Abstract
To compare the clinical outcomes of 2 procedures, closed or mini-open reduction with percutaneous pinning (ORPP), for the treatment of supracondylar fractures of the humerus in children.
Patients aged less than 15 years who had undergone surgery for supracondylar fracture of the humerus between 2004 and 2013 were identified. The case records and radiographs from 34 patients were reviewed. Twenty-one patients had undergone closed reduction followed by percutaneous pinning (CRPP), while 13 had undergone mini-open reduction through the anterior approach with percutaneous pinning (mini-ORPP). The average age of the patients at the time of surgery was 5.4 (1–13) years in the CRPP group and 5.4 (2–9) years in the mini-ORPP group. The average age of the patients at the time of surgery was 5.4 (1–13) years in the CRPP group and 5.4 (2–9) years in the mini-ORPP group. Based on the Gartland classification system, the CRPP group included 12 type 2 and 9 type 3 fractures, while the mini-ORPP group included 4 type 2 and 9 type 3 fractures. The average postoperative follow-up duration was 8 (3–21) months in the CRPP group and 10 (3–10) months in the mini-ORPP group. The investigated parameters were postoperative complications, radiographic evaluation, and clinical evaluation, including range of motion (ROM) and Flynn's criteria. To evaluate the deformity of the humerus, Baumann's angle and the carrying angle (CA) were calculated on anteroposterior radiographs.
Although no patient showed loss of reduction, deep infection, or neurovascular complications, 1 patient in the CRPP group had a cubitus varus deformity. The average CA loss in the injured elbow compared with the CA of the contralateral side was significantly larger in the CRPP group than the mini-ORPP group. In accordance with Flynn's criteria, the results in the CRPP group were excellent in 12 patients, good in 8, and poor in 1; the results in the mini-ORPP group were excellent in 12, and good in 1.
To eliminate the possibility of postoperative cubitus varus deformity, the mini-ORPP is the optimal procedure for supracondylar fracture of the humerus in children.
Keywords: children, closed reduction, comparative study, elbow, mini-open reduction, supracondylar fracture of the humerus
1. Introduction
Supracondylar fracture of the humerus is the most common elbow injury in children.[1,2] Most of these fractures are treated with closed reduction followed by percutaneous pinning (CRPP);[1,3] however, the clinical outcome is occasionally deteriorated by postoperative complications such as cubitus varus deformity, restricted range of motion (ROM), pin tract infection, or neurovascular disturbance.[3–5] Cubitus varus deformity is the most common residual deformity after supracondylar fracture of the humerus in children.[3–5] Cubitus varus deformity is caused by residual internal rotation and/or medial displacement of the fracture fragment due to the failure of anatomical reduction.[3,6,7] The cause of failure of anatomical reduction is usually due to the entrapment of structures between the fracture fragments; these trapped structures include the brachialis muscle, joint capsule, and neurovascular bundle.[8–10]
Open reduction with percutaneous pinning (ORPP) is an accepted treatment option for open, severely displaced, irreducible, and neglected fractures of the distal humerus.[3,5,8–16] When failure of anatomical reduction occurs due to structures being caught between the fracture fragments, ORPP provides precise anatomical reduction by enabling the direct removal of the trapped structures.[8,9] However, ORPP reportedly results in several complications, including a higher risk of infection than in closed reduction, restriction of ROM, and possible unsightly and/or painful scarring.[8,12,14,16] To prevent complications due to conventional ORPP, ORPP using a miniature incision in the anterior cubital skin crease (mini-open reduction through the anterior approach with percutaneous pinning [mini-ORPP]) has been reported.[17,18] Mini-ORPP also reportedly results in a satisfactory clinical outcome for supracondylar fracture of the humerus in children.[18] However, no study has yet compared the radiological evaluations of CRPP versus mini-ORPP. In the present study, the clinical results and radiographic changes were compared between 2 treatment groups (CRPP and mini-ORPP), and the cause of the occurrence of cubitus varus deformity is discussed.
2. Methods
This retrospective case series evaluated pediatric patients aged less than 15 years who underwent surgery for displaced supracondylar fracture of the humerus between April 2004 and March 2013 in our institution and related hospitals. Demographic, medical history, imaging, and follow-up data were extracted from the medical records. The present study was a retrospective, human, non-interventional study. Public Health Japanese Law states that human, non-interventional studies do not require approval from an institutional review board. However, in accordance with ethical considerations, informed consent was obtained from both the guardians and the patients themselves who were selected for inclusion in the present study. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki.
