Abstract
The discharge of elderly patients from hospital on the basis of their independent gait program (DOPPO) is a new rehabilitation strategy for physically frail hospitalized elderly that aims to recover independent gait and to achieve ambulatory discharge. We retrospectively investigated baseline determinants of physical measures associated closely with the 6-min walking distance (6MWD) after DOPPO. Participants were 137 consecutive elderly inpatients, irrespective of the causative disease (mean age: 82±7 years; 76 women), who had a Short Physical Performance Battery (SPPB) score of less than 12 and low independent walking capacity. The rehabilitation comprised muscle stretching, muscle strengthening, balance training, and endurance exercise, including walking. The exercises were gradually increased until the goal of ambulatory discharge was attained. The SPPB, isometric knee-extension muscle strength (IKEMS), functional reach test (FRT), one-leg stance time (OLST), and the 10-m gait speed (TMGS) were measured, before and after the DOPPO intervention, and their association with the 6MWD was evaluated. All participants achieved ambulatory discharge, requiring on average 35±19 hospital days and 32±18 h of rehabilitation. The SPPB, IKEMS, FRT, OLST, and TMGS improved. The SPPB scores increased from 7.1 at baseline to 9.2 at discharge. Eighty-eight patients completed the 6MWD. The SPPB, IKEMS, FRT, OLST, and TMGS were strongly associated with the 6MWD. Only the baseline TMGS and SPPB predicted the 6MWD, with a cut-off TMGS value of 0.84 m/s providing the best prediction of achieving a distance of more than 300 m on the 6MWD. Thus, the baseline TMGS is the best prediction of the ambulatory outcome after the present DOPPO rehabilitation.
Keywords: ambulatory discharge, DOPPO, frail elderly, 10-m gait speed, Short Physical Performance Battery
Introduction
It is estimated that the proportion of octogenarians in Japan will reach 11.1% of the general population by 2025 (National Institute of Population and Social Security Research, 2012; Arai et al. 2015). In super-aging societies, such as Japan, the number of elderly patients with physical, mental, and social frailty is predicted to continue increasing. This is a major socioeconomic burden that will also affect the next generation. Thus, repetitive hospitalization of the same elderly individual is alarming, with the resulting sedentary lifestyle being a risk factor for the loss of walking ability, causing difficulty in achieving ambulatory discharge, irrespective of the underlying cause. Considering the importance of managing healthcare costs, identifying the most effective way to promote walking among frail elderly inpatients has become a leading rehabilitation issue in Japan.
In May 2014, the Japanese Geriatrics Society issued a statement on frailty (Ouchi and Arai, 2014), on the basis of the previous description by Fried et al. (2001), which is now accepted widely in Japan. Moreover, several initiatives have been developed to address frailty, including the establishment of the Japanese Association on Sarcopenia in 2016 (Arai, 2016) and the publication of the Asia-Pacific Clinical Practice Guidelines for the Management of Frailty in 2017 (Dent et al., 2017).
Physical frailty in elderly individuals leads to a self-perpetuating vicious cycle, accelerated by sarcopenia and malnutrition (Xue et al., 2008). Through this vicious cycle, low muscle strength and low muscle function develop, leading to a loss of balance and a decline in mobility, with an increase in the risk for falls and fall-related fractures. Ultimately, frail individuals require continuous nursing care. Thus, in April 2013, the Niigata-minami Hospital implemented a new rehabilitation program for frail hospitalized elderly individuals who have low walking capacity. Our ‘Discharge of elderly patients from hospital on the basis of their independent gait (DOPPO)’ aims to rehabilitate frail elderly to regain sufficient independent walking capacity for ambulatory discharge.
The end-point of our DOPPO intervention is the ability to achieve a distance of more than 300 m on the 6-min walk test 6MWD (ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories, 2002). However, measurement of the 6MWD in this clinical population is not easy in practice. Therefore, our aim in this study was to seek simpler baseline physical measures that would predict the capacity to achieve the 6MWD criterion of 300 m after the DOPPO intervention.
