Abstract
Rationale:
Retroperitoneal colonic perforation is a rare cause of retroperitoneal abscess. It presents, more frequently in frail elderly patients, with heterogeneous signs and symptoms which hamper the clinical diagnosis. Subcutaneous emphysema with pneumomediastinum and iliopsoas muscle abscess are unusual signs. Colonic retroperitoneal perforation may be consequent to diverticulitis or locally advanced colon cancer. Due to the anatomy of the retroperitoneal space and different physiopathology, diverticular perforation may present with air and pus collection; on the other hand perforated colon cancer may cause groin mass and psoas abscess. We reported 2 cases of colonic retroperitoneal perforation from diverticulitis and locally advanced colon cancer, respectively. Aim of this report is to improve differential diagnosis based on clinical signs.
Patients’ concerns:
A 71-year-old man presented with pain in his left side, fatigue, fever, nausea, massive subcutaneous emphysema of the neck, and Blumberg sign in the left iliac fossa. A 67-year-old man presented with abdominal pain, sub-occlusion, left groin mass, left groin, and lower limb pain during walking, negative Blumberg sign.
Diagnosis:
In the first patient the computerized tomography revealed pneumoperitoneum, gas in the mesosigma, pneumomediastinum, wall thickening of the descending colon, and retroperitoneal collection from diverticular perforation. In the second patient abdominal CT scan found thickening of the sigmoid colon adherent to the iliopsoas and fluid collection.
Interventions:
In the first patient, a left hemicolectomy extending to the transverse colon, followed by a toilette and debridement of the retroperitoneum were performed. In the second patient, tumor of descending colon perforated in the retroperitoneum with iliopsoas abscess was treated with left hemicolectomy and a drainage of the abscess.
Outcomes:
The first patient underwent right colectomy with ileostomy in the 7th postoperative day for large bowel necrosis. He died of sepsis 2 days after. The second patient had regular postoperative and he is still alive.
Lessons:
The spread of retroperitoneal abscess in complicated colonic diverticulitis is different from that in advanced colonic cancer. The former can present with a subcutaneous emphysema, the latter with a groin mass. Hence a thorough clinical examination and radiological studies are needed to diagnose these conditions.
Keywords: cancer, case report, clinical, colon, diverticulitis, perforation, retroperitoneal abscess
1. Introduction
The retroperitoneal infections are associated with a mortality rate approximately 20%.[1] The retroperitoneal colonic perforations are rare causes of retroperitoneal abscess and are relatively frequent in frail elderly patients. These perforations have various etiology and show up with heterogeneous signs and symptoms, so the clinical diagnosis can be very difficult. Two unusual signs are associated with retroperitoneal perforation: subcutaneous emphysema with pneumomediastinum and muscle psoas abscesses. Subcutaneous emphysema is a swelling due to the presence of air or gas in the interstices of connective tissue.[2] Subcutaneous cervical, mediastinal, and retroperitoneal emphysema usually can occur as an endoscopic or traumatic complication. The origin of gas diffusion could be various such as the respiratory tract (e.g., pneumothorax and bronchial fistula), the gastrointestinal tract (perforation), and infective causes (necrotizing fasciitis).[3] In these cases, the continuum of fascial planes between the cervical tissues, thorax, and abdomen allows the spread of infection in the retroperitoneum, in the mediastinum to the subcutaneous tissues of the neck.[4] Thus, pneumoretroperitoneum, pneumomediastinum, and neck subcutaneous emphysema are rare signs of colonic retroperitoneal perforation from complicated diverticular disease or locally advanced colon cancer (T4).[5] Rarely, the colonic perforation may cause a pus collection in the iliopsoas muscle. In these cases, the typical manifestation of retroperitoneal perforation of colon can be a groin mass from the diffusion of pus along iliopsoas muscular tract.[6] In this article, we reported two cases of retroperitoneal abscess from colonic perforation: one from complicated diverticular disease and the other from locally advanced colon cancer. The patient affected by colon cancer presented with an abscess of the iliopsoas muscle, while the patient with a perforated diverticulitis had pneumomediastinum and subcutaneous emphysema only. Aim of this report is to improve differential diagnosis based on clinical signs and radiological findings.
