Abstract
Although longer duration of untreated psychosis (DUP) is associated with poor response to antipsychotic treatment, it remains unclear whether it independently influences time to symptomatic remission in first-episode psychosis (FEP). This study examined rate of symptomatic remission, and explored if DUP, premorbid functioning, global functioning, insight and socio-demographic characteristics were independently associated with time to symptomatic remission in FEP.
This prospective study enrolled 126 FEP patients (aged 18–65) between June 2009 and September 2012. Subjects were followed-up monthly over 18 months after they had received antipsychotic medication. Remission in positive and negative symptoms was defined as in the Remission in Schizophrenia Working Group (RSWG) criteria. Subjects were defined as “in symptomatic remission” if they remitted in both negative and positive symptoms. At baseline, the following explanatory variables were measured: socio-demographic characteristics; DUP as short (≤5 months) and long (>5 months); premorbid functioning as deteriorating, stable poor, and stable good according to Cannon-Spoor Premorbid Adjustment Scale; global functioning as “worst (1–10) to serious (41–50)” and “moderate (51–60) to superior (91–100),” according to the Global Assessment of Functioning Scale; and insight as poor (≤8) and good (≥9) according to the Insight Scale (Birchwood). Univariate and multivariable analyses were used to generate results.
Out of 126 subjects, 98 (78%) completed follow-up, of which 70 (71.4%) achieved symptomatic remission within mean duration of 8.05 (4.54) months. Besides, having long DUP and separated/divorced/widowed (adjusted hazard ratio [aHR] = 0.07, 95%CI = [0.01, 0.46]), long DUP and poor insight (aHR = 0.18, 95%CI = [0.04, 0.89]), poor insight and separated/divorced/widowed (aHR = 0.09, 95%CI = [0.01, 0.70]), deteriorating premorbid functioning (aHR = 0.47, 95%CI = [0.23, 0.97]), family history of psychiatric disorders (aHR = 0.52, 95%CI = (0.30, 0.93]), and being male (aHR = 0.47, 95%CI = [0.24, 0.92]) delayed symptomatic remission.
These results propose that psychological interventions and social support for mental health problems are warranted and may enhance better response to antipsychotic medications among separated/divorced/widowed patients with long DUP or poor insight, and poor insight patients with long DUP. Deteriorating premorbid functioning, family history of psychiatric disorders and being male continue being important risk factors for poor odds of remission.
Keywords: antipsychotic medication, FEP, prospective study, risk factors, social support
1. Introduction
Improving functional outcomes in patients with first-episode psychosis (FEP) is a necessary mental health priority, and medications like prescription of antipsychotic drugs have been shown to improve symptomatic and functional outcomes, particularly positive symptoms.[1–4] However, despite prescription of effective antipsychotic treatment, a considerable number of occurrences of nonremission over time have been reported.[5–8]
Therefore, understanding risk factors for delayed response to antipsychotic medication would be essential because that may help future medications to affect modifiable risk factors, or to parse patients into therapeutically meaningful subgroups according to nonmodifiable risk factors.[9–11]
Some studies have shown that long duration of untreated psychosis (DUP),[8,12–14] poor premorbid functioning,[7,15,16] and poor insight[17,18] have been associated with delayed response to antipsychotic medication. On the other hand, socio-demographic factors such as younger age, tertiary level of education, being female, and being married significantly predicted recovery at 2 years follow-up.[19–21] However, it remains unclear whether each of the preceding factors could predict symptomatic remission in first-episode psychosis when adjusted for the others, socio-demographic characteristics, and some relevant prognostic factors. Furthermore, most research on rate of and time to symptomatic remission in first-episode psychosis were conducted in high- and middle- income countries whose findings may not generally apply elsewhere as evidence has shown that factors influencing symptomatic remission differed across countries,[22] and rates of remission differed across regions,[23] and across studies.[24]
In Malawi, cases of FEP with long DUP are common,[25] and no study has investigated the rate of and time to symptomatic remission and associated factors following prescription of antipsychotic medication. Therefore, with an aim to add more knowledge for improving treatment response in psychosis, particularly from Sub-Saharan Africa where such type of studies are rare, this study aimed to examine rate of symptomatic remission and find out if duration of untreated psychosis, premorbid functioning, global functioning, insight and socio-demographic characteristics were independently associated with time to symptomatic remission after prescription of antipsychotic medication in FEP.
2. Methods
2.1. Setting
This study was conducted in Northern Malawi, a landlocked country in the South of the Equator and South East Africa. As shown in Figure 1,[26] Lake Malawi, third largest in Africa, separates Malawi from Tanzania and Mozambique in the North East and East, respectively. There is Zambia to the North West border and Mozambique to the South East, South, and South West borders. Northern Malawi is where Saint John of God provides community services. According to the latest population and housing census,[27] it was estimated that there are 13.1 million people in Malawi, with annual growth rate of 2.8%. In particular, Northern Malawi comprises approximately 1.7 million people of which 47% are aged at least 18, 48.5% are male and 51.5% are female. Among those who are aged at least 18, 47.5% are male and 52.5% are female.
Figure 1.
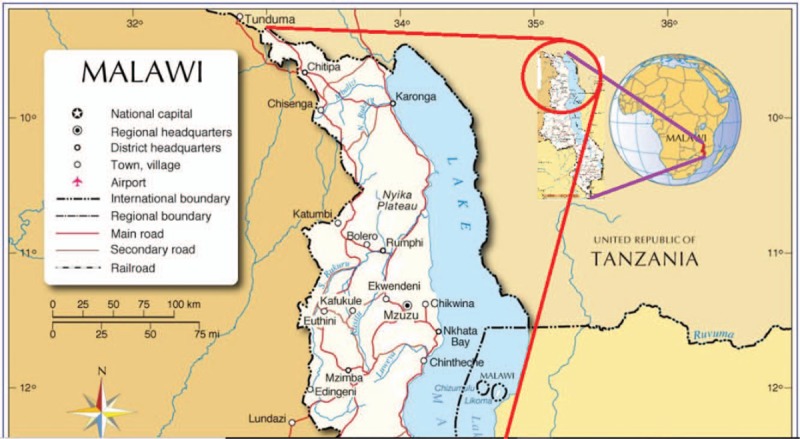
Map of Malawi[26] depicting the study area—Northern Malawi.
