Abstract
Endoscopic thyroidectomy (ET) via an axillo-breast (ABA), axillary or breast approach (BA) is effective for treatment of unilateral papillary thyroid microcarcinoma (PTMC). However, several disadvantages still exist, including inconvenience for using endoscopic instruments and poor cosmetic results. Here, we introduced a modified ABA (MABA) to overcome these disadvantages and evaluated its therapeutic outcomes by comparison with conventional BA.
Fifty-five patients undergoing ET via MABA (n = 22) or BA (n = 33) for PTMC were retrospectively enrolled between June 2012 and June 2015. Surgical outcomes, including the operation time, blood loss, amount of drainage, number of dissected lymph nodes, complications, cosmetic satisfaction and prognosis (recurrence and survival), were analyzed.
The operation time (87.1 ± 9.3 min vs 93.2 ± 8.3 min; P = .014) and drainage tube removal time (4.4 ± 1.0 days vs 5.1 ± 1.1 days; P = .018) were shorter in the MABA group than those in the BA group. There was less postoperative drainage (54.3 ± 35.7 mL vs 137.6 ± 87.0 mL; P < .01) in the MABA group compared with the BA group. No significant differences in the blood loss (15.9 ± 7.5 mL vs 19.2 ± 11.7 mL, P = .243) and the number of dissected lymph nodes (1.8 ± 1.5 vs 2.3 ± 2.1, P = .309) were observed between the 2 groups. Subcutaneous ecchymosis occurred more frequently in the BA group than that in the MABA group (33.3% vs 9.1%; P = .038). Patients treated by MABA were more satisfied with their cosmetic results than those undergoing BA (100% vs 81.8%; P = .034). At the last follow-up time, all patients were alive although 1 patient in the BA group developed cervical lymph node recurrence ipsilateral to the original tumor at 4 years after surgery. Multivariate logistic regression analysis showed MABA surgery was a protective factor for postoperative complications (OR = 0.209, 95% confidence interval [CI] = 0.054–0.817, P = .024).
ET via the MABA strategy may be a good choice for unilateral PTMC because of shorter operation time, fewer complications, greater cosmetic satisfaction, and excellent prognosis.
Keywords: complications, cosmetic satisfaction, endoscopic thyroidectomy, modified axillo-breast approach, papillary thyroid carcinoma
1. Introduction
Thyroid cancer (TC) is the most common endocrine malignancy, with an estimated 64,300 new cases and 1980 deaths in 2016.[1] Greater than 90% of TCs are well differentiated, among which papillary thyroid cancer (PTC) is the most prevalent type.[2] With the advancements in ultrasonography and fine-needle aspiration biopsy, the detection rate of PTC, particular small PTC (<1 cm; also known as papillary thyroid microcarcinoma, PTMC), is increased remarkably, with a predicted incidence rate up to 26.9 per 100,000 person-years for Asian/ Pacific Islanders by 2019.[3] Thus, how to manage PTMC is a main problem faced by the surgeons.
Currently, there continues to be controversial with regard to the optimal treatment for PTMC, especially unilateral PTMC, a common clinical phenomenon. According to the extent of resection, the surgical approaches can be divided into total thyroidectomy (TT), hemithyroidectomy (HT), or thyroid lobectomy (TL). A retrospective study of Hirsch et al indicated that the HT provided no clear benefit compared with TT, leading to a high suspected recurrent/persistent disease.[4] Also, Macedo et al used the meta-analysis to demonstrate that TT was associated with lower recurrence and mortality rates compared with TL.[5] These findings suggest TT may be the most effective for PTMC. However, a recent study considered that completion thyroidectomy was not mandatory for the low-risk patients and even, the morbidity rates of transient nerve palsy and hypoparathyroidism were significantly lower in TL than TT.[6] Yu et al also recommended the completion lobectomy, including the ipsilateral residual lobe, central lymph nodes (compartment VI) and the isthmus, with no mortality recorded after a follow up of 18 to 66 months.[7] Accordingly, completion lobectomy may be reasonable for the low-risk patients, which was also performed in our clinic.
In addition, unilateral PTMC occurs more frequently in young women[8] in whom the oncologic safety and excellent cosmetic results are strongly demanded simultaneously. Therefore, the endoscopic thyroidectomy (ET) is introduced and several studies have demonstrated that postoperative cosmesis after ET is significantly better than conventional open thyroidectomy, but surgical outcomes are similar between them.[9–11] Recently, various endoscopic operative methods have been developed by the surgeons, including a cervical approach,[12] anterior chest wall approach,[13] axillo-breast approach (ABA),[10,14,15] axillary[16–18] or breast approach (BA).[19,20] Among them, cervical and anterior chest wall approaches are commonly excluded because of the visible scar in a natural position. The incision in the breast is also not accepted for some patients.[19,20] Although the cosmetic results are excellent after the axillary approach because the small scars left in the axilla can be covered by the patient's arm, it is inconvenient to use the endoscopic and surgical instruments due to the narrow area of the axilla, which leads to longer operation time required and underlying oncologic unsafety.[16–18] ABA is performed by 1 large incision in the axilla (approximately 5 cm) and another small 1 in the areola (0.5 cm), both of which minimize the visible scar. Nevertheless, similar to the axillary approach, the endoscopic lens and operating arm are needed to be inserted into the large incision in the axilla, resulting in their inevitable collision and influencing the surgical handling.[21] To overcome these disadvantages, we introduced a modified axillo-breast approach (MABA) in which 3 small incisions at the ipsilateral axilla (0.5 cm), areola (0.5 cm), and the location between them (1 cm) were made and the endoscopic lens was alone placed in the small incision between the ipsilateral axilla and areola. We believe the cosmetic results and safety could be further improved by our approach.
