Abstract
Background:
To investigate the efficacy of acellular dermal matrix in penis augmentation (ADMPA) for premature ejaculation (PE).
Methods:
A total of 39 patients treated with ADM in penis augmentation from June 2014 to December 2017 were evaluated. Detailed evaluations on PE were conducted before operation and at the 6-month and 2-year follow-up visits after operation. Self-estimated intravaginal ejaculatory latency time (IELT) and 5-item version of the International Index of Erectile Function (IIEF-5) were used to measure the ejaculation and the erectile function for all subjects.
Results:
Compared to the baseline data, the IELT and IIEF-5 scores were increased, and PE was relieved at 6 months and 2 years after operation. No major complications occurred in the series. Minor complications were resolved with conservative treatment within 3 weeks. The psychosexual impact of the operation was beneficial in the majority of cases.
Conclusion:
Our survey systematically evaluated the effects of ADMPA for PE. ADMPA might be an optional surgical method in patients with PE, especially for those who seek penile augmentation. However, given the small amount of cases involved in this study, further studies on the effect of ADMPA for PE were still needed.
Keywords: augmentation, glans penis, hypersensitivity, premature ejaculation
1. Introduction
Men are often worried about the size of their penis and ejaculatory latency time, and sometimes seek enhancement to improve their self-esteem or to satisfy and/or impress their partners.[1] A variety of exogenous materials has been used in procedures to enhance the penile girth, since penile augmentation was reported in the 19th century.[2,3] Allografts in the form of an acellular inert dermal matrix derived from donated human skin tissue have also been used for penile girth. Penile girth enlargement by acellular dermal matrix (ADM) grafts has several advantages over augmentation with autogenous dermis-fat grafts: the elimination of donor site morbidity and a significantly shorter operation time.[4] With this approach, through a short dorsal incision at the base of the penis, the scar is concealed in a crease covered by pubic hair and thus hardly visible. Although a survey conducted by Tealab et al showed that penile augmentation by porcine acellular dermal grafts might negatively affect male sexual status (4 in 18 patients reported decreased penile sensation at 6-month visit),[5] penile enlargement by implantation of ADM was a safe and effective operation in most of the reports[4,6] and, no major complications occurred in the patients received penile augmentation by ADM.[7]
To the best of our knowledge, there were few studies to evaluate the relationships between adult penile augmentation by ADM and premature ejaculation (PE). Therefore, we conducted an observational study to investigate whether there were any relationship between ADMPA and PE.
2. Subjects and methods
2.1. Subjects, inclusion criteria, and exclusion criteria
A total of 39 patients treated with ADM in penis augmentation from June 2014 to December 2017 were evaluated (mean age at the time of surgery was 29 years, range 24–37). The indications for augmentation were the perception of a short penis, seeking more sexual pleasure, or a combination of both.
Inclusion criteria: the age of patients treated with ADMPA was over 18 years; all subjects had not been treated with any penile augmentations prior to ADMPA; all subjects had have a heterosexual, stable, and monogamous sexual relationship with the same partner for at least 6 months. In addition, because some subjective questions were asked in our study, eligible men should be able to comprehend and speak Chinese.
Exclusion criteria mainly included deformity of penis, a bleeding disorder, keloid formation, and other conditions that might unduly increase the risks of elective surgery. In addition, men who have used medications that could affect their ejaculatory function were excluded (e.g., selective serotonin reuptake inhibitors and phosphodiesterase type inhibitors).
2.2. Study design and procedure
Prior to the survey, all subjects were informed about the procedure of the survey, and those who participated were asked to provide written consent. The IRB was obtained from Peking University People's Hospital. This survey was designed as a 3-stage protocol.