Patients and methods
We included consecutive frail hospitalized elderly, aged older than 65 years, who had low walking capacity. All patients consented to participate in the DOPPO project and completed the program. The presentation of the clinical results of our DOPPO project was approved by the Research Ethics Committee of our hospital (approval number: 1403).
Physical frailty was assessed using the Short Physical Performance Battery (SPPB) (Guralnik et al., 1994) just before the start of the DOPPO program. All participants had an SPPB score of less than 12 (but over 0). Walking capacity was determined from responses by the patient and/or his/her family on three parameters: ability to walk 30 m without pausing; ability to walk independently to meals; ability to walk independently to the bathroom. Individuals who did not fulfill these three criteria were candidates for the DOPPO program and were provided a doctor’s referral to the program. Patients with mental and social frailty, extremely low activities of daily living before hospitalization, and with a high risk for falls and/or bone fracture were excluded. Efforts were made to recruit as many hospitalized elderly individuals as possible for this study.
The DOPPO program has been presented in detail in all Japanese Journals (Izumi et al., 2016). However, in the first presentation in an official Journal, we will repeat the project in as much detail as possible. The DOPPO program is based on the Japanese Guidelines for Rehabilitation in Patients with Cardiovascular Disease (Japanese Circulation Society, 2012), and is very comprehensive. Activities are provided across four domains: systematic muscle stretching, lower limb muscle strengthening, balance training, using single-leg stance and/or tandem standing/walking, and endurance exercise, and using effort walking and/or a recumbent ergometer. For risk management, the program uses a gradual progression, starting with self-activities, and subsequently includes muscle strengthening and balance training, improving sit-to-stand, and increasing walking speed. The progression through these steps was individualized and based on a patient’s abilities and exercise capacity. Training was provided in bouts of at least 20 min, for a maximum of 60 min per one time, with rest provided as needed. If possible, the DOPPO was repeated twice a day. The exercise intensity was set to a level where a patient reported mild shortness of breath and/or felt lower limb fatigue (Borg scale score of 13) (Borg, 1974). Depending on a patient’s health status, the intervention was performed under hemodynamic monitoring, including electrocardiogram, as necessary.
The DOPPO goal was clearly stated for each patient: ‘Let’s recover your independent gait, to walk, if possible, to more than 300 m within 6 min on discharge.’ The DOPPO was always provided by well-trained physical and occupational therapists, supported by a nurse and a dietician, and supervised by a physiatrist. Before initiating the DOPPO training, the cardiovascular and orthopedic status of the patients was checked to avoid undue risk.
The following physical tests were repeated before and after the DOPPO. These included the SPPB (Guralnik et al., 1994), isometric knee-extension muscle strength (IKEMS), the functional reach test (FRT), one-leg standing time (OLST), and 10-m gait speed (TMGS). Lower limb muscle power was expressed as the IKEMS, measured using a fixed belt and a μTas F-1 dynamometer (Anima Corp., Tokyo, Japan), with the highest strength value (either the right or the left lower limb, N/kg body weight) used for the analysis. Balance capacity was measured, with the eyes open, using the FRT and OLST, with the highest value (right or left) used in the analysis. The TMGS was quantified as the speed required to walk along a 10-m straight path.
The outcome measure of the DOPPO program was the gait speed used to complete 6MWD, measured on the last day of the DOPPO program.
Statistical analyses
Statistical analyses were carried out using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan) (Kanda, 2013), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria), Ystat 2013 for Excel (Igakutosho Shuppan, Tokyo, Japan), and SPSS (version 24, IBM, Armonk, New York, USA). Data were reported as the mean±SD. Statistical significance was assumed at P less than 0.05. Wilcoxon’s signed-rank test was used to compare values before and after the DOPPO. Spearman’s correlation coefficients, multivariate analysis using the stepwise method, and binomial logistic regression analysis using the forward selection method were used to evaluate the association between the 6MWD, measured as the end-point of the DOPPO program and baseline physical measures. A receiver operating characteristic analysis was used to determine the cut-off values of baseline physical measure associated with ability to walk more than 300 m on the 6MWD test.