2.1. Patients
We retrospectively reviewed pediatric patients aged less than 15 years who underwent surgery for displaced supracondylar fracture of the humerus. The mean age at the time of surgery was 5.4 ± 2.9 (range 1–14) years. Supracondylar fractures were defined in accordance with the Gartland classification system, which divides fractures into 3 types based on the degree of displacement; type 1: undisplaced, type 2: displaced with an intact posterior cortex, and type 3: displaced with no cortical contact. We excluded patients with Gartland type 1 (non-displaced) fracture with associated bony injuries in the ipsilateral limb, and those with incomplete data. Patients were included if they were followed up postoperatively for at least 3 months.
The patient characteristics are shown in Table 1. Twenty patients were male (59%) and 14 were female (41%). The fractured elbow was the left in 16 (47%) patients and the right in 18 (53%). From 2004 to 2007, closed reduction with percutaneous pinning (CRPP) had performed, but postoperative varus deformity was observed in a patient. Therefore, since 2008, mini-ORPP had performed. Based on the procedure performed, the patients were divided into 2 groups: the CRPP group (n = 21), and the mini-ORPP group (n = 13). Preoperative neurological disturbance occurred in 3 of 21 patients in the CRPP group (affecting the radial nerve in 2, and the ulnar nerve in 1), and 5 of 13 patients in the mini-ORPP group (affecting the radial nerve in 2, the median nerve in 1, and the ulnar nerve in 2). There were no significant differences between groups regarding age, sex, affected side, interval between injury and surgery, follow-up duration, Gartland classification, and preoperative neurological disturbance.
Table 1.
Demographic data for pediatric patients with displaced supracondylar fractures of the humerus.

2.2. Surgical procedures
Surgery was performed under general anesthesia by a hand surgeon in all 34 patients. The CRPP group were in the prone or lateral position intraoperatively and underwent closed reduction using a reduction bar, followed by percutaneous pinning. The surgeon applied traction to the limb with elbow flexion using a traction bar while the assistant applied counter-traction to the distal humerus (Fig. 1A). The mini-ORPP group were in the supine position intraoperatively and underwent mini-open reduction via the anterior approach followed by percutaneous pinning. The anterior approach through a 2.5 cm incision in the anterior cubital crease was used for the mini-open reduction. The surgeon used a finger to remove the structures that were caught between the fracture fragments and then applied traction to the limb with the elbow extended and maintained the alignment of the fracture fragment with the left thumb while the assistant flexed the patient's elbow (Fig. 1B). For percutaneous pinning, the surgeon confirmed that the fracture was appropriately reduced, and then percutaneously inserted 2 or 3 crossed Kirschner wires into the distal humerus under visualization using an X-ray image intensifier. After percutaneous pinning, the Baumann's angle (BA) was measured on both perioperative radiography and the image intensifier, and anatomical fracture reduction was confirmed.
Figure 1.
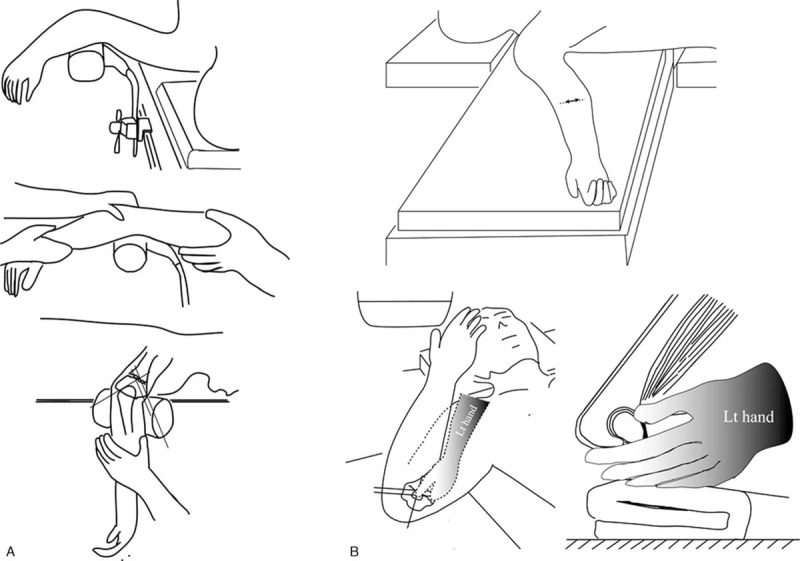
Illustrations demonstrating the 2 different operative procedures used to treat supracondylar fracture of the humerus in pediatric patients. (A) Closed reduction with percutaneous pinning. Closed reduction was performed using a reduction bar, followed by percutaneous pinning with the patient in prone or lateral position. The surgeon applied traction to the limb with elbow flexion on the traction bar while the assistant applied counter-traction to the distal humerus. Percutaneous pinning was then performed after anatomical reduction was obtained. (B) Mini-open reduction through the anterior approach with percutaneous pinning. Open reduction was performed via the anterior approach, followed by percutaneous pinning with the patient in supine position. The anterior approach was used through an incision (2.5 cm) in the anterior cubital crease. After using the surgeon's finger to remove the structures caught between fracture fragments, the surgeon applied traction to the limb with elbow extension and maintained the alignment of the fracture fragments with the left thumb while the assistant flexed the elbow of the patient. Percutaneous pinning was then performed after anatomical reduction was obtained.