The goal of this study was to retrospectively evaluate the treatment outcomes of ET via our MABA to completely resect the ipsilateral lobe, central lymph nodes, and the isthmus for patients with unilateral PTMC by comparison with conventional BA.[19,20]
2. Materials and methods
2.1. Patients
Patients with PTMC who underwent ET via MABA or BA in the Department of Head and Neck Surgery of Zhejiang Cancer Hospital between June 2012 and June 2015 were retrospectively enrolled. The inclusion criteria were set as follows:
-
1)
diagnosed with PTC by fine needle aspiration;
-
2)
age between 15 and 50 years old;
-
3)
no history of neck surgery or radiotherapy;
-
4)
unilateral solitary nodule and tumor size <1 cm on preoperative ultrasonography;
-
5)
no evidence of lymph node metastasis or local invasion on preoperative ultrasonography and computed tomography; and
-
6)
ET was chosen as the preferred surgical treatment due to concern with the cosmetic appearance of the neck.
Patients were excluded if they:
-
1)
having a history of neck surgery or radiotherapy;
-
2)
their thyroidal function tests indicating the presence of Hashimoto's thyroiditis or hyperthyroidism preoperatively;
-
3)
possessing thyroid nodules ≥1 in size;
-
4)
requiring a surgery for removal of bilateral thyroid nodules; and
-
5)
incapable of cooperating or receiving the ET surgery.
All patients signed an informed consent form for the surgery and the use of outcome data. This study was approved by ethics committee of our institution (approval code: ZJZLYY-2014–05–56) and performed in accordance with the ethical standards.
2.2. Surgical procedures
All procedures were performed by the same surgeon. All patients underwent general endotracheal anesthesia and were placed in a supine position. The neck was slightly extended, and the lesion-side arm was raised to expose the axillary fossa.
In the MABA treatment group, 3 incisions were separately made at the ipsilateral axilla (0.5 cm), areola (0.5 cm), and the location between them (1 cm) (Fig. 1). Inflation liquid (200–350 mL, consisting of 1 mg adrenaline and 10 mL lidocaine mixed with 500 mL saline) was injected into the subcutaneous layer of the anterior chest and cervical skin to reduce the bleeding events. Skin flap was separated along the deep layer of the superficial fascia till the opposite side of the anterior cervical muscle, the lateral margin of sternocleidomastoid, the level of thyroid cartilage and 4 to 6 cm below the clavicle. The medial border of sternocleidomastoid was dissected from the anterior cervical muscle. The lateral margin of the anterior cervical muscle was separated followed the direction of the muscle fibers, and the thyroid was exposed (Fig. 2). The superior thyroid vessels were resected close to the thyroid to avoid injuring the superior laryngeal nerve. The recurrent laryngeal nerve (RLN) was exposed by blunt dissection. The inferior thyroid vessels were resected carefully to avoid injuring the RLN. The superior and inferior parathyroid gland were identified and left intact (Fig. 3). The lobe was dissected from the trachea, and the isthmus was excised. The resected specimens were sent for frozen pathology; if confirmed to be PTC, ipsilateral central lymph node dissection was performed routinely. A negative pressure drainage was placed to the wound at the areola through a special sealed dressing and incisions were closed with 2/0 absorbable sutures in a layered fashion.
Figure 1.

Modified axillo-breast approach. Three incisions were made and trocars were inserted.
Figure 2.
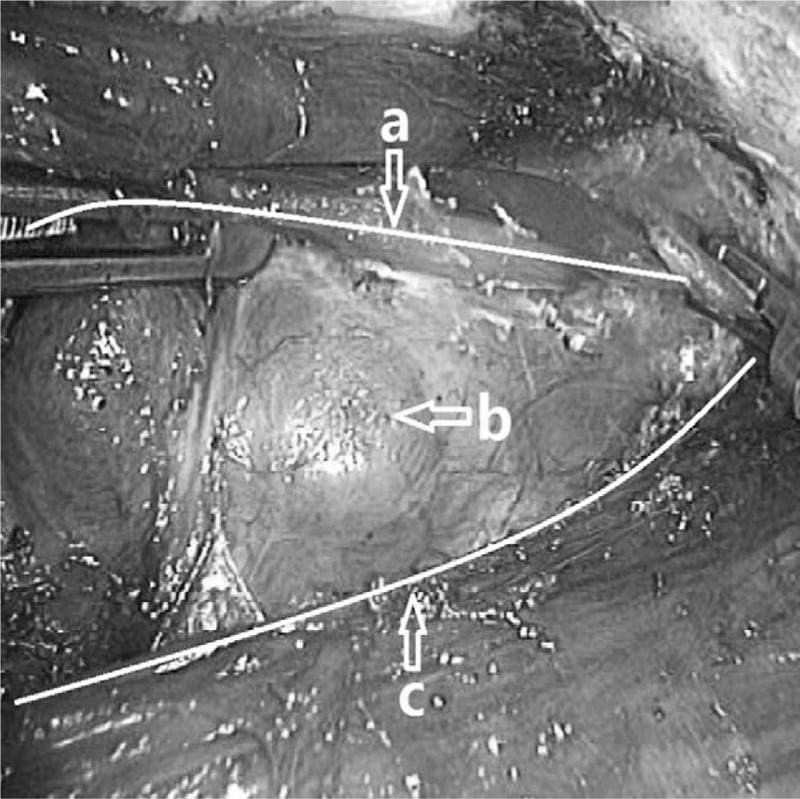
Thyroid exposure via modified axillo-breast approach. a: lateral margin of anterior cervical muscle; b: thyroid; c: medial border of sternocleidomastoid.
