Supplemental Digital Content is available in the text.
Abstract
Background:
Many recent studies have evaluated the clinical safety and efficacy of therapeutic lasers in laser lipolysis, but without detailed description of the safe and effective parameters.
Purpose:
To propose a method for adjusting safe and effective parameters for laser lipolysis.
Methods:
Detailed calculations of the safe and effective laser parameters for fat melting are proposed in the study. Amount of energy delivered in joules was calculated based on data from Havenith research. External skin and internal tissues temperatures during the procedure were kept in a recommended range and monitored for safety and efficacy. Prospective statistical study was designed on a series of 300 patients who underwent laser-assisted lipolysis and /or liposuction using 2 different machine manufacturers, delivering 1,064/1,320 nm.
Results:
All areas submitted to laser-assisted liposuction in this series have resulted in no clinical thermal burns injury to the skin. There was improvement in the bulk of fats, skin tightening, skin textures, and cellulites.
Conclusion:
This study is proposing a simple method for calculations of safe and effective laser lipolysis. Skin burn injury could be highly prevented by following up the proposed detailed basic parameters for laser lipolysis treatment.
INTRODUCTION
Laser lipolysis and liposculpture techniques have produced significant updates to refine, address, and improve patients’ recovery and aesthetic results.1,2
Laser lipolysis and liposculpture have high success potential in difficult areas such as medial thighs, upper abdomen, arms and submental areas, as well as areas, which carry high risk of fibrosis, such as male breast gynecomastia, recurrent cases, and other cases who are presented by post suction skin irregularities.3,4
Laser-assisted liposculpture has been investigated many times in the literature, both clinically5 and objectively, through an magnetic resonance imaging6 measuring of a fatty layer thickness, skin retraction, and tightness using the “India ink tattoo and the histological studies.1 But there isn’t enough attention to the amount of safe and effective energy.
Selective photo-thermolysis is the mainstay theory for laser penetration, fat absorption, and fat melting using certain types of laser wave lengths.1,7,8 According to selective photo-thermolysis theory, the blend combinations of 2 different wave lengths, in new technologies are allowing us to get better fat melting and heat production for collagen denaturation and subsequent skin tightness.9,10
This may carry the risk of the increase of the tissue temperature9,10 and subsequent burn injuries at the treated areas.
This study is proposing a method to apply safe and effective energy parameters in laser lipolysis, with assessment of their efficacy and safety.
PATIENTS AND METHODS
In this prospective study, after consideration of safe and effective proposed parameters for laser lipolysis, the calculations have been applied to 300 cases. The cases were divided into 2 groups using 2 machines.
Each of the 150 cases were submitted using the same protocol for wave lengths, joules, delivery, power applied, technique of the procedure, but using 2 different manufacturers to note any clinical differences.
In 1 group, 150 patients were submitted for laser lipolysis by laser protocol for lipolysis by automated blending, delivered by the Smart Lipo triplex model system, 1,064 and 1,320 nm, US made (Cynosure).
The other 150 patients were submitted using the same parameters and wave lengths, but without the machine-automated blending mode. In these cases, the surgeon performed manual subsequent passes, using the DaVinci model, made in Italy, (Quanta).
Any objective evaluation of burn incidence during this study is based on size, degree, and depth of the burn injury. Burn size is assessed according rule of nine. Clinical degree of burn injury classification to epidermal, superficial partial thickness, deep partial thickness, and full thickness burn injury is assessed clinically by visual and tactile characteristic of burn, exactly; burn wound appearance, capillary refill, touch stability, pin prick for pain and bleeding, high resolution digital imaging, laser Doppler flow-meter, and punch biopsy then histology.
Proposed Helmy’s Method for Detailed Safe and Effective Calculations of Laser Energy Parameters
Steps
Each patient’s treatment area (s) are marked when standing, the boundaries of each treated area in length and width, are measured by a ruler and the depth (thickness) of the fat contents estimated with calipers.
The applied formula: Volume of the fat in targeted area = Length × Width × Thickness, while the thickness equal (1/2 of the caliper measurement). Second check, for the volume of targeted fatty area is confirmed by ultrasound assessment. The amount of required laser energy is calculated, based on the data from Havenith.11 Havenith’s formula is applying an individualized model of human thermoregulation for the simulation of heat stress response; the equation for the specific heat of body tissue (CB). Cb = (fat mass/body mass) × 2.51 + (body mass- fat mass)/body mass × 3.65.