2. Case presentation
Case 1: A 71-year-old male patient was admitted at Emergency Department. The patient had undergone a lung biopsy for a suspected recurrence of lung cancer 7 days before. He reported pain in his left side for about 2 days with fatigue, fever, and nausea. The physical examination showed massive subcutaneous emphysema of the neck, tenderness in the left iliac fossa, and positive Blumberg sign. Blood tests showed white blood cells (WBC): 11.62 × 103/mm3; Neutrophils: 90% (10,45 ×103/mm3). The computerized tomography (CT) scan revealed pneumoperitoneum with gas in the mesosigma (Fig. 1), pneumomediastinum (Fig. 2), and subcutaneous emphysema of the neck region and of the left chest wall (Fig. 3). Wall thickening of the descending colon with edematous imbibition of peritoneal tissue and retroperitoneal abscess and signs of an acute diverticulitis with peritoneal fluid in the paracolic gutter were also observed. The emergency laparotomy revealed retroperitoneal left colonic diverticular perforation. A left hemicolectomy extending to the transverse colon, followed by a toilette and debridement of the retroperitoneum were performed. After a week, a re-laparotomy was needed from the massive necrosis of the colostomy and a right colectomy with an ileostomy were performed. Two days later the patient died of septic shock caused by Escherichia coli and Pseudomonas aeruginosa.
Figure 1.
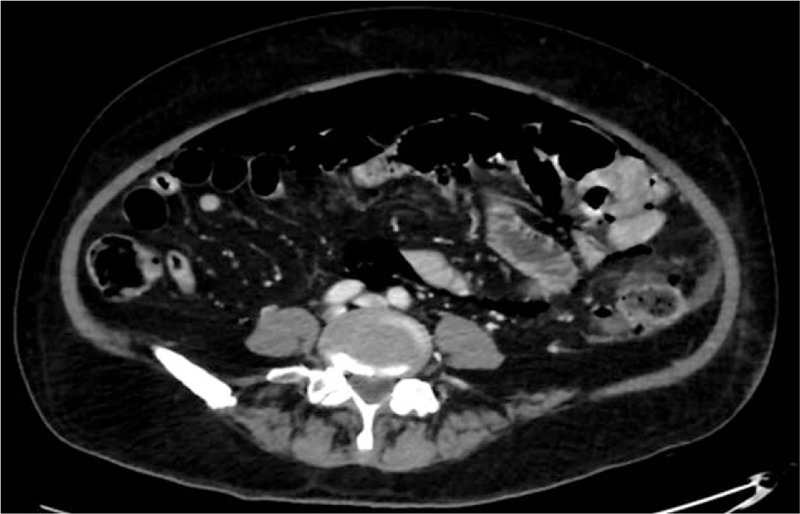
CT scan with evidence of pneumoretroperitoneum. CT = computed tomography.
Figure 2.
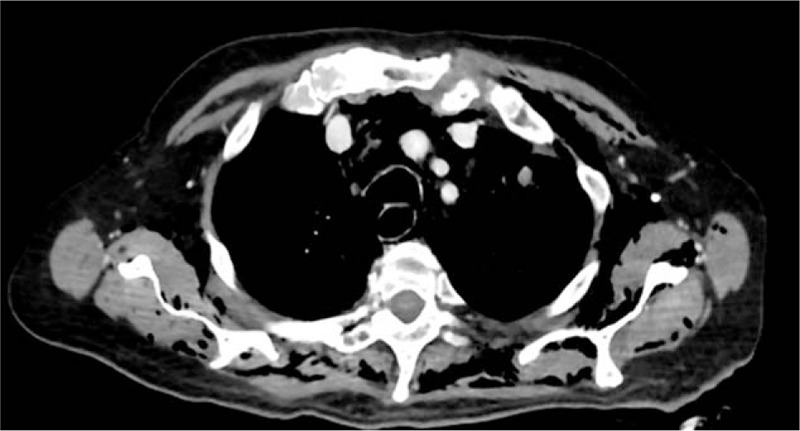
CT scan showing pneumomediastinum. CT = computed tomography.
Figure 3.
