Abstract
Objective
We conducted a scoping review of the tools used to measure therapeutic relationship in patients with haemophilia.
Background
Haemophilia is an inherited bleeding disorder caused by a deficiency of a clotting factor in the blood. Therapeutic relationship is foundational to the management of patients with chronic diseases like haemophilia. A reliable and valid measurement tool for assessing therapeutic relationship is needed to evaluate the quality of care received by these patients, and to rigorously study the association between therapeutic relationship and the outcomes of treatment.
Methods
We adopted the Arksey and O'Malley framework for scoping studies. The following electronic databases were searched for studies that measured a construct related to therapeutic relationships in haemophilia care: MEDLINE, EMBASE, CINAHL, PsycINFO and Scopus. We inventoried these studies, identified the measurement tools used, and described each tool by purpose, content, measurement properties and target population. We identified gaps in the current evidence and directions for future research.
Results
There were 253 unique records retrieved in the search, and twenty studies were deemed relevant. Ten measurement tools were identified. None of the tools measured therapeutic relationship as a single entity; however, six tools measured constructs considered part of patient‐provider relationship (eg trust, communication, working alliance). There has been little validation testing of these tools in haemophilia patient populations.
Conclusions
There is a need for a validated tool for measuring therapeutic relationship in the care of patients with haemophilia. This review provides a foundation for future research in this area.
Keywords: blood coagulation disorders, inherited; health‐care surveys; patient outcome assessment; patient participation; patient‐reported outcome measures; professional‐patient relations; validation studies
1. INTRODUCTION
Haemophilia is an inherited bleeding disorder caused by a deficiency of a clotting factor in the blood. Patients are at a lifelong risk of bleeding into joints and muscles. Recurrent bleeding often results in chronic impairment of musculoskeletal structures and function, leading to pain and disability.1 Prevention of this process is a priority in the improvement of health and quality of life of patients with haemophilia. This is accomplished through regular encounters and monitoring by an interdisciplinary haemophilia treatment clinic (HTC), which consists of physicians, nurses, physical therapists and social workers.2 Successful management of haemophilia requires that patients actively participate in their care with the HTC. This purposeful partnership of patient and health‐care providers from the HTC is described as the “therapeutic relationship.”
Therapeutic relationship has been consistently associated with treatment outcomes in health research.3, 4, 5, 6 Kelley et al4 conducted a systematic review and meta‐analysis of randomized controlled trials examining the effect of manipulating patient‐clinician relationships on medical outcomes. A significant effect in favour of the enhanced patient‐provider relationships group was found in the meta‐analysis. The review included studies of populations of patients with complex chronic conditions (eg diabetes, asthma, hypertension, oncology, obesity), which requiring on‐going management similar to haemophilia. In the care of patients with haemophilia, therapeutic relationship is widely acknowledged as a fundamental part of providing care.7 It has been suggested that a close partnership between patient and health‐care providers facilitates the dynamic management of haemophilia throughout life through tailored treatment and personalized therapeutic goals.8 A number of authors have highlighted the significance of therapeutic relationship in the care of patients with haemophilia. Therapeutic relationship has been the topic of expert narrative reviews exploring the evolution of patient‐provider relationships and patient autonomy,9, 10 and ideas about therapeutic relationship in contemporary haemophilia care.11, 12, 13 Findings from qualitative studies suggest that patients and health‐care providers consider aspects of patient‐provider relationship to be a key component of haemophilia treatment.12, 14, 15, 16, 17
At present, there is an emphasis in haemophilia research on understanding the factors that influence patient's degree of adherence to treatment, which is important because patient adherence to treatment is linked with positive outcomes such as reduced pain and improved joint health.18, 19 Further, preliminary research suggests significant associations between patients' degree of adherence to factor replacement therapy and certain dimensions of therapeutic relationship.20 Specifically, patients reporting a higher degree of trust in their haemophilia physician have higher rates of adherence to treatment.20 Similarly, a good relationship with a haemophilia health‐care provider has been positively correlated with adherence levels.21
As interest in this area of haemophilia research grows, it becomes important to establish a validated and standardized approach to measuring therapeutic relationship. A high‐quality measurement tool will improve the validity of research into the processes and mechanisms by which therapeutic relationships impact outcomes, such as pain, joint health, and quality of life for patients with haemophilia. A standardized approach to measurement will also facilitate comparisons between studies of interventions aimed at improving therapeutic relationship.