Joules, Wattage Settings, and Flouncex
In total, 2.51 joules of laser energy is required to raise the subcutaneous temperature of 1 gram of fat 1°C.11 Since the physical fat density is 0.9 g/1 cc,12,13 therefore the required joules become 2.51 × 0.9 = 2.259 ~ 2.3/1 cc. For example, if a 11°C temperature rise is required from the body baseline of 37°C, then optimal dosage is reached at 48°C. Mathematical equation is performed as the following; Volume × 2.3 × 11°C (desired temperature rise). The product is expressed in total required joules for each treatment area.
Fat temperature is physiologically lower than the core body temperature,14 but the melting point of fat is less than other tissues. So when energy increases in doing fat melting, it could be less than the thermal point of the skin injury. So, energy could be increased until the limit is kept effective but safe.
Tissue heating did not exceed 41°C on external skin surface, and internal subcutaneous temperature ranges between 48 and 50°C, as this is above the required melting point of human fat.15 This safely allows energy to reach the melting point for the fat and the collagen denaturation without skin injuries. Surgeon can feel easy cannula movement throughout the melted fat. External skin and internal subcutaneous temperature are monitored.
The wattage settings were ranged from 8 to 12 W for the neck and up to 28 W for extremities, abdomen, and other areas. Irradiance or power density ranged from 8 to 28 W/cm2.
Flounce measured in average between 50 and 100 J/cm2. Duration of laser delivery procedure varies from one area to another and from one patient to another according to the fat volume that has been lipolyzed, and if it is a fibro-fatty nature or not, but on average, it ranged from 2 to 10 minutes.
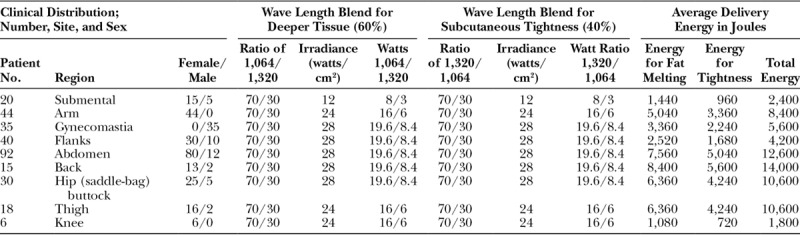
Laser lipolysis had been got by a blend mode, combination of 1,064/1,320 nm, wavelengths with more percentage for 1,064 nm. Fat removal is carried out by suction liposculpture, and then skin tightening achieved by blend mode also, with more percentage for 1,320 nm (Fig. 1).
Fig. 1.

Guide laser beams. Photograph shows the guide of laser beam subcutaneously.
The cumulative number of joules is calculated for each treated area then divided in a ratio of 60%/40%, where the 60% of energy was delivered to pass through a deeper fat planes aiming to a deep penetration and lipolysis using blend mode of 1,064/1,320 nm in ratio of 70/30% (smart lipo triplex model) or 70% of 1,064 and 30% of 1,320 nm (lipo laser Da Vinci model). The remaining 40% of total energy goes to the second pass, aiming to superficial tightening with 70%/30% 1,320/1,064 nm, which is vice versa to the previous deep planes passes (Table 1).
Table 1.
Data of the Study Including Wave Length Blend Ratio and Amount of Energy in Joules, Which Were Delivered for Each Treated Area
These parameters have been applied to different body areas including the belly, love handles, male breasts, arms, neck, thighs, and calves are involved. Aspiration of the treated fatty tissue revealed the fragmented cells, oily fat with residual tumescent fluid.
Full history, physical examinations, and routine investigations were performed for patients. All were seeking reduction of excess fat masses, and improvement of the skin elasticity in specific areas.
Patient follow-up, for pain, hyperemia, edema, seroma, ecchymosis, incidence rate of burns, and aesthetic outcomes are recorded at 1 week, 4 weeks, 3 months, 6 months, and 1 year (Figs. 2–7).
Fig. 2.
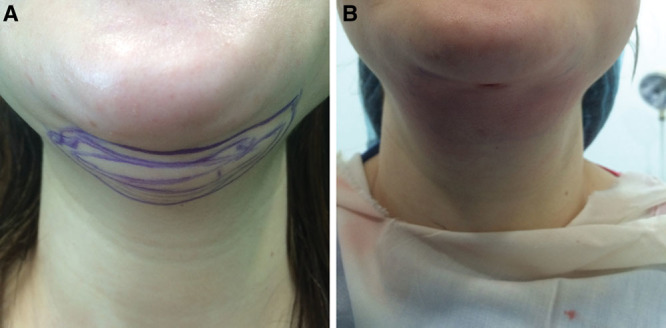
A, Pre-laser lipolysis. B, Immediate post-laser lipolysis and suction for submental area.