2.2. Subjects
In the period between June 2009 and September 2012, the Community Mental Health Care Team (CMHCT) of Saint John of God (SJOG) community services sensitized people about mental health disorders in the Northern part of Malawi, during a pilot study of early intervention service for psychosis, and an advertisement was made to receive and assess individuals for psychiatric disorders. In response to the advert, community members brought patients to the CMHCT for assessment, during which collateral information was sought from patients’ significant others or relatives in order to verify some symptoms and make sure about a diagnosis. An assessment was complete within 24 to 48 hours and, subsequently, treatment was initiated as appropriate. Depending on presentation, the following antipsychotic medications, commonly used in Malawi, were prescribed: oral drugs such as haloperidol tablets, chlorpromazine tablets, and risperidone tablets; and injectable medications which stay in the body working for 4 weeks such as haloperidol decanoate, fluphenazine, and depixol. This was an 18 months follow-up study which enrolled subjects from these patients. The inclusion criteria were as follows: diagnosed of psychosis disorder as defined in the Diagnostic and Statistical Manual of Mental Disorders, DSM-IV-TR Axis I Disorders, criteria[28]; classified by CMHCT research clinicians as having FEP and never ever received antipsychotic medication before; aged between 18 and 65 at first assessment by CMHCT research clinicians; and consented to take part in the study. Patients were excluded if they had a history of drug abuse, learning disability, neurological disorders, and organic illness. Figure 2 shows sample selection process in more detail. This study was approved by the National Health Sciences Research Committee (NHSRC) of the Ministry of Health in Malawi (NHSRC/577), and written informed consent was obtained from the patients or their guardians.
Figure 2.
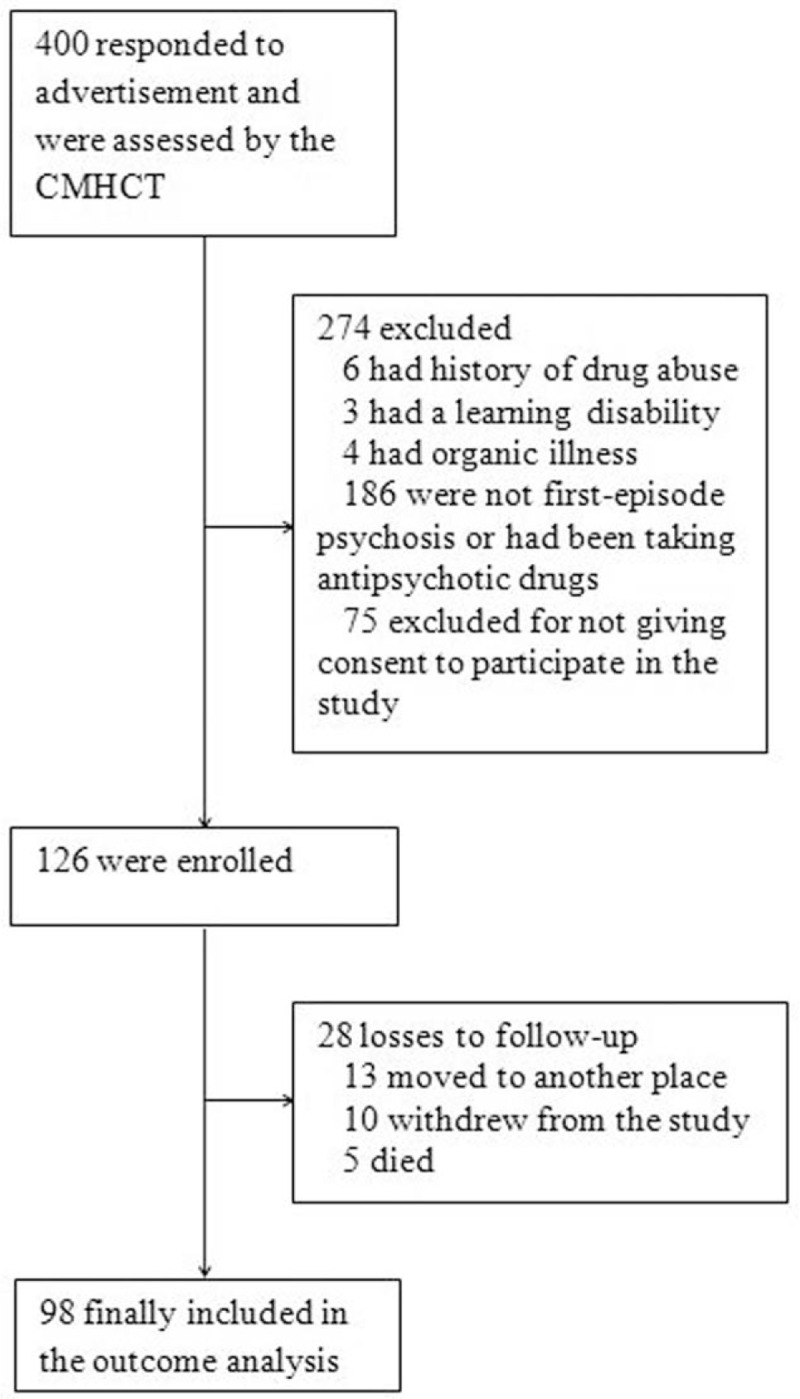
Flow diagram of subjects in Study Cohort. CMHCT = Community Mental Health Care Team.
2.3. Explanatory baseline variables
At baseline, clinical interviews were used with the scales described in this subsection to make psychiatric assessments and, as appropriate, collateral information were obtained from patients’ significant others or relatives to verify some symptoms. In this regard, mental disorders of participants were assessed using the Structured Clinical Interview for the DMS-IV-TR Axis I Disorders (SCID-I).[28] Also, socio-demographic variables such as age at assessment, age at onset, sex, marital status, level of education, employment status, and family history of psychiatric disorders were measured. The seriousness of mental illness in terms of the social, occupational, and psychological functioning of adults was subjectively rated using the Global Assessment of Functioning (GAF) scale as described in the DMS-IV-TR Axis V.[28] Subjects are rated using natural number codes between any of the 10 intervals (1–10, 11–20, 21–30, 31–40, 41–50, 51–60, 61–70, 71–80, 81–90, and 91–100). A score of zero means inadequate information. Then scores range from worst (1–10) to serious (41–50), and from moderate (51–60) to superior (91–100).
