Abstract
HIV status disclosure is a key support strategy to start and maintain HIV care and treatment and to reduce HIV transmission. We explored the patterns and correlates of disclosure and described the effectiveness of nurse-facilitated disclosure among HIV-infected mothers of infants in coastal Tanzania. We enrolled 400 HIV positive women in an observational longitudinal study in 2011, interviewed them about maternal sociodemographic and economic characteristics, maternal and child health and history of HIV disclosure experiences and offered nurse-facilitated HIV disclosure at enrolment or at follow-up 1 month later. Mothers frequently disclosed their status to husbands and/or female relatives and experienced predominantly positive reactions. Economically vulnerable women disclosed more often to elderly female relatives, indicating that Infant and Young Child Feeding counselling given to HIV positive women should garner the support of elderly female relatives for implementing appropriate feeding practices. Nurse-facilitated disclosure was feasible in this low resource setting and was used by patients to help them with both first-time disclosure and disclosure to new persons.
INTRODUCTION
HIV status disclosure is a key support strategy to start and maintain HIV care and treatment (Ostermann et al., 2015) and to reduce horizontal (Medley, Bachanas, Grillo, Hasen, & Amanyeiwe, 2015) and vertical transmission (World Health Organisation, 2010). People living with HIV generally disclose their HIV status gradually (Norman, Chopra, & Kadiyala, 2007) and to an increasing number of people over time (Antelman et al., 2001; Maman, van Rooyen, & Groves, 2014). In sub-Saharan Africa (SSA), many women learn they have HIV when they are tested in a Prevention of Mother to Child Transmission (PMTCT) program (UNAIDS, 2014). These women must balance the risks and benefits of disclosure at a time when their pregnancy makes them biologically and socio-economically vulnerable and their HIV positivity puts them in acute need of support to be able to adhere to PMTCT guidelines, maintain their own health and protect their partner. Pregnant women in SSA disclose most often to their partners and family members (Tam, Amzel, & Phelps, 2015). HIV disclosure increases adherence to ARV prophylaxis for PMTCT (Gourlay, Birdthistle, Mburu, Iorpenda, & Wringe, 2013; Spangler, Onono, Bukusi, Cohen, & Turan, 2014), possibly mediated through increased social, practical and material support (Obermeyer, Baijal, & Pegurri, 2011) and through reduced depression (Byakika-Tusiime et al., 2009; Kaaya et al., 2013). Findings are contradictory for the role of disclosure in adherence to infant feeding guidelines (Onono, Cohen, Jerop, Bukusi, & Turan, 2014; Sibeko, Coutsoudis, Nzuza, & Gray-Donald, 2009; Williams et al., 2015). Disclosure may also have negative consequences, including divorce, withdrawal of financial support or intimate partner violence (IPV) (Neuman et al., 2013), especially in communities with high levels of stigma (Hardon et al., 2013).
A close collaboration between patients and their families, treatment supporters and primary health care providers is needed to optimize outcomes for the chronically ill, such as HIV patients (WHO, 2002). Patient peer support groups have been shown to improve disclosure rates, retention in care and quality of life and reduce morbidity and mortality of PLHIV (Bateganya, Amanyeiwe, Roxo, & Dong, 2015). Health workers are able to facilitate disclosure in couple counselling settings (Kairania et al., 2010), and as part of combined IPV reduction and HIV testing programs (Kennedy, Haberlen, Amin, Baggaley, & Narasimhan, 2015). Less is known on how health workers can support HIV disclosure in PMTCT programs (13,23), including for women fearing or experiencing IPV (Kennedy et al., 2015).
Because of these gaps in evidence, we explored the patterns and correlates of disclosure and described the effectiveness of nurse-facilitated disclosure among HIV-infected mothers of infants in coastal Tanzania. Specifically, we analyzed how the socio-demographic, economic and clinical characteristics of a mother-child dyad were associated with HIV disclosure to family members and we analyzed the experienced consequences of disclosure. Lastly, we developed and implemented a nurse-led role-play-based counseling script to assist a woman to disclose her HIV+ status to one or more persons of her choice, and measured whether she subsequently disclosed and to whom.
METHODS
Setting
The study took place in government-owned Chalinze Health Center (CHC), Bagamoyo District Hospital (BDH) and Tumbi Regional Hospital (TRH) in Pwani region, Tanzania. TRH serves a peri-urban population, CHC and BDH have rural patient populations. These sites represent the three health service levels at which the majority of HIV care and treatment (CTC) is given. The prevalence of HIV infection among women of reproductive age in the region was 9.2% in 2011/12 (Tanzania Commission for AIDS (TACAIDS), Zanzibar AIDS Commission (ZAC) & Statistics (NBS), Office of the Chief Government Statistician (OCGS), 2013).
Study design, population and data collection
This observational longitudinal study between June and December 2011 invited women attending postnatal care or HIV CTC services to enroll when they came for a routine clinic visit. HIV-positive women were eligible if they were 18 years or older, had a child < 18 months old, had access to a mobile phone in order to receive calls during the one month study period, and were willing to return to the clinic for a follow-up visit one month later.
