Abstract
Objectives:
To characterize the current burden, outcomes, and costs of managing sepsis patients in U.S. hospitals.
Design:
A retrospective observational study was conducted using the Premier Healthcare Database, which represents ~20% of U.S. inpatient discharges among private and academic hospitals. Hospital costs were obtained from billing records per the cost accounting method used by each hospital. Descriptive statistics were performed on patient demographics, characteristics, and clinical and economic outcomes for the index hospitalization and 30-day readmissions.
Setting:
Sepsis patient hospitalizations, including inpatient, general ward, and ICU (intermediate and/or step-down).
Patients:
Adults over 18 years old with a hospital discharge diagnosis code of sepsis from January 1, 2010, to September 30, 2016.
Interventions:
None. This was a retrospective observational study of deidentified data.
Measurements and Main Results:
The final study cohort consisted of 2,566,689 sepsis cases, representing patients with a mean age of 65 years (50.8% female). Overall mortality was 12.5% but varied greatly by severity (5.6%, 14.9%, and 34.2%) for sepsis without organ dysfunction, severe sepsis, and septic shock, respectively. Costs followed a similar pattern increasing by severity level: $16,324, $24,638, and $38,298 and varied widely by sepsis present at admission ($18,023) and not present at admission ($51,022).
Conclusions:
The highest burden of incidence and total costs occurred in the lowest severity sepsis cohort population. Sepsis cases not diagnosed until after admission, and those with increasing severity had a higher economic burden and mortality on a case-by-case basis. Methods to improve early identification of sepsis may provide opportunities for reducing the severity and economic burden of sepsis in the United States.
Keywords: cost, epidemiology, incidence, sepsis, shock, mortality
Sepsis management continues to be a major challenge for healthcare systems worldwide. In the United States, over 970,000 sepsis cases are admitted annually, and the numbers have been rising year over year (1). A 2-decade study of U.S. hospitalizations identified an increase in the incidence of sepsis among hospitalized patients by 8.7% per year (2). Additionally, sepsis accounts for more than 50% of hospital deaths (3), and mortality increases dramatically with greater disease severity: 10–20% for sepsis, 20–40% for severe sepsis, and 40–80% for septic shock (4).
Septic patients represent a disproportionately high burden in terms of hospital utilization. The average length of stay (LOS) for sepsis patients in U.S. hospitals is approximately 75% greater than for most other conditions (5), and the mean LOS in 2013 was reported to dramatically increase with sepsis severity: 4.5 days for sepsis, 6.5 days for severe sepsis, and 16.5 days for septic shock (6).
The cost of sepsis management in U.S. hospitals ranks highest among admissions for all disease states. For example, in 2013, sepsis accounted for more than $24 billion in hospital expenses, representing 13% of total U.S. hospital costs, but accounted for only 3.6% of hospital stays. The $24 billion (~$18,244 per hospitalization) attributed to sepsis far surpassed the next most costly conditions: second most costly being osteoarthritis at $17 billion (~$16,148 per hospitalization) and third most costly being childbirth at $13 billion (~$3,529 per hospitalization) (7). Hospital costs for sepsis are currently more than twice those of other conditions and continue to grow at three times the rate of other admissions (8). As with mortality and LOS, mean daily hospital costs were shown in 2013 to increase markedly with increasing sepsis severity: $1,830 for sepsis (Diagnosis-Related Group [DRG]–870), $2,193 for severe sepsis (DRG-871), and $3,087 for septic shock (DRG-872) (6).
The timing of sepsis diagnosis is critical in terms of outcomes given the acute and significant impact of the condition. Poor sepsis outcomes are observed when diagnosis and treatment are delayed (9–15) and when sepsis develops or is not detected until after hospital admission (16). Although the clinical outcomes have been well studied and there is a broad array of literature on the economics of sepsis hospitalization, there is limited evidence that is up to date, nationally generalizable, and provides granular insight into the heterogeneity of sepsis hospitalization economics. Therefore, the current study was designed to rigorously characterize the clinical features of sepsis that most strongly influence healthcare utilization. Based upon the aforementioned variables known to influence patient outcomes, we focused on the timing of sepsis diagnosis and sepsis severity as it relates to hospital service utilization and related costs.
MATERIALS AND METHODS
Design and Data Source
A retrospective observational database study was conducted on patients with a hospital discharge date of January 1, 2010, to September 30, 2016. Data were derived from the statistically deidentified Premier Healthcare Database which contains data from more than 659 million patient encounters, approximately 20% of U.S. admissions among private and academic hospitals. This database contains standard hospital discharge files, including a patient’s demographics, disease state, medications, laboratory, diagnostics, and therapeutic services in deidentified patient daily service records. It is a complete census of inpatients and hospital-based outpatients from geographically diverse hospitals. Costs were obtained from billing records per the cost accounting method used by each hospital. For this study, all financial and utilization data came from the hospital chargemaster. For approximately 15% of hospitals, costs were derived from the cost to charge ratio from the respective hospital department to estimate total cost. For all other hospitals, costs were reported on their chargemaster.