Figure 3.
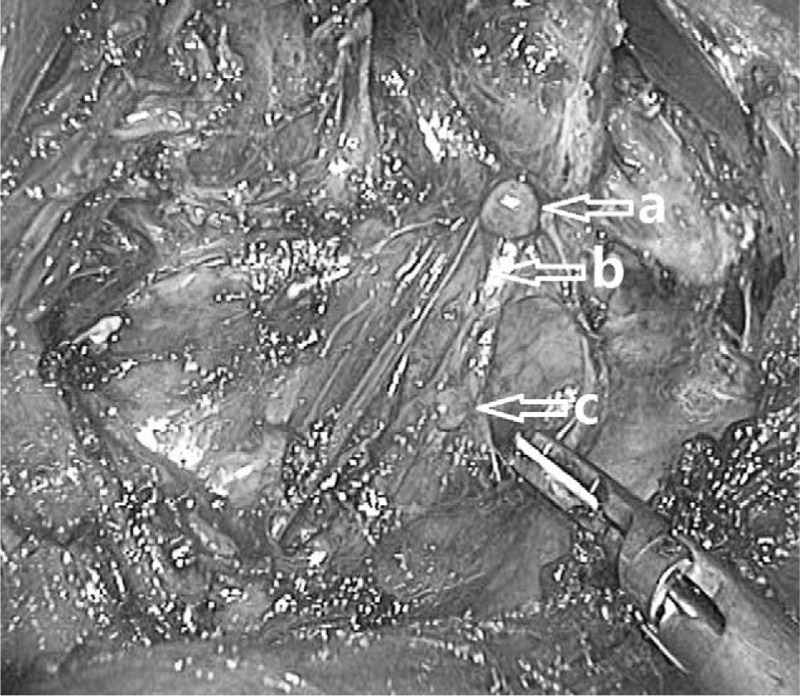
The recurrent laryngeal nerve exposed by blunt dissection. The superior and inferior parathyroid gland were identified and left intact. a: superior parathyroid gland; b: recurrent laryngeal nerve; c: inferior parathyroid gland.
In the BA treatment group, three skin incisions were separately made at the bilateral areola (0.5 cm) and the location 2 cm outside of the sternum at the level of the nipple (1 cm).[19,20] Inflation liquid (200–350 mL) was also injected into the subcutaneous layer of the anterior chest and cervical skin. Skin flap was separated through the incision, resulting in fanning out from the deep layer of the superficial fascia toward the suprasternal notch. Cervical linea alba was dissected and the anterior cervical muscle was separated by the ultrasonic scalpel. Thyroid was exposed. The remaining steps were the same as those in the MABA approach.
2.3. Evaluation of therapeutic efficiency
The operative data between 2 groups were recorded and analyzed, including the operation time (min), intraoperative blood loss (mL), the number of dissected lymph nodes, amount of postoperative drainage (mL), time of removing drainage tube (days), postoperative complication (such as transient or permanent RLN palsy, vocal cord palsy, hypocalcemia, tracheal fistula, subcutaneous ecchymosis, subcutaneous emphysema, bleeding, infection, and swallowing discomfort), and patients’ satisfaction. The operative time was recorded from the first skin incision to the last suture. Intraoperative blood loss was estimated from suction volumes. Ultrasonography was performed to examine the postoperative residual thyroid 1 month after surgery. Vocal cord movement was examined with laryngoscopy before and after surgery. Patients’ satisfaction with the cosmetic results and scar symptoms were divided into 3 ratings: satisfied, acceptable, and unsatisfied. In addition, the prognosis information (including recurrence and survival) was also collected during the follow-up.
2.4. Statistical analysis
All statistical analyses were performed by using the SPSS software (version 22.0, Chicago, IL). Continuous variables were expressed as mean ± standard deviation (SD) and analyzed using the independent t test, while categorical variables were presented as number (percentages) and compared using chi-square (or Fisher exact) tests. Multivariate logistic regression model was used to filter risk factors for the postoperative complications. P < .05 was considered to be statistically significant.