Detailed study procedures are described elsewhere (Williams et al., 2015). Briefly, trained nurses obtained written informed consent and performed a structured interview on maternal socio-demographic and economic characteristics, maternal and child health and a history of HIV disclosure experiences. Household food insecurity in the 30 days prior to enrolment and its sub-category, household hunger, were measured using the 9 item Household Food Insecurity Access Scale (Coates, Swindale, & Bilinsky, 2007) and 3 item Household Hunger Scale tool, respectively (Deitchler, Ballard, Swindale, & Coates, 2010). House construction materials and asset ownership were measured to estimate household wealth. Activities at enrolment took approximately 1.5 hours and women received monetary compensation for their time (~ 1US dollar). Women returning for the follow-up visit one month after enrollment received ~ 3 USD for transportation.
Facilitation of disclosure
At the enrolment visit, study nurses offered all mothers facilitated disclosure according to a standardized counseling script, i.e. mothers were asked whether they wished to disclose their HIV status to another person, either at this visit (if they came with a supporter) or at the follow-up visit. The nurse further explained the process and benefits of disclosure facilitation, followed by role play in which the mother practiced disclosing her status to the person of her choice. After the mother actually shared her status, the nurse facilitated a discussion about knowledge of HIV/AIDS, including transmission, prevention and how the supporter could help her patient to reach the best health status for herself and her child. Supporters coming for the follow-up visit received ~ 3 USD for transportation.
Variable definitions
We defined disclosure as having told a person about one’s HIV positive status, i.e. active disclosure. Reasons for non-disclosure and experiences after disclosure were asked with open-ended questions. Correlates of disclosure assessed were study site, mother’s age, education level and wealth, relationship status to the father of the child, child’s age, child’s HIV test status, household food insecurity as a continuous variable, and household hunger as a binary variable: little to no hunger, or moderate to severe hunger.
Data analysis
We conducted all analyses using Stata version 13 (StataCorp. 2013). An asset-based wealth variable was constructed as previously described (Williams et al., 2015). Categorical variables were described as frequencies and continuous variables as mean and standard deviation. We tested the bivariate associations between disclosure and its associates using Fisher’s exact tests and t-tests (alpha = 0.05). We then created three logistic regression models of disclosure: to partner, mother and mother-in-law. A priori covariates included study site, mother’s education, relationship status to child’s father, child’s age, child’s HIV test status and result, household food insecurity and household hunger. Household wealth was correlated with household food insecurity. The latter was chosen as a potential covariate, because it had fewer missing values and probably represents a more current indicator of wealth. We tested theoretically plausible two-way interactions and used stepwise forward model building, adding covariates until model fit no longer improved as assessed with the likelihood-ratio test. The final models’ explanatory capacity was assessed by the area under ROC curve (AUC) measure.
EG translated text responses to the question about disclosure experiences from Swahili into English, coded the responses using the framework method (Gale, Heath, Cameron, Rashid, & Redwood, 2013) and broadly grouped them as “positive” and “negative” experiences. Those experiences that could not be unambiguously labeled as positive or negative were grouped as “other” experiences. Because some women experienced multiple consequences or reactions, the classification of one person’s experience could fall in multiple groups.
Ethical approval
The institutional review boards at the University of California, Davis and the Ifakara Health Institute (IHI), Tanzania, the Tanzanian National Research Ethics Committee and the Tanzanian Commission for Science and Technology approved the study. All women gave written informed consent for participation.
RESULTS
Participant characteristics
Four hundred women enrolled and complete data from the enrolment visit were available from 396 mother-infant dyads. Nearly all women (94%) returned for the follow-up visit. One maternal and one child death were reported after enrollment. Mean maternal age was 29.6 years (5.1 SD). Three quarters of women reported primary school as their maximum level of education. Most (71%) cohabited with the index child’s father. Thirty-seven percent were on antiretroviral treatment (this was prior to introduction of PMTCT Option B+). Mean infant age was 6.0 months (SD 5.0), and HIV prevalence was 11%, although 27% of all children were still awaiting test results. Half of all households were classified as severely food insecure and a third experienced either moderate or severe hunger (Table I).
Table I.
Description of study population, n=396
| Variable | N | % |
|---|---|---|
| Site | ||
| Tumbi | 129 | (32.6) |
| Chalinze | 157 | (39.7) |
| Bagamoyo | 110 | (27.8) |
| Maternal education | ||
| None | 39 | (9.9) |
| Primary | 307 | (77.5) |
| Secondary | 47 | (11.9) |
| Missing | 3 | (0.8) |
| Maternal age in years (SD) | 29.6 | (5.1) |
| Marital status | ||
| Living together married | 135 | (34.1) |
| Living together unmarried | 149 | (37.6) |
| Living apart | 80 | (20.2) |
| Partner died/ RTA/DK | 19 | (4.8) |
| Missing | 13 | (3.3) |
| Mother’s HIV medication status | ||
| None | 14 | (3.5) |
| ART with or without CTX | 147 | (37.1) |
| CTX only | 232 | (58.6) |
| Other / RTA / DK | 3 | (0.8) |
| Child age | ||
| ≤6 months | 226 | (57.1) |
| > 6 to 12 months | 113 | (28.5) |
| > 12 to 18 months | 55 | (13.9) |
| Missing | 2 | (0.5) |
| Child HIV status | ||
| Negative | 170 | (42.9) |
| Positive | 20 | (5.1) |
| Not yet tested | 78 | (19.7) |
| Awaiting results | 107 | (27.0) |
| Test status unknown | 21 | (5.3) |
| Household Food Insecurity | ||
| None | 78 | (19.7) |
| Mild to moderate | 114 | (28.8) |
| Severe | 201 | (50.8) |
| Missing | 3 | (0.8) |
| Household Hunger | ||
| Little or none | 272 | (68.7) |
| Moderate or severe | 123 | (31.1) |
| Missing | 1 | (0.3) |
| Wealth | ||
| Lowest tertile | 120 | (30.3) |
| Middle tertile | 119 | (30.1) |
| Highest tertle | 119 | (30.1) |
| Missing | 38 | (9.6) |
Patterns and correlates of past disclosure
Only 5% of women had not yet disclosed their HIV positive status to anyone at the time of enrolment, mainly because they feared being expelled from their homes. Those who had disclosed (n=377) had told a median of 2 people (range 1–10). Most women had disclosed to their partner (65%) or a close female relative, such as mother (62%) or sister (55%). Disclosure to brother (27%), mother–in-law (11%) and other relatives (24%) was less common. Only 15% had told a friend and disclosure to other community-members was rare (6%). For the 27% of women who had only told one person, this one person was most often the husband (47%).