Firstly, prior to the ADMPA, all subjects were asked to undergo a physical examination by an experienced clinician. Then, all subjects were asked to complete a verbal questionnaire, which included information regarding basic demographic variables (e.g., age and educational and occupational status), medical and sexual histories (e.g., self-estimated intravaginal ejaculatory latency time [IELT], duration of the relationship, and frequency of sexual intercourse), and self-estimated scales (e.g., the Chinese version of International Index of Erectile Function-5 [IIEF-5]).[8] The contents of verbal questionnaire were recorded and assessed by a single physician to exclude interpersonal variation. In addition, based on the PE definition suggested by ISSM,[9–11] men were diagnosed with lifelong PE if they experienced vaginal penetration for <1 minute, a loss of control, and/or negative sexual consequences. The IIEF-5 questionnaire contained 5 questions that were answered according to symptoms (scale range 0–5). IIEF-5 scores ≥22 points were rated as normal erectile function, while scores <22 were rated as erectile dysfunction (ED). The Chinese version of IIEF-5 has been used in Chinese male population in previous studies.[12] The Cronbach alpha coefficients for the Chinese version of IIEF-5 in our survey were 0.79, which indicated acceptable internal consistent reliability. Emotional, psychologic and social factors are excluded by patient reporting before answering the questionnaires. The flaccid girth (Fig. 1A) and erect girth of penis was measured before operation. In the 2nd stage, all men received a penile augmentation with ADM. Briefly, under local or spinal anesthesia, a circumferential subcoronal incision was used for penile degloving. The incision was deepened through the skin, Colles’ fascia, and down to Buck fascia, which was preserved. The shaft was then degloved down to the root of the penis. One layer of ADM (10 cm × 10 cm) was incised according to the penis size and then used to wrap around the penile shaft from the coronal sulcus to the root (Fig. 2A and B). These grafts were then sutured to Buck fascia with 4-0 vicryl from the root to coronary sulcus of glans. A pressure bandage was then used to wrap the penis with moderate compression to avoid these grafts’ shifting, wound hematoma and edema of penis, exclusively around the shaft (Fig. 2C). Antibiotic prophylaxis began to be used the night before surgery and continued for 1 week after surgery. Patients were instructed not to have sexual intercourse for the first 2 months after surgery. The incision after operation is shown in Figure 3.
Figure 1.
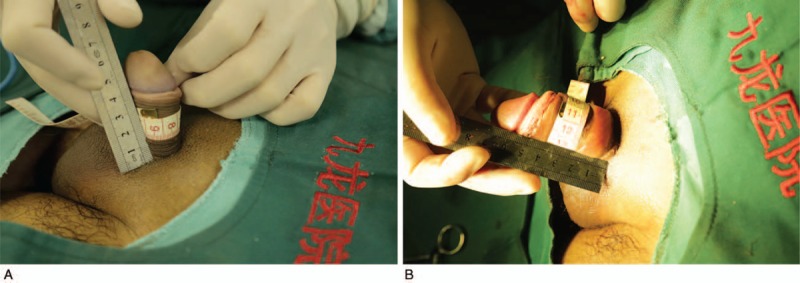
The flaccid girth of penis before and after operation. (A) The flaccid girth before operation. (B) The flaccid girth after operation.
Figure 2.
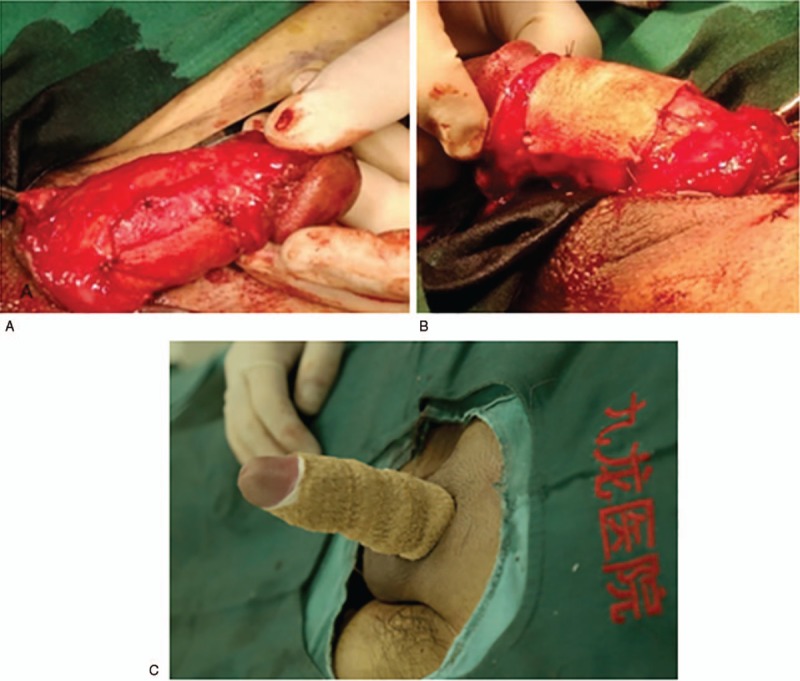
(A) The shaft was degloved down to the root of the penis. (B) ADM was wrapped around the penile shaft and sutured to Buck fascia. (C) The penis was wrapped with a 5-cm pressure bandage after operation.