Positive symptoms were assessed using the Scale for the Assessment of Positive Symptoms (SAPS), whereas negative symptoms were assessed using the Scale for the Assessment of Negative Symptoms (SANS).[29,30] The SAPS has 4 symptoms domains and the SANS has 5 symptoms domains. Items for each domain are scored on a scale from 0 (absent) to 5 (severe) and these are used to obtain a global rating for the domain. An overall score for both scales is the sum of the global ratings of their respective domains.
Premorbid functioning concerning sociability and withdrawal, peer relationships, scholastic performance, adaptation to school and socio-sexual aspects of life were assessed in participants using the Premorbid Adjustment Scale (PAS) before the onset of symptoms of psychosis during developmental stages of childhood (at most 11 year), early adolescence (between 12 and 15 years), late adolescence (between 16 and 18 years), and adulthood (19 or more years).[31] The average of the mean developmental scores represents the total score for the scale and scores closer to but less than 1 indicate good premorbid. Changes in PAS total scores from one developmental stage to the other were classified as deteriorating, stable poor and stable good.[32]
Insight was measured using an insight scale according to Birchwood et al[33] to assess the 3 categories of insight: awareness of illness, awareness of symptoms, and awareness for need for treatment. Equal weight is given to each category to obtain total subscore between 0 and 4, which means the overall score ranges between 0 and 12, and good insight is identified by an overall score of 9 or greater.[34,35] The item, “my stay in hospital was necessary,” was omitted because all participants were not in admission at a hospital.[35]
Duration of untreated psychosis (DUP), defined as the length of the interval between the occurrence of first psychotic symptoms and the beginning of first antipsychotic medication, was measured using the Beiser Scale.[36,37] With reference to previous studies,[38,39] DUP was dichotomized as short (≤5) and long (>5).
2.4. Outcome variables
Follow-up assessments were conducted every month after initiation of antipsychotic medication and patients were censored at the end of follow-up time (after 18 months), or at the first time symptomatic remission was observed during the study period. Assessors at follow-up were blinded of patients’ previous assessment outcomes to avoid subjective bias. The primary outcome variable, time until observing positive and negative symptoms remission was recorded in months. Symptomatic remission at follow-up was defined according to the Remission in Schizophrenia Working Group (RSWG) criteria, which specified that a global score of at most 2 on all domains (hallucinations, delusions, bizarre behavior, and positive formal thought disorder) of the SAPS indicated patient was in positive symptom remission and, similarly, a global score of at most 2 on the domains (affective flattening or blunting, alogia, avolition apathy, anhedonia asociality) of the SANS indicated patient was in negative symptom remission.[40] When both of these conditions were satisfied a subject was classified as “in symptomatic remission,” otherwise a subject was classified as “not in symptomatic remission.
2.5. Statistical analysis
Windows Statistical Package for the Social Sciences (SPSS) Version 23.0 (IBM Corp, Armonk, NY) was used to compare distributions of baseline explanatory variables across the groups: lost to follow-up and follow-up completed. This was done using independent sample t-test or Mann Whitney U test for continuous variables depending on the normality of data and, on the other hand, the χ2 test (Pearson or Fisher's Exact test) was used for categorical variables.[41,42] In addition, the χ2 test was used to test the homogeneity of frequencies across categories of each categorical variable for the follow-up completed group.[41] Furthermore, predictors of time to symptomatic remission were identified using both univariate and multivariable Cox proportional hazard regression analyses,[41,43,44] using the R software version 3.4.1. Schoenfeld tests were performed to confirm proportional-hazard (PH) assumption and all the baseline explanatory variables, which satisfied the PH assumption, were included in the multivariable model of the Cox proportional hazard regression.[45] Interactions of potential predictor variables were also explored, and all terms showing significant interactions were included in the final multivariable model.[46] The final model was also tested for PH assumption. All statistical tests were two-tailed and the significance level was 0.05.
3. Results
3.1. Participants’ baseline characteristics
Of the 400 patients assessed by the CMHCT during a pilot early intervention study, 126 (31.5%) were enrolled in this study within a mode and median of 12 months, and 274 met the exclusion criteria (Fig. 2). Enrolled subjects were identified as Bipolar I disorder 12 (9.5%), Schizophrenia 100 (79.4%), and Schizophreniform disorder 14 (11.1%). With the exception of the variable, sex, the measurements of all other explanatory variables were evenly distributed between the follow-up completed and the loss to follow-up groups. The 98 patients in the follow-up completed group had mean (standard deviation [SD]) age of 35.8 (12.4), SAPS 8.3 (3.3), and SANS 4.4 (5.5) at first time receiving antipsychotic medication. In addition, majority in this group were male 66 (67.3), married 53 (54.1), more than primary level of education 63 (64.3), unemployed 82 (83.7), long DUP 67 (68.4), diagnosed with schizophrenia 79 (80.6), and poor insight 81 (82.7). Normality test indicated that data were skewed for the continuous variables: age at first time receiving antipsychotic medication, age at onset of psychotic symptoms, SANS, and SAPS (P value < 0.001). Therefore, Mann Whitney U test was used to compare the distribution of the measurements of these variables between the follow-up completed group and the lost to follow-up group. Table 1 shows the results in more detail.
Table 1.
Baseline characteristics.

3.2. Rate of and time to symptomatic remission
During a period of 18 months, 70 (71.4%) of the subjects achieved symptomatic remission at the mean time of 8.6 (5.1) months. Also, of the subjects who achieved symptomatic remission, one quarter of them achieved symptomatic remission within 4.7 months, while half within 8.0 months, and 3 quarters within 11.9 months.