In multivariable analyses, study site was a strong determinant of a woman having disclosed to her mother (aOR (95% CI): Chalinze 3.2 (1.8 – 5.7)) and her mother-in-law (Chalinze 4.7 (5.5 – 365.0); Bagamoyo 9.4 (1.1 – 82.7)). Study site also modified the association between the couple’s living status and disclosure; women living apart from the father of their child were much less likely than married women to have disclosed to him in both Tumbi (aOR 0.2; 95% CI 0.1 – 0.6) and Bagamoyo (aOR 0.1; 95% CI 0.0 – 0.4). Cohabitating mothers were less likely to have disclosed to their partner in Chalinze only (aOR 0.3; 0.1 – 0.9). Mothers having an HIV-positive child were much less likely to have shared their own status with their husband (aOR 0.2 (0.1–0.6)), but the associations for disclosure to mothers or mothers-in-law that were present in univariate analysis did not hold. Household’s food security was strongly associated with disclosure to the mother-in-law only (mild-to-moderate food insecurity aOR 6.1 (1.4 – 26.2); severe food insecurity aOR 3.7 (0.8 – 16.1)) (Tables II, Tables IIIa and IIIb).
Table II.
Univariable association between demographic, clinical and socio-economic covariates and disclosure to partner, mother and mother-in-law
| Covariatea | Disclosure to partner (n=376) | Disclosure to mother (n=396) | Disclosure to mother-in-law (n=376) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | % | No | % | Pb | Yes | % | No | % | Pb | Yes | % | No | % | Pb | |
| Overall | 244 | (65) | 132 | (35) | 235 | (59) | 161 | (41) | 45 | (12) | 331 | (88) | |||
| Site | |||||||||||||||
| Tumbi | 78 | (66) | 41 | (34) | 57 | (44) | 72 | (56) | 1 | (1) | 118 | (99) | |||
| Chalinze | 95 | (63) | 55 | (37) | 117 | (75) | 40 | (25) | 36 | (24) | 114 | (76) | |||
| Bagamoyo | 71 | (66) | 36 | (34) | 0.889 | 61 | (55) | 49 | (45) | .000 | 8 | (7) | 99 | (93) | .000 |
| Maternal education | |||||||||||||||
| None | 21 | (55) | 17 | (45) | 22 | (56) | 17 | (44) | 3 | (8) | 35 | (92) | |||
| Primary | 185 | (64) | 106 | (36) | 158 | (60) | 122 | (40) | 36 | (12) | 255 | (88) | |||
| Secondary | 35 | (80) | 9 | (20) | .049 | 26 | (55) | 21 | (45) | .733 | 6 | (14) | 38 | (86) | .750 |
| Marital status | |||||||||||||||
| Living together married | 100 | (78) | 28 | (22) | 69 | (51) | 66 | (49) | 21 | (16) | 107 | (84) | |||
| Living together unmarried | 100 | (70) | 43 | (30) | 95 | (64) | 54 | (36) | 11 | (8) | 132 | (92) | |||
| Living apart | 34 | (45) | 41 | (55) | 47 | (59) | 33 | (41) | 6 | (8) | 69 | (92) | |||
| Partner died/ RTA/DK | 2 | (11) | 17 | (89) | .000 | 14 | (74) | 5 | (26) | .091 | 3 | (16) | 16 | (84) | .086 |
| Mother’s HIV medication | |||||||||||||||
| None | 9 | (75) | 3 | (25) | 8 | (57) | 6 | (43) | 0 | (0) | 12 | (100) | |||
| ART with or without CTX | 92 | (63) | 53 | (37) | 99 | (67) | 48 | (33) | 20 | (14) | 125 | (86) | |||
| CTX only | 141 | (65) | 76 | (35) | 127 | (55) | 105 | (45) | 25 | (12) | 192 | (88) | |||
| Other / RTA / DK | 2 | (100) | 0 | (0) | .750 | 1 | (33) | 2 | (67) | .057 | 0 | (0) | 2 | (100) | .557 |
| Child age | |||||||||||||||
| ≤6 months | 140 | (65) | 74 | (35) | 127 | (56) | 99 | (44) | 18 | (8) | 196 | (92) | |||
| > 6 to 12 months | 70 | (64) | 39 | (36) | 71 | (63) | 42 | (37) | 11 | (10) | 98 | (90) | |||
