipping any questions if they felt discomfort or anxiety, we did not specifically screen patients for anxiety related to decision-making which could have affected survey responses. Additionally, although survey items to assess possession of DNR/living will and health care proxies had readability that was appropriate for patients with limited health literacy, we did not specifically assess patient understanding of these legal terms. Lastly, we recognize that although CPR knowledge questions were derived from similar surveys and publicly available information regarding CPR facts and outcomes in the CKD population, the questionnaire had not been validated and newer data regarding survival post-CPR for CKD patients has since been published.2 Despite these limitations, we believe our data reliably demonstrate key differences in understanding of CPR between Black and White CKD patients and the mediating effect of health literacy in this relationship.
In conclusion, our study is the first to identify the association of health literacy with CPR knowledge and its mediatory effect on racial differences in knowledge among Black and White patients with advanced CKD. These findings indicate that health literacy is one of the factors that should be considered when engaging patients in advance care planning to optimize informed-decision making and decrease racial disparities in EOL care among patients with CKD. Future studies may be helpful in defining the relationships between health literacy, belief systems, and decision-making among diverse patient populations to improve patient centered-care.
Supplementary Material
Acknowledgments:
Dr. Eneanya is supported by NIH grant K23DK114526.
Footnotes
Disclosure Statement: All authors have approved this manuscript for submission. No competing financial interests exist.
References
- 1.Saeed F, Adil MM, Malik AA, et al. : Outcomes of In-Hospital Cardiopulmonary Resuscitation in Maintenance Dialysis Patients. Journal of the American Society of Nephrology : JASN. 2015;26(12):3093–3101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saeed F, Adil MM, Kaleem UM, et al. : Outcomes of In-Hospital Cardiopulmonary Resuscitation in Patients with CKD. Clinical journal of the American Society of Nephrology : CJASN. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davis TR, Young BA, Eisenberg MS, et al. : Outcome of cardiac arrests attended by emergency medical services staff at community outpatient dialysis centers. Kidney international. 2008;73(8):933–939. [DOI] [PubMed] [Google Scholar]
- 4.Wong SP, Kreuter W, Curtis JR, et al. : Trends in in-hospital cardiopulmonary resuscitation and survival in adults receiving maintenance dialysis. JAMA internal medicine. 2015;175(6):1028–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bedell SE, Delbanco TL, Cook EF, et al. : Survival after cardiopulmonary resuscitation in the hospital. The New England journal of medicine. 1983;309(10):569–576. [DOI] [PubMed] [Google Scholar]
- 6.Eneanya ND, Hailpern SM, O’Hare AM, et al. : Trends in Receipt of Intensive Procedures at the End of Life Among Patients Treated With Maintenance Dialysis. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2017;69(1):60–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wong SP, Kreuter W, O’Hare AM: Treatment intensity at the end of life in older adults receiving long-term dialysis. Archives of internal medicine. 2012;172(8):661–663; discussion 663–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thomas BA, Rodriguez RA, Boyko EJ, et al. : Geographic variation in black-white differences in end-of-life care for patients with ESRD. Clinical journal of the American Society of Nephrology : CJASN. 2013;8(7):1171–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eneanya ND, Wenger JB, Waite K, et al. : Racial Disparities in End-of-Life Communication and Preferences among Chronic Kidney Disease Patients. American journal of nephrology. 2016;44(1):46–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eneanya ND, Winter M, Cabral H, et al. : Health Literacy and Education as Mediators of Racial Disparities in Patient Activation Within an Elderly Patient Cohort. Journal of health care for the poor and underserved. 2016;27(3):1427–1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Volandes AE, Paasche-Orlow M, Gillick MR, et al. : Health literacy not race predicts end-of-life care preferences. Journal of palliative medicine. 2008;11(5):754–762. [DOI] [PubMed] [Google Scholar]
- 12.Gupta VK, Winter M, Cabral H, et al. : Disparities in Age-Associated Cognitive Decline Between African-American and Caucasian Populations: The Roles of Health Literacy and Education. Journal of the American Geriatrics Society. 2016;64(8):1716–1723. [DOI] [PubMed] [Google Scholar]
- 13.Osborn CY, Paasche-Orlow MK, Davis TC, et al. : Health literacy: an overlooked factor in understanding HIV health disparities. American journal of preventive medicine. 2007;33(5):374–378. [DOI] [PubMed] [Google Scholar]
- 14.Ricardo AC, Yang W, Lora CM, et al. : Limited health literacy is associated with low glomerular filtration in the Chronic Renal Insufficiency Cohort (CRIC) study. Clinical nephrology. 2014;81(1):30–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Devraj R, Borrego M, Vilay AM, et al. : Relationship between Health Literacy and Kidney Function. Nephrology (Carlton, Vic.). 2015;20(5):360–367. [DOI] [PubMed] [Google Scholar]
- 16.Nielsen-Bohlman LPA, Kindig DA, eds.: Health literacy: a prescription to end confusion. Washington: National Academies Press; 2004. [PubMed] [Google Scholar]
- 17.Waite KR, Federman AD, McCarthy DM, et al. : Literacy and race as risk factors for low rates of advance directives in older adults. Journal of the American Geriatrics Society. 2013;61(3):403–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kerridge IH, Pearson SA, Rolfe IE, et al. : Impact of written information on knowledge and preferences for cardiopulmonary resuscitation. The Medical journal of Australia. 1999;171(5):239–242. [DOI] [PubMed] [Google Scholar]