3.3. Predictors of time to symptomatic remission
Univariate analysis was performed with each baseline explanatory variable except “type of psychosis” because this variable did not satisfy the PH assumption for Cox proportional hazard regression model (P = .014). The results indicated that being separated/divorced/widowed (hazard ratio (HR) = 0.46, 95%CI = [0.22–0.94]), having long DUP (HR = 0.60, 95%CI = (0.36–0.98), and having an increase in the severity of negative symptoms (HR = 0.95, 95%CI = [0.90–0.99]) reduced the likelihood to symptomatic remission at any time during the 18 months. Table 2 shows the results.
Table 2.
Association of baseline characteristics with time to symptomatic remission.

All the baseline explanatory variables in Table 2 were then entered into the multivariable Cox proportional hazard regression model to see their independent associations with time to symptomatic remission. Also, it was found that interactions when predicting time to symptomatic remission existed between marital status and DUP; marital status and insight; and insight and DUP. Thus, these interactions were also added to the model. Table 3 shows the results.
Table 3.
Independent predictors of time to symptomatic remission including interaction terms.
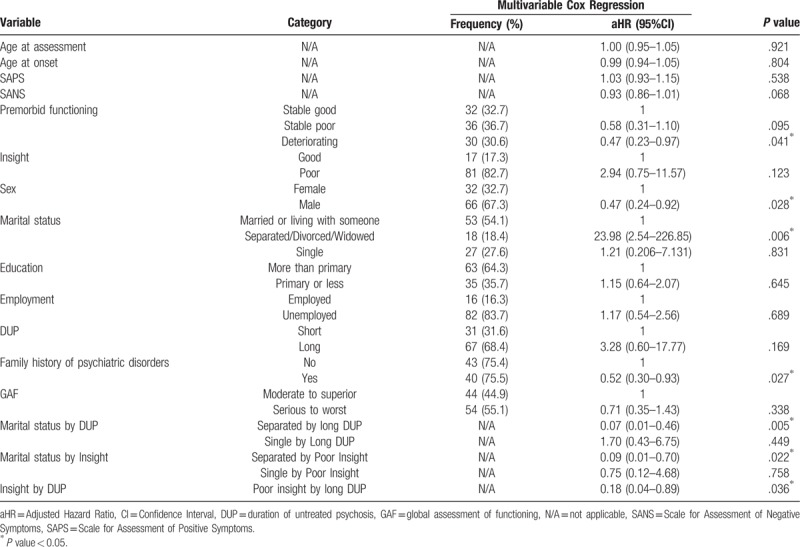
It should be noted here that it is common that when several covariates are investigated in a multivariable Cox proportional hazard regression model, the rate of false-positive or the chance of finding a spurious effect may increase with each additional test.[45] Therefore, the effect sizes may be exaggerated and a spurious effect by marital status in Table 3 was observed due to the addition of interaction terms involving this variable. However, results of the interaction terms in such analyses are the ones which matter most.[46,47] Additionally, the likelihood ratio test indicated that this model significantly predicted time to symptomatic remission (P value = .007), and also the global Schoenfield test suggested that the PH assumption was satisfied (P value = .148). Thus, it is a useful model for identifying potential predictors of time to symptomatic remission.
Results in this final model showed that having long DUP and separated/divorced/widowed (adjusted hazard ratio [aHR] = 0.07, 95%CI = [0.01, 0.46]), long DUP and poor insight (aHR = 0.18, 95%CI = [0.04, 0.89]), poor insight and separated/divorced/widowed (aHR = 0.09, 95%CI = [0.01, 0.70]), deteriorating premorbid functioning (aHR = 0.47, 95%CI = [0.23, 0.97]), family history of psychiatric disorders (aHR = 0.52, 95%CI = [0.30, 0.93]), and being male (aHR = 0.47, 95%CI = [0.24, 0.92]) reduced the likelihood of remission at any given time over 18 months by 93.3%, 82%, 91%, 53%, 48%, and 53%, respectively.
4. Discussion
This is the first study to explore predictors of symptomatic remission in Malawi and it established the following evidence. First, 71.4% of the subjects achieved symptomatic remission over 18-month period, during which they received antipsychotic medications. Second, long DUP or poor insight may increase the time to symptomatic remission among the separated/divorced/widowed group. Third, long DUP may prolong time to symptomatic remission among the poor insight group. Finally, deteriorating premorbid functioning, having family history of psychiatric disorders, and being male reduced the likelihood of symptomatic remission at any time within 18 months.
The rate of symptomatic remission in this study is higher than that of similar studies in Ethiopia,[48,49] perhaps because of sample or methodological or regional differences. Nonetheless, just like our findings, one of those studies indicated that living in a household with 3 or more adults was significantly associated with attaining remission.[48] However, in contrast with our findings, the other study indicated that being single was significantly associated with attaining remission but was quick to clarify that majority of those who were single stayed with relatives, which could be a confounding factor.[49] Furthermore, despite longer DUP being shown to be associated with poor response to antipsychotic treatment,[19,22,50,51] this study has shown that its effect could be altered by marital status, with those having long DUP and separated/divorced/widowed slow to respond to antipsychotic medication. Also, despite poor insight being shown to be associated with poor response to antipsychotic medication,[17,18] this study showed that marital status could alter its effect on symptomatic remission, with those having poor insight and separated/divorced/widowed being slow to respond to antipsychotic medication. Therefore, social support, particularly the emotional support, often from a close relationship, is one important protective factor for mental health problems. For example, being married and social support were shown to improve medication adherence,[52–54] which was associated with better response to antipsychotic medication.[7,15,55] Therefore, among other reasons, it may be speculated that those with marital status, separated/divorced/widowed, and long DUP or poor insight might have needed social support to enhance their response to antipsychotic medication. In fact, support systems that have been there when in marriage may no longer be sustained or cease to be effective after family separation/divorced/widowed.[56] In such circumstances, if no substitute support could be attained elsewhere, the mental health condition of family members with psychosis may go from bad to worse. Also, patients with poor insight may disagree that they have mental illness, unusual experiences, abnormal behaviors, and that they are in need of clinical treatment.[33,34,57] Hence they are more unlikely to achieve response to medication.[58] Consequently, as found in this study, it can be suggested that long DUP participants with poor insight were less likely to achieve symptomatic remission within 18 months of follow-up when compared with long DUP participants with good insight. In this regard, family social support and good insight may play a crucial role in helping long DUP or poor insight patients to achieve quicker response to antipsychotic medication and hence improve the prognosis of the disease.[58–62] Therefore, psychological interventions and social support related to prescription of antipsychotic medications are warranted and may improve better response to antipsychotic medications among separated patients with long DUP or poor insight, and poor insight patients with long DUP.