| > 12 to 18 months | 32 | (63) | 19 | (37) | .918 | 36 | (65) | 19 | (35) | .322 | 14 | (27) | 37 | (73) | .002 |
| Child HIV status | |||||||||||||||
| Negative | 114 | (71) | 47 | (29) | 113 | (66) | 57 | (34) | 30 | (19) | 131 | (81) | |||
| Positive | 9 | (45) | 11 | (55) | 15 | (75) | 5 | (25) | 1 | (5) | 19 | (95) | |||
| Not yet tested | 48 | (64) | 27 | (36) | 37 | (47) | 41 | (53) | 2 | (3) | 73 | (97) | |||
| Awaiting results | 60 | (59) | 42 | (41) | 62 | (58) | 45 | (42) | 12 | (12) | 90 | (99) | |||
| Test status unknown | 13 | (72) | 5 | (28) | .092 | 8 | (38) | 13 | (62) | .007 | 0 | (0) | 18 | (100) | .002 |
| Household Food Insecurity | |||||||||||||||
| None | 51 | (72) | 20 | (28) | 39 | (50) | 29 | (50) | 3 | (4) | 68 | (96) | |||
| Mild to moderate | 73 | (68) | 35 | (32) | 63 | (55) | 51 | (45) | 18 | (17) | 90 | (83) | |||
| Severe | 118 | (61) | 77 | (39) | .184 | 132 | (66) | 69 | (34) | .030 | 24 | (12) | 171 | (88) | .033 |
| Household Hunger | |||||||||||||||
| Little or none | 168 | (66) | 86 | (34) | 151 | (56) | 121 | (44) | 33 | (13) | 221 | (87) | |||
| Moderate or severe | 75 | (62) | 46 | (38) | .488 | 83 | (67) | 40 | (33) | .027 | 12 | (10) | 109 | (90) | .497 |
| Wealth | |||||||||||||||
| Lowest tertile | 76 | (65) | 41 | (35) | 80 | (67) | 40 | (33) | 23 | (20) | 94 | (80) | |||
| Middle tertile | 68 | (59) | 47 | (41) | 74 | (62) | 45 | (38) | 10 | (9) | 105 | (91) | |||
| Highest tertile | 72 | (66) | 37 | (34) | .525 | 57 | (48) | 62 | (52) | .009 | 7 | (6) | 102 | (94) | .006 |
| Maternal age, mean ( SD) | 29.2 | (5.8) | 29.4 | (5.7) | .823 | 29.3 | (5.8) | 29.2 | (5.5) | .793 | 30.2 | (4.3) | 29.2 | (5.9) | .238 |
Missing categories were excluded from analysis;
Fisher’s exact test
Table IIIa.
Multivariable association between demographic, clinical and socio-economic covariates and disclosure to partner (n=355, AUC 0.765)
| Covariate | OR | (95% CI) |
|---|---|---|
| Enrolment site * Relationship with father of child | ||
| Tumbi, married | 1 | |
| Tumbi, cohabiting | 1.77 | (0.69 – 4.54) |
| Tumbi, living apart | 0.18 | (0.06 – 0.59) |
| Tumbi, partner died | -- | -- |
| Chalinze, married | 1 | |
| Chalinze, cohabiting | 0.33 | (0.13 – 0.87) |
| Chalinze, living apart | 0.32 | (0.10 – 1.08) |
| Chalinze, partner died | 0.04 | (0.00 – 0.35) |
| Bagamoyo, married | 1 | |
| Bagamoyo, cohabiting | 0.40 | (0.10 – 1.57) |
| Bagamoyo, living apart | 0.10 | (0.03 – 0.36) |
| Bagamoyo, partner died | 0.02 | (0.00 – 0.26) |
| Maternal education | ||
| None | 1 | |
| Primary | 1.08 | (0.47–2.46) |
| Secondary | 2.76 | (0.87–8.72) |
| Maternal HIV medication | ||
| None | 1 | |
| ART with or without CTX | 0.86 | (0.19–3.86) |
| CTX only | 0.90 | (0.20–3.98) |
| Other / RTA / DK | -- | -- |
| Child age | ||
| ≤6 months | 1 | |
| > 6 to 12 months | 1.40 | (0.70–2.82) |
| > 12 to 18 months | 1.08 | (0.44–2.68) |
| Child HIV status | ||
| Negative | 1 | |
| Positive | 0.18 | (0.05–0.62) |
| Not yet tested | 0.83 | (0.36–1.89) |
| Awaiting results | 0.64 | (0.30–1.33) |
| Test status unknown | 1.18 | (0.32–4.38) |
| Household Food Insecurity | ||
| None | 1 | |
| Mild to moderate | 0.93 | (0.44–1.95) |
| Severe | 0.82 | (0.37–1.84) |
| Household Hunger | ||
| Little or none | 1 | |
| Moderate or severe | 1.13 | (0.55–2.29) |
Table IIIb.