Given the importance of a validated tool, and the relevance of studying therapeutic relationship in this population, we conducted a scoping review to provide a comprehensive overview of the research in the area of measurement of therapeutic relationship in the care of patients with haemophilia. Although we focus on research applications of measurement, this review also has implications for evaluating quality of care and assessing the patient's experience of care.
The objectives of our scoping study were to:
Locate and inventory the studies that assess therapeutic relationship in haemophilia, and describe the nature and extent of this evidence.
Identify the measurement tools that were used, and examine the literature associated with each tool.
Summarize the characteristics of the tools that are relevant to researchers when selecting an appropriate measure of therapeutic relationship.
Identify knowledge gaps in this area and directions for future research.
2. METHODS
2.1. Design
We adopted the Arksey and O'Malley22 framework for scoping studies. There are five stages in the framework22: (a) Identifying the research question; (b) Identifying relevant studies; (c) Selecting studies for analysis; (d) Charting the data; and (e) Collating, summarizing and reporting results. We complemented these stages with the recommendations of Levac et al.23 Briefly, Levac et al23 emphasize the need for an iterative and team approach to study design, establishing inclusion and exclusion criteria, searching and selecting relevant articles, and identifying key variables for data extraction. We incorporated these recommendations into the methods of this study.
2.2. Search strategy
We identified studies that were relevant to our research question through online searches of relevant health databases from their inception to April 2017. These searches were performed with the assistance of an experienced health research librarian at the University of Alberta. The following electronic databases were searched: MEDLINE (Ovid), EMBASE (Ovid), CINAHL (EBSCOhost), PsycINFO (Ovid) and Scopus. Each search strategy was adapted to the various databases as required, and we did not apply any search limits.
There were three concepts in our search strategy: (a) the relationship between a health‐care provider and patient, (b) haemophilia and (c) measurement. For each concept, we included multiple synonyms and key words. Additionally, we searched the reference lists of the articles selected for inclusion and hand‐searched one key clinical journal, Haemophilia, from 1998 to April 2017. During this stage, as the researchers became familiar with the literature, the selection criteria were established. An example of the search strategy is included as Appendix 1. The full search strategy is available upon request from the corresponding author.
2.3. Study selection
Two members of the research team independently screened the titles and abstracts of the publications retrieved in the database search. Full texts of the potentially relevant articles were acquired and appraised in reference to our study selection criteria. We included peer‐reviewed articles that described the development, testing or use of a measurement tool in a research study to assess or measure therapeutic relationship or related construct, focusing on a population of patients with inherited bleeding disorders and the health‐care providers (from any discipline) involved in their treatment. We included an article if it measured a subcomponent of therapeutic relationship (eg trust, empathy, communication) or a construct that may be considered to contribute to therapeutic relationship (eg patient‐centredness, satisfaction with care, shared decision making). We included self‐report questionnaires (patient or health‐care provider perspective), observer‐rated scales and coding schemes, all modes of administration (eg paper and pencil, computerized or interview). Any discrepancies between reviewers that arose during the review process were resolved through discussion. We used a kappa coefficient to quantify inter‐rater reliability between reviewers.
As the reviewers became familiar with the literature, they noticed that therapeutic relationship was often conflated with other constructs related to clinical encounters and that authors often did not clearly define the construct being assessed. This made it difficult to determine the content of the measurement tools. To address the issue, we added an item content analysis step to our methods (described in the “Data analysis” section below), similar to methods used by Eveleigh et al.24 This iterative approach to methods is an advantage of scoping study methodology for an emerging research area like therapeutic relationship, where little is known about the literature prior to starting the study.23
A second challenge encountered during study selection related to the definition of “patient satisfaction with care.” This term might refer to patient satisfaction with interpersonal aspects of care, satisfaction with the specific intervention or satisfaction with the outcomes of treatment. We addressed this challenge through discussion within the research team, which resulted in a clearer definition and common understanding to only include studies assessing satisfaction with interpersonal aspects of care.
2.4. Charting the data
A single reviewer extracted relevant study features, which were determined based on our research question and objectives. We obtained a copy of each measurement tool that was identified.
2.5. Data analysis
To describe the nature and extent of the evidence, we calculated descriptive statistics (frequencies and percentages) for the key characteristics of the studies included in the review. Figure 1 shows the flow of the methods of data analysis.