Results
From April 2013 to October 2016, of the 1732 hospitalized elderly individuals, 256 were referred to the DOPPO rehabilitation program and 137 completed the program, with their data included in the analysis. The group included 61 men and 76 women, with a mean age of 81.8±7.1 years, with 70.1% of our cohort being older than 80 years of age (Fig. 1). The underlying causes of hospitalization and decreased walking capacity varied widely, and included cardiovascular (29.9%), bone and muscle (16.8%), neurological (14.6%), respiratory (10.2%), hematological (6.6%), gastrointestinal (5.1%), and ‘other’ (16.8%) causes.
Fig. 1.
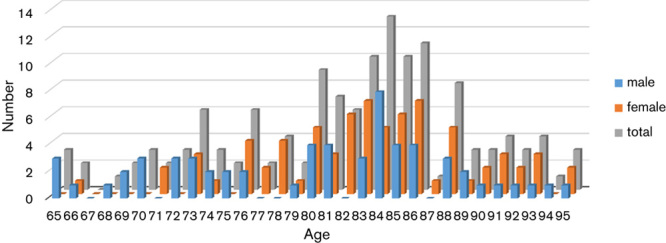
The age distribution of the participants, with 70.1% aged over 80 years.
All participants succeeded in recovering their independent walking capacity to achieve an ambulatory discharge status, with 83.2% of these patients (114) being discharged. The other 22.6% of patients were transferred to a nursing home. No adverse events were noted during the rehabilitation.
The outcomes of the DOPPO are summarized in Fig. 2. To reach the a priori goal of ambulatory discharge, patients required a rehabilitation period of 34.5±19.2 days, with 31.6±17.7 h of rehabilitation. Values for each measured variable of physical function improved, from baseline, at the end of the DOPPO program. The SPPB score increased from 7.1±2.5 to 9.2±2.5 patients (P<0.01), with 29 (21.2%) patients achieving the full score of SPPB. On the specific domains of the SPPB, improvement was as follows: balance improved from 2.9±1.2 to 3.5±0.9 patients (P<0.01); walking speed improved from 2.3±1.0 to 3.0±1.0 patients (P<0.01); and sit-to-stand improved from 1.9±1.2 to 2.8±1.3 patients (P<0.01). The IKEMS improved from 29.5±11.0 to 33.4±11.3% (P<0.01), the FRT improved from 24.1±9.1 to 28.5±8.4 cm (P<0.01), the OLST improved from 7.1±9.2 to 13.8±6.0 s (P<0.01), and the TMGS improved from 0.83±0.28 to 1.01±0.31 m/s (P<0.01).
Fig. 2.
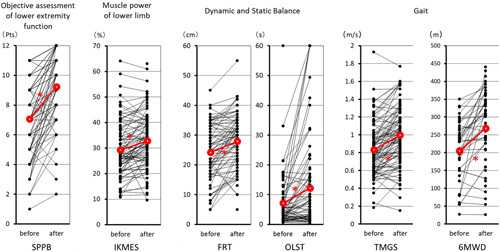
Improvement in physical function measures after the DOPPO program, with a marked improvement on the 6MWD. FRT, functional reach test (cm); IKEMS, isometric knee-extension muscle strength (%); 6MWD, 6-min walking distance; OLST, one-leg stance time (s); SPPB, Short Physical Performance Battery (points); TMGS, 10-m effort gait speed (m/s).
After completion of the DOPPO, 88 (64.2%) patients could complete the 6MWD test. For the other 49 patients, the 6MWD test was terminated by the physiatrist because of unstable walking. The distance covered during the 6MWD was 271.7±99.5 m (range: 26–445 m), with 39 (44.3%) patients achieving a distance of more than 300 m.