Multivariable association between demographic, clinical and socio-economic covariates and disclosure to mother (n=371, AUC 0.695) and mother-in-law (n=324, AUC 0.856)
| Covariate | Disclosure to mother | Disclosure to mother-in-law | ||
|---|---|---|---|---|
| OR | (95% CI) | OR | (95% CI) | |
| Enrolment site | ||||
| Tumbi | 1 | 1 | ||
| Chalinze | 3.22 | (1.81 – 5.74) | 44.71 | (5.48 – 364.98) |
| Bagamoyo | 1.55 | (0.86 – 2.80) | 9.37 | (1.06 – 82.66) |
| Relationship with father of child | ||||
| Married | 1 | 1 | ||
| Cohabiting | 1.55 | (0.93 – 2.60) | 0.31 | (0.12 – 0.76) |
| Living apart | 1.27 | (0.69 – 2.35) | 0.43 | (0.14 – 1.33) |
| Partner died | 1.55 | (0.44 – 5.45) | 0.87 | (0.17 – 4.39) |
| Maternal education | ||||
| None | 1 | 1 | ||
| Primary | 1.07 | (0.50 – 2.27) | 1.18 | (0.28 – 4.97) |
| Secondary | 1.09 | (0.42 – 2.83) | 1.41 | (0.23 – 8.66) |
| Maternal HIV medication | ||||
| None | 1 | -- | -- | |
| ART with or without CTX | 0.80 | (0.21 – 3.07) | 1.02 | (0.46 – 2.23) |
| CTX only | 0.46 | (0.12 – 1.73) | 1 | |
| Other / RTA / DK | 0.13 | (0.08 – 2.07) | -- | -- |
| Child age | ||||
| ≤6 months | 1 | 1 | ||
| > 6 to 12 months | 0.81 | (0.44 – 1.50) | 0.73 | (0.25– 2.10) |
| > 12 to 18 months | 0.62 | (0.27 – 1.43) | 2.37 | (0.74 – 7.58) |
| Child HIV status | ||||
| Negative | 1 | 1 | ||
| Positive | 1.39 | (0.42 – 4.58) | 0.16 | (0.02 – 1.47) |
| Not yet tested | 0.51 | (0.25 – 1.07) | 0.40 | (0.07 – 2.25) |
| Awaiting results | 0.79 | (0.41 – 1.52) | 2.14 | (0.68 – 6.71) |
| Test status unknown | 0.45 | (0.15 – 1.39) | -- | -- |
| Household Food Insecurity | ||||
| None | 1 | 1 | ||
| Mild to moderate | 1.05 | (0.56 – 1.99) | 6.09 | (1.41 – 26.23) |
| Severe | 1.07 | (0.52 – 2.22) | 3.66 | (0.83 – 16.14) |
| Household Hunger | ||||
| Little or none | 1 | 1 | ||
| Moderate or severe | 1.33 | (0.69 – 2.57) | 0.55 | (0.19 – 1.59) |
Disclosure experiences
Nearly all women (376/377) described the reactions of the person(s) to whom they had disclosed (Figure 1). Many more women had entirely positive experiences (56%), than entirely negative ones (15%), while 8% experienced mixed positive and negative consequences. For 22% of women, their disclosure resulted only or also in “other” types of responses. Five percent of women spontaneously mentioned that family members who had initially reacted negatively became supportive over time. The opposite was not reported.
Figure 1.
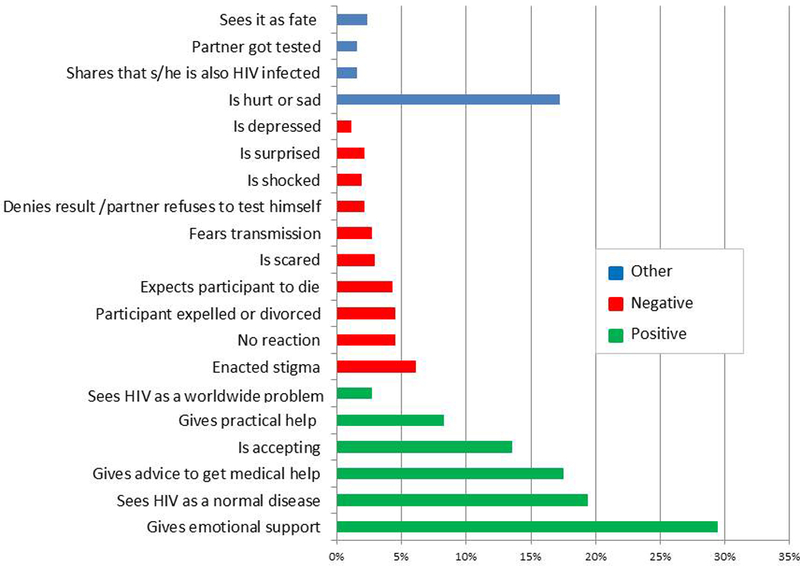
Reactions of recipients and consequences of HIV disclosure, reported by study participants (n = 376; multiple answers possible).
The majority of positive reactions consisted of some form of emotional support, mostly receiving consolation or encouragement (reported by 30% of women). For one fifth of the participants, the person(s) they disclosed to said they considered HIV to be a normal disease (20%) or a worldwide problem (3%). Advice to get or continue with medical help, especially ART (18%) and acceptance (14%) were also commonly experienced. Only 8% of women mentioned that practical help was given or promised, such as buying formula milk for the baby, providing transport to the clinic, or helping to care for the woman herself. Negative reactions most commonly consisted of enacted stigma (for 6% of women) such as violence, isolating the participant, or blaming her, e.g. for bringing the disease into the family, for being a prostitute or for refusing to get married. Five percent of women were either expelled from their homes or divorced. Four percent of women said their relatives considered the positive HIV test a death sentence. Less common negative reactions were being feared by their relatives, refusal to believe the test result, shock, surprise and depression. “Other” reactions predominantly consisted of the relative feeling hurt or sad (17%). In only 2% of cases did the woman’s disclosure result in the husband also taking an HIV test.