Moreover, available evidence has shown that good premorbid functioning was associated with better response to treatment and fewer extrapyramidal symptoms.[15,63–65] Also, poor premorbid functioning was suspected to indicate an illness subtype less likely to respond to antipsychotic treatment regardless of when it was instituted.[66,67] Therefore, the preceding results are in agreement with the findings of this study which suggested that deteriorating premorbid functioning may impede quick response to antipsychotic medication. Thus, this study supports the idea that premorbid symptom assessment should remain an important clinical tool in the evaluation of psychotic symptoms and is of potential prognostic value.[67] Interventions to ensure good premorbid functioning in individuals at high risk of psychosis may help them respond positively to antipsychotic medications later in life should they suffer from psychotic disorders.
Also, family history of developing a disease is considered as an important variable in understanding prognosis of the disease.[68–70] For example, in patients with affective disorders, having a family history of bipolar illness and response of affected family members to lithium treatment were important indicators of favorable lithium response.[71] Similarly but in the opposite manner to this finding, in this study, having family history of psychiatric disorders was associated with delayed time to treatment response. This is consistent with some studies, which also showed that it was associated with poor response to antipsychotic drugs.[72,73] Therefore, it was suggested that there might be a genetic influence on treatment response in psychosis.[74] Thus, this result supports the necessity for research to identify biological markers that could influence response to antipsychotic drugs and, should they be discovered, they may be helpful to optimize medications to improve prognosis of the disease.[69,75] Apparently, early interventions for first-episode psychosis could be a precautionary measure to improve treatment response in individuals with family history of psychiatric disorders.[76] Additionally, being male reduced the likelihood of symptomatic remission in this study. This outcome is consistent with results of some previous studies which found that compared with men being female significantly predicted more likelihood to recovery in FEP and schizophrenia.[19,63,77,78] Some possible explanation of this heterogeneity was that males had more risk factors for relapse than females, including substance abuse, nonadherence, reduced help seeking behavior and increased baseline psychopathology.[78,79] In this regard, men may require special attention to help them avoid the preceding factors, so as to enhance their response to antipsychotic medication.
Some factors need to be considered when interpreting the results of this study. First, the final model may be susceptible to an increased rate of false-positive or chance of spurious effect due to the additional covariates involving interactions.[45] Hence the effect sizes may be exaggerated. Nevertheless, the model significantly predicted time to symptomatic remission under the PH assumption and managed to replicate some findings from other similar studies. Second, subjects of this study were aged between 18 and 65, hence this may limit generalizing these findings to children and adolescents, and due to a smaller sample size of the locally characterized population enrolled, extrapolation of these results to other patient groups need to be verified with more investigations using larger sample sizes. Nonetheless, the findings may accordingly be inferred to other members of the sample and hence lay a foundation for better understanding of the predictors of treatment response specific for this local population. Third, drop out of participants due to loss to follow-up may cause selection bias. However, the drop out group had virtually the same baseline characteristics with the group included in all the analyses of this study. Hence, low possibility of selection bias. Fourth, nonadherence which was positively related to new episodes was not measured in this study. It could be interesting to see its influence on symptomatic remission in this group. However, since being married was associated with adherence to medication and adherence to medication was associated with better response to medication in first-episode psychosis, the effect of marital status on symptomatic remission in this study may, to some extent, be implied on the outcomes of adherence to medication on symptomatic remission. Finally, DUP was measured retrospectively, which is prone to recall bias. Thus, there is a possibility that this measure could be exaggerated in some cases.
5. Conclusions
This study suggests that, although long DUP was an independent predictor of poor treatment response in other studies, its effect could be altered by marital status or insight. Similarly, the effect of poor insight on symptomatic remission could be altered by marital status. Therefore, in addition to prescribing antipsychotic medications, psychological interventions and social support for mental health problems are warranted and may enhance better response to antipsychotic medications among separated patients with long DUP or poor insight, and poor insight patients with long DUP. More research integrating premorbid functioning, family history of psychiatric disorders, and gender with genetic and environmental factors related to response to antipsychotic medications is needed and may have great potential for generating better clinically relevant predictors.
Acknowledgments
The authors are very grateful to all participants for consenting to provide information for this study, and to the Editor and all Reviewers for their constructive comments which improved the clarity of this paper.
Author contributions
Conceptualization: Atipatsa Chiwanda Kaminga, Aizhong Liu.
Data curation: Atipatsa Chiwanda Kaminga, Wenjie Dai, Japhet Myaba, Richard Banda, Xiongfeng Pan.
Formal analysis: Atipatsa Chiwanda Kaminga, Wenjie Dai, Xiongfeng Pan.
Investigation: Atipatsa Chiwanda Kaminga, Wenjie Dai, Japhet Myaba, Richard Banda, Xiongfeng Pan.
Methodology: Atipatsa Chiwanda Kaminga, Wenjie Dai, Aizhong Liu, Shi Wu Wen.
Project administration: Aizhong Liu.
Resources: Aizhong Liu, Japhet Myaba, Richard Banda, Shi Wu Wen.
Supervision: Aizhong Liu, Shi Wu Wen.
Validation: Atipatsa Chiwanda Kaminga, Wenjie Dai, Shi Wu Wen.
Visualization: Atipatsa Chiwanda Kaminga.
Writing – original draft: Atipatsa Chiwanda Kaminga.
Writing – review & editing: Wenjie Dai, Aizhong Liu, Japhet Myaba, Richard Banda, Shi Wu Wen, Xiongfeng Pan.
Atipatsa Chiwanda Kaminga: 0000-0002-6556-4590.
Atipatsa Chiwanda Kaminga orcid: 0000-0002-6556-4590.