Fig. 7.
A case of abdominal laser liposuction. A, Preoperative. B, Fifteen days postoperative with some bruises.
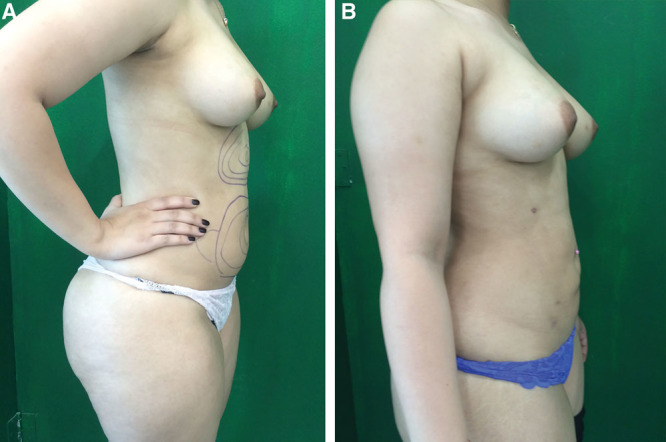
Fig. 3.

A case of abdominal and thighs laser liposuction. A, Preoperative front view. B, Six months’ postoperative front view. C, Preoperative lateral view. D, Six months’ postoperative results, after laser liposuction for the abdomen and lateral thighs with an improvement of the cellulites.
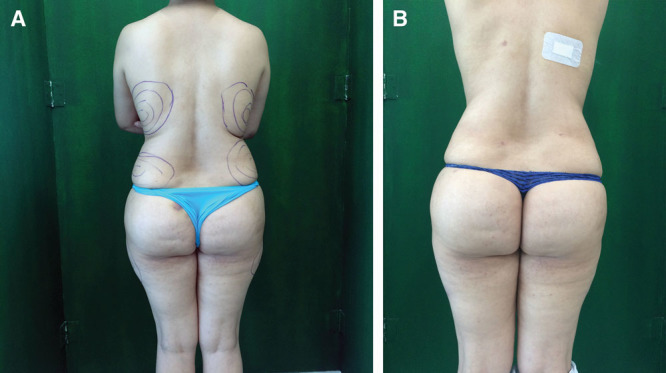
Fig. 4.
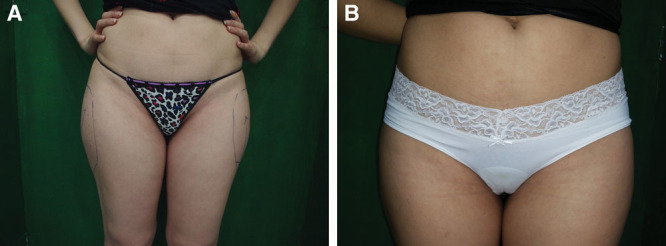
A case of Trochanteric laser liposuction. A, Preoperative. B, One-year postoperative laser liposuction for the abdomen.
Fig. 5.
A case of back laser liposuction. A, Preoperative. B, Fifteen days postoperative laser liposuction for the back.
The study was conducted between August 2013 and September 2017. Each patient submitted a signed informed written consent for both the study and photographs. The ethical committee of my institution has approved the study.
RESULTS
The joules calculated according to this method were effective and safe to get fat melting and skin tightening in each case. The lower effective limit or the initial laser dosage is the calculated energy, and the upper limit is the amount of laser energy which is delivered when the monitored subcutaneous and skin temperatures are 48–50°C and 41°C, respectively. No clinical differences were recorded regarding thermal safety, efficacy, or aesthetic outcome for both machines, used in the study (see figure, Supplemental Digital Content 1, which displays the machines which were used in the study, http://links.lww.com/PRSGO/A873).
Age of patients is ranged from 18 to 48 years old with an average age of 35 years. Two hundred twenty-nine patients were female, whereas 71 were male. All patients were in body mass index range from 25 to 35.
In the study, and based on the above calculations, the average cumulative energies were required for each treated area depending on location, and the volume of targeted fat mass. They were in average total joules as the following: 2,000–2,500 J for the chin, 8,000–12,000 J for the arm, 5,000–6,000 J for male gynecomastia in each side, 4,000–5,000 J for flanks (love handles), 10,000–14,000 J for abdomen, 12,000–18,000 J for the back, 8,000–15,000 J for saddle bags, 10,000–14,000 J for the thigh and 800–2,000 J for the knee (see video, Supplemental Digital Content 2, which displays the delivery of Laser Joules of Nd-Yag 1,064 nm, into the right flank area, for thermal lipolysis, http://links.lww.com/PRSGO/A874).