Uptake of facilitated disclosure
Seven out of 18 women (39%) who had not yet disclosed to anyone, disclosed during a nurse-facilitated session; two told a friend, two a sister, and the remaining three women brought their mother, mother-in-law and brother. Among those who had previously disclosed, 31% (116/377) participated in the nurse-facilitated disclosure session. Their relation with the person whom they disclosed to was recorded for 81 women; 46% (36/81) disclosed to a new person of whom 12 were sisters, 5 were their mother, 5 were their mother-in-law and 4 were their husband. Women who reported to have had any previous positive disclosure experiences were more likely to participate in the nurse-facilitated disclosure session (p=0.026).
DISCUSSION
Nurse-facilitated disclosure was feasible in this low resource setting. Though the past disclosure rate was already very high, nurse facilitated disclosure was moderately effective in helping women who had not yet disclosed to do so (39% newly disclosed) and in expanding the potential support base for women who had already disclosed to someone (46% disclosed to a new person). Disclosure is associated with reduced mother to child transmission (Torpey et al., 2012), horizontal transmission (Medley et al., 2015) and virological failure (Ramadhani et al., 2007). Even this modest uptake of nurse-facilitated disclosure may therefore lead to population health benefits and is worth exploring further in an adequately powered study design allowing for causal inference. Recently, a pilot randomized controlled trial from China also reported nurses were able to deliver a counseling intervention in a clinic setting that helped improve disclosure experiences, in this case from parents disclosing their own HIV positivity to their adolescent or adult children (Simoni et al., 2015).
The very large proportion of women (95%) who had disclosed their HIV positive status to at least one person at enrollment puts our study at the high end of the range of disclosure rates (5%−96.7%) recently reported in a systematic review (Tam et al., 2015). This high disclosure rate, as well as some of the disclosure experiences recounted by study participants, suggests that HIV infection is becoming normalized and antiretroviral treatment is being accepted in this population. Disclosure patterns that we observed were in line with the systematic review (Tam et al., 2015).
A mother with a child who tested HIV positive was much less likely to have disclosed her own HIV status to her partner. To our knowledge this is the first study in sub Saharan Africa reporting such an association. It is unlikely that women who hide their own status will disclose their infant’s HIV positivity. To ensure good adherence to pediatric ART and other aspects of care and treatment it is paramount that those taking care of the child, including the father, are aware of his or her HIV status (Bikaako-Kajura et al., 2006).
In multivariate models, women who were in other living arrangements with their partner than being married were much less likely to have disclosed to their partner, though this was strongly linked with enrolment site. In a study in Côte d’Ivoire, women living with their own family without their partner were three times less likely to have disclosed to him than women living with only their partner (Brou et al., 2007). The higher disclosure rates when being married could reflect a stronger relationship that may exist when legally married or may be the consequence of passive disclosure resulting from e.g. taking ART medication or following infant feeding guidelines that differ from norms in the community. However, since co-habitation without marriage was not associated with equally high partner disclosure rates, it is more likely that the marriage bond itself facilitates disclosure. Partly this may be due to the higher investment or commitment put into the relationship by married partners (Hattori, 2008), but may also be an effect of some churches in Tanzania requiring or heavily promoting pre-marriage counseling and testing for HIV before allowing the couple to get married.
Women in food-insecure households and households with lower wealth were more likely to have disclosed to their older female relatives, though after adjustment for site and other covariates, only mild-to-moderate food insecurity remained statistically significantly linked to disclosure to mother-in-law. Infant feeding is considered a women’s business in which the father’s role is limited to providing economical support and counsel by health workers is not given much weight. Instead, mothers or other elderly female relatives experienced in child rearing are viewed as voices of authority when a woman makes her infant feeding decisions (47,48). Possibly, in settings such as Tanzania where mixed feeding is commonly practiced (Centre, 2014), women are more likely to disclose to their elderly female relatives when they are economically vulnerable, either to generate funds for formula feeding or indirectly, to attain empowerment.
Despite the majority of women having positive disclosure experiences, a small group of women experienced severe negative consequences. Though IPV is reported to be common in Tanzania and is condoned in many households (Macro, 2011) only one woman explicitly mentioned that violence occurred between her and her husband. Several women were left by their husband and taken in by relatives. HIV control programs should therefore continue to strive to address stigma and IPV, both through community education and when exploring the possibility to disclose with a patient, as part of post-test HIV counseling.
Strengths and limitations
A strength of our study is that it was performed under programmatic circumstances in both semi-urban and rural settings, thus increasing its generalizability. Our relatively large sample size allowed us to unpack the correlates of disclosure to separate key persons who influence a woman’s ability to adhere to the different interventions in the PMTCT and the ART cascades, including the characteristics of the infant. The inclusion of open-text analysis of disclosure experiences allowed for a better understanding of the quantitative results. Limitations of the study were that we did not assess health outcomes associated with disclosure. Several potential correlates of disclosure were not measured, including relationship quality, partner characteristics and the woman’s psychological characteristics.
CONCLUSION
HIV positive mothers frequently disclosed their status to husbands and/or female relatives and experienced predominantly positive reactions. The finding that economically vulnerable women choose to disclose more often to elderly female relatives indicates that infant feeding counseling given to HIV positive women should acknowledge the role these elderly female relatives play and garner their support for implementing appropriate feeding practices. Both the enacted stigma experienced by some mothers, as well as the high number of women who brought a person they had already disclosed to for the nurse-facilitated disclosure session show that HIV education of family members and the wider community remains a key priority. Future research should confirm or refute the effectiveness of primary care provider facilitated disclosure, estimate its costs and establish its role in the landscape of disclosure interventions such as peer-support groups and partner notification.