In all patients, the wires were bent back and left unburied on the skin to enable wire removal in the outpatient clinic. A long arm fiberglass cast with the elbow flexed at 90° was used in all patients for 4 weeks, after which the wires were removed in the outpatient clinic.
2.3. Postoperative evaluation
Radiographic imaging evaluation, ROM of the elbow joint, and postoperative complications (iatrogenic nerve injuries, infection, and cubitus valgus or varus deformity) were investigated. The BA and the carrying angle (CA) were calculated on anteroposterior radiographs to evaluate the deformity of the humerus.[19] Postoperative cosmetic and functional outcomes were assessed using the clinical criteria described by Flynn et al,[20] which involves evaluation of the elbow ROM and the CA (Table 2).
Table 2.
Flynn's criteria results for pediatric patients with supracondylar fractures of the humerus.

2.4. Statistic analysis
All statistical analyses were carried out using SPSS 18 software (SPSS Inc., Chicago, IL). Data are displayed as mean ± standard deviation. Continuous normally-distributed variables were compared using Welch t test, while continuous non-normally distributed variables were compared using the Mann–Whitney U test. The Fisher exact test was used for the comparison of 2 independent groups. Differences among categorical variables were analyzed using the chi-squared test. P values less than .05 were considered statistically significant.
3. Results
Radiographic evaluations, ROM, Flynn's criteria, and the incidence of cubitus valgus deformity are shown in Table 3.
Table 3.
Radiographic evaluations, ROM, Flynn's criteria, and the incidence of cubitus varus deformity.

3.1. Radiographic evaluation
There was no significant difference between the 2 groups in the BA of the unaffected elbow; however, compared with the mini-ORPP group, the CRPP group had a significantly larger BA of the injured elbow (P =.006), and a significantly larger increase in the BA of the affected elbow compared with the contralateral elbow (P =.003).
There was no significant difference between the 2 groups in the CA of the unaffected elbow and the CA of the injured elbow; however, compared with the mini-ORPP group, the CRPP group had a significantly greater loss of CA in the affected elbow compared with the contralateral elbow (P =.016).
3.2. Elbow ROM at final follow-up
There were no significant differences between groups in the ROM (Arc) of the injured elbow (P =.13, Table 3). In accordance with Flynn's criteria, the outcomes in the CRPP group were excellent in 12, good in 8, and poor in 1, while the outcomes in the mini-ORPP group were excellent in 12 and good in 1. There were no significant differences between the 2 groups in the incidences of excellent and good outcomes (P =.83, Table 3), or cubitus varus deformity (P =.83, Table 3). There were also no significant differences between groups in the distribution of the outcome in accordance with Flynn’ criteria (Table 4).
Table 4.
Clinical outcomes based on Flynn's criteria in the CRPP and mini-ORPP groups.

3.3. Complications
All preoperative nerve injures completely resolved spontaneously within 4 months in both groups. Although no patients experienced postoperative fracture displacement, pin tract infection, or neurovascular disturbance, 1 patient in the CRPP group had cubitus varus deformity.
4. Discussion
The present study compared and evaluated the clinical results and radiographic changes after treatment of supracondylar fracture of the humerus in pediatric patients via either the CRPP or the mini-ORPP. Regarding radiographic evaluation, the CRPP group had a significantly greater BA of the injured elbow, greater increase in the BA of the injured elbow compared with the contralateral elbow, and greater loss of CA in the injured elbow compared with the contralateral elbow than the mini-ORPP group; these results indicate that the CRPP group had a greater degree of postoperative varus deformity of the injured elbow than the mini-ORPP group.