Figure 1.
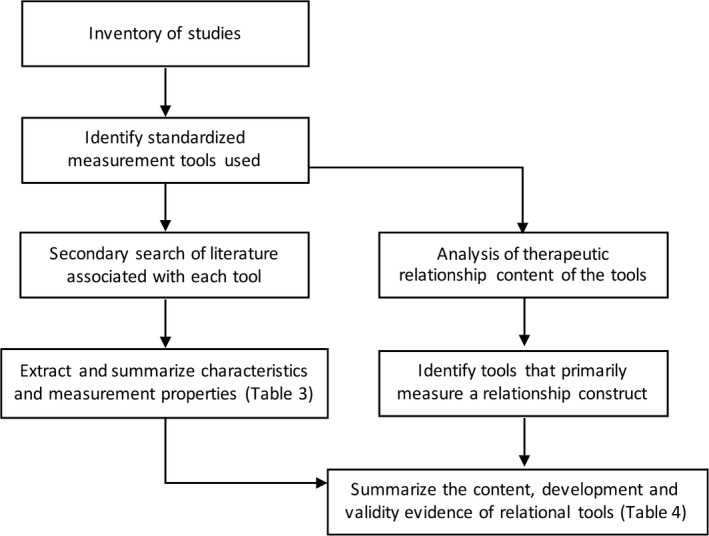
Flow chart of the methods used for data analysis
2.5.1. Measurement properties
A useful measurement tool should meet two standards of comprehensiveness.25 First, a tool should be accurate and precise through the full range of the variable being measured (eg from poor to strong therapeutic relationships) within the target patient population. It is therefore important to examine the evidence concerning the tool's measurement properties, that is, reliability and validity, in the context of the intended target population.25 Second, the content of the tool should adequately represent all the multiple dimensions or components of a health construct.25 Therefore, we conducted a second search of the literature to find all published work associated with each measurement tool identified. We searched reference lists, MEDLINE, and the search engine Google, using the name of the tool, any known synonym and abbreviations. We extracted information related to the development and testing of the tool, the measurement properties reported and the theoretical basis of the tools from the articles retrieved in the second search. We examined the extent of the validity evidence for each of the measurement tools identified. We used the COSMIN26 (COnsensus‐based Standards for the selection of health status Measurement Instruments) taxonomy and definitions for measurement properties as a guide. We summarized the characteristics of the tools in table form.
2.5.2. Content analysis
The content of the tools was analysed using the framework of therapeutic relationship in physiotherapy developed by Miciak.27 Therapeutic relationship has not been conceptualized in the haemophilia literature, and Miciak's framework has qualities that made it appealing for use in this study. The framework was developed using rigorous qualitative methods, it is comprehensive in scope, and it is sufficiently detailed to provide a clear understanding of the fundamental components of the therapeutic relationship.27
The three components of therapeutic relationship are as follows: (a) The conditions of engagement, (b) Ways of establishing connections and (c) Elements of the bond (Figure 2).27 Further, each component is comprised of subcomponents that describe its nature. The conditions of engagement are the attitudes and intentions of the patient and health‐care provider that contribute to “ways of being”—that is, how the patient and health‐care provider “are” together. The conditions of engagement are as follows: committed, genuine, receptive and present.28 The ways of establishing connections describe the actions and behaviours of the health‐care provider and patient within a clinical encounter. Connections involve using the body as a pivot point (ie health‐care provider and patient connecting through the patient's body, physiological health condition or physical symptoms), giving‐of‐self and acknowledging the individual (ie validating, individualizing treatment).29 The elements of the bond—caring, trust, respect and nature of the rapport—describe the emotional or affective resonance between the patient and provider.27 Further, Miciak et al identified three themes that should be reflected in the content of a tool intended to measure therapeutic relationship: (a) Therapeutic relationships are a mutual endeavour—patients and health‐care providers contribute to the process; (b) Body is central to the therapeutic relationship—the patient's experiences with the physiological impact of the health condition (ie body) is the common ground between providers and patients; (c) Therapeutic relationship is “personal” and “professional”—positions the therapeutic relationship as part of the health‐care provider's professional responsibilities, while acknowledging the potential for the health‐care provider and patient to have interest and care about the other beyond the clinical reasons for the interaction.27
Figure 2.