Figure 3.
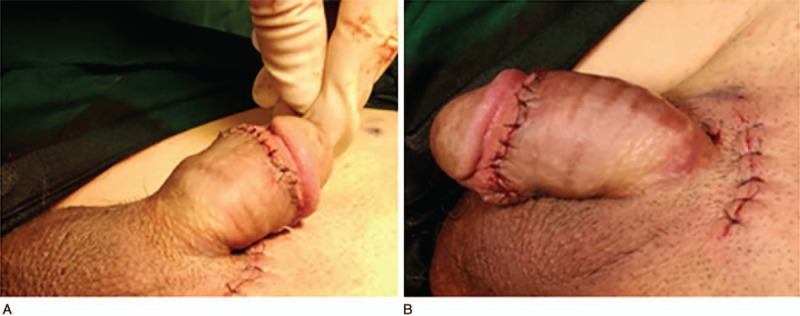
(A) The penis after the completion of penis augmentation operation. (B) The infrapubic incision was made for penile lengthening.
The 3rd stage involved 6-month and 2-year follow-up visits. At the visit, all subjects underwent a standardized medical history and physical examination. Then, information on ejaculatory and erectile function was collected by the same physician who conducted the verbal questionnaire using a verbal questionnaire, which mainly concentrated on sexual history, and included the Chinese assessment of IELT and IIEF-5. The flaccid girth (Fig. 1B) and erect girth of penis after operation was measured. Finally, detailed records for all subjects before circumcision and at follow-up visit were entered into the database.
2.3. Statistical analysis
All statistical analyses were performed using the SPSS software (version 13.0; SPSS Inc, Chicago, IL). Descriptive statistics were used to summarize the subjects’ characteristics. Data on demographic information for all subjects were expressed as mean ± standard deviation (SD). Data (including self-estimated IELT and IIEF-5 measurements) at baseline (before operation) and 6-month and 2-year follow-up visit for all subjects were expressed as mean ± SD. Data with a normal distribution were evaluated by analysis of variance and paired t test. P < .05 was considered to be statistically significant.
3. Results
3.1. Demographic information
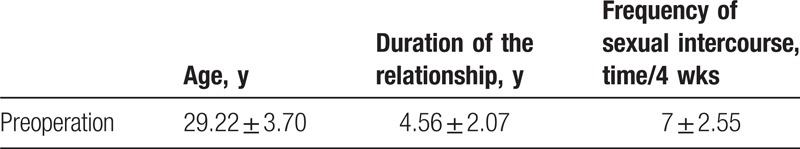
Of the 39 patients enrolled in the study, 39 (100%) males completed 6-month and 2-year follow-up. Detailed demographic information for all subjects at baseline is summarized in Table 1.
Table 1.
Demographic information and sexual status for all subjects prior to operation.