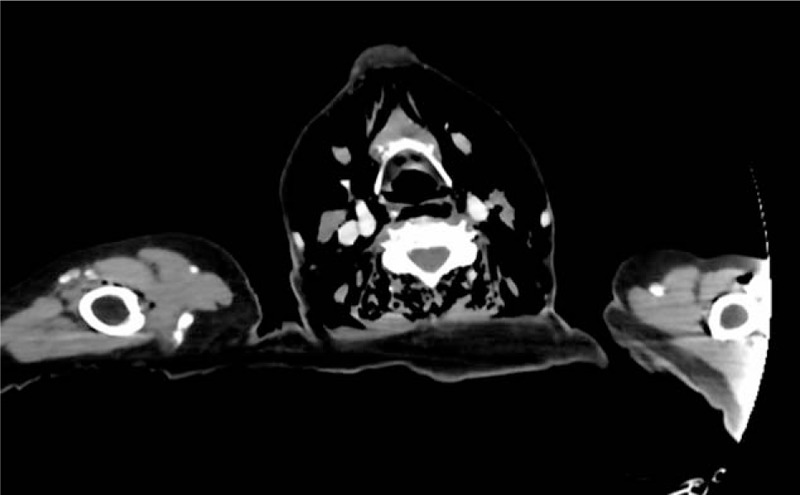
CT scan revealing subcutaneous emphysema of neck. CT = computed tomography.
Case 2: A 67- year-old man was urgently admitted to our hospital for abdominal pain associated with constipation and the presence of a left groin mass. He reported a 5-day history of left groin and lower limb pain during walking. The physical examination showed sore and painful abdomen with negative Blumberg sign and empty rectal ampulla. Blood tests showed WBC: 21.23 × 103/mm3; Neutrophils: 87.1% (16.88 × 103/mm3). The ultrasound examination of the abdomen showed the presence of fluid with thickening of the descending colon. Abdominal CT scan found thickening of the sigmoid colon in contact with the iliopsoas muscle and fluid collection (Fig. 4). An urgent laparotomy was performed. A tumor of descending colon perforating the retroperitoneum with an abscess of the iliopsoas muscle was found. A left hemicolectomy and a drainage of the abscess was performed. The patient is still alive at last follow up in August 2018.
Figure 4.
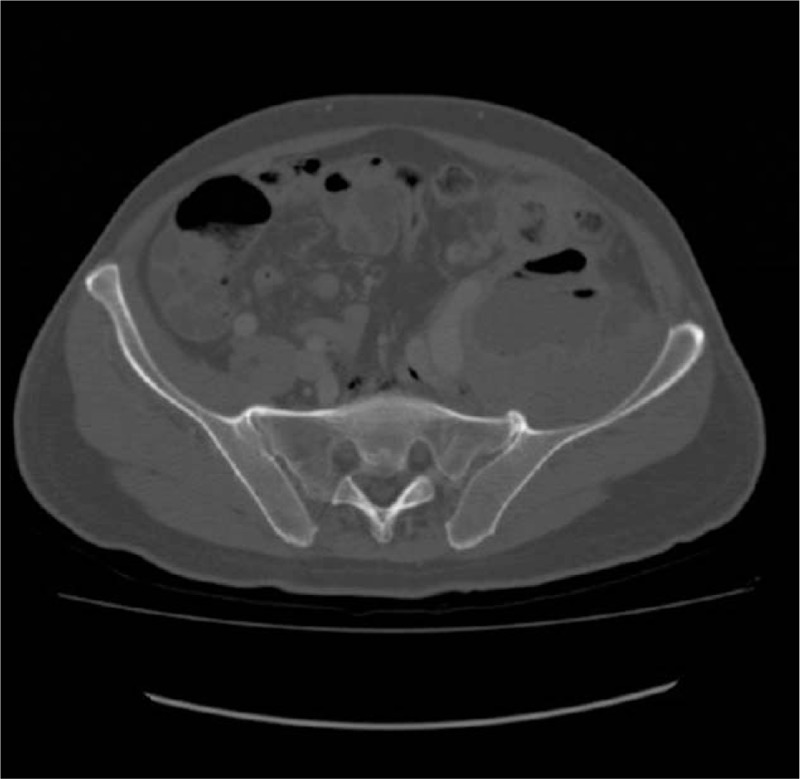
CT scan, iliopsoas abscess. CT = computed tomography.