Perioperative measurement of the BA must be performed to minimize the risk of cubitus varus deformity; however, it is reportedly difficult to detect rotational displacement using an X-ray image intensifier.[6] In our study, to eliminate uncertainty regarding the detection of rotational displacement, the BA after fixation was measured using both perioperative radiographs and an image intensifier, and the anatomical reduction of the fractures was confirmed. Nevertheless, the CRPP group had a significantly greater BA and smaller CA in the injured elbow compared with the contralateral elbow at the last follow-up radiological evaluation; this increase in the BA and decrease in the CA indicate that anatomical reduction was not obtained, and that fracture displacement remained. Thus, the detection of rotational displacement using radiographic examination is difficult, if not impossible. Relying on radiographic examination to detect rotational displacement will inevitably lead surgeons to overlook the failure of anatomical reduction of supracondylar fracture. In contrast, the mini-ORPP group had a negligible loss of CA, with the postoperative CA of the injured elbow being almost the same as that of the contralateral elbow; this indicates that mini-ORPP provides anatomical reduction of supracondylar fractures of the humerus. The reason anatomical reduction was obtained in almost all patients in the mini-ORPP group could be due to the following 2 reasons. First, mini-ORPP enabled precise reduction due to the removal of the inhibitory structures between the fracture fragments. Second, manual reduction with the surgeon's thumb enabled detection of fracture displacement and maintenance of anatomical reduction.
Although ORPP is an accepted treatment for severely displaced, irreducible, and neglected fractures of the distal humerus, the open procedure reportedly has several complications, including a relatively greater risk of infection and ROM limitation compared with the closed procedure, and possible unsightly and/or painful scarring.[8,12,14,16] However, the present results showed no harmful effects of open reduction, and there were no significant differences between the CRPP and mini-ORPP groups in terms of complications and the postoperative ROM of the elbow. Moreover, our study showed that the scars resulting from fracture treatment via the anterior approach through the cubital crease provided a high degree of cosmetic satisfaction from the patients. We believe that our results support the first-line use of the mini-ORPP procedure, as it is cosmetically and functionally satisfactory, and is less invasive than standard ORPP.
The present study had some limitations. The main limitation is the retrospective design, which is susceptible to bias compared with a prospective design. Although there was no difference between the 2 groups regarding patient background, a prospective randomized study is generally the ideal research method. However, the current study clearly showed that the mini-ORPP-group achieved anatomical reduction compared with the contralateral side, while the CRPP group had inadequate reduction. Therefore, conducting a prospective, randomized study for the treatment of supracondylar fracture of the humerus in children is ethically inappropriate. Another limitation is the small sample size and short follow-up duration. Although the average follow-up in our study was 10 months, the minimum follow-up period was only 3 months. We believe that a longer follow-up duration would not change the results in most patients, but the increased BA or decreased CA might affect the alignment of the limb over the long-term. Therefore, longer follow-up periods are required to evaluate late deformity of the injured elbow.
5. Conclusion
To eliminate the possibility of postoperative cubitus varus deformity, mini-ORPP is an optimal procedure for the treatment of supracondylar fracture of the humerus in children.
Acknowledgments
We thank Kelly Zammit, BVSc, from Edanz Group (www.edanzediting.com/ac), for editing a draft of this manuscript.
Author contributions
Data curation: Yuji Tomori.
Formal analysis: Yuji Tomori.
Investigation: Yuji Tomori.
Methodology: Yuji Tomori.
Project administration: Yuji Tomori.
Supervision: Mitsuhiko Nanno, Shinro Takai.
Writing – original draft: Yuji Tomori.
Writing – review & editing: Mitsuhiko Nanno.
Footnotes
Abbreviations: BA = Baumann's angle, CA = carrying angle, CRPP = closed reduction followed by percutaneous pinning, mini-ORPP = mini-open reduction through the anterior approach with percutaneous pinning, ORPP = open reduction with percutaneous pinning, ROM = range of motion.
The authors have no conflicts to declare.
The author(s) of this work have nothing to disclose.