- 19.Sharma R, Jayathissa S, Weatherall M: Cardiopulmonary resuscitation knowledge and opinions on end of life decision making of older adults admitted to an acute medical service. The New Zealand medical journal. 2016;129(1428):26–36. [PubMed] [Google Scholar]
- 20.Miller DL, Jahnigen DW, Gorbien MJ, et al. : Cardiopulmonary resuscitation: how useful? Attitudes and knowledge of an elderly population. Archives of internal medicine. 1992;152(3):578–582. [DOI] [PubMed] [Google Scholar]
- 21.Zijlstra TJ, Leenman-Dekker SJ, Oldenhuis HK, et al. : Knowledge and preferences regarding cardiopulmonary resuscitation: A survey among older patients. Patient education and counseling. 2016;99(1):160–163. [DOI] [PubMed] [Google Scholar]
- 22.Levey AS, Bosch JP, Lewis JB, et al. : A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Annals of internal medicine. 1999;130(6):461–470. [DOI] [PubMed] [Google Scholar]
- 23.Pfeiffer E: A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. Journal of the American Geriatrics Society. 1975;23(10):433–441. [DOI] [PubMed] [Google Scholar]
- 24.Wright JA, Wallston KA, Elasy TA, et al. : Development and results of a kidney disease knowledge survey given to patients with CKD. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2011;57(3):387–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jain D, Sheth H, Green JA, et al. : Health literacy in patients on maintenance peritoneal dialysis: prevalence and outcomes. Peritoneal dialysis international : journal of the International Society for Peritoneal Dialysis. 2015;35(1):96–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cavanaugh KL, Wingard RL, Hakim RM, et al. : Low health literacy associates with increased mortality in ESRD. Journal of the American Society of Nephrology : JASN. 2010;21(11):1979–1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Charlson ME, Pompei P, Ales KL, et al. : A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of chronic diseases. 1987;40(5):373–383. [DOI] [PubMed] [Google Scholar]
- 28.Moss AH, Holley JL, Upton MB: Outcomes of cardiopulmonary resuscitation in dialysis patients. Journal of the American Society of Nephrology : JASN. 1992;3(6):1238–1243. [DOI] [PubMed] [Google Scholar]
- 29.CPR & First Aid. http://cpr.heart.org/AHAECC/CPRAndECC/AboutCPRFirstAid/CPRFactsAndStats/UCM_475748_CPR-Facts-and-Stats.jsp. Accessed April 2013.
- 30.Thorevska N, Tilluckdharry L, Tickoo S, et al. : Patients’ understanding of advance directives and cardiopulmonary resuscitation. Journal of critical care. 2005;20(1):26–34. [DOI] [PubMed] [Google Scholar]
- 31.Heyland DK, Frank C, Groll D, et al. : Understanding cardiopulmonary resuscitation decision making: perspectives of seriously ill hospitalized patients and family members. Chest. 2006;130(2):419–428. [DOI] [PubMed] [Google Scholar]
- 32.Baron RM, Kenny DA: The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of personality and social psychology. 1986;51(6):1173–1182. [DOI] [PubMed] [Google Scholar]
- 33.Kurella Tamura M, Goldstein MK, Perez-Stable EJ: Preferences for dialysis withdrawal and engagement in advance care planning within a diverse sample of dialysis patients. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association. 2010;25(1):237–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Davison SN: End-of-life care preferences and needs: perceptions of patients with chronic kidney disease. Clinical journal of the American Society of Nephrology : CJASN. 2010;5(2):195–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hashim MJ: Patient-Centered Communication: Basic Skills. American family physician. 2017;95(1):29–34. [PubMed] [Google Scholar]
- 36.Volandes AE, Ferguson LA, Davis AD, et al. : Assessing end-of-life preferences for advanced dementia in rural patients using an educational video: a randomized controlled trial. Journal of palliative medicine. 2011;14(2):169–177. [DOI] [PubMed] [Google Scholar]
- 37.Volandes AE, Barry MJ, Chang Y, et al. : Improving decision making at the end of life with video images. Medical decision making : an international journal of the Society for Medical Decision Making. 2010;30(1):29–34. [DOI] [PubMed] [Google Scholar]
- 38.Volandes AE, Paasche-Orlow MK, Barry MJ, et al. : Video decision support tool for advance care planning in dementia: randomised controlled trial. BMJ (Clinical research ed.). 2009;338:b2159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sudore RL, Landefeld CS, Barnes DE, et al. : An advance directive redesigned to meet the literacy level of most adults: a randomized trial. Patient education and counseling. 2007;69(1–3):165–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Smith AK, Davis RB, Krakauer EL: Differences in the quality of the patient-physician relationship among terminally ill African-American and white patients: impact on advance care planning and treatment preferences. Journal of general internal medicine. 2007;22(11):1579–1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sanders JJ, Robinson MT, Block SD: Factors Impacting Advance Care Planning among African Americans: Results of a Systematic Integrated Review. Journal of palliative medicine. 2016;19(2):202–227. [DOI] [PubMed] [Google Scholar]
- 42.Huang CH, Crowther M, Allen RS, et al. : A Pilot Feasibility Intervention to Increase Advance Care Planning among African Americans in the Deep South. Journal of palliative medicine. 2016;19(2):164–173. [DOI] [PubMed] [Google Scholar]
- 43.Song MK, Ward SE, Lin FC, et al. : Racial Differences in Outcomes of an Advance Care Planning Intervention for Dialysis Patients and Their Surrogates. Journal of palliative medicine. 2016;19(2):134–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Perry E, Swartz J, Brown S, et al. : Peer mentoring: a culturally sensitive approach to end-of-life planning for long-term dialysis patients. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2005;46(1):111–119. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.