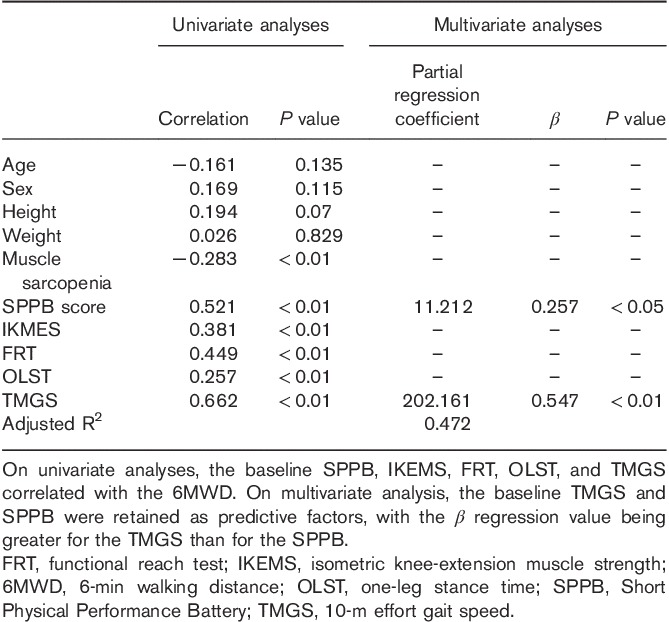
The following factors were associated with the 6MWD, with the following r and P values, respectively: age (−0.161 and 0.135); sex (0.169 and 0.115); height (0.194 and 0.07); weight (0.026 and 0.829); SPPB score (0.521 and <0.01); IKEMS (0.381 and <0.01); FRT (0.449 and <0.01); OLST (0.257 and <0.05); and TMGS (0.662 and <0.01). Significant factors on univariate analysis (SPPB, IKEMS, FRT, OLST, and TMGS) were included in a multivariate regression analysis, using a stepwise method, with only the TMGS and SPPB as independent predictive factors. The regression coefficients (β value) of the TMGS and SPPB were 0.547 and 0.257, indicative of the stronger predictive value of the TMGS than SPPB (Table 1).
Table 1.
Association between physical performance measures, at baseline, and the 6-m walk test after rehabilitation
Binomial regression analysis, with the forward selection method, identified the TMGS as the best independent predictor of a 6MWD distance of more than 300 m. The odds ratio, 95% confidence interval, and the P value of TMGS were 265.743, 7.783−9073.393, and less than 0.01, respectively (Fig. 3). Using a receiver operating characteristic analysis, we identified the cut-off TMGS value of 0.84 m/s as being predictive of a 6MWD of more than 300 m, with a sensitivity of 0.681, a specificity of 0.774, and an area under the curve of 0.774 (95% confidence interval, 0.676−0.872). In our cohort, 71.8% of patients with a baseline TMGS of more than 0.84 m/s achieved a 6MWD of more than 300 m.
Fig. 3.
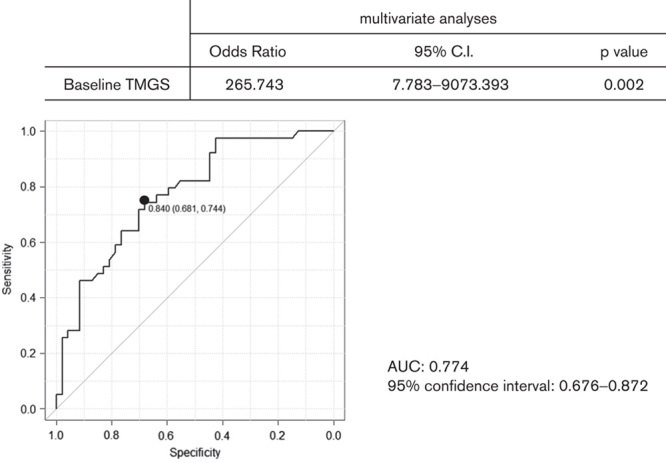
The cut-off criterion of the TMGS, predictive of achieving a distance of more than 300 m on the 6MWD. The cut-off value, sensitivity, and specificity were 0.840 m/s, 0.681, and 0.774, respectively. The area under the curve (AUC) was 0.774 (95% confidence interval: 0.676–0.872). CI, confidence interval; 6MWD, 6-min walking distance; TMGS, 10-m effort gait speed (m/s).