Video Graphic 1.

See video, Supplemental Digital Content 2, which displays the delivery of Laser Joules of Nd-Yag 1,064 nm, into the right flank area, for thermal lipolysis, http://links.lww.com/PRSGO/A874.
There was clinical improvement in the bulk of fat, skin tightening; skin textures and cellulites during follow-up. Each treated area had decreased in width, length, and depth estimated by ruler, calipers, and ultrasound. Although there were some postoperative irregularities in Figure 6, as the patient had complained of lipo-dystrophy in lower legs with subsequent preoperative impaired lymphatic system, she has noticeably improved post laser treatment.
Fig. 6.
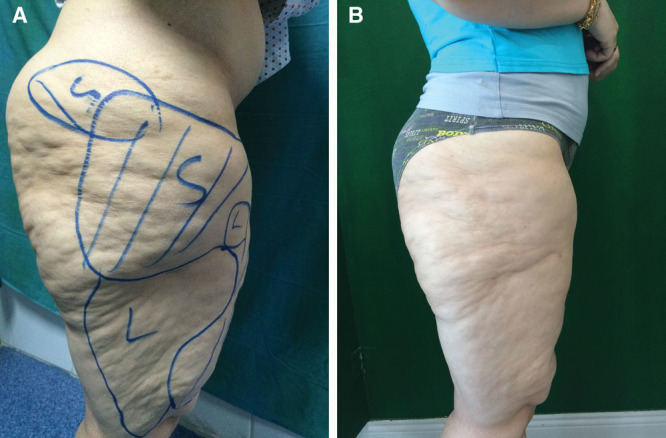
A case of thighs laser liposuction: Local lipodystrophy with impaired lymphatic drainage: A, Preoperative. B, At 6 months of laser liposuction for the front and lateral sides of the thighs and above knee area. Areas marked by L mean that they were submitted only to laser lipolysis, whereas areas marked with S mean they were submitted to laser lipolysis then liposuction.
Each patient’s treatment area (s) are marked when standing; the boundaries of each treated area in length and width are measured by a ruler and the depth (thickness) of the fat contents estimated with calipers. Second check, for the volume of removed fat, is confirmed by ultrasound assessment.
Skin tightness was assessed by 2 points skin marking, using temporary tattoo needling, which is lasting for 1 month only, then repeated for another month. Skin textures and cellulites are judged by surgeon’s inspection and palpation.
Incidence rate for burn liposuction or laser Sculpture in this series is zero percentage.
Burn ratio to the number of patient in the study is found 0/300 (0%). All areas submitted to laser lipolysis do not have any infection or hyperpigmentation, although 10% of the study complained of discomfort and pain for couple of hours after some local procedures or after the recovery from anesthesia.
All patients had completely improved within 24 hours. In fact, 6 of the 300 patients (approximately 2% of the study) developed hyperemia for 48 hours postoperative. Furthermore, 30 patients (approximately 10% of the study) had developed postoperative bruises, which were improved by the 10th day of the procedure. The longevity and efficacy of treatment were recorded all over the follow-up period.
DISCUSSION
The safety of laser lipolysis is discussed generally in literatures; this marked my attention for accurate calculations of safe and effective joules. The technique is considered less invasive, safer, and effective13 than ordinary liposuction,16 and carried better aesthetic outcomes, but literatures are reporting evidence of some adverse effects17,18,19 without any details about the dangerous amount of laser energy.
There are dermatological complications for laser.20 So, laser safety is a priority before efficacy when providing health services. The author’s goal was to propose safe and effective parameters through this innovative method, which is not available in any of the machine manufacturer’s methods.
There is no detailed parameter description in literature, so the study has designed the calculations upon physics and tissue physiology interpretation, and then applied these parameters in a series. This study didn’t record any immediate, early burns or any delayed tissue fibrosis or loss of skin integrity.
We have to avoid the thermal point for burn injury, so it is better to calculate, to deliver the minimum, but effective energy for melting of the fats. Melting of fat differs from one patient to another and from an area to another.15 Uncalculated energy may be more than required, and in case, the tissue may be more vulnerable to burns, edema, impaired healing, and even postoperative fibrosis and less satisfactory outcome.