References
- [1].Mitchelson AJ, Illingworth KD, Robinson BS, et al. Patient demographics and risk factors in pediatric distal humeral supracondylar fractures. Orthopedics 2013;36:e700–706. [DOI] [PubMed] [Google Scholar]
- [2].Landin LA, Danielsson LG. Elbow fractures in children. An epidemiological analysis of 589 cases. Acta Orthop Scand 1986;57:309–12. [DOI] [PubMed] [Google Scholar]
- [3].Howard A, Mulpuri K, Abel MF, et al. The treatment of pediatric supracondylar humerus fractures. J Am Acad Orthop Surg 2012;20:320–7. [DOI] [PubMed] [Google Scholar]
- [4].Labelle H, Bunnell WP, Duhaime M, et al. Cubitus varus deformity following supracondylar fractures of the humerus in children. J Pediatr Orthop 1982;2:539–46. [DOI] [PubMed] [Google Scholar]
- [5].Mehlman CT, Crawford AH, McMillion TL, et al. Operative treatment of supracondylar fractures of the humerus in children: the Cincinnati experience. Acta Orthop Belg 1996;62suppl 1:41–50. [PubMed] [Google Scholar]
- [6].Sawaizumi T, Takayama A, Ito H. Surgical technique for supracondylar fracture of the humerus with percutaneous leverage pinning. J Shoulder Elbow Surg 2003;12:603–6. [DOI] [PubMed] [Google Scholar]
- [7].Kim TJ, Sponseller PD. Pediatric supracondylar humerus fractures. J Hand Surg Am 2014;39:2308–11. [DOI] [PubMed] [Google Scholar]
- [8].Manandhar RR, Lakhey S, Pandey BK, et al. Open reduction and internal fixation of supracondylar fractures of the humerus: revival of the anterior approach. JNMA J Nepal Med Assoc 2011;51:67–71. [PubMed] [Google Scholar]
- [9].Reitman RD, Waters P, Millis M. Open reduction and internal fixation for supracondylar humerus fractures in children. J Pediatr Orthop 2001;21:157–61. [PubMed] [Google Scholar]
- [10].Wilkins KE. Changes in the management of monteggia fractures. J Pediatr Orthop 2002;22:548–54. [PubMed] [Google Scholar]
- [11].Walmsley PJ, Kelly MB, Robb JE, et al. Delay increases the need for open reduction of type-III supracondylar fractures of the humerus. J Bone Joint Surg Br 2006;88:528–30. [DOI] [PubMed] [Google Scholar]
- [12].Ersan O, Gonen E, İlhan RD, et al. Comparison of anterior and lateral approaches in the treatment of extension-type supracondylar humerus fractures in children. J Pediatr Orthop B 2012;21:121–6. [DOI] [PubMed] [Google Scholar]
- [13].Schmid T, Joeris A, Slongo T, et al. Displaced supracondylar humeral fractures: influence of delay of surgery on the incidence of open reduction, complications and outcome. Arch Orthop Trauma Surg 2015;135:963–9. [DOI] [PubMed] [Google Scholar]
- [14].Sibly TF, Briggs PJ, Gibson MJ. Supracondylar fractures of the humerus in childhood: range of movement following the posterior approach to open reduction. Injury 1991;22:456–8. [DOI] [PubMed] [Google Scholar]
- [15].Yaokreh JB, Gicquel P, Schneider L, et al. Compared outcomes after percutaneous pinning versus open reduction in paediatric supracondylar elbow fractures. Orthop Traumatol Surg Res 2012;98:645–51. [DOI] [PubMed] [Google Scholar]
- [16].Aronson DC, Meeuwis JD. Anterior exposure for open reduction of supracondylar humeral fractures in children: a forgotten approach. Eur J Surg 1994;160:263–6. [PubMed] [Google Scholar]
- [17].Tomori Y, Sawaizumi T, Nanno M, et al. A case report: distal humeral diaphyseal fracture in a child. Medicine (Baltimore) 2017;96:e5812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Suh SW, Oh CW, Shingade VU, et al. Minimally invasive surgical techniques for irreducible supracondylar fractures of the humerus in children. Acta Orthop 2005;76:862–6. [DOI] [PubMed] [Google Scholar]
- [19].Goldfarb CA, Patterson JM, Sutter M, et al. Elbow radiographic anatomy: measurement techniques and normative data. J Shoulder Elbow Surg 2012;21:1236–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Flynn JC, Matthews JG, Benoit RL. Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years’ experience with long-term follow-up. J Bone Joint Surg Am 1974;56:263–72. [PubMed] [Google Scholar]