The Premier database is an aggregated, deidentified dataset in which no one patient can be individually identified and therefore no patient consent is required and the study is Institutional Review Board exempt.
Population
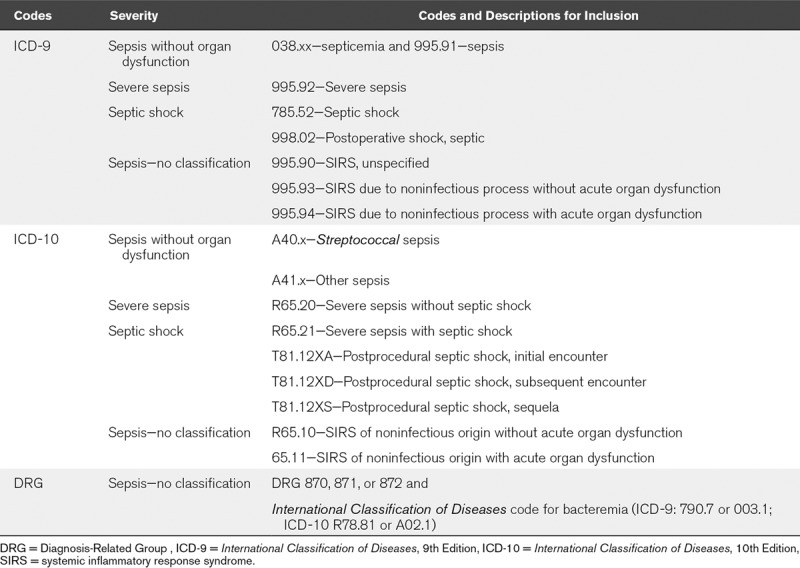
Patients included were greater than or equal to 18 years old upon admission and had an International Classification of Diseases, 9th Edition (ICD-9) or International Classification of Diseases, 10th Edition (ICD-10) diagnosis code for sepsis at discharge or if they were reimbursed under a sepsis DRG code with an associated diagnosis for bacteremia (Table 1). Patients were excluded if their discharge date was after September 30, 2016 or if they had a sepsis admission in the 90 days prior to the first sepsis event thus ensuring each sepsis event in the dataset was truly a patient’s first event and not a readmission. If an event was found that was within the 90 days prior, that event then became the first event, and the subsequent would be categorized as a readmission. The unit of analysis was a sepsis-related inpatient hospitalization, and patients were eligible to contribute multiple unique sepsis events over the study period.
TABLE 1.
Sepsis-Related Event Inclusion Codes and Classification
Analysis
The primary analysis addressed all sepsis-related cases. We also examined the data by whether the sepsis diagnosis was present at admission (POA). Identification of POA diagnoses are part of a requirement of the Centers for Medicaid and Medicare Services (CMS) Deficit Reduction Act for diseases which are high in cost or volume, assigned to higher paying DRGs and reasonably preventable through evidence-based medicine. Unfortunately, CMS does not require POA diagnoses at admission to be later verified; therefore, those in the non-POA group could have disease that was acquired later in the admission or was missed on initial assessment.
Patients were evaluated from the time of their admission until discharge. Clinical features of interest included demographics, outcomes, and costs. Outcomes were further stratified by the index admission and any readmissions within 30 days of discharge. During the index admission, outcomes evaluated included LOS, ICU time, time on a mechanical ventilator, inpatient mortality, discharge status (to home, skilled nursing facility, etc), and cost of visit. Additionally, 30-day follow-up outcomes included all-cause readmissions and readmission cost.
The secondary analysis focused on better characterizing the economic burden of sepsis by severity level. A hierarchy of ICD-9 and ICD-10 codes was created to stratify patients into severity categories. Those with septic shock codes were classified septic shock, those with severe sepsis codes but no septic shock codes were classified as severe sepsis, those with sepsis codes but no severe sepsis or septic shock codes were classified as sepsis without organ dysfunction, and everyone else was classified as other (Table 1).
Data were measured on a continuous scale and analyzed as mean, sd, and median. Categorical data are reported as counts and percentages. Index hospitalization cost, defined as the cost incurred by the hospital to treat the patient, is reported in total. All analyses were conducted with SAS (version 9.4, SAS Institute Inc. Cary, NC).