3.2. Outcomes of penile circumference, IELT, and IIEF-5
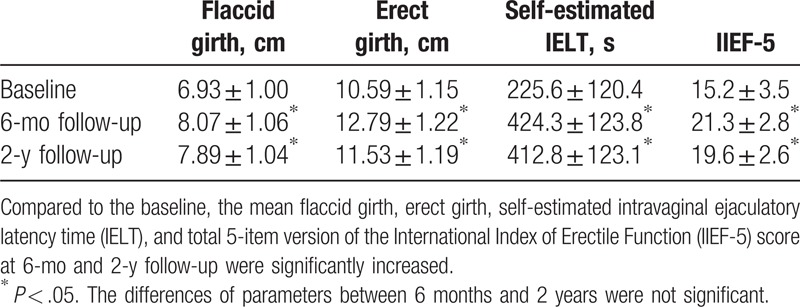
As shown in Table 2, the mean flaccid girth and erect girth were 6.93 ± 1.00 cm and 10.59 ± 1.15 cm, respectively; 8.07 ± 1.06 cm and 12.79 ± 1.22 cm at 6 months, respectively; 7.89 ± 1.04 cm and 11.53 ± 1.19 cm at 2 years, respectively. Compared to the baseline (225.6 ± 120.4 seconds and 15.2 ± 3.5), the mean self-estimated IELT and total IIEF-5 scores were increased to 424.3 ± 123.8 seconds and 21.33 ± 2.8 at 6 months, to 412.8 ± 123.1 seconds and 19.6 ± 2.6 at 2 years (P < .05). Although the mean flaccid girth, erect girth, self-estimated IELT, and total IIEF-5 score were slightly decreased at 2 years compared to those at 6 months, statistical differences were not observed. No major complications occurred. Although 2 patients developed delayed wound healing, the ADM was not exposed and the 2 patients’ wounds healed well after recurrent wound dressing changes for 1 month.
Table 2.
Outcomes of penile circumference, IELT, and IIEF-5 at baseline and follow-up visit.
4. Discussion
The PE was a multifactorial disease that might caused by a variety of factors, including biologic and psychologic aspects. Management of PE has evolved tremendously over the last 20 years. Current treatment choice for PE is medical treatment.[13] However, the recurrence after withdrawal of medication is still the main limitation of medical treatment for PE.[14] Patients with primary PE often had penile hypersensitivity, which provided further implications for an organic basis of PE.[15] In hypersensitivity of glans penis, various topical agents were applied, but the efficacies were still controversial.
Surgical treatments to decrease sensation of the glans had demonstrated efficacy on treating PE but were not recommended due to possible sensory loss and rare ED. The major concern of guideline committees was not efficacy but safety. Dorsal neurectomy was also created to decrease the sensitivity of glans penis. Dorsal neurectomy was not an established treatment for penile hypersensitivity ejaculation due to the uncertain pathophysiology, invasiveness, and side effects, for example, numbness paresthesia, pain for neuroma, Peyronie disease, and even ED.[16–18] Despite these limitations, dorsal neurectomy was still performed in selective patients who do not respond to conventional treatment for PE.
Hyaluronic acid (HA) gel glans penis augmentation treating PE had also gained popularity in some Asian country, like South Korea, albeit at a slower rate than dorsal nerve neurectomy.[19] Glans penis augmentation by subcutaneous injections of HA gel was initially developed to augment a small glans penis, but some patients were reported to have PE improvement treated with HA gel.[16] They postulated the theoretical efficacy of glans penis augmentation by subcutaneous injections of HA gel (GPAH) in patients with PE. It neither completely abolished sense of the glans or penis nor caused sexual dysfunction because GPAH did not affect the dorsal nerve, especially the dorsal nerve in the glans. However, the main limitations of GPAH were possible long-term volume loss, unnaturally looking surface, expense of filler, and lack of multicenter studies. Major contributing factors of sensation in glans penis were distribution of dorsal nerve, number of receptor, threshold of receptor, and accessibility of stimuli to the receptor. Therefore, new treatment strategies for PE should be studied to increase the efficacy of treatment on PE and decrease the complications.