Discussion
To the best of our knowledge, the DOPPO is the first structured rehabilitation program for frail hospitalized elderly patients with poor independent walking capacity. The effectiveness of our program is underscored by the fact that the majority of patients in our study cohort were older than 80 years of age. Our measure of effectiveness was the ability to recover independent walking for ambulatory discharge, irrespective of the underlying cause of hospitalization. Among our cohort, 83.2% were discharged home, indicative of the capacity of these elderly patients overcoming their own physical frailty and recovering sufficient walking ability for return to independent self-care. The successful medical and social outcomes of the DOPPO will be easily acceptable to reduce the burden of a super-aging society, such as Japan.
We used the SPPB as a measure of physical frail assessment. Although other more complete frailty diagnostic tools have been used widely, such as the Fried score (Fried et al., 2001), we were only concerned with physical frailty in our study, aiming to improve independent daily activity. The SPPB provides a convenient assessment of physical function (Guralnik et al., 1994). The SPPB assesses three domains of mobility (balance, gait speed, and sit-to-stand time), with a possible score ranging 0 to 12. Performance on each of these domains can inform the diagnosis and rehabilitation process. Although the SPBB score is rather crude, it was predictive of the 6MDW after the DOPPO program. Therefore, the SPBB score can provide a clinical index to identify patients who would benefit from the DOPPO program, to guide the rehabilitation, and predict the short-term outcome. All patients in our study cohort fulfilled the concept of frailty proposed by Fried et al. (2001) and by the Asia-Pacific Clinical Practice Guidelines for the Management of Frailty (Dent et al., 2017), including poor physical activity, slow gait speed, and muscle weakness.
The DOPPO program was initiated immediately after completion of the medical treatment for the causative disease. Although the overall goal was to recover the maximum walking distance (with a target of >300 m) on the 6MWD, the goal of the intervention was individualized to some extent. The level of intensity was set at a Borg scale (Borg, 1974) score of 13 (mild shortness of breath and/or lower limb fatigue), which is cited by the Japanese Guidelines for Cardiovascular Rehabilitation (Japanese Circulation Society, 2012) as aligning with the anaerobic threshold for exercise training. As it is not always possible to perform cardiopulmonary testing in elderly individuals, the Borg scale provides a reasonable measure of exertion during exercise.
We used the 6MWD as the outcome measure of the effectiveness of the DOPPO program, with a distance walked more than 300 m within 6 min considered to be the best indicator for ambulatory discharge and to return to independent self-care. The distance of 300 m was selected on the basis of the concept of a ‘compact city,’ which has gained interest in the field of urban planning for the elderly (Yekyeong, 2012), where selective attention is paid to the distance between public transport facilities and the residential area to facilitate transportation and access to shopping. Several studies (Faggianoa et al., 2004; Cahalin et al., 1996; Roul et al., 1998b; Arslan et al., 2007) have reported that the ability for independent walking more than 300 m within 6 min is predictive of lower mortality and morbidity in elderly patients with heart failure, irrespective of the severity of the underlying disease. Our study cohort included patients with symptomatic and occult cardiovascular disease. Therefore, the training target for the 6MWD of 300 m seems appropriate.