RESULTS
The study identified a total of 2,566,689 sepsis-related cases over the study period, of which 2,466,605 required an inpatient admission with the remaining cases (3.9%) being managed in an outpatient setting. Among the inpatient admissions, sepsis POA was 86.8% (2,142,104) of eligible inpatient events (Fig. 1). Overall, patients were primarily (88.3%) from urban hospitals, and roughly half (50.5%) were treated at hospitals with trauma services.
Figure 1.
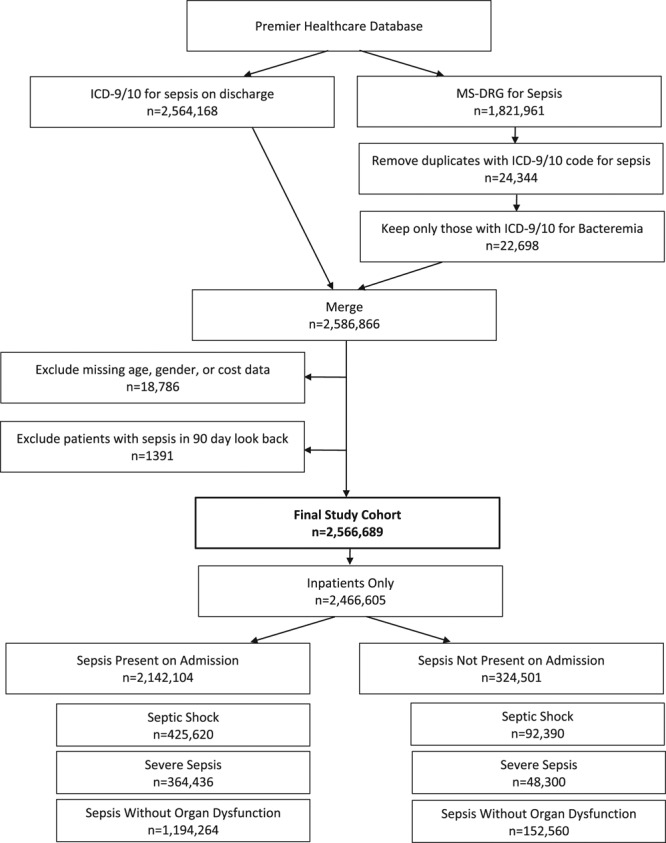
Attrition diagram for inpatient sepsis hospitalizations included for analysis. ICD-9/10 = International Classification of Diseases, 9/10th Edition, MS-DRG = Medicare Severity Diagnosis Related Groups.
Total sepsis cases represented patients with a mean age of 65 years (sd, ±18.1), and 50.8% were female. They were a very sick population with a Charlson Comorbidity Index of 2.5 (Table 2). Comorbidities were frequent, and sepsis non-POA cases represented a slightly more severe population with higher rates of history of cardiovascular disease, chronic kidney disease, and active cancer. The majority (70.1%) of the sepsis cases were not able to document a specific causal organism. Among the organisms identified, the primary included Escherichia coli, other Gram-negative bacteria, and Staphylococcus. Among sepsis POA cases, E. coli (7.4%) was two times more common than those diagnosed after admission (3.2%) (Fig. 2).
TABLE 2.
Sepsis-Related Inpatient Hospitalization Event Demographics and Characteristics
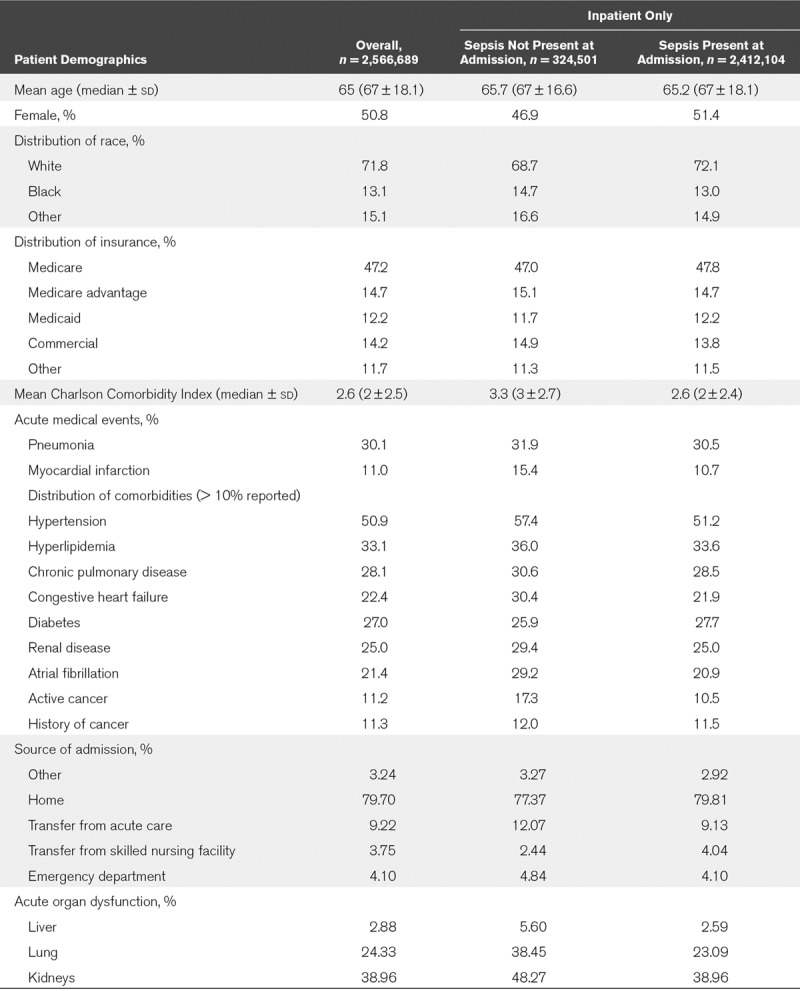
Figure 2.