Katz and McBean21 in 2008 presented their results of 537 laser lipolysis procedures, without any adverse systemic effects but they reported 4 cases of superficial burn injuries and 1 case developed local infection. The corresponding rate of those adverse effects was 0.93%. Yu et al.,22 in 2009, reported a case of burn injury after laser lipolysis, while using diode laser for blepharoplasty, but both studies did not give accurate explanation for the cause of burn injury and its relation to the amount/area.
One of the frequent doctors’ comments about laser liposuction is possible adverse burn injury. During the laser lipolysis, the internal temperature ranges mostly between 48°C and 50°C, and it is really a narrow range. That range in which laser interact with fat and collagen deserves attention, because excess energy in the treated area will result in burns especially in thin dermis’ areas.
So, this clinical study is designed to evaluate the possible thermal injury in wide scale of patients, 300 of whom were submitted for laser lipolysis. Study takes into consideration the laser tissue interaction accurate physics, thermos-regularity principles, and tissue heat stress response. This study provides a proposed method for the calculation of actual required joules for each treated area, which allows for good fat melting and skin tightness safely.
Kim et al.23 in 2012 have reported 3 cases of burn injuries after axillary laser treatment of 29 patients. One explanation in their study was the high level of accumulated energy used by the authors (up to 500 J/2 cm2), and this comes with our observation that concludes that actual calculation for the total energy required is safer to avoid thermal or burn injuries.
Clinical results came from Reynaud et al.24 in 2009 when they evaluated 534 cases and they did not report any cases of burns, infections, hematomas, edemas, or hyperpigmentation.
In the study by Reynaud et al.,24 a week later, 83% of patients did not report pain or discomfort, whereas in my study pain and discomfort were totally improving within 24 hours’ postoperative and 10% of patients in my study developed bruises, but they were improved by the 10th day of the procedure. This may be attributed to better safety due to accurate joules and power estimation per treated areas.
In this study, significant skin smoothening and tightness by N-D YAG laser have been achieved, as well as, results of the study on Diode laser lipolysis came out.25,26 Laser lipolysis is still safely competing with Ultrasound lipolysis in the evolution and refinement even in gynecomastia management.27
CONCLUSIONS
This study is proposing a method for calculations of safe and effective laser energy in lipolysis. Procedure monitoring and calculations of the delivered amount of energy result in safe and effective treatment. The lower effective limit or the initial laser dosage is the calculated energy, and the upper limit is the monitored subcutaneous and skin temperatures, 48–50°C and 41°C, respectively.
Supplementary Material
Footnotes
Published online 3 October 2018.
Disclosure: The author has no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the author.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.McBean JC, Katz BE. Laser lipolysis. An update. J Clin Aesthet Dermatol. 2011;4:25. [PMC free article] [PubMed] [Google Scholar]
- 2.Goldman A. Submental Nd:Yag laser-assisted liposuction. Lasers Surg Med. 2006;38:181. [DOI] [PubMed] [Google Scholar]
- 3.Wells JH, Hurvitz KA. An evidence-based approach to liposuction. Plast Reconstr Surg. 2011;127:949. [DOI] [PubMed] [Google Scholar]
- 4.Agullo FJ, Palladino H, Sozer SO. Serdev NIkolay. Complications of liposuction, advanced techniques in liposuction and fat transfer. Available at http://www.intechopen.com/books/advanced-techniques-in-liposuction-andhttp://www.intechopen.com/books/advanced-techniques-in-liposuction-and-fattransfer/fattransfer/ complications-of-liposuction. Accessed at 15 May 2017 [Google Scholar]
- 5.Massoud K, Hussein H, Aboul fotouh S, et al. Evaluation of blood-loss in laser-assisted liposuction. Egypt J Plast Reconstr Surg. 2008;32:237. [Google Scholar]