The ADM has been used with increased frequency over the last decade to assist during prosthetic breast reconstruction and other reconstructive surgeries.[20–22] ADM was also used for patients with penile augmentation and no major complications occurred in the patients received penile augmentation with ADM.[4,5,7] Alei et al used porcine dermal acellular grafts for penile augmentation in 69 candidates and followed for more than 1 year. They reported a 40% increase in penile girth during flaccidity, and 22% during erection with no major complications.[7]
Results from our survey showed that self-estimated IELT was significantly associated with adult penile augmentation with ADM. At the 6-month and 2-year visits, patients treated with the penile augmentation by ADMPA were with higher self-estimated IELT and total IIEF-5 score compared with that at baseline. In addition, the flaccid girth and erect girth were also increased after treatment with ADMPA. No major complications occurred in the series. Minor complications were resolved with conservative treatment within 3 weeks. Sexual activity was resumed from 2 months after surgery.
Combining with the above parameters such as self-estimated IELT and IIEF-5 questions, we were able to perform a comprehensive analysis of the relationships between adult penile augmentation with ADM and PE. In addition, there were no significant differences at 6-month and 2-year follow-up, which indicated a relative stable efficacy of ADMPA for PE. Therefore, our findings might provide a framework for understanding the effect of penile augmentation with ADM on sexual dysfunction. ADMPA for PE might work in 3 ways. Firstly, ADMPA may take effect in the same way as GPAH. ADMs inhibited the tactic stimuli to reach to receptor. The skin of human phallus was innervated by the dorsal nerve of the penis (DNP), trunk of which was composed of 2 different populations of axons.[18] The 1st group traveling along the dorsal midline and terminating in the glans and the other group of fibers radiated from the main trunk over the lateral and ventral aspects of the penile shaft with branches to the corpus spongiosum and urethra.[23,24] At 1 to 2 cm proximal to the corona glandis, the DNP dorsal trunk divided into 2 to 3 nerve bundles. The DNP and its branches along the shaft run just beneath the skin and fascia, the main branches within the glans are 3 to 6 mm from the epithelial surface. The extent of nerve fibers, including in dorsal neurectomy, was important in postoperative sensory of glans penis.[25] ADMs sutured to Buck fascia might cover the micro-branches of the DNP continuously, which resulted in depression of receptor threshold. Second, ADMPA may decrease the proprioception of penis, especially when the ADM is very thick. As we know, millions of proprioception receptors are located in different parts of human body, such as joint space, skin, inner ear, and so forth.[26] Undoubtedly, proprioception receptors are also located in the penis and deeper layer of the skin.[27,28] These receptors are responsible for pressure difference and temperature change in the sexual intercourse.[29–31] Third, glans penis augmentation could increased self-esteem and self-confidence of patients, which might act positively for PE.[32]
Several limitations of the currently study should be considered. First, the limitation of the present study was relatively few patients, which possibly resulted in a type II statistical error, and thus the results and conclusions must be considered provisional until other studies confirm or refute them. Second, although 6-month and 2-year follow-up visits were conducted in our study, longer follow-up visit (e.g., 5-year follow-up visit) should be performed in future studies. Third, this study was patient oriented and based only on subjective reports. Objective data such as penile biothesiometry should be measured to assess penile sensation in the future studies. Fourth, the subjects in our study were not diagnosed with PE, because we could not assure the efficacy of ADMPA on PE but it was effective and safe for girth augmentation. In next step, we need more patients with PE in future studies to demonstrate the efficacy in these targeted patient populations.
5. Conclusion
With the assessments of IELT and IIEF-5, our survey systematically evaluated the effect of ADMPA on PE in China. It provided a better framework with which to determine their relationships. At 6-month and 2-year follow-up visits, patients treated with ADMPA experienced higher IELT and better scores of control over ejaculation than before. ADMPA was found to be associated with PE and might be an optional surgical method in patients with PE, especially for those who seek penile augmentation.
Author contributions
Data curation: Qing Li, Wenjun Bai.
Formal analysis: Min Zhang.
Funding acquisition: Tao Xu.
Investigation: Xiaowei Zhang.
Methodology: Yuanyi Wu, Qing Li.
Project administration: Xiaowei Zhang.
Resources: Wenjun Bai.
Software: Huaqi Yin.
Supervision: Tao Xu.
Validation: Huaqi Yin.