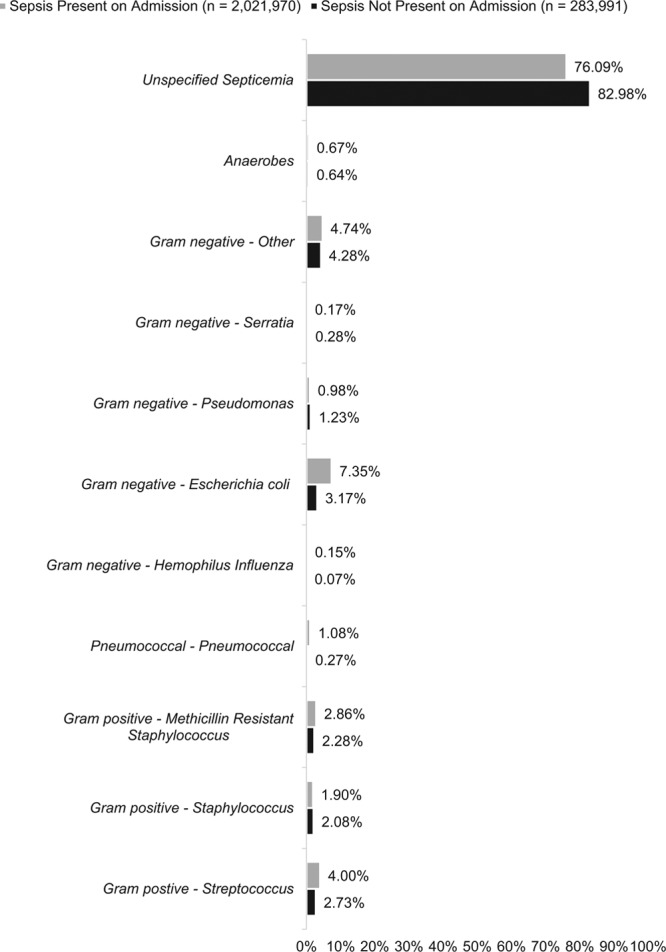
Distribution of bacteria detected among inpatient sepsis hospitalizations.
The hospital mortality rate was 12.5% and was more than two-fold higher (11.4% vs 25.6%) in non-POA cases. A substantial proportion surviving the hospitalization were discharged to home (52.3%) or other forms of supportive care including skilled nursing facilities, rehabilitation, and long-term care (28.0%). Non-POA patients had lower rates of discharge to home (34.9%) than POA patients (55.7%). Among only the survivors, non-POA cases had lower rates of discharge to home (47%) than POA patients (62.7%), some of which was influenced by discharge to other long-term care settings (non-POA: 46.1% and POA: 31.7%) and the remainder due to the higher mortality rates observed.
On average, non-POA sepsis cases spent nearly double the amount time in the hospital, in the ICU, and on mechanical ventilation compared with sepsis POA cases, that is, from 7.7 to 17.6 days, from 5.2 to 10.1 days, and from 6.6 to 10.1 days, respectively. Cause of sepsis was generally not specified, with 96.7% of the events classified as “other,” postoperative infection at 2.1%, burn at 0.1%, and trauma at 0.9%. As expected, there were more postoperative infections in cases with sepsis not POA (5.4%). Mean patient costs were considerable at $21,568, and when stratified, POA was $18,023 and a staggering $51,022 for non-POA. Although outliers may have skewed the results, the median costs demonstrated a three-fold increase in costs for non-POA cases ($10,371 vs $32,085, respectively).