3. Results
3.1. Clinicopathologic characteristics of patients
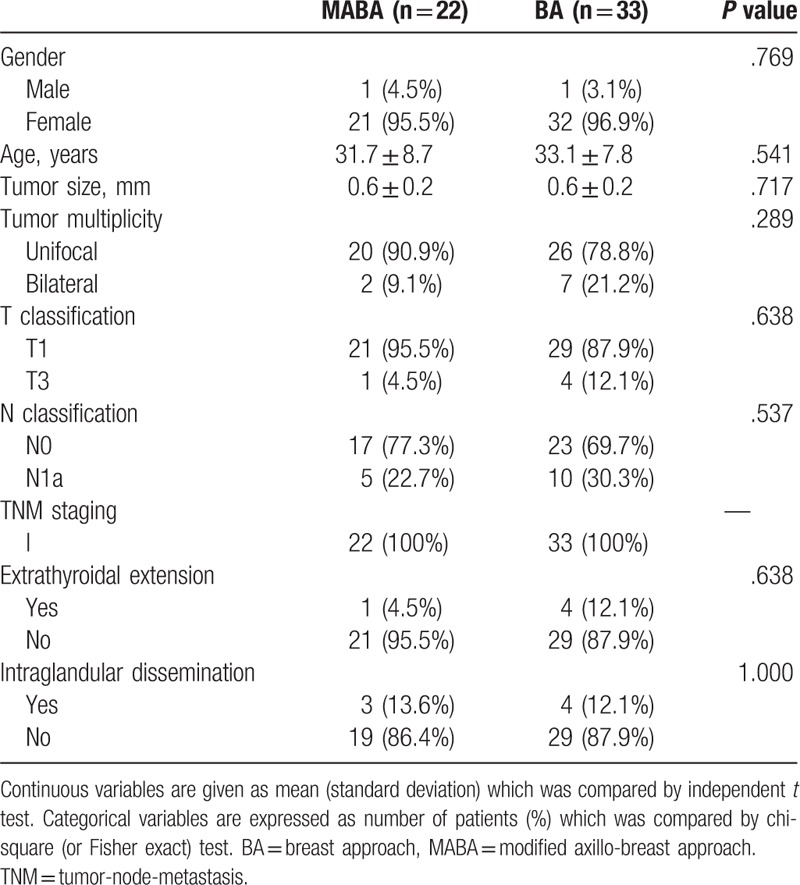
Fifty-five patients were enrolled according to the inclusion and exclusion criteria. Of them, 22 patients underwent unilateral MABA and 33 received BA surgery with prophylactic ipsilateral central node dissection. The clinicopathologic characteristics of these 55 patients are summarized in Table 1. The mean age of the patients was 33.1 ± 7.8 years in the MABA group and 31.7 ± 8.7 years in the BA group (P = .541). The male-to-female gender ratios were 1:21 in the MABA group and 1: 32 in the BA group, which was not statistically different (P = .769). There were also no significant differences in the tumor size, multiplicity, T classification, N classification, TNM staging, extrathyroidal extension and intraglandular dissemination between the 2 groups (P > .05; Table 1), indicating the comparability of them.
Table 1.
Clinicopathologic characteristics of the patients in 2 groups.
3.2. Assessment of surgical efficiency
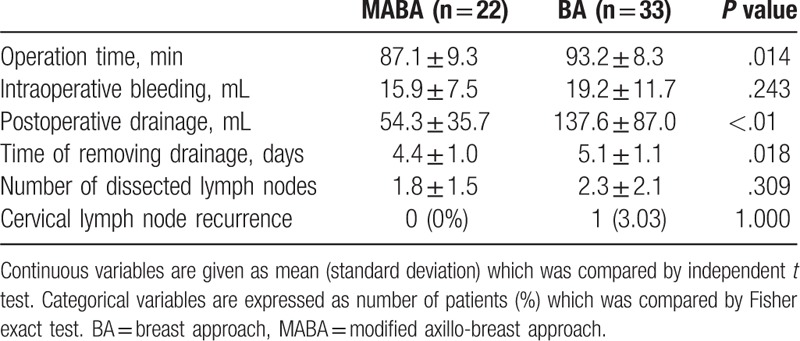
The ET was successfully performed in all patients, with no case of conversion to the open surgery. To assess the operational advantages of ET via MABA, the operation time, intraoperative blood loss, postoperative drainage, time of removing drainage, and the number of dissected lymph nodes were compared with the control BA group. As expected, the total operation time (87.1 ± 9.3 min vs 93.2 ± 8.3 min, P = .014) and the time of removing drainage tube (4.4 ± 1.0 days vs 5.1 ± 1.1 days, P = .018) in the MABA group were significantly shorter than those of the BA group. There was less amount of postoperative drainage collected in the MABA group than that of the BA group (54.3 ± 35.7 mL vs 137.6 ± 87.0 mL, P < .01). However, no statistically significant differences in the mean volume of intraoperative bleeding (15.9 ± 7.5 mL vs 19.2 ± 11.7 mL, P = .243) and the number of retrieved lymph nodes (1.8 ± 1.5 vs 2.3 ± 2.1, P = .309) were observed between the 2 groups (Table 2). Also, no obvious residual thyroid was detected in both groups by ultrasonography 1 month after surgery. Until to the follow-up time point of July 2018, all patients in 2 groups were found to be still alive although 1 patient (T3N1aM0; tumor size = 0.9 cm) in the BA group developed cervical lymph node recurrence (area III, 1; area IV, 2) ipsilateral to the original tumor (left) at 4 years after surgery which was resolved by further lymph node dissection via open surgery (Table 2).