3. Discussion
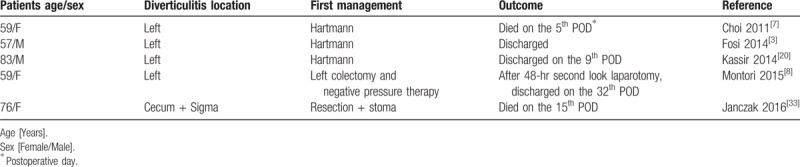
A retroperitoneal abscess from colonic perforation is an unusual event. The presence of air or pus in the soft tissues of the body represents a particular sign of retroperitoneal colonic perforation. Choi[7] reported the mechanism of the spread of abscess, gas, and necrosis along the retroperitoneum and mediastinum through the anatomic connection between regions. The anatomical site of perforation could determine the route of spread of the pus and air in the retroperitoneum.[3] In the case of necrotizing fasciitis, there is a rapid spread of the infection and gas in the tissues. In such cases, the causes of the infection are often both aerobic and anaerobic bacteria.[8] Retroperitoneal colonic perforation can be associated both with the diffusion of gases and pus into soft tissues.[7,9] Perforations of large bowel are rare but cause severe complications with overall mortality about 17%.[10] Retroperitoneal colonic perforation is a rare clinical condition, and people of any age and sex can be affected. From our experience and from the review of international literature they appear to have a higher mortality rate. In fact, in these cases the diagnosis is often delayed and patients have multiple comorbidities.[8,11] The most common cause of colonic retroperitoneal perforation is diverticular disease.[8] The incidence of perforated colon cancer ranges from 3% to 10%.[12,13] These 2 types of retroperitoneal perforations can be associated with 2 different clinical manifestations: subcutaneous emphysema with pneumomediastinum and muscle psoas abscesses. Subcutaneous emphysema, pneumomediastinum, and pneumoretroperitoneum can be manifestations of various diseases, rarely they can originate from an intra-abdominal pathology. In the literature, there are few reported cases of pneumomediastinum and subcutaneous emphysema resulting from gastrointestinal tract and are usually caused by surgical procedures.[3] Intra-abdominal causes of subcutaneous emphysema can be trauma, iatrogenic causes (high and low endoscopy),[14,15] infections (necrotizing fasciitis, Fournier gangrene, etc.) and faecaloma.[16,17] The gas diffusion in tissues follows the path of least resistance. In 1974, Meyers reported that in presence of air in the para-renal space, gas could progress from the posterior para-renal space through the diaphragm hiatus causing the pneumomediastinum and the cervical subcutaneous emphysema.[18] Thus, among the rare causes of gas in retroperitoneal tissue and in subcutaneous tissue, there are colonic perforations associated with diverticulitis. The relevant literature also describes cases of scrotal emphysema caused by gastrointestinal tract perforation.[17,19,20] Retroperitoneal abscesses with no triggering cause are rare. In the past, the most frequent retroperitoneal abscesses were the “cold” ones in tuberculosis, whereas today the “hot” ones are secondary to Crohn disease, pyelonephritis, and diverticulitis prevailed.[21] The incidence of perforation ranges from 3% to 10% of all colon cancers. Colon cancer perforation results in local infection and/or systemic sepsis. Colonic cancer usually has intraperitoneal spread and its spread in the retroperitoneal direction is relatively rare.[22] Thus, an infrequent presentation is the abscess of the psoas muscle caused by perforation of a colon cancer with an incidence estimated between 0.3% and 0.4%.[13,23] The formation of an iliopsoas abscess, secondary to a perforated colon cancer in the retroperitoneum, may also be associated with the onset of a necrotizing fasciitis, which it can quickly lead to the death of the patient.[24] There are several reports on necrotizing fasciitis due to colorectal cancer involving the abdominal wall.[25,26] This complication could be fatal especially in immunocompromised patients during chemotherapy.[24] Retroperitoneal abscesses spread is a very rare event and is relatively frequent in elderly frail patients. Our experience shows that the spread of retroperitoneal abscess in complicated colonic diverticulitis is different from those in advanced colonic cancer. Practically, in retroperitoneal abscess from colonic cancer perforation there is a spread along the iliopsoas muscle, whereas in complicated colonic diverticulitis the pus spreads toward mediastinum, thoracic wall, and neck soft tissue. Actually, the physiopathology of these different types of spread is unknown. We suggest that in complicated diverticular diseases there are pronounced and dense inflammatory fibrotic adhesions in lower left retroperitoneum near the muscle lacuna behind inguinal ligament. This extensive fibrosis prevents the spread of pus to the Scarpa triangle and it can easily diffuse to the upper abdominal and thorax wall. In contrast, in colonic cancer there is only a local invasion of the cancer in the retroperitoneum, so the pus can spread for gravity along the muscle lacuna behind the inguinal ligament to the Scarpa triangle. In elderly frail patients, the clinical sign of a retroperitoneal abscess in colonic advanced cancer can be a groin mass; on the other hand, the clinical sign of a colonic diverticular perforation into the retroperitoneum can be a subcutaneous emphysema of the neck, the chest, and the abdomen. In the review of literature, 14 papers described this rare complication (Fig. 5)—9 papers reported cases with iliopsoas abscess (Table 1)[9,13,24,27–32] and 5 reported cases with subcutaneous emphysema and pneumomediastinum (Table 2).[3,7,8,20,33] This review of the literature seems to confirm our opinion that the presentation of perforated diverticulitis in the retroperitoneum have a different evolution than retroperitoneal perforation of colon cancer.[27–35] The management of retroperitoneal abscess from visceral perforation in complicated diverticular disease is still a challenge during the common surgical treatment of colonic diverticulitis.[36–39]
Figure 5.