To further explore the differences in sepsis outcomes and costs, an analysis by sepsis severity among cases with sepsis overall and by POA was conducted as a secondary objective. The study found a distribution of severity levels with the majority classified as sepsis without organ dysfunction (51.2%) followed by 19.1% for severe sepsis and 29.7% for septic shock. Details on the sepsis-related outcomes by sepsis severity and sepsis at the point of admission are summarized in Table 3.
TABLE 3.
Index and 30-Day Readmission Sepsis Hospitalization Morbidity, Mortality, and Costs
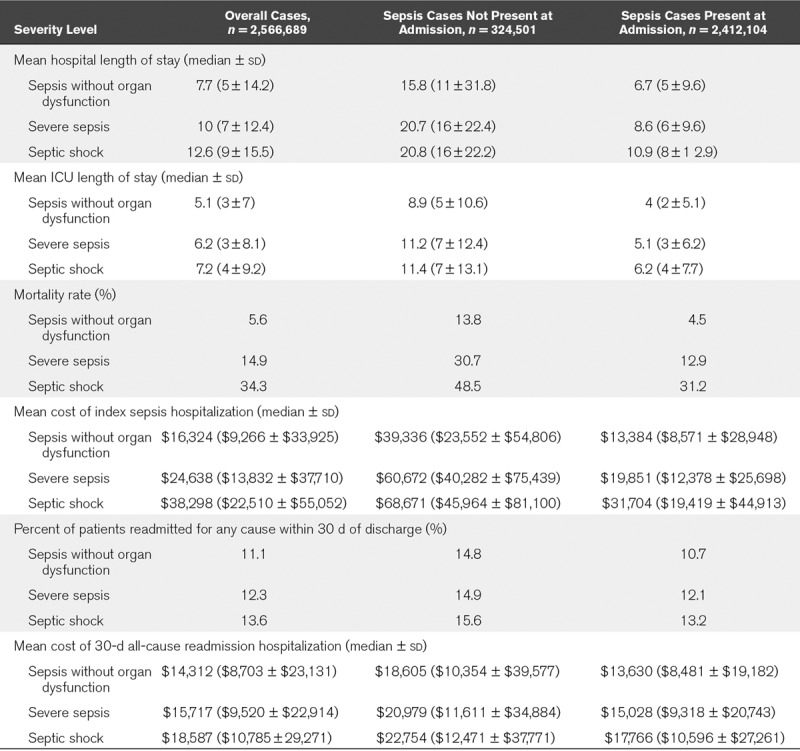
Overall, the mortality rates as well as the healthcare resource use and costs increased as severity increased. The mortality rate overall by sepsis severity was 5.6%, 14.9%, and 34.3% for sepsis without organ dysfunction, severe sepsis, and septic shock, respectively. Despite the high mortality rates, LOS increased from 7.7 to 12.6 days, and the costs of sepsis increased from $16,324 to $38,298 from sepsis without organ dysfunction to septic shock. A clear trend toward increased resource use and costs and poor clinical outcomes was associated with increasing severity (Table 3). The largest driver of better clinical outcomes was less severity as demonstrated by a larger range in mortality rates by severity level as compared to stratifying by POA status. Mortality ranged from 5.6% to 14.9% to 34.3% for the overall cohort for sepsis without organ dysfunction, severe sepsis, and septic shock, respectively. This trend followed when severity levels were also stratified by POA status (13.8%, 30.7%, 48.5% for non-POA vs 4.5%, 12.9%, 31.2% for POA diagnosis) (Table 3). Costs, however, were more influenced by stratification by POA diagnosis. Those with sepsis not POA had higher mean costs overall ($51,022 as compared to POA at $18,023). This trend also followed when POA status was stratified by severity ($39,336 to $60,672 to $60,671 for non-POA patients and $13,384 to $19,851 to $31,704 for non-POA patients by severity level: sepsis without organ dysfunction, severe sepsis, and septic shock, respectively). Readmission rates ranged from ~10% to 16% regardless of severity or sepsis POA.
Despite increased costs and worse outcomes with increasing sepsis severity on a case-by-case basis, the aggregate costs for sepsis without organ dysfunction were the greatest. This is due to the higher prevalence of sepsis without organ failures (n = 1,346,824) compared with severe sepsis (n = 412,736) or septic shock (n = 518,010) over the ~7-year evaluation period. The higher prevalence of sepsis without organ failures accounted for higher aggregate costs (and LOS) ~$22 billion (LOS~10.4 million d), compared with ~$10.2 billion (LOS~4.1 million d) and $19.8 billion (LOS~6.5 million d) for severe sepsis and septic shock, respectively.