REFERENCES
- Antelman G, Smith Fawzi MC, Kaaya S, Mbwambo J, Msamanga GI, Hunter DJ, & Fawzi WW (2001). Predictors of HIV-1 serostatus disclosure: a prospective study among HIV-infected pregnant women in Dar es Salaam Tanzania. AIDS (London, England), 15(14), 1865–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bateganya M, Amanyeiwe U, Roxo U, & Dong M (2015). The Impact of Support Groups for People Living with HIV on Clinical Outcomes: a systematic review of the literature. J Acquir Immune Defic Syndr, 68(3), S368–S374. http://doi.org/10.1097/QAI.0000000000000519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bezner Kerr R, Dakishoni L, Shumba L, Msachi R, & Chirwa M (2008). “We Grandmothers Know Plenty”: Breastfeeding, complementary feeding and the multifaceted role of grandmothers in Malawi. Social Science and Medicine, 66(January 2016), 1095–1105. http://doi.org/10.1016/j.socscimed.2007.11.019 [DOI] [PubMed] [Google Scholar]
- Bikaako-Kajura W, Luyirika E, Purcell DW, Downing J, Kaharuza F, Mermin J, … Bunnell R (2006). Disclosure of HIV status and adherence to daily drug regimens among HIV-infected children in Uganda. AIDS and Behavior, 10(4 Suppl), S85–93. http://doi.org/10.1007/s10461-006-9141-3 [DOI] [PubMed] [Google Scholar]
- Brou H, Djohan G, Becquet R, Allou G, Ekouevi DK, Viho I, … Desgrées-du-Loû A (2007). When do HIV-infected women disclose their HIV status to their male partner and why? A study in a PMTCT programme, Abidjan. PLoS Medicine, 4(12), e342 http://doi.org/10.1371/journal.pmed.0040342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buskens I, Jaffe a, & Mkhatshwa H (2007). Infant feeding practices: realities and mind sets of mothers in Southern Africa. AIDS Care, 19(9), 1101–1109. http://doi.org/10.1080/09540120701336400 [DOI] [PubMed] [Google Scholar]
- Byakika-Tusiime J, Crane J, Oyugi JH, Ragland K, Kawuma A, Musoke P, & Bangsberg DR (2009). Longitudinal antiretroviral adherence in HIV+ Ugandan parents and their children initiating HAART in the MTCT-Plus family treatment model: role of depression in declining adherence over time. AIDS and Behavior, 13 Suppl 1, 82–91. http://doi.org/10.1007/s10461-009-9546-x [DOI] [PubMed] [Google Scholar]
- Centre, T. F. and N. (2014). Tanzania National Nutrition Survey 2014. Dar es Salaam, Tanzania. [Google Scholar]
- Coates J, Swindale A, & Bilinsky P (2007). Household Food Insecurity Access Scale (HFIAS) for Measurement of Food Access: Indicator Guide (v. 3). Washington, D.C. [Google Scholar]
- Deitchler M, Ballard T, Swindale A, & Coates J (2010). Food and Nutrition Technical Assistance II Project (Fanta 2) Validation of a Measure of Household Hunger for Cross- Cultural Use. Washington, D.C. [Google Scholar]
- Gale NK, Heath G, Cameron E, Rashid S, & Redwood S (2013). Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Medical Research Methodology, 13(1), 117 http://doi.org/10.1186/1471-2288-13-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gourlay A, Birdthistle I, Mburu G, Iorpenda K, & Wringe A (2013). Barriers and facilitating factors to the uptake of antiretroviral drugs for prevention of mother-to-child transmission of HIV in sub-Saharan Africa: A systematic review. Journal of the International AIDS Society, 16, 1–21. http://doi.org/10.7448/IAS.16.1.18588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardon A, Gomez GB, Vernooij E, Desclaux A, Wanyenze RK, Ky-Zerbo O, … Obermeyer CM (2013). Do support groups members disclose less to their partners? The dynamics of HIV disclosure in four African countries. BMC Public Health, 13(1), 589 http://doi.org/10.1186/1471-2458-13-589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hattori M (2008). Trust, Commitment, Fidelity, and Condom Use among Young Adults in Tanzania. University of Maryland. [Google Scholar]
- Kaaya SF, Blander J, Antelman G, Cyprian F, Emmons KM, Matsumoto K, … Smith Fawzi MC (2013). Randomized controlled trial evaluating the effect of an interactive group counseling intervention for HIV-positive women on prenatal depression and disclosure of HIV status. AIDS Care, 25(7), 854–62. http://doi.org/10.1080/09540121.2013.763891 [DOI] [PubMed] [Google Scholar]
- Kairania RM, Gray RH, Kiwanuka N, Makumbi F, Nelson K, Serwadda D, … Wawer MJ (2010). Disclosure of HIV results among discordant couples in Rakai, -Uganda : A facilitated couple counselling approach. AIDS Care, 22(9), 1041–1051. http://doi.org/10.1080/09540121003602226.Disclosure [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy CE, Haberlen S, Amin A, Baggaley R, & Narasimhan M (2015). Safer disclosure of HIV serostatus for women living with HIV who experience or fear violence: A systematic review. Journal of the International AIDS Society, 18(Suppl 5). http://doi.org/10.7448/IAS.18.6.20292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macro, N. B. of S. (NBS) [Tanzania] and I. (2011). Tanzania Demographic and Health Survey. Dar es Salaam, Tanzania. [Google Scholar]