- 6.Kim KH, Geronemus RG. Laser lipolysis using a novel 1,064 nm Nd:YAG Laser. Dermatol Surg. 2006;32:241. [PubMed] [Google Scholar]
- 7.McBean JC, Katz BE. A pilot study of the efficacy of a 1,064 and 1,320 nm sequentially firing Nd:YAG laser device for lipolysis and skin tightening. Lasers Surg Med. 2009;41:779. [DOI] [PubMed] [Google Scholar]
- 8.Lukac M, Vizintin Z, Zabkar J, et al. QCW pulsed Nd: YAG 1064 nm laser lipolysis. J Laser Health Acad. 2009;4 Avilable at: https://www.researchgate.net/publication/263920469_QCW_Pulsed_NdYAG_1064_nm_Laser_Lipolysis. Accessed: August 2018 [Google Scholar]
- 9.Dudelzak J, Hussain M, Goldberg DJ. Laser lipolysis of the arm, with and without suction aspiration: clinical and histologic changes. J Cosmet Laser Ther. 2009;11:70. [DOI] [PubMed] [Google Scholar]
- 10.DiBernardo BE, Reyes J, Chen B. Evaluation of tissue thermal effects from 1064/1320-nm laser-assisted lipolysis and its clinical implications. J Cosmet Laser Ther. 2009;11:62. [DOI] [PubMed] [Google Scholar]
- 11.Havenith G. Individualized model of human thermoregulation for the simulation of heat stress response. J Appl Physiol (1985). 2001;90:1943. [DOI] [PubMed] [Google Scholar]
- 12.Atashroo DA, Paik KJ, Michael T, et al. Assessment of viability of human fat injection into nude mice with micro-computed tomography. J Vis Exp. 2015 (95):52217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Neves EB. A C Chierighini and Rafael Melode Oliveirab et al. Effect of body fat and gender on body temperature distribution. J Thermal Biol. 2017;70:1. [DOI] [PubMed] [Google Scholar]
- 14.Heikens MJ, Gorbach AM, Eden HS. Core body temperature in obesity. Am J Clin Nutr. 2011;93:963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.NUT SCHMIDT-NIELSEN. Melting points of human fats as related to their location in the body. Act PHYSIOLOGICA. 1946;12. [Google Scholar]
- 16.Shelton RM, Rokhsar CK.Tumescent liposuction. Available at emedicine.medscape.com. 2016; Article 138: updated: Nov 09. Accessed at 15 May 2017.
- 17.Neda Va, Niloofar Y, Manijeh Z, et al. Evaluation of safety and efficacy of 980 nm diode laser-assisted lipolysis versus traditional liposuction for submental rejuvenation: a randomized clinical trial. J Cosmet Laser Ther. 2015;18:41. Available at http://www.tandfonline.com/doi/full/10.3109/14764172.2015.1039041. Accessed at 10 April 2017 [DOI] [PubMed] [Google Scholar]
- 18.Badin AZ, Moraes LM, Gondek L, et al. Laser lipolysis: flaccidity under control. Aesthetic Plast Surg. 2002;26:335. [DOI] [PubMed] [Google Scholar]
- 19.Ahmad J, Eaves FF, 3rd, Rohrich RJ, et al. The American Society for Aesthetic Plastic Surgery (ASAPS) survey: current trends in liposuction. Aesthet Surg J. 2011;31:214. [DOI] [PubMed] [Google Scholar]
- 20.Al-Niaimi F. Laser and energy-based devices’ complications in dermatology. J Cosmet Laser Ther. 2016;18:25. [DOI] [PubMed] [Google Scholar]
- 21.Katz B, McBean J. Laser-assisted lipolysis: a report on complications. J Cosmet Laser Ther. 2008;10:231. [DOI] [PubMed] [Google Scholar]
- 22.Yu D, Biesman B, Khan JA. Bilateral eyelid dermal burn from subcutaneous diode laser lipolysis blepharoplasty. Lasers Surg Med. 2009;41:609. [DOI] [PubMed] [Google Scholar]
- 23.Kim D, Kim J, Yeo H, et al. Treatment of axillary osmidrosis using a subcutaneous pulsed Nd-YAG laser. Arch Plast Surg. 2012;39:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reynaud JP, Skibinski M, Wassmer B, et al. Lipolysis using a 980-nm diode laser: a retrospective analysis of 534 procedures. Aesthetic Plast Surg. 2009;33:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marc J.Salzman, Laser-Assisted Lipolysis Using ProLipo PLUS. 2009. Available at https://sciton.com/wp-content/uploads/2017/02/2600-003-01rC-PLPLUS-WP.pdf. Accessed at 15 May 2017.
- 26.Ferreira LM, Wolfenson, Moisés, et al. Laser lipolysis: skin tightening in lipoplasty using a diode laser. Plast Reconstr Surg. 2015;135:1369. [DOI] [PubMed] [Google Scholar]
- 27.Rohrich RJ, Steven H, Guenther D, et al. Gynecomastia management: an evolution and refinement in technique at UT Southwestern Medical Center. Plast Reconstr Surg. 2016;4:e734. [DOI] [PMC free article] [PubMed] [Google Scholar]