DISCUSSION
This analysis of over 2.5 million U.S. sepsis cases demonstrates substantial burden while elucidating the vast heterogeneity of sepsis epidemiology, outcomes, and costs by severity level, including cases where sepsis was not diagnosed until after admission (non-POA). The overall inpatient mortality rate was 12.5% representing a slightly lower estimate as compared to the 2013 Nationwide Inpatient Sample of 14.7–16.3% (6), but when examining the data closer, a wide range of mortality rates exists: 11.4% for POA and 25.6% for non-POA, whereas mortality rates by severity ranged from 5.6% for sepsis without organ dysfunction, 14.9% for severe sepsis, and 34.2% for septic shock. Costs followed this same pattern: $18,023 for POA compared with $51,022 for non-POA, a 322% increase, wherein the cost per case of severe sepsis and septic shock were 50% and 235% higher, respectively, compared with sepsis without organ failures (Table 3).
The greatest costs were observed in non-POA sepsis ranging from $39,336 in sepsis without organ dysfunction, $60,672 in severe sepsis, and $68,671 for septic shock per case. These higher costs could in part be attributable to delayed sepsis diagnosis and treatment (e.g., sepsis cases diagnosed within 48 hr of admission but not at baseline) and sepsis complicating other acute medical conditions (e.g., sepsis onset that is delayed beyond 48 hr of admission). It is well known that delayed sepsis diagnosis and/or treatment adversely affect sepsis outcomes (9–15) emphasizing the need for early diagnosis even after admission. In this regard, sepsis diagnosis and/or treatment is frequently delayed during inpatient admissions. A more detailed analysis on a case-by-case basis is needed to determine what proportion of non-POA patients would be characterized as delayed sepsis diagnosis compared with new-onset after hospital admission. Non-POA combines those cases of sepsis that were missed during initial screening (most of these cases would presumably be caught within the first 24 hr of admission) with cases of new onset (e.g., complication of surgery or relating to central catheters, aspiration, etc). This dataset is unable to discriminate one from the other. Nonetheless, any delay in the diagnosis of sepsis typically carries a worse prognosis, and for this reason, the non-POA cohort would be of particular interest for further study.
Regardless of the factors influencing non-POA diagnosis and treatment, the costs of care within this cohort were 2–3× higher than the POA cohort. A related study using data from the multicenter Sepsis Early Recognition and Response Initiative (SERRI) (16) found a similar proportion of sepsis cases identified at admission of almost 85% (compared with our estimate of almost 87%). The SERRI mortality rates reported were slightly higher with an overall mortality rate of 17.2% (ours at 12.5%) and 14.1% (ours at 11.1%) and 38.6% (ours at 25.6%) for those with sepsis POA and non-POA, respectively. Costs reported were of similar magnitude and directionally aligned with the findings of our study. Thus, the Premier healthcare cohort data presented here are consistent with previous reports which serves to validate its results.
Another interesting finding was the higher aggregate cost and LOS for those presenting with milder forms of sepsis. The aggregate costs and LOS for sepsis without organ failure was higher than for either severe sepsis or septic shock, which is in keeping with prior studies showing that the aggregate mortality of the sepsis without organ failure is higher than for either severe sepsis or septic shock (3). Most published studies to date have focused on severe sepsis and septic shock (e.g., the new Sepsis-3 definition [17]) when in fact milder sepsis manifestations account for most sepsis cases and represents the largest disease burden (3). It follows that future research aimed at reducing overall sepsis clinical and financial burden should aim to include this cohort.
The ability to detect and treat sepsis early, before progression to organ failure, leads to less mortality and ultimately less costs (9). Specifically, a body of evidence demonstrates that early sepsis identification and treatment lead to decreased sepsis severity (10–12), mortality (3, 9, 11, 13, 14), and costs (9, 18, 19). Given that a vast majority of sepsis cases initially fall within the “mild” category (i.e., not manifesting with overt organ failures or circulatory shock), and because inherent delays in the detection and treatment of sepsis are common, there is an urgent need for new technologies that aid physicians in earlier detection of sepsis in order to begin treatment as soon as possible.
The present study showed lower readmission rates at 30 days compared with other published studies. Prescott et al (20) 2014 found that survivors of hospitalization for severe sepsis had 30-, 60-, and 365-day hospital readmission rates of 26.5%, 41%, and 63.0%, respectively, compared with the current findings for severe sepsis at 30 days of 12.3%. These lower rates could reflect more current data (Prescott et al [20] represent data from 1992 to 2006) in which hospitals have been implementing early sepsis identification programs and follow-up clinics for sepsis patients and the demographics of the population as Prescott et al (20) was focused on a Medicare only population with a mean age of 78.6 years old.