Table 2.
Comparison of surgical outcomes of the patients in 2 groups.
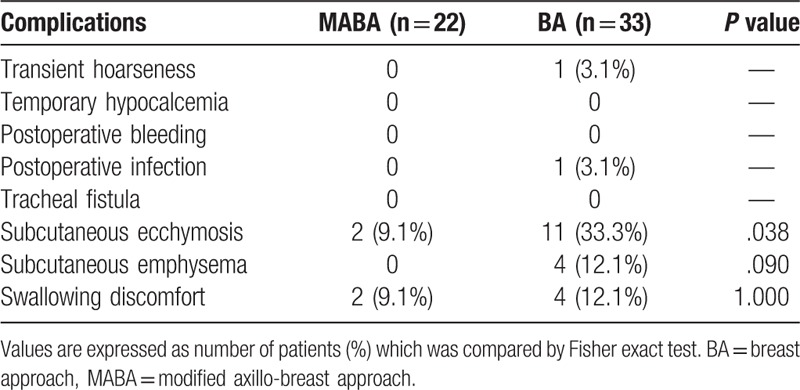
3.3. Assessment of surgical safety
The higher safety of the MABA method than the BA group was assessed by recording their complications (Table 3). As a result, transient RLN palsy occurred in 1 patient of the BA group, with the manifestation of transient hoarseness. This symptom was spontaneously recovered within 2 months without any treatment. No permanent RLN and vocal cord palsy were present in any patients of the 2 groups. One patient in the BA group suffered from postoperative infection which was resolved by anti-inflammatory therapies for 1 week. There was no hypocalcemia, tracheal fistula and postoperative bleeding in both groups. Subcutaneous ecchymosis (11/33, 33.3% vs 2/22, 9.1%; P = .038) and emphysema (4/33, 12.1% vs 0/22, 0%; P = .09) occurred more frequently in the BA group than those in the MABA group. Two and 4 patients complained of swallowing discomfort in the MABA and BA groups, respectively (Table 3). After 6 months, these complaints resolved spontaneously.
Table 3.
Comparison of postoperative complications of the patients in 2 groups.
3.4. Assessment of surgical satisfaction
Cosmetic satisfaction was another important concern for young women, which was rated by directly asking the patients in our study (Table 4). The results showed that all of the patients in the MABA group (Fig. 4) and 27 patients (81.8%) in the BA group were satisfied with the cosmetic results, which was statistically different (P = .034). Because of subcutaneous ecchymosis and postoperative paresthesia, 6 patients (18.2%) in the BA group evaluated satisfaction ratings as “acceptable”. No 1 was unsatisfied with the cosmetic results and scar symptoms in both groups.
Table 4.
Satisfaction ratings of the patients in 2 groups.
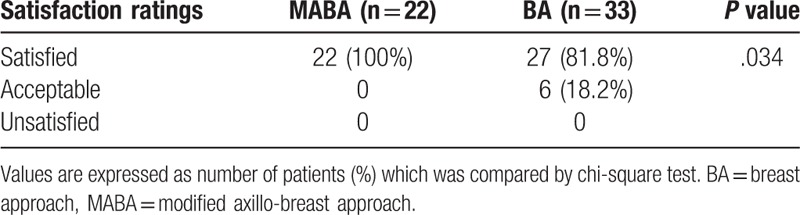
Figure 4.

Representative photographs showing the cosmetic results after the modified axillo-breast surgery.
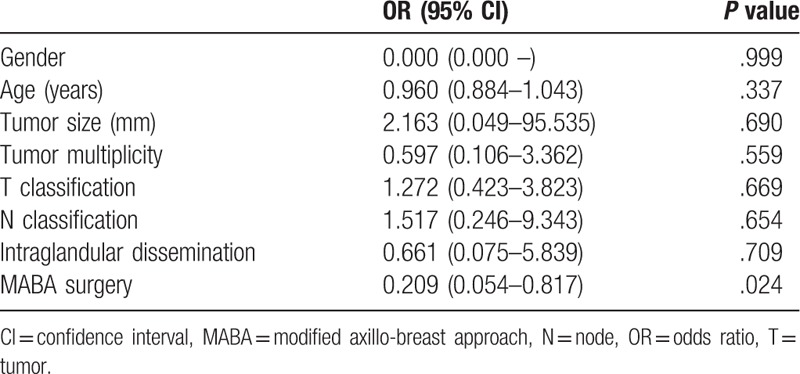
3.5. Risk factors for postoperative complications
Due to the fact that few (or no) patients developed recurrence and death, logistic regression analysis for recurrence and survival could not be performed. Multivariate logistic regression analysis was only carried out for postoperative complications and patients’ satisfaction. The results showed MABA surgery method may be a protective factor for postoperative complications with the OR (odds ratio) of 0.209 (P = .024) and the 95% CI (confidence interval) of 0.054 to 0.817 (Table 5). The multivariate analysis results for patients’ satisfaction are not shown because of the absence of the lower or upper limit for 95% CI in several variables, which may be unbelievable.