Writing – original draft: Xiaowei Zhang.
Writing – review & editing: Xiaowei Zhang, Tao Xu.
Footnotes
Abbreviations: ADM = acellular dermal matrix, ADMPA = acellular dermal matrix in penis augmentation, DNP = dorsal nerve of the penis, GPAH = glans penis augmentation by subcutaneous injections of hyaluronic acid gel, HA = hyaluronic acid, IELT = intravaginal ejaculatory latency time, IIEF-5 = 5-item version of the International Index of Erectile Function, PE = premature ejaculation.
Informed consent was obtained from all participants. Permissions for use were received from participants who provided photos.
This work was supported by the Specialized Research Fund for the Doctoral Program of Higher Education of China (grant no: 20120001120056), and National Natural Science Foundation of China (grant no: 81472393).
The authors have no conflicts of interest to disclose.
References
- [1].Vardi Y, Har-Shai Y, Gil T, et al. A critical analysis of penile enhancement procedures for patients with normal penile size: Surgical techniques, success, and complications. EUR UROL 2008;54:1042–50. [DOI] [PubMed] [Google Scholar]
- [2].Silberstein J, Downs T, Goldstein I. Penile injection with silicone: case report and review of the literature. J Sex Med 2008;5:2231–7. [DOI] [PubMed] [Google Scholar]
- [3].Shamsodini A, Al-Ansari AA, Talib RA, et al. Complications of penile augmentation by use of nonmedical industrial silicone. J Sex Med 2012;9:3279–83. [DOI] [PubMed] [Google Scholar]
- [4].Zhang JM, Cui YY, Pan SJ, et al. Penile augmentation using acellular dermal matrix [in Chinese]. Zhonghua Zheng Xing Wai Ke Za Zhi 2004;20:418–20. [PubMed] [Google Scholar]
- [5].Tealab AA, Maarouf AM, Habous M, et al. The use of an acellular collagen matrix in penile augmentation: a pilot study in Saudi Arabia. Arab J Urol 2013;11:169–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Park JY, Lee TG, Kim JY, et al. Acellular dermal matrix to treat full thickness skin defects: follow-up subjective and objective skin quality assessments. Arch Craniofac Surg 2014;15:14–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Alei G, Letizia P, Ricottilli F, et al. Original technique for penile girth augmentation through porcine dermal acellular grafts: Results in a 69-patient series. J Sex Med 2012;9:1945–53. [DOI] [PubMed] [Google Scholar]
- [8].Hatzichristou D, Rosen RC, Broderick G, et al. Clinical evaluation and management strategy for sexual dysfunction in men and women. J Sex Med 2004;1:49–57. [DOI] [PubMed] [Google Scholar]
- [9].McMahon CG, Althof SE, Waldinger MD, et al. An evidence-based definition of lifelong premature ejaculation: Report of the International Society for Sexual Medicine (ISSM) ad hoc committee for the definition of premature ejaculation. J Sex Med 2008;5:1590–606. [DOI] [PubMed] [Google Scholar]
- [10].Serefoglu EC, McMahon CG, Waldinger MD, et al. An evidence-based unified definition of lifelong and acquired premature ejaculation: Report of the second international society for sexual medicine ad hoc committee for the definition of premature ejaculation. Sex Med 2014;2:41–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Althof SE, McMahon CG, Waldinger MD, et al. An update of the international society of sexual medicine's guidelines for the diagnosis and treatment of premature ejaculation (PE). Sex Med 2014;2:60–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Gao J, Zhang X, Su P, et al. The impact of intravaginal ejaculatory latency time and erectile function on anxiety and depression in the four types of premature ejaculation: a large cross-sectional study in a Chinese population. J Sex Med 2014;11:521–8. [DOI] [PubMed] [Google Scholar]