There are several limitations to this study many of which are common to observational database research. This study relied on International Classification of Diseases and DRG coding provided by the hospitals to Premier. Although coding variations exist within and across hospitals, the degree to which coding variation may affect this analysis is unknown. Hospitals that submit data to Premier may differ from nonreporting hospitals due to the fact that Premier hospitals submit data to drive quality efforts, thus affecting the ability to generalize results to all U.S. hospitals. In comparison with the American Hospital Association (AHA) hospitals, the Premier hospitals have a similar distribution of geography, urbanicity, and teaching focus, whereas the size of the hospitals suggest that Premier hospitals are larger (21). However, the number of cases over the 7-year study period yields ~ 350,000 cases per year. Assuming Premier hospitals represent 20% of U.S. hospitals, this results in ~1.7 M sepsis hospitalizations per year, which is consistent with the most recent national estimates provided by Rhee et al (22). The 2018 AHA statistics show a difference in cost with smaller hospitals incurring greater cost per hospitalization (23). The findings of this study may underestimate the clinical and economic burden among smaller hospitals.
Last, the use of diagnosis codes to identify sepsis cases differs from clinical definitions. Cases which were clinically septic and/or treated for sepsis may have been missed by coders who go through medical records retrospectively for billing purposes, and therefore, the volume of sepsis patients and the total cohort costs reported here are likely underreported. The optimal method for accurately capturing sepsis cases from an epidemiologic perspective may be best through clinical criteria, but databases like the Premier dataset lack such details. The literature regarding the accuracy of sepsis diagnostic coding versus the use of clinical criteria for reporting of epidemiology does differ, but the use of the Premier dataset using specific sepsis diagnosis codes of case identification may better reflect the economic burden by avoiding dilution in the study with nonsepsis cases (22, 24). In addition, recent updates to the sepsis definitions (from Sepsis-2 to Sepsis-3) have introduced new classifications of sepsis severity, which may result in shifts in coding as the ICD-10 diagnosis and DRG codes are not evolving with the clinical definitions of sepsis. The new definitions remove the concept of severe sepsis leaving only two classifications: sepsis and septic shock. Future diagnostic codes and database analyses will need to address the new definitions and to determine the clinical utility of the new Sepsis-3 criteria in terms of sepsis detection especially given how such definitions may impact diagnosis codes and allocated DRG codes used for payment.
CONCLUSIONS
Early recognition and prompt treatment of sepsis remain the pivotal steps in reducing the overall burden of sepsis-related hospitalization. Our study focuses on the heterogeneity of sepsis cases and highlights less severe sepsis (sepsis without organ dysfunction), which accounts for the majority of cases and costs. By applying a nationally representative dataset, we could focus on differences within the sepsis population and understand the varying outcomes and costs when sepsis is POA and evaluated by severity level. The quantification of this granularity suggests an opportunity, both clinically and economically, to reduce the burden of sepsis in the United States, particularly through efforts to enhance early identification and treatment of patients in the earliest phases of sepsis.
Footnotes
*See also p. 2043.
This research was conducted at Premier, Inc.
Supported, in part, by Beckman Coulter, Inc.
Drs. Paoli and Reynolds are both employees of and hold stock in Beckman Coulter, Inc./Danaher Corp. (parent company of Beckman Coulter). Dr. Sinha is an employee of Premier, Inc., which received funding to conduct the research project. Dr. Gitlin is an employee of BluePath Solutions, which received funding to conduct the research project, and his institution received funding from Danaher Corp., Diagnostics & Life Science Platforms. Drs. Sinha’s and Crouser’s institutions received funding from Beckman Coulter, Inc. Dr. Crouser has received support from Beckman Coulter, Inc. as a scientific consultant and as principal investigator of a clinical trial investigating a novel sepsis biomarker, and his institution also received funding from the National Institutes of Health and Foundation for Sarcoidosis Research
REFERENCES
- 1.Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: Analysis of incidence, outcome, and associated costs of care. Crit Care Med 2001; 29:1303–1310. [DOI] [PubMed] [Google Scholar]
- 2.Martin GS, Mannino DM, Eaton S, et al. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med 2003; 348:1546–1554. [DOI] [PubMed] [Google Scholar]
- 3.Liu V, Escobar GJ, Greene JD, et al. Hospital deaths in patients with sepsis from 2 independent cohorts. JAMA 2014; 312:90–92. [DOI] [PubMed] [Google Scholar]
- 4.Martin GS. Sepsis, severe sepsis and septic shock: Changes in incidence, pathogens and outcomes. Expert Rev Anti Infect Ther 2012; 10:701–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hall MJ, Williams SN, DeFrances CJ, et al. Inpatient Care for Septicemia or Sepsis: A Challenge for Patients And Hospitals, 2000–2008. National Center for Health Statistics. Data Brief No. 62. June 2011. Available at: http://www.cdc.gov/nchs/data/databriefs/db62.pdf. Accessed June 24, 2016. [PubMed]
- 6.HCUP National Inpatient Sample (NIS): Healthcare Cost and Utilization Project (HCUP), 2013. Rockville, MD: Agency for Healthcare Research and Quality, Available at: at www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed June 24, 2016 [Google Scholar]
- 7.Torio CM, Moore BJ.National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2013. Available at: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb204-Most-Expensive-Hospital-Conditions.jsp. Accessed September 7, 2017. [PubMed]
- 8.O’Brien J.The Cost of Sepsis. CDC Safe Healthcare Blog. 9 Sept 2015. Available at: http://blogs.cdc.gov/safehealthcare/the-cost-of-sepsis/. Accessed March 3, 2016.