Footnotes
Abbreviations: aHR = adjusted hazard ratio, CMHCT = Community Mental Health Care Team, DSM-IV-TR = Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition (Text Revision), DUP = duration of untreated psychosis, FEP = first-episode psychosis, GAF = Global Assessment of Functioning, HR = hazard ratio, IBM = International Business Machines Corporation, NHSRC = National Health Sciences Research Committee, NY = New York, PAS = premorbid adjustment scale, PH = proportional hazard, RSWG = Remission in Schizophrenia Working Group, SANS = Scale for the Assessment of Negative Symptoms, SAPS = Scale for the Assessment of Positive Symptoms, SCID-I = Structured Clinical Interview for the DMS-IV-TR Axis I Disorders, SD = standard deviation, SOJG = Saint John of God, SPSS = Statistical Package for the Social Sciences.
Financial Support: This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Ethical Standard: The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Availability of Data and Materials: The data and materials supporting the findings of this study could be obtained from AL by contacting him on the email lazroy@live.cn.
The authors have no conflicts of interest to disclose.
References
- [1].Correll CU, Malhotra AK, Kaushik S, et al. Early prediction of antipsychotic response in schizophrenia. Am J Psychiatry 2003;160:2063–5. [DOI] [PubMed] [Google Scholar]
- [2].Lee NY, Kim SH, Cho SJ, et al. A prospective, open-label study to evaluate symptomatic remission in schizophrenia with risperidone long-acting injectable in Korea. Int Clin Psychopharmacol 2014;29:279–87. [DOI] [PubMed] [Google Scholar]
- [3].Simonsen C, Faerden A, Romm KL, et al. Early clinical recovery in first-episode psychosis: symptomatic remission and its correlates at 1-year follow-up. Psychiatry Res 2017;254:118–25. [DOI] [PubMed] [Google Scholar]
- [4].Marques TR, Arenovich T, Agid O, et al. The different trajectories of antipsychotic response: antipsychotics versus placebo. Psychol Med 2011;41:1481–8. [DOI] [PubMed] [Google Scholar]
- [5].Emsley R, Oosthuizen PP, Kidd M, et al. Remission in first-episode psychosis: predictor variables and symptom improvement patterns. J Clin Psychiatry 2006;67:1707–12. [DOI] [PubMed] [Google Scholar]
- [6].Loebel AD, Lieberman JA, Alvir JM, et al. Duration of psychosis and outcome in first-episode schizophrenia. Am J Psychiatry 1992;149:1183–8. [DOI] [PubMed] [Google Scholar]
- [7].Malla A, Norman R, Schmitz N, et al. Predictors of rate and time to remission in first-episode psychosis: a two-year outcome study. Psychol Med 2006;36:649–58. [DOI] [PubMed] [Google Scholar]
- [8].Demjaha A, Lappin JM, Stahl D, et al. Antipsychotic treatment resistance in first-episode psychosis: prevalence, subtypes and predictors. Psychol Med 2017;47:1981–9. [DOI] [PubMed] [Google Scholar]
- [9].Carbon M, Correll CU. Clinical predictors of therapeutic response to antipsychotics in schizophrenia. Dialogues Clin Neurosci 2014;16:505–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Murray R, Correll CU, Reynolds GP, et al. Atypical antipsychotics: recent research findings and applications to clinical practice: Proceedings of a symposium presented at the 29th Annual European College of Neuropsychopharmacology Congress, 19 September 2016, Vienna, Austria. Ther. Adv Psychopharmacol 2017;7Suppl 1:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Lally J, MacCabe JH. Antipsychotic medication in schizophrenia: a review. Br Med Bull 2015;114:169–79. [DOI] [PubMed] [Google Scholar]
- [12].Perkins DO, Gu H, Boteva K, et al. Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: a critical review and meta-analysis. Am J Psychiatry 2005;162:1785–804. [DOI] [PubMed] [Google Scholar]
- [13].Wiersma D, Nienhuis FJ, Slooff CJ, et al. Natural course of schizophrenic disorders: a 15-year followup of a Dutch incidence cohort. Schizophr Bull 1998;24:75–85. [DOI] [PubMed] [Google Scholar]
- [14].Zhang HX, Shen XL, Zhou H, et al. Predictors of response to second generation antipsychotics in drug naive patients with schizophrenia: a 1 year follow-up study in Shanghai. Psychiatry Res 2014;215:20–5. [DOI] [PubMed] [Google Scholar]
- [15].Ezeme MS, Uwakwe R, Ndukuba AC, et al. Clinical correlates of treatment response among patients with schizophrenia in a tertiary Nigerian hospital. J Health Care Poor Underserved 2017;28:721–38. [DOI] [PubMed] [Google Scholar]
- [16].AlAqeel B, Margolese HC. Remission in schizophrenia: critical and systematic review. Harv Rev Psychiatry 2012;20:281–97. [DOI] [PubMed] [Google Scholar]
- [17].Lizzette G-d-R, Thomas RK, Joan Manel B, et al. Predictors of outcome in the early course of first-episode psychosis. Eur J Psychiatry 2010;24:87–97. [Google Scholar]
- [18].Catts SV, O’Toole B. Raising the standard of care in the treatment of schizophrenia: yes we can!. Aust N Z J Psychiatry 2017;51:438–40. [DOI] [PubMed] [Google Scholar]
- [19].Verma S, Subramaniam M, Abdin E, et al. Symptomatic and functional remission in patients with first-episode psychosis. Acta Psychiatr Scand 2012;126:282–9. [DOI] [PubMed] [Google Scholar]
- [20].Chung YC, Cui Y, Kim MG, et al. Early predictors of a clinical response at 8 weeks in patients with first-episode psychosis treated with paliperidone ER. J Psychopharmacol 2016;30:810–8. [DOI] [PubMed] [Google Scholar]
- [21].Mihaljevic-Peles A, Sagud M, Filipcic IS, et al. Remission and employment status in schizophrenia and other psychoses: one-year prospective study in Croatian patients treated with risperidone long acting injection. Psychiatr Danub 2016;28:263–72. [PubMed] [Google Scholar]