We sought baseline predictors of achieving the 300 m 6MWD criterion. We identified the SPPB and TMGS, at baseline, as independent predictors of the 300-m 6MWD. The best predictor was a TMGS of 0.84 m/s, with an area under the curve of 0.774, with 71.8% of patients in our study group having a TMGS of more than 0.84 m/s at baseline exceeding the criterion of 300 m on the 6MWD at the end of the DOPPO program, and regained their independence in activities of daily living of self-care. Although our focus was on elderly patients who developed frailty secondary to hospitalization, with the program being sufficiently challenging to regain independent walking, we did not neglect individuals who were unable to achieve 300 m on the 6MWD at discharge. As shown in Fig. 2, patients with a baseline TMGS of more than 0.84 m/s could progress through the rehabilitation program. For patients with a TMGS of less than 0.84 m/s at baseline, the program was graded on a patient-by-patient basis. Although these patients did not reach the desired discharge criterion of a 6MWD of more than 300 m, a meaningful improvement in physical function was attained from the perspective of the patients and their family/caregivers. These improvements would decrease the burden of care, despite not achieving the criterion for ambulatory discharge.
Clinically, it is important to note that we included in our DOPPO program patients with moderate levels of cognitive impairment as long as they were able to communicate and comply with instructions. Further research should evaluate the effectiveness of the DOPPO program in enhancing mental and social function, in addition to its benefits on physical function.
Kamiya et al. (2018) reported that gait speed has the same predictive value as the 6MWD for all-cause mortality. We found in our study that the TMGS score was predictive of achieving a distance of more than 300 m on the 6MWD. The TMGS might also better reflect the standing and walking capacity that is required for independence in performing activities of daily living as it includes phases of acceleration and deceleration, as well as having acceptable levels of interobserver and intraobserver reliability (Watson, 2002; Japanese Physical Therapy Association, 2011; Peters et al., 2013). For these reasons, the TMGS could be used as the outcome measure for the DOPPO program.
Limitations
This was a single-center study; therefore, the possibility of bias cannot be excluded. Thus, our findings will need to be confirmed in a multicenter trial. In addition, our single-arm design did not include a control group. Once the DOPPO program has been standardized, controlled trials can provide high-quality evidence on the effectiveness of the program.
Conclusion
The DOPPO is a new rehabilitation program for elderly inpatients with physical frailty, particularly those aged older than 80 years of age. The aim of the program is to recover independent gait for ambulatory discharge. The program led to a marked improvement in physical measures (SPPB, IKEMS, FRT, OLST, and TMGS), with a baseline TMGS of more than 0.84 m/s being predictive of achieving the more than 300 m 6MWD criterion for ambulatory discharge.
Acknowledgements
This study was supported in part by the medical association of Niigata city, Japan (NO GC01920163 Uehara), as well as by the Japan Agency for Medical Research and Development (No. JP17ek0210058 Obata and Izumi).
Conflicts of interest
There are no conflicts of interest.
References
- Arai H. (2016). Japanese Association on Sarcopenia and Frailty. Available at: http://jssf.umin.jp/aisatsu.html. [Accessed 5 June 2018].