Table 5.
Multivariate logistic regression analysis of postoperative complications.
4. Discussion
In this study, we, for the first time, introduced a MABA for treatment of PTMC. Compared with conventional ABA, there were 2 modifications in our approach: 3 small skin incisions were made at the ipsilateral axilla, areola, and the location between them, not 1 large incision in the axilla and another small in the areola as described in the introduction,[21] which may prevent the inconvenience for the surgical handling; the thyroid was exposed by dissecting the medial border of the sternocleidomastoid muscle from the strap muscle, not separating the skin flap till the suprasternal notch and dissecting the cervical linea alba similar to the BA method.[22–24] These modifications made the operation simple and thus may shorten the operation time and reduce the risk of potential surgical complications and poor prognosis. As expected, the results showed that our new approach exhibited shorter operation time (87.1 ± 9.3 min vs 154 ± 64.88 min,[14] 192.4 ± 56.6 min,[15] 121.65 ± 20.78)[25] and better prognosis (recurrence: 0% vs 1.7%[10] or 1.5%)[26] compared with the known ABA. However, a slightly higher occurrence rate of subcutaneous ecchymosis was observed by comparing with the study of Xia et al[27] (9.1% vs 8.3%), which may be resulted from the unskilled operation for this new operative approach. The operation time and complications may be further shortened or reduced when we overcome the learning curve of MABA. Furthermore, less separation of the chest wall flap may also lead to less postoperative pain. Also, the addition of preemptive analgesia in our inflation liquid (lidocaine) may provide significant postoperative pain control in the intraoperative and postoperative period.[28] Although the pain was not scored in this study, no patients complained of it, indirectly demonstrating the pain relief of our approach. Although the incision in the location between that in axilla and areola seemed to more visible compared with the ABA, most of the women patients could accept it because this small incision can be sheltered by the underwear. As anticipated, the cosmetic satisfaction rate of patients undergoing MABA in our study seemed to be similar to or even higher than that in the patients undergoing the ABA (100% vs 96.2%).[14]
As previously described, completion lobectomy including the ipsilateral residual lobe, central lymph nodes (compartment VI) and the isthmus, may be reasonable and acceptable for the low-risk patients.[7,29] Thus, this surgical extent was also utilized for our patients in our study, all of whom had no evidence of lymph node metastasis or local invasion. As anticipated, the PTMC was resected radically, with no postoperative residual thyroid. Only 1 patient developed cervical lymph nodes recurrence ipsilateral to the original tumor in the BA group during the follow-up period, but not any in the MABA group. This recurrence may be associated with its poor pathologic characteristics (T3N1aM0, tumor size = 0.9 cm, having extrathyroidal extension, and intraglandular dissemination, which all were high-risk factors for recurrence and metastasis),[30–33] although which could not be demonstrated by logistic regression analysis due to the limited number of patients. It is also important to note that the muscular sternocleidomastoid covered the field of operation in a male patient of MABA group when we dissected the inferior edge of central lymph nodes, which might affect the radical resection of operation. Thus, ET via MABA may be more suitable for the female and male without muscular sternocleidomastoid.
There were some limitations in our study. First was the retrospective in nature, which led to inevitable selection bias and some outcomes unavailable (i.e., quality of life score). Second, only the BA approach, the most commonly used in clinic,[19,20] was used as a control in this study, but not the conventional ABA due to the lacked samples in our hospital. In line with the potential superiority to ABA as above described, our results also indicated MABA was superior to BA because of shorter operation time (87.1 ± 9.3 vs 93.2 ± 8.3), fewer complications (9.1% vs 51.5%) and more cosmetic satisfaction (100% vs 81.8%). Also, multivariate logistic regression analysis showed MABA surgery method may be a protective factor for postoperative complications. These findings indicate our MABA may be a good choice for unilateral PTMC. Third, our sample size of MABA was relatively small and follow up was short, which may result in the underestimation of the complication rate and prognosis as well as overestimation of resection and cosmetic outcomes.[9] Fourth, the descending hypoglossal branch might be cut off when we dissected the lateral margin of anterior cervical muscle to expose the thyroid via MABA. The main function of descending hypoglossal branch is to dominate the anterior cervical muscle. At the follow-up, we have not found any bad influence on appearance or function of anterior cervical muscle, but more observation is still necessary. Fifth, MABA is confined to unilateral thyroidectomy and ipsilateral central lymph node dissection. It is unsuitable for bilateral thyroidectomy, so it cannot replace BA and conventional ABA completely. Accordingly, further prospective, long-term studies should be performed by comparison between MABA and ABA using the multicenter, larger samples and comprehensive outcomes scoring systems, including cosmetic, pain (Visual Analogue Scale [VAS]) and quality of life (European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-Core 30-question [EORTC-QLQ-C30]).[9,20,34,35]
5. Conclusion
ET with central lymph node dissection via MABA may be a feasible, safe, and effective operative approach for therapy of unilateral PTMC, which has shorter operation time, fewer complications, higher satisfaction, and excellent prognosis.