- [22].Lambert M, De Marinis T, Pfeil J, et al. Establishing remission and good clinical functioning in schizophrenia: predictors of best outcome with long-term risperidone long-acting injectable treatment. Eur Psychiatry 2010;25:220–9. [DOI] [PubMed] [Google Scholar]
- [23].Novick D, Haro JM, Hong J, et al. Regional differences in treatment response and three year course of schizophrenia across the world. J Psychiatr Res 2012;46:856–64. [DOI] [PubMed] [Google Scholar]
- [24].Emsley R, Chiliza B, Asmal L, et al. The concepts of remission and recovery in schizophrenia. Curr Opin Psychiatry 2011;24:114–21. [DOI] [PubMed] [Google Scholar]
- [25].Chilale HK, Banda R, Muyawa J, et al. Duration of untreated psychosis and associated factors in first episode psychosis in Mzuzu in Northern Malawi. Afr J Psychiatry 2014;17:503–7. [Google Scholar]
- [26].Nations Online Project. Political Map of Malawi based on United Nations Geospatial Information Section. Available at: http://www.nationsonline.org/oneworld/map/malawi_map.htm Accessed September 25, 2018. [Google Scholar]
- [27].Malawi Government. 2008 Population and Housing Census Preliminary Report. In: Office NS, ed. Malawi: National Statistical Office; 2008:1–35. [Google Scholar]
- [28].Biometrics Research, New York State Psychiatric Institute, First, Michael B, Spitzer, et al. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition With Psychotic Screen (SCID-I/P W/PSY SCREEN) New York. 2002. [Google Scholar]
- [29].Andreasen NC. Scale for the Assessment of Negative Symptoms (SANS). Iowa City: University of Iowa Press; 1983. [Google Scholar]
- [30].Andreasen NC. The Scale for the Assessment of Positive Symptoms (SAPS). Iowa City: University of Iowa Press; 1984. [Google Scholar]
- [31].Cannon-Spoor HE, Potkin SG, Wyatt RJ. Measurement of premorbid adjustment in chronic schizophrenia. Schizophr Bull 1982;8:470–84. [DOI] [PubMed] [Google Scholar]
- [32].Larsen TK, McGlashan TH, Johannessen JO, et al. First-episode schizophrenia: II. Premorbid patterns by gender. Schizophr Bull 1996;22:257–69. [DOI] [PubMed] [Google Scholar]
- [33].Birchwood M, Smith J, Drury V, et al. A self-report insight scale for psychosis: reliability, validity and sensitivity to change. Acta Psychiatr Scand 1994;89:62–7. [DOI] [PubMed] [Google Scholar]
- [34].Cooke MA, Peters ER, Greenwood KE, et al. Insight in psychosis: influence of cognitive ability and self-esteem. Br J Psychiatry 2007;191:234–7. [DOI] [PubMed] [Google Scholar]
- [35].Jonsdottir H, Engh JA, Friis S, et al. Measurement of insight in patients with bipolar disorder: are self-rated scales developed for patients with schizophrenia applicable? J Nerv Ment Dis 2008;196:333–5. [DOI] [PubMed] [Google Scholar]
- [36].Beiser M, Erickson D, Fleming JA, et al. Establishing the onset of psychotic illness. Am J Psychiatry 1993;150:1349–54. [DOI] [PubMed] [Google Scholar]
- [37].Register-Brown K, Hong LE. Reliability and validity of methods for measuring the duration of untreated psychosis: a quantitative review and meta-analysis. Schizophr Res 2014;160:20–6. [DOI] [PubMed] [Google Scholar]
- [38].Tang JY, Chang WC, Hui CL, et al. Prospective relationship between duration of untreated psychosis and 13-year clinical outcome: a first-episode psychosis study. Schizophr Res 2014;153:1–8. [DOI] [PubMed] [Google Scholar]
- [39].Cechnicki A, Cichocki L, Kalisz A, et al. Duration of untreated psychosis (DUP) and the course of schizophrenia in a 20-year follow-up study. Psychiatry Res 2014;219:420–5. [DOI] [PubMed] [Google Scholar]
- [40].Andreasen NC, Carpenter WT, Jr, Kane JM, et al. Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatry 2005;162:441–9. [DOI] [PubMed] [Google Scholar]
- [41].Wiley-Blackwell, Kirkwood BR, Sterne JAC. Essential Medical Statistics. 2nd edn2003. [Google Scholar]
- [42].Shapiro SS, Wilk MB. An analysis of variance test for normality (complete samples). Biometrika 1965;52:591–611. [Google Scholar]
- [43].Cox DR. Regression models and life-tables. J R Stat Soc Series B Stat Methodol 1972;34:187–220. [Google Scholar]
- [44].Crowley JJ, Hu M. Covariance analysis of heart transplants survival data. J Am Stat Assoc 1977;72:27–36. [Google Scholar]
- [45].Bradburn MJ, Clark TG, Love SB, et al. Survival analysis Part III: multivariate data analysis—choosing a model and assessing its adequacy and fit. Br J Cancer 2003;89:605–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Kamangar F. Effect modification in epidemiology and medicine. Arch Iran Med 2012;15:575–82. [PubMed] [Google Scholar]
- [47].VanderWeele TJ, Knol Mirjam J. A Tutorial on Interaction. Epidemiol Methods 2014;3:33. [Google Scholar]
- [48].Alem A, Kebede D, Fekadu A, et al. Clinical course and outcome of schizophrenia in a predominantly treatment—naive cohort in rural Ethiopia. Schizophr Bull 2009;35:646–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Teferra S, Shibre T, Fekadu A, et al. Five-year clinical course and outcome of schizophrenia in Ethiopia. Schizophr Res 2012;136:137–42. [DOI] [PubMed] [Google Scholar]
- [50].Friis S, Melle I, Johannessen JO, et al. Early predictors of ten-year course in first-episode psychosis. Psychiatr Serv 2016;67:438–43. [DOI] [PubMed] [Google Scholar]
- [51].Wunderink L, Sytema S, Nienhuis FJ, et al. Clinical recovery in firste-episode psychosis. Schizophr Bull 2009;35:362–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Gomes-Villas Boas LC, Foss MC, Freitas MC, et al. Relationship among social support, treatment adherence and metabolic control of diabetes mellitus patients. Rev Lat Am Enfermagem 2012;20:52–8. [DOI] [PubMed] [Google Scholar]