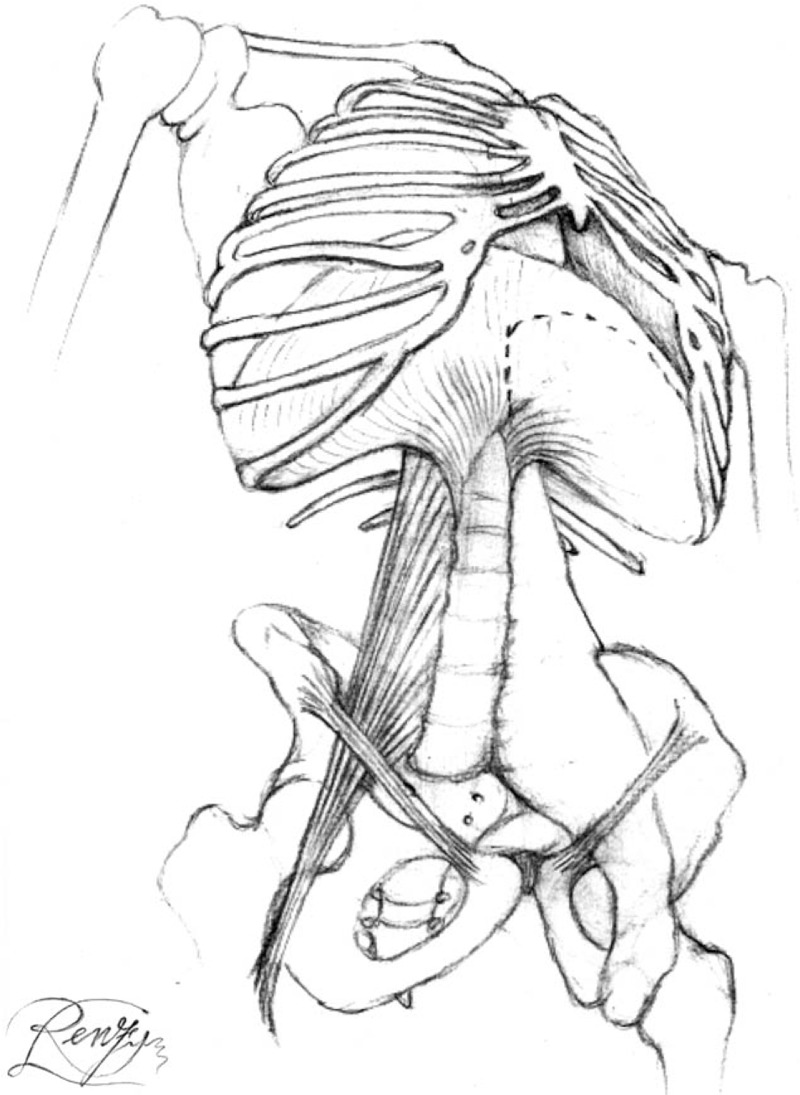
Anatomy of different retroperitoneal abscess spreading.
Table 1.
Review of literature: colon cancer complicated with psoas abscess.
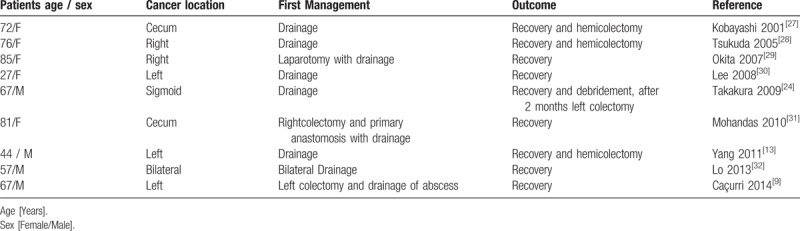
Table 2.