The theoretical framework of therapeutic relationship. There are 3 components in the framework, each with subcomponents which further describe its nature
We used the themes and the components in the therapeutic relationship framework to describe the content of the tools and to systematically distinguish the tools that primarily measure a component or subcomponent of therapeutic relationship. We termed these “relational tools,” which we operationally define as a measurement tool that assesses attitudes, intentions, behaviours or feelings between a health‐care provider and a patient. A general patient satisfaction questionnaire is not a “relational tool” as we have defined it. Although it may contain a small proportion of items that address patient‐provider relationship, patient satisfaction questionnaires also typically assess organizational‐ or system‐level health services and processes. We examined the content of a tool using the items as the unit of analysis. We coded each item in reference to the component of therapeutic relationship that it measured (if any). Items that did not fit the therapeutic relationship framework were coded as either “satisfaction with care” or “not interpersonal.” Examples of the item appraisal are included as Appendix 2. For each tool, we calculated the proportion of items in each category (ie relationship, satisfaction or not interpersonal). We distinguished the relational tools based on the proportion of items that measured therapeutic relationship. Finally, we checked whether the tool addressed each of the three themes Miciak identified in therapeutic relationship (personal and professional, body as central and mutuality). Appendix 3 contains the findings of the content analysis. One member of the research team conducted item analysis, and a second member reviewed the results, with any discrepancies resolved through discussion. We summarized the content, function and validity evidence of each relational tool to provide a comprehensive overview of the relational tools used in haemophilia for researchers selecting a measurement tool.
2.6. Patient and public involvement and engagement
The aim of patient and public involvement and engagement (PPIE) in this study was to plan, conduct and interpret findings of the research in a manner that was meaningful to patients and their health‐care providers. One patient partner was involved throughout the study as a member of the study team (JH). He is a person with haemophilia and a Master's student at the University of Alberta . He helped design the study, refine the research question and scope, interpret results and critically review written reports. This was accomplished through meetings with the lead researcher, electronic communications and informal conversations at related scientific gatherings. Health‐care providers were also consulted during project planning and after the literature search.
3. RESULTS
The search and selection process is summarized in Figure 3. The initial search of electronic databases returned 416 records. After 163 duplicates records were removed, two reviewers screened 253 titles and abstracts for potential inclusion. Inter‐rater reliability between reviewers was high in the screening process (Kappa = 0.81). Forty‐nine articles were retrieved for full‐text appraisal. Thirty articles did not fit the criteria for inclusion. One of the articles was a systematic review, which was excluded from further analysis after a search of its reference list for relevant publications. Subsequent to the search, one article was located through the professional networks of the research team. Twenty articles were selected for inclusion, and inter‐rater reliability was good (Kappa = 0.76).
Figure 3.

Flow chart of the article search and selection stages
3.1. General description of the included studies
The main characteristics of the included articles are summarized in Table 1. The majority of studies (95%) originated in western Europe or North America. A large proportion of the studies (40%) were published in the last 2 years (2016‐2017). The earliest article was published in 1995. A variety of study designs and target populations were used.
Table 1.
Descriptive characteristics of the studies included in the review
| Characteristic | Number of articles | Percentage of studies |
|---|---|---|
| Geographic region | ||
| Canada | 1 | 5 |
| United States | 5 | 25 |
| Germany | 2 | 10 |
| Italy | 2 | 10 |
| Spain | 4 | 20 |
| The Netherlands | 3 | 15 |
| Finland | 1 | 5 |
| European (multinational) | 1 | 5 |
| Republic of Georgia | 1 | 5 |
| Date of publication | ||
| 2016‐2017 | 8 | 40 |
| 2011‐2015 | 3 | 15 |
| 2006‐2010 | 2 | 10 |
| 2001‐2005 | 4 | 20 |
| 2000 or before | 3 | 15 |
| Study purpose | ||
| Characterize the haemophilia population | 6 | 30 |
| Evaluate health services | 4 | 20 |
| Evaluative an intervention | 4 | 20 |
| Develop a measurement tool | 6 | 30 |
| Study design | ||
| Cross‐sectional | 12 | 60 |
| Prospective cohort study | 2 | 10 |
| Methodological | 6 | 30 |
| Types of relational constructs assessed | ||