- [53].Trivedi RB, Ayotte B, Edelman D, et al. The association of emotional well-being and marital status with treatment adherence among patients with hypertension. J Behav Med 2008;31:489–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Wu JR, Lennie TA, Chung ML, et al. Medication adherence mediates the relationship between marital status and cardiac event-free survival in patients with heart failure. Heart Lung 2012;41:107–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Bernardo M, Cañas F, Herrera B, et al. Adherence predicts symptomatic and psychosocial remission in schizophrenia: Naturalistic study of patient integration in the community. Rev Psiquiatr Salud Ment 2017;10:149–59. [DOI] [PubMed] [Google Scholar]
- [56].Robinson E, Rodgers B, Butterworth P. Family Relationships and Mental Illness: Impacts and Service Responses. Australian Family Relationships Clearinghouse, Melbourne, Vic: Australian Institute of Family Studies; 2008. [Google Scholar]
- [57].Bitter I, Fehér L, Tényi T, et al. Treatment adherence and insight in schizophrenia. Psychiatr Hung 2015;30:18–26. [PubMed] [Google Scholar]
- [58].Novick D, Montgomery W, Treuer T, et al. Relationship of insight with medication adherence and the impact on outcomes in patients with schizophrenia and bipolar disorder: results from a 1-year European outpatient observational study. BMC Psychiatry 2015;15:189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Ascher-Svanum H, Zhao F, Detke HC, et al. Early response predicts subsequent response to olanzapine long-acting injection in a randomized, double-blind clinical trial of treatment for schizophrenia. BMC Psychiatry 2011;11:152–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Samara MT, Leucht C, Leeflang MM, et al. Early improvement as a predictor of later response to antipsychotics in schizophrenia: a diagnostic test review. Am J Psychiatry 2015;172:617–29. [DOI] [PubMed] [Google Scholar]
- [61].Yildiz M, Yazici MK, Yagcioglu AEA, et al. Prediction of response to antipsychotic drugs in schizophrenia patients within the early phase of treatment. Klinik Psikofarmakol Bülteni 2015;25:390–8. [Google Scholar]
- [62].Harrison G, Hopper K, Craig T, et al. Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506–17. [DOI] [PubMed] [Google Scholar]
- [63].Cannavo D, Minutolo G, Battaglia E, et al. Insight and recovery in schizophrenic patients. Int J Psychiatry Clin Pract 2016;20:83–90. [DOI] [PubMed] [Google Scholar]
- [64].Rabinowitz J, Harvey PD, Eerdekens M, et al. Premorbid functioning and treatment response in recent-onset schizophrenia. Br J Psychiatry 2018;189:31–5. [DOI] [PubMed] [Google Scholar]
- [65].Rabinowitz J, Napryeyenko O, Burba B, et al. Premorbid functioning and treatment response in recent-onset schizophrenia: prospective study with risperidone long-acting injectable. J Clin Psychopharmacol 2011;31:75–81. [DOI] [PubMed] [Google Scholar]
- [66].Perkins D, Lieberman J, Gu H, et al. Predictors of antipsychotic treatment response in patients with first-episode schizophrenia, schizoaffective and schizophreniform disorders. Br J Psychiatry 2004;185:18–24. [DOI] [PubMed] [Google Scholar]
- [67].Strous RD, Alvir JM, Robinson D, et al. Premorbid functioning in schizophrenia: relation to baseline symptoms, treatment response, and medication side effects. Schizophr Bull 2004;30:265–78. [DOI] [PubMed] [Google Scholar]
- [68].Do CB, Hinds DA, Francke U, et al. Comparison of family history and SNPs for predicting risk of complex disease. PLoS Genet 2012;8:e1002973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].McMahon FJ. Prediction of treatment outcomes in psychiatry—where do we stand ? Dialogues Clin Neurosci 2014;16:455–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Pyeritz RE. The family history: the first genetic test, and still useful after all those years? Genet Med 2012;14:3–9. [DOI] [PubMed] [Google Scholar]
- [71].Ananth J, Pecknold JC. Prediction of lithium response in affective disorders. J Clin Psychiatry 1978;39:95–100. [PubMed] [Google Scholar]
- [72].Crespo-Facorro B, de la Foz VO-G, Ayesa-Arriola R, et al. Prediction of acute clinical response following a first episode of non affective psychosis: Results of a cohort of 375 patients from the Spanish PAFIP study. Prog Neuropsychopharmacol Biol Psychiatry 2013;44:162–7. [DOI] [PubMed] [Google Scholar]
- [73].Huber CG, Naber D, Lambert M. Incomplete remission and treatment resistance in first-episode psychosis: definition, prevalence and predictors. Expert Opin Pharmacother 2008;9:2027–38. [DOI] [PubMed] [Google Scholar]
- [74].Moretti PN, Ota VK, Gouvea ES, et al. Accessing gene expression in treatment-resistant schizophrenia. Mol Neurobiol 2018;55:7000–8. [DOI] [PubMed] [Google Scholar]
- [75].Hyman SE. The genetics of mental illness: implications for practice. Bull World Health Organ 2000;78:455–63. [PMC free article] [PubMed] [Google Scholar]
- [76].Crumlish N, Whitty P, Clarke M, et al. Beyond the critical period: longitudinal study of 8-year outcome in first-episode non-affective psychosis. Br J Psychiatry 2018;194:18–24. [DOI] [PubMed] [Google Scholar]
- [77].Robinson DG, Woerner MG, Alvir JM, et al. Predictors of treatment response from a first episode of schizophrenia or schizoaffective disorder. Am J Psychiatry 1999;156:544–9. [DOI] [PubMed] [Google Scholar]
- [78].Rabinowitz J, Werbeloff N, Caers I, et al. Determinants of antipsychotic response in schizophrenia: implications for practice and future clinical trials. J Clin Psychiatry 2014;75:e308–16. [DOI] [PubMed] [Google Scholar]
- [79].Emsley R. New advances in pharmacotherapy for early psychosis. Early Interv Psychiatry 2009;3Suppl 1:S8–12. [DOI] [PubMed] [Google Scholar]