Review of literature: retroperitoneal perforated diverticulitis complicated with subcutaneous emphysema and pneumomediastinum.
4. Conclusions
Pneumoretroperitoneum, pneumomediastinum, and abscess of iliopsoas are rare manifestations of retroperitoneal colonic perforation with often-delayed diagnosis due to absence of peritoneal irritation. Our experience and the literature show that the spread of retroperitoneal abscess in complicated colonic diverticulitis is different from that in advanced colonic cancer. The clinical sign of a retroperitoneal abscess in colonic advanced cancer can be a groin mass, whereas in colonic diverticular perforation the subcutaneous emphysema of the neck, chest, and abdomen are more typical. For this reason, a thorough, clinical examination, and radiological studies are needed to diagnose these conditions.
Acknowledgments
The authors are the only ones responsible for the content and writing of the paper.
Author contributions
All authors contributed equally to the manuscript drafting. All authors read and approved the final manuscript.
Conceptualization: Paolo Ruscelli, Claudio Renzi, Alessandro Sanguinetti, Nicola Avenia, Georgi Popivanov, Roberto Cirocchi, Massimo Lancia, Sara Gioia, Renata Tabola.
Data curation: Paolo Ruscelli, Claudio Renzi, Andrea Polistena, Alessandro Sanguinetti, Roberto Cirocchi, Sara Gioia, Renata Tabola.
Formal analysis: Paolo Ruscelli, Claudio Renzi, Andrea Polistena, Alessandro Sanguinetti, Nicola Avenia, Georgi Popivanov, Roberto Cirocchi, Massimo Lancia, Renata Tabola.
Funding acquisition: Claudio Renzi, Nicola Avenia, Roberto Cirocchi, Massimo Lancia, Sara Gioia, Renata Tabola.
Investigation: Paolo Ruscelli, Claudio Renzi, Andrea Polistena, Alessandro Sanguinetti, Georgi Popivanov, Roberto Cirocchi, Sara Gioia, Renata Tabola.
Methodology: Paolo Ruscelli, Claudio Renzi, Nicola Avenia, Georgi Popivanov, Roberto Cirocchi, Massimo Lancia, Renata Tabola.
Project administration: Paolo Ruscelli, Claudio Renzi, Andrea Polistena, Alessandro Sanguinetti, Nicola Avenia, Georgi Popivanov, Roberto Cirocchi, Sara Gioia.
Resources: Claudio Renzi, Nicola Avenia, Roberto Cirocchi, Massimo Lancia, Renata Tabola.
Software: Paolo Ruscelli, Claudio Renzi, Alessandro Sanguinetti, Georgi Popivanov, Sara Gioia, Renata Tabola.
Supervision: Paolo Ruscelli, Claudio Renzi, Andrea Polistena, Alessandro Sanguinetti, Georgi Popivanov, Roberto Cirocchi, Massimo Lancia, Renata Tabola.
Validation: Paolo Ruscelli, Claudio Renzi, Alessandro Sanguinetti, Nicola Avenia, Georgi Popivanov, Roberto Cirocchi, Massimo Lancia, Renata Tabola.
Visualization: Paolo Ruscelli, Claudio Renzi, Alessandro Sanguinetti, Nicola Avenia, Georgi Popivanov, Roberto Cirocchi, Massimo Lancia, Sara Gioia, Renata Tabola.
Writing – original draft: Claudio Renzi, Andrea Polistena, Alessandro Sanguinetti, Georgi Popivanov, Roberto Cirocchi, Sara Gioia, Renata Tabola.
Writing – review & editing: Paolo Ruscelli, Claudio Renzi, Andrea Polistena, Alessandro Sanguinetti, Nicola Avenia, Georgi Popivanov, Roberto Cirocchi, Massimo Lancia, Sara Gioia, Renata Tabola.
Footnotes
Abbreviations: CT = computed tomography, WBC = white blood cell.
Ethics approval and consent to participate: Ethical board approval was unnecessary since this is a retrospective study. Written informed consent to participate was obtained from the patients.
Consent for publication: Written informed consent was obtained from the patients for the publication of this report.
Availability of data and materials: Not applicable.
Funding: The Fudation Cassa di Risparmio di Terni pays the publication costs of this paper.