- Maman S, van Rooyen H, & Groves AK (2014). HIV status disclosure to families for social support in South Africa (NIMH Project Accept/HPTN 043). AIDS Care, 26(2), 226–32. http://doi.org/10.1080/09540121.2013.819400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medley A, Bachanas P, Grillo M, Hasen N, & Amanyeiwe U (2015). Integrating prevention interventions for people living with HIV into care and treatment programs: A systematic review of the evidence. Journal of Acquired Immune Deficiency Syndromes, 68, S286–S296. http://doi.org/http://dx.doi.org/10.1097/QAI.0000000000000520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuman A, Makhlouf Obermeyer C, Cherutich P, Desclaux A, Hardon A, Ky-Zerbo O, … Wanyenze R (2013). Experiences of stigma, discrimination, care and support among people living with HIV: A four country study. Aids Behav, 17(5), 1796–1808. http://doi.org/10.1007/s10461-013-0432-1.Experiences [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman A, Chopra M, & Kadiyala S (2007). Factors related to HIV disclosure in 2 South African communities. American Journal of Public Health, 97(10), 1775–81. http://doi.org/10.2105/AJPH.2005.082511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obermeyer CM, Baijal P, & Pegurri E (2011). Facilitating HIV disclosure across diverse settings: A review. American Journal of Public Health, 101(6), 1011–1023. http://doi.org/10.2105/AJPH.2010.300102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onono M.a., Cohen CR, Jerop M, Bukusi E, & Turan JM (2014). HIV serostatus and disclosure: implications for infant feeding practice in rural south Nyanza, Kenya. BMC Public Health, 14(1), 390 http://doi.org/10.1186/1471-2458-14-390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostermann J, Pence B, Whetten K, Yao J, Itemba D, Maro V, … Thielman N (2015). HIV serostatus disclosure in the treatment cascade: evidence from Northern Tanzania. AIDS Care, 27 Suppl 1(May 2016), 59–64. http://doi.org/10.1080/09540121.2015.1090534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramadhani HO, Thielman NM, Landman KZ, Ndosi EM, Gao F, Kirchherr JL, … Crump JA (2007). CSE THEME ARTICLE Predictors of Incomplete Adherence, Virologic Failure, and Antiviral Drug Resistance among HIV-Infected Adults Receiving Antiretroviral Therapy in Tanzania. Clinical Infectious Diseases, 45, 1492–1498. http://doi.org/10.1086/522991 [DOI] [PubMed] [Google Scholar]
- Sibeko L, Coutsoudis A, Nzuza S, & Gray-Donald K (2009). Mothers’ infant feeding experiences: constraints and supports for optimal feeding in an HIV-impacted urban community in South Africa. Public Health Nutrition, 12(11), 1983–1990. http://doi.org/10.1017/S1368980009005199 [DOI] [PubMed] [Google Scholar]
- Simoni J, Yang J, Shiu C, Chen W, Udell W, Bao M, … Lu H (2015). Nurse-delivered counselling intervention for parental HIV disclosure: results from a pilot randomized controlled trial in China. AIDS, 29(Suppl 1), S99–S107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spangler SA, Onono M, Bukusi EA, Cohen CR, & Turan JM (2014). HIV-Positive Status Disclosure and Use of Essential PMTCT and Maternal Health Services in Rural Kenya, 67, 235–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tam M, Amzel A, & Phelps BR (2015). Disclosure of HIV serostatus among pregnant and postpartum women in sub-Saharan Africa: a systematic review. AIDS Care, 27(4), 436–450. http://doi.org/10.1080/09540121.2014.997662 [DOI] [PubMed] [Google Scholar]
- Tanzania Commission for AIDS (TACAIDS), Zanzibar AIDS Commission (ZAC), N. B. of, & Statistics (NBS), Office of the Chief Government Statistician (OCGS), and I. I. 2013. (2013). Tanzania HIV / AIDS and Malaria Indicator Survey.
- Torpey K, Mandala J, Kasonde P, Bryan-Mofya G, Bweupe M, Mukundu J, … Welsh M (2012). Analysis of HIV early infant diagnosis data to estimate rates of perinatal HIV transmission in Zambia. PLoS ONE, 7(8), 3–10. http://doi.org/10.1371/journal.pone.0042859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. (2014). 2014 Progress Report on the global plan towards the elimination of new HIV infections among children by 2015 and keeping their mothers alive. Geneva. [Google Scholar]
- WHO. (2002). Innovative care for chronic conditions: building blocks for action: global report. Geneva. [Google Scholar]
- Williams AM, Chantry C, Geubbels EL, Ramaiya AK, Shemdoe AI, Tancredi DJ, & Young SL (2015). Breastfeeding and Complementary Feeding Practices among HIV-Exposed Infants in Coastal Tanzania. Journal of Human Lactation. http://doi.org/10.1177/0890334415618412 [DOI] [PubMed] [Google Scholar]
- World Health Organisation. (2010). PMTCT Strategic Vision 2010–2015. Preventing mother-to-child transmission of HIV to reach the UNGASS and Millennium Development Goals. Geneva. [Google Scholar]
- Young SL, Mbuya MNN, Chantry CJ, Geubbels EP, Israel-ballard K, Cohan D, … Latham MC (2011). Current Knowledge and Future Research on Infant Feeding in the Context of HIV : Basic, Clinical,. Advances in Nutrition, (6), 225–243. http://doi.org/10.3945/an.110.000224.highlight [DOI] [PMC free article] [PubMed] [Google Scholar]