Author contributions
Conceptualization: KangNan Mo.
Data curation: KangNan Mo, Ming Zhao, JiaLei Gu.
Formal analysis: KangNan Mo.
Funding acquisition: Zhuo Tan.
Investigation: KangNan Mo.
Methodology: KangNan Mo.
Supervision: Zhuo Tan.
Writing – original draft: KangNan Mo.
Writing – review & editing: KeJing Wang, Zhuo Tan.
Footnotes
Abbreviations: ABA = axillo-breast approach, BA = breast approach ET = endoscopic thyroidectomy, HT = hemithyroidectomy, MABA = modified axillo-breast approach, PTC = papillary thyroid cancer, PTMC = papillary thyroid microcarcinoma, RLN = recurrent laryngeal nerve, TC = thyroid cancer, TL = thyroid lobectomy, TT = total thyroidectomy.
This study was supported by the Foundation of Ministry of Health of Zhejiang Province, Hangzhou, China (no.2014KYB038).
The authors have no conflicts of interest to disclose.
References
- [1].Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin 2016;66:7–30. [DOI] [PubMed] [Google Scholar]
- [2].Hundahl SA, Fleming ID, Fremgen AM, et al. A National Cancer Data Base report on 53,856 cases of thyroid carcinoma treated in the U.S., 1985–1995. Cancer 1998;83:2638–48. [DOI] [PubMed] [Google Scholar]
- [3].Aschebrook-Kilfoy B, Kaplan EL, Chiu BC-H, et al. The acceleration in papillary thyroid cancer incidence rates is similar among racial and ethnic groups in the United States. Ann Surg Oncol 2013;20:2746–53. [DOI] [PubMed] [Google Scholar]
- [4].Hirsch D, Levy S, Tsvetov G, et al. Total versus hemithyroidectomy for small unilateral papillary thyroid carcinoma. Oncol Lett 2014;7:849–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Macedo FI, Mittal VK. Total thyroidectomy versus lobectomy as initial operation for small unilateral papillary thyroid carcinoma: a meta-analysis. Surg Oncol 2015;24:117–22. [DOI] [PubMed] [Google Scholar]
- [6].Donatini G, Castagnet M, Desurmont T, et al. Partial thyroidectomy for papillary thyroid microcarcinoma: is completion total thyroidectomy indicated. World J Surg 2015;40:510–5. [DOI] [PubMed] [Google Scholar]
- [7].Wenbin YU, Song Y, Zhang N. Completion lobectomy and central compartment dissection in low-risk patients who had undergone less extensive surgery than hemithyroidectomy. Oncol Lett 2013;5:743–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Malandrino P, Pellegriti G, Attard M, et al. Papillary thyroid microcarcinomas: a comparative study of the characteristics and risk factors at presentation in two cancer registries. J Clin Endocrinol Metab 2013;98:1427–34. [DOI] [PubMed] [Google Scholar]
- [9].Ji YB, Song CM, Bang HS, et al. Long-term cosmetic outcomes after robotic/endoscopic thyroidectomy by a gasless unilateral axillo-breast or axillary approach. J Laparoendosc Adv Surg Tech A 2014;24:248–53. [DOI] [PubMed] [Google Scholar]
- [10].Kim SK, Sang YK, Youn HJ, et al. Comparison of conventional thyroidectomy and endoscopic thyroidectomy via axillo-bilateral breast approach in papillary thyroid carcinoma patients. Surg Endosc 2016;30:3419–25. [DOI] [PubMed] [Google Scholar]
- [11].Min JC, Park KS, Min JC, et al. A comparative analysis of endoscopic thyroidectomy versus conventional thyroidectomy in clinically lymph node negative thyroid cancer. Ann Surg Treat Res 2015;88:69–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Rd IW, Jacob BP, Gagner M. Minimally invasive endoscopic thyroidectomy by a cervical approach. Surg Endosc 2003;17:1808–11. [DOI] [PubMed] [Google Scholar]
- [13].Wang X, Yang W, Sun Y. Clinical application of endoscopic thyroidectomy via an anterior chest wall approach. Surg Laparosc Endosc Percutan Tech 2014;24:254–8. [DOI] [PubMed] [Google Scholar]
- [14].Koh YW, Kim JW, Lee SW, et al. Endoscopic thyroidectomy via a unilateral axillo-breast approach without gas insufflation for unilateral benign thyroid lesions. Surg Endosc 2009;23:2053–60. [DOI] [PubMed] [Google Scholar]
- [15].Tae K, Ji YB, Cho SH, et al. Initial experience with a gasless unilateral axillo-breast or axillary approach endoscopic thyroidectomy for papillary thyroid microcarcinoma: comparison with conventional open thyroidectomy. Surg Laparosc Endosc Percutan Tech 2011;21:162–9. [DOI] [PubMed] [Google Scholar]