The authors declare that they have no competing interests
References
- [1].Crepps JT, Welch JP, Orlando R. Management and outcome of retroperitoneal abscesses. Ann Surg 1987;205:276–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].O’Reilly P, Chen HK, Wiseman R. Management of extensive subcutaneous emphysema with a subcutaneous drain. Respirol Case Rep 2013;1:28–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Fosi S, Giuricin V, Girardi V, et al. Subcutaneous emphysema, pneumomediastinum, pneumoretroperitoneum, and pneumoscrotum: unusual complication of acute perforated diverticulitis. Case Rep Radiol 2014;2014:431563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Maunder RJ, Pierson DJ, Hudson LD. Subcutaneous and mediastinal emphysema. Pathophysiology, diagnosis, and management. Arch Int Med 1984;144:1447–53. [PubMed] [Google Scholar]
- [5].Edge SB, Byrd SR, Compton CC, et al. AJCC Cancer Staging Manual. Springer-Verlag, 7th editionNew York, NY: 2010. [Google Scholar]
- [6].Maglinte DDT, Pollack HM. Retroperitoneal abscess: a presentation of colon carcinoma. Gastrointest Radiol 1983;8:177–81. [DOI] [PubMed] [Google Scholar]
- [7].Choi PW. Pneumomediastinum caused by colonic diverticulitis perforation. J Korean Surg Soc 2011;80suppl:S17–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Montori G, Di Giovanni G, Mzoughi Z, et al. Pneumoretroperitoneum and pneumomediastinum revealing a left colon perforation. Int Surg 2015;100:984–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Cacurri A, Cannata G, Trastulli S, et al. A rare case of perforated descending colon cancer complicated with a fistula and abscess of left iliopsoas and ipsilateral obturator muscle. Case Rep Surg 2014;2014:128506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Bielecki K, Kamiński P, Klukowski M. Large bowel perforation: morbidity and mortality. Tech Coloproctol 2002;6:177–82. [DOI] [PubMed] [Google Scholar]
- [11].Ravo B, Khan SA, Ger R, et al. Unusual extraperitoneal presentations of diverticulitis. Am J Gastroenterol 1985;80:346–51. [PubMed] [Google Scholar]
- [12].Donaldson GA. The management of perforative carcinoma of the colon. N Engl J Med 1958;258:201–7. [DOI] [PubMed] [Google Scholar]
- [13].Yang JY, Lee JK, Cha SM, et al. Psoas abscess caused by spontaneous rupture of colon cancer. Clin Orthop Surg 2011;3:342–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Cappello M, Randazzo C, Peralta S, et al. Subcutaneous emphysema, pneumomediastinum and pneumoperitoneum after diagnostic colonoscopy for ulcerative colitis: a rare but possible complication in patient with multiple risk factors. Int J Colorectal Dis 2011;26:393–4. [DOI] [PubMed] [Google Scholar]
- [15].Marwan K, Farmer KC, Varley C, et al. Pneumothorax, pneumomediastinum, pneumoperitoneum, pneumoretroperitoneum, and subcutaneous emphysema following diagnostic colonoscopy. Ann R Coll Surg Engl 2007;89:W20–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Brunet C, Thomas P, Sielezneff I, et al. Subcutaneous cervical emphysema: complication of constipation. Review of the literature. J Chir 1995;132:198–200. [PubMed] [Google Scholar]
- [17].Arana-Arri E, Cortés H, Cabriada V, et al. Giant fecaloma causing perforation of the rectum presented as a subcutaneous emphysema, pneumoperitoneum and pneumomediastinum: a case report. Eur J Emerg Med 2007;14:351–3. [DOI] [PubMed] [Google Scholar]
- [18].Meyers MA. Radiological features of the spread and localization of extraperitoneal gas and their relationship to its source: an anatomical approach. Radiology 1974;111:17–26. [DOI] [PubMed] [Google Scholar]
- [19].Mirzayan R, Cepkinian V, Asensio JA. Subcutaneous emphysema, pneumomediastinum, pneumothorax, pneumopericardium and pneumoperitoneum from rectal barotrauma. J Trauma 1996;41:1073–5. [DOI] [PubMed] [Google Scholar]
- [20].Kassir R, Abboud K, Dubois J, et al. Perforated diverticulitis of the sigmoid colon causing a subcutaneous emphysema. Int J Surg Case Rep 2014;5:1190–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Martino A, Catuogno F, Festaetal P. Retroperitonealabscess by suppurative psoas. Case report. Ann Ita di Chir 2008;79:377–82. [PubMed] [Google Scholar]