- 9.Judd WR, Stephens DM, Kennedy CA. Clinical and economic impact of a quality improvement initiative to enhance early recognition and treatment of sepsis. Ann Pharmacother 2014; 48:1269–1275. [DOI] [PubMed] [Google Scholar]
- 10.Whiles BB, Deis AS, Simpson SQ. Increased time to initial antimicrobial administration is associated with progression to septic shock in severe sepsis patients. Crit Care Med 2017; 45:623–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferrer R, Martin-Loeches I, Phillips G, et al. Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: Results from a guideline-based performance improvement program. Crit Care Med 2014; 42:1749–1755. [DOI] [PubMed] [Google Scholar]
- 12.Filbin MR, Arias SA, Camargo CA, Jr, et al. Sepsis visits and antibiotic utilization in U.S. emergency departments*. Crit Care Med 2014; 42:528–535. [DOI] [PubMed] [Google Scholar]
- 13.Kumar A, Roberts D, Wood KE, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 2006; 34:1589–1596. [DOI] [PubMed] [Google Scholar]
- 14.Liu VX, Fielding-Singh V, Greene JD, et al. The timing of early antibiotics and hospital mortality in sepsis. Am J Respir Crit Care Med 2017; 196:856–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pruinelli L, Westra BL, Yadav P, et al. Delay within the 3-hour surviving sepsis campaign guideline on mortality for patients with severe sepsis and septic shock. Crit Care Med 2018; 46:500–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones SL, Ashton CM, Kiehne LB, et al. Outcomes and resource use of sepsis-associated stays by presence on admission, severity, and hospital type. Med Care 2016; 54:303–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 2016; 315:801–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ost DE, Hall CS, Joseph G, et al. Decision analysis of antibiotic and diagnostic strategies in ventilator-associated pneumonia. Am J Respir Crit Care Med 2003; 168:1060–1067. [DOI] [PubMed] [Google Scholar]
- 19.Houck PM, Bratzler DW, Nsa W, et al. Timing of antibiotic administration and outcomes for Medicare patients hospitalized with community-acquired pneumonia. Arch Intern Med 2004; 164:637–644. [DOI] [PubMed] [Google Scholar]
- 20.Prescott HC, Langa KM, Liu V, et al. Increased 1-year healthcare use in survivors of severe sepsis. Am J Respir Crit Care Med 2014; 190:62–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Premier Applied Sciences, the Research and Analytics Division of Premier, Inc.: Premier Healthcare Database White Paper: Data That Informs and Performs, 2018. Premier Applied Sciences, Premier Inc. Available at: https://learn.premierinc.com/pharmacy-and-research/premier-healthcare-database-whitepaper. Accessed May 20, 2018.
- 22.Rhee C, Dantes R, Epstein L, et al. ; CDC Prevention Epicenter Program: Incidence and trends of sepsis in US hospitals using clinical vs claims data, 2009-2014. JAMA 2017; 318:1241–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.American Heart Association (AHA): AMA Hospital Statistics, 2018 Edition. Available at: https://www.aha.org/statistics/2016-12-27-aha-hospital-statistics-2018-edition. Accessed May 20, 2018
- 24.Jafarzadeh SR, Thomas BS, Marschall J, et al. Quantifying the improvement in sepsis diagnosis, documentation, and coding: The marginal causal effect of year of hospitalization on sepsis diagnosis. Ann Epidemiol 2016; 26:66–70. [DOI] [PMC free article] [PubMed] [Google Scholar]