- [16].Lee H, Lee J, Sung KY. Comparative study comparing endoscopic thyroidectomy using the axillary approach and open thyroidectomy for papillary thyroid microcarcinoma. World J Surg Oncol 2012;10:269–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Huang JK, Ma L, Song WH, et al. Quality of life and cosmetic result of single-port access endoscopic thyroidectomy via axillary approach in patients with papillary thyroid carcinoma. Onco Targets Ther 2016;9:4053–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Cho J, Lee D, Baek J, et al. Single-incision endoscopic thyroidectomy by the axillary approach with gas inflation for the benign thyroid tumor: retrospective analysis for a single surgeon's experience. Surg Endosc 2017;31:437–44. [DOI] [PubMed] [Google Scholar]
- [19].Tan Z, Gu JL, Han QB, et al. Comparison of conventional open thyroidectomy and endoscopic thyroidectomy via breast approach for papillary thyroid carcinoma. Int J Endocrinol 2015;2015:239610–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Ren XT ZD, Sha HC, Wu JY, et al. Comparative study of endoscopic thyroidectomy via a breast approach versus conventional open thyroidectomy in papillary thyroid microcarcinoma patients. Biomed Res 2017;28:5315–20. [Google Scholar]
- [21].Park KN, Jung CH, Ji OM, et al. Prospective comparative study of endoscopic via unilateral axillobreast approach versus open conventional total thyroidectomy in patients with papillary thyroid carcinoma. Surg Endosc 2015;30:3797–801. [DOI] [PubMed] [Google Scholar]
- [22].He QQ, Zhu J, Zhuang DY, et al. Comparative study between robotic total thyroidectomy with central lymph node dissection via bilateral axillo-breast approach and conventional open procedure for papillary thyroid microcarcinoma. Chin Med J (Engl) 2016;129:2160–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Lee MC, Mo JA, Joon Choi I, et al. New endoscopic thyroidectomy via a unilateral axillo-breast approach with gas insufflation: preliminary report. Head Neck 2013;35:471–6. [DOI] [PubMed] [Google Scholar]
- [24].Youn YK, Lee KE, Choi JY. Endoscopic thyroidectomy: bilateral axillo-breast approach (BABA). Color Atlas Thyroid Surg 2014;83–125. [Google Scholar]
- [25].Hong HJ, Shik KW, Woo KY, et al. Endoscopic thyroidectomy via an axillo-breast approach without gas insufflation for benign thyroid nodules and micropapillary carcinomas: preliminary results. Yonsei Med J 2011;52:643–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Kim SK, Woo JW, Park I, et al. Propensity score-matched analysis of robotic versus endoscopic bilateral axillo-breast approach (BABA) thyroidectomy in papillary thyroid carcinoma. Langenbecks Arch Surg 2017;402:243–50. [DOI] [PubMed] [Google Scholar]
- [27].Xia LY, He C, Huang XW, et al. The operation experience of endoscopic thyroidectomy by areola and axilla approach. Eur Arch Otorhinolaryngol 2016;273:555–8. [DOI] [PubMed] [Google Scholar]
- [28].Choi KW, Nam KH, Lee JR, et al. The effects of intravenous lidocaine infusions on the quality of recovery and chronic pain after robotic thyroidectomy: a randomized, double-blinded, controlled study. World J Surg 2017;41:1305–12. [DOI] [PubMed] [Google Scholar]
- [29].Lee CR, Son H, Lee S, et al. Lobectomy and prophylactic central neck dissection for papillary thyroid microcarcinoma: do involved lymph nodes mandate completion thyroidectomy. World J Surg 2014;38:872–7. [DOI] [PubMed] [Google Scholar]
- [30].Wang C, Chen X, Wei X, et al. Recurrence factors and prevention of complications of pediatric differentiated thyroid cancer. Asian J Surg 2016;40:55–60. [DOI] [PubMed] [Google Scholar]
- [31].Kim SJ, Park SY, Lee YJ, et al. Risk factors for recurrence after therapeutic lateral neck dissection for primary papillary thyroid cancer. Ann Surg Oncol 2014;21:1884–90. [DOI] [PubMed] [Google Scholar]
- [32].Erol V, Makay O, Icoz G, et al. Prognostic factors of survival and recurrence pattern in differentiated thyroid cancer: a retrospective study from Western Turkey. Endocr Regul 2014;48:173–81. [DOI] [PubMed] [Google Scholar]
- [33].Lamartina L, Borget I, Mirghani H, et al. Surgery for neck recurrence of differentiated thyroid cancer: outcomes and risk factors. J Clin Endocrinol Metab 2017;102:1020–31. [DOI] [PubMed] [Google Scholar]
- [34].Liu W, Zhou M. A comparative study on the transareola single-site versus three-port endoscopic thyroidectomy. J Laparoendosc Adv Surg Tech A 2017;27:242–6. [DOI] [PubMed] [Google Scholar]
- [35].Lee MC, Park H, Lee BC, et al. Comparison of quality of life between open and endoscopic thyroidectomy for papillary thyroid cancer. Head Neck 2016;38:E827–31. [DOI] [PubMed] [Google Scholar]