- [22].Costa G, Ruscelli P, Balducci G, et al. Clinical strategies for the management of intestinal obstruction and pseudo-obstruction. A Delphi Consensus study of SICUT (Società Italiana di Chirurgia d’Urgenza e del Trauma). Ann Ital Chir 2016;87:105–17. [PubMed] [Google Scholar]
- [23].Alvi AR, Ur Rehman Z, Nabi ZU. Pyogenic psoas abscess: case series and literature review. Trop Doct 2010;40:56–8. [DOI] [PubMed] [Google Scholar]
- [24].Takakura Y, Ikeda S, Yoshimitsu M, et al. Retroperitoneal abscess complicated with necrotizing fasciitis of the thigh in a patient with sigmoid colon cancer. World J Surg Oncol 2009;7:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Ku HW, Chang KJ, Chen TY, et al. Abdominal necrotizing fasciitis due to perforated colon cancer. J Emerg Med 2006;30:95–6. [DOI] [PubMed] [Google Scholar]
- [26].Marron CD, McArdle GT, Rao M, et al. Perforated carcinoma of the caecum presenting as necrotising fasciitis of the abdominal wall, the key to early diagnosis and management. BMC Surg 2006;6:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Kobayashi H, Sakurai Y, Shoji M, et al. Psoas abscess and cellulitis of the right gluteal region resulting from carcinoma of the cecum. J Gastroenterol 2001;36:623–8. [DOI] [PubMed] [Google Scholar]
- [28].Tsukuda K, Ikeda E, Miyake T, et al. Abdominal wall and thigh abscess resulting from the penetration of ascending colon cancer. Acta Med Okayama 2005;59:281–3. [DOI] [PubMed] [Google Scholar]
- [29].Okita A, Kubo Y, Tanada M, et al. Unusual abscesses associated with colon cancer: report of three cases. Acta Med Okayama 2007;61:107–13. [DOI] [PubMed] [Google Scholar]
- [30].Lee KN, Lee HL, Yoon JH, et al. A case of mucinous adenocarcinoma of the colon presenting with psoas abscess. Korean J Gastroenterol 2008;52:120–3. [PubMed] [Google Scholar]
- [31].Mohandas SK, Mazarello F, Bisset R. Right gluteal abscess: an unusual presentation of perforated caecal adenocarcinoma. J Gastrointest Canc 2010;41:285–7. [DOI] [PubMed] [Google Scholar]
- [32].Lo CH, Yang YS, Ho CL. Rectal adenocarcinoma with bilateral psoas muscle abscess: case report and review of the literature. J Med Sci 2013;33:225–7. [Google Scholar]
- [33].Janczak D, Ziomek A, Dorobisz T, et al. Subcutaneous emphysema of the neck, chest, and abdomen as a symptom of colonic diverticular perforation into the retroperitoneum. Kardiochir Torakochirurgia Pol 2016;13:55–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Aghayev E, Yen K, Sonnenschein M, et al. Pneumomediastinum and so tissue emphysema of the neck in postmortem CT and MRI; a new vital sign in hanging? Forensic Sci Int 2004;153:181–8. [DOI] [PubMed] [Google Scholar]
- [35].Rees JR, Burgess P. Conservative management of complex diverticular disease causing a retroperitoneal perforation. BMJ Case Rep. doi:10.1136/bcr.03.2009.1692. [published ahead of print October 5, 2009]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Cirocchi R, Cesare Campanile F, Di Saverio S, et al. Laparoscopic versus open colectomy for obstructing right colon cancer: a systematic review and meta-analysis. J Visc Surg 2017;154:387–99. [DOI] [PubMed] [Google Scholar]
- [37].Abraha I, Binda GA, Montedori A, et al. Laparoscopic versus open resection for sigmoid diverticulitis. Cochrane Database Syst Rev 2017;11:CD009277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Cirocchi R, Afshar S, Shaban F, et al. Perforated sigmoid diverticulitis: Hartmann's procedure or resection with primary anastomosis-a systematic review and meta-analysis of randomised control trials. Tech Coloproctol. doi: 10.1007/s10151-018-1819-9. [published ahead of print July 11, 2018]. [DOI] [PubMed] [Google Scholar]
- [39].Cirocchi R, Fearnhead N, Vettoretto N, et al. The role of emergency laparoscopic colectomy for complicated sigmoid diverticulits: a systematic review and meta-analysis. Surgeon. doi: 10.1016/j.surge.2018.08.010 [published ahead of print October 9, 2018]. [DOI] [PubMed] [Google Scholar]