- [13].Hisasue S. The drug treatment of premature ejaculation. Transl Androl Urol 2016;5:482–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Mantovani F. Pharmacological/dynamic rehabilitative behavioural therapy for premature ejaculation: Results of a pilot study. Arch Ital Urol Androl 2017;89:148–50. [DOI] [PubMed] [Google Scholar]
- [15].Xin ZC, Chung WS, Choi YD, et al. Penile sensitivity in patients with primary premature ejaculation. J Urol 1996;156:979–81. [PubMed] [Google Scholar]
- [16].Kim JJ, Kwak TI, Jeon BG, et al. Effects of glans penis augmentation using hyaluronic acid gel for premature ejaculation. Int J Impot Res 2004;16:547–51. [DOI] [PubMed] [Google Scholar]
- [17].Kwak TI, Jin MH, Kim JJ, et al. Long-term effects of glans penis augmentation using injectable hyaluronic acid gel for premature ejaculation. Int J Impot Res 2008;20:425–8. [DOI] [PubMed] [Google Scholar]
- [18].Yang CC, Bradley WE. Neuroanatomy of the penile portion of the human dorsal nerve of the penis. Br J Urol 1998;82:109–13. [DOI] [PubMed] [Google Scholar]
- [19].Yang DY, Ko K, Lee WK, et al. Urologist's practice patterns including surgical treatment in the management of premature ejaculation: a Korean nationwide survey. World J Mens Health 2013;31:226–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Nahabedian MY. Acellular human dermis implantation in 153 immediate two-stage tissue expander breast reconstructions: determining the incidence and significant predictors of complications. Plast Reconstr Surg 2011;127:481–2. [DOI] [PubMed] [Google Scholar]
- [21].Lee JH, Park Y, Choi KW, et al. The effect of sterile acellular dermal matrix use on complication rates in implant-based immediate breast reconstructions. Arch Plast Surg 2016;43:523–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Ganske I, Verma K, Rosen H, et al. Minimizing complications with the use of acellular dermal matrix for immediate implant-based breast reconstruction. Ann Plast Surg 2013;71:464–70. [DOI] [PubMed] [Google Scholar]
- [23].Suhaimi FH, Abd GN, Das S. Re: Kozacioglu et al.: Anatomy of the dorsal nerve of the penis, clinical implications (Urology 2014;83:121-125). Urology 2014;83:1207–8. [DOI] [PubMed] [Google Scholar]
- [24].Kozacioglu Z, Kiray A, Ergur I, et al. Anatomy of the dorsal nerve of the penis, clinical implications. Urology 2014;83:121–4. [DOI] [PubMed] [Google Scholar]
- [25].Morey AF. Re: Anatomy of the dorsal nerve of the penis, clinical implications. J Urol 2014;191:1813–4. [DOI] [PubMed] [Google Scholar]
- [26].Proske U, Gandevia SC. The proprioceptive senses: their roles in signaling body shape, body position and movement, and muscle force. Physiol Rev 2012;92:1651–97. [DOI] [PubMed] [Google Scholar]
- [27].Yiee JH, Baskin LS. Penile embryology and anatomy. Sci World J 2010;10:1174–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Li WP, Jiang H, Liu Y, et al. Electrophysiology research on the spinal nerve source of rabbit penis cutaneous sensation [in Chinese]. Zhonghua Nan Ke Xue 2007;13:312–4. [PubMed] [Google Scholar]
- [29].Lefaucheur JP, Yiou R, Salomon L, et al. Assessment of penile small nerve fiber damage after transurethral resection of the prostate by measurement of penile thermal sensation. J Urol 2000;164:1416–9. [PubMed] [Google Scholar]
- [30].Yarnitsky D, Sprecher E, Vardi Y. Penile thermal sensation. J Urol 1996;156:391–3. [DOI] [PubMed] [Google Scholar]
- [31].Johnson RD, Kitchell RL. Mechanoreceptor response to mechanical and thermal stimuli in the glans penis of the dog. J Neurophysiol 1987;57:1813–36. [DOI] [PubMed] [Google Scholar]
- [32].Zhang GX, Weng M, Wang MD, et al. Autologous dermal graft combined with a modified degloving procedure for penile augmentation in young adults: A preliminary study. Andrology 2016;4:927–31. [DOI] [PubMed] [Google Scholar]