- Arai H, Ouchi Y, Toba K, Endo T, Shimokado K, Tsubota K, et al. (2015). Japan as the front-runner of super-aged societies: perspectives from medicine and medical care in Japan. Geriatr Gerontol Int 15:673–687. [DOI] [PubMed] [Google Scholar]
- Arslan S, Erol MK, Gundogdu F, Sevimli S, Aksakai E, Senocak H, et al. (2007). Prognostic value of 6-minute walk test in stable outpatients with heart failure. Tex Heart Inst J 34:166–169. [PMC free article] [PubMed] [Google Scholar]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories (2002). ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 166:111–117. [DOI] [PubMed] [Google Scholar]
- Borg GA. (1974). Perceived exertion. Exerc Sport Sci Rev 2:131–153. [PubMed] [Google Scholar]
- Cahalin LP, Mathier M, Semigran MJ, Dec WG, DiSalvo TG. (1996). The 6-min walk test predicts peak oxygen uptake and survival in patients with advanced heart failure. Chest 110:325–332. [DOI] [PubMed] [Google Scholar]
- Dent E, Lien C, Lim WS, Wong WC, Wong CH, Ng TP, et al. (2017). The Asia-Pacific clinical practice guidelines for the management of frailty. J Am Med Dir Assoc 18:564–575. [DOI] [PubMed] [Google Scholar]
- Faggianoa P, D’Aloiab A, Gualenic A, Brentana L, Dei Cas L. (2004). The 6 min walking test in chronic heart failure: indications, interpretation and limitations from a review of the literature. Eur J Heart Failure 6:687–691. [DOI] [PubMed] [Google Scholar]
- Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. (2001). Frailty in the older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56:M146–M157. [DOI] [PubMed] [Google Scholar]
- Guralnik JM, Simonsick EM, Furrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. (1994). A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 49:M85–M94. [DOI] [PubMed] [Google Scholar]
- Izumi T, Uehara A, Izumi Y, Suzuki Y, Obata H. (2016). A project for discharge of super-elderly patients from hospital on the basis of their independent gait. Jpn J Rehabil Med 53:392–400. [Google Scholar]
- Japanese Circulation Society (2012). Guidelines for rehabilitation in patients with cardiovascular disease. Available at: http://www.j-circ.or.jp/guideline/pdf/JCS2012_ nohara_h.pdf. [Accessed 5 June 2018].
- Japanese Physical Therapy Association (2011). Japanese guideline for physical therapy. Available at: http://www.japanpt.or.jp/upload/jspt/obj/files/guideline/19_physical_vulnerability.pdf. [Accessed 5 June 2018].
- Kamiya K, Hamazaki N, Matsue Y, MezzaniA, Corra U, Matsuzawa R, et al. (2018). Gait speed has comparable prognostic capability to six-minute walk distance in older patients with cardiovascular disease. Eur J Prev Cardiol 25:212–219. [DOI] [PubMed] [Google Scholar]
- Kanda Y. (2013). Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 48:452–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Population and Social Security Research (2012) [Population Projection for Japan] Available at: http://www.ipss.go.jp/syoushika/tohkei/newest04/sh2401smm.html. [Accessed 5 June 2018].
- Ouchi Y, Arai H. (2014). Statement on frailty from The Japan Geriatrics Society. Available at: http://www.jpn-geriat-soc.or.jp/info/topics/pdf/20140513_01_01.pdf. [Accessed 5 June 2018].
- Peters DM, Fritz SL, Krotish DE. (2013). Assessing the reliability and validity of a shorter walk test compared with the 10-meter walk test for measurements of gait speed in healthy, older adults. J Geriatr Phys Ther 36:24–30. [DOI] [PubMed] [Google Scholar]
- Roul G, Germain P, Bareiss P. (1998). Does the 6-min walk test predict the prognosis in patients with NYHA class II or III chronic heart failure? Am Heart J 136:449–457. [DOI] [PubMed] [Google Scholar]
- Watson MJ. (2002). Refining the ten-metre walking test for use with neurologically impaired people. Physiotherapy 88:386–397. [Google Scholar]
- Xue QL, Bandeen-Roche K, Varadhan R, Zhou J, Fried LP. (2008). Initial manifestations of frailty criteria and the development of frailty phenotype in the women’s health and aging study II. J Gerontol A Biol Sci Med Sci 63A:984–990. [DOI] [PubMed] [Google Scholar]
- Yekyeong S.Kim T, Ramos C, Kim H, Kiumi A, Mohammed S, Ślęzak D. (2012). TOD as a rail integrated urban regeneration strategies of old city through case study about Toyama Station and the surroundings area in Japan. Computer applications for software engineering, disaster recovery, and business continuity 340 Berlin, Heidelberg: Springer; 429–436. [Google Scholar]