| Working alliance | 1 | 5 |
| Socio‐emotional element | 7 | 35 |
| Communication behaviour | 4 | 20 |
| Satisfaction with health services | 8 | 40 |
| Study population diagnosis | ||
| Haemophilia | 15 | 75 |
| Mixed inherited bleeding disorders | 3 | 15 |
| Mixed haematological conditions | 1 | 5 |
| Haemophilia carriers | 1 | 5 |
| Study population ages | ||
| Adults | 5 | 25 |
| Adult and paediatric patients | 8 | 40 |
| Paediatric patients and parents | 3 | 15 |
| All ages and parents/caregivers | 4 | 20 |
| Disciplines assessed | ||
| Physician | 8 | 40 |
| Nurse | 5 | 25 |
| Physical therapist | 3 | 15 |
| Social worker | 3 | 15 |
| Nonspecific haemophilia health‐care providers | 10 | 50 |
| Other services | 2 | 10 |
With regard to the relationship construct measured in each study, there were no articles that measured therapeutic relationship as a single entity. One study assessed working alliance—a concept originating in the psychotherapy literature.30 Seven studies assessed socio‐emotional elements in therapeutic relationship, for instance, patient trust in the physician, empowerment, collaboration or provider receptiveness. Task‐focused communication—communicative “acts” of the patient or provider—was assessed in four studies. Eight studies evaluated patient satisfaction with health services (n = 8). Six of these articles assessed satisfaction with the services of a HTC, and two assessed satisfaction with other health services (genetic testing, pain therapy). Table 2 contains an inventory of the studies included in this review.
Table 2.
Inventory of the studies included in the review
| Brief citation | Title | Description of study purpose and design | Study population characteristics | Description of relationship construct | Relationship outcome measure(s) used | Measurement properties testeda |
|---|---|---|---|---|---|---|
| Ely 199542 | The Working Alliance in Pediatric Chronic Disease Management: A pilot study of instrument reliability and feasibility | A pilot study of aiming to test reliability, interpretability and usability of a measure of patient‐provider relationship adapted from the Working Alliance Inventory60 | Children (7‐14 y old)), adolescents (15‐20 y old), their parents or guardian, physicians and nurse practitioners from a haematology clinic | Quality of the relationship between health‐care providers and their patients | Working Alliance Inventory for Chronic Conditions | Internal consistency, test‐retest reliability, construct validity |
| Carl 199561 | HealthDesk for haemophilia: an interactive computer and communications system for chronic illness self‐management | A pilot study of the implementation of a computer software program for home self‐management. Patient satisfaction with the program, patient‐provider communication and user confidence in self‐management were assessed. Cross‐sectional design | Male patients ages 9‐39 y old with severe haemophilia on home infusion programme (n = 8) | Ease of communication with HTC using the software | Not a standardized measurement tool | None |
| Jacobson 201641 | Telehealth videoconferencing for children with haemophilia and their families: A clinical project | Descriptive study of implementing teleconferencing for evaluating bleeds in children with haemophilia. Data collected regarding bleeds, and user satisfaction. Cross‐sectional design | Male patients (2‐18 y old) with severe haemophilia in New Mexico and Texas, USA (n = 12) | Satisfaction with teleconferencing in terms of communication with haemophilia treatment centre | Not a standardized measurement tool | None |
| Lock 201662 | Optimization of home treatment in haemophilia: effects of transmural support by a haemophilia nurse on adherence and quality of life | A prospective cohort study of the effects of transmural support (home visits) on adherence, quality of life and self‐efficacy for patients with haemophilia | Paediatric patients (mean 9.4 y) with haemophilia A or B, any disease severity, on home infusions (n = 46) | Behaviour of patient in communicating with haemophilia treatment centre | Communication subscale of the Veritas‐PRO | Interpretability |
| Miesbach 201640 | Adherence to prophylactic treatment in patients with haemophilia in Germany | Cross‐sectional survey of German patients to explore associations between adherence to treatment and patient characteristics, such as age, severity of disease, home treatment, pain level, comorbidities, on adherence | Patients with moderate or severe haemophilia A or B, from Germany (n = 397) | Behaviour of patient in communicating with haemophilia treatment centre | Communication subscale of the Veritas‐PRO | None |
| de Moerloose 200821 | A survey of adherence to haemophilia therapy in six European countries: results and recommendations | A descriptive correlational study using structured interviews with patients and health‐care providers. Explored factors that influence adherence, including treatment regimen, environment, patient attitudes, and knowledge of treatment, experiences and preferences | Patients with severe haemophilia A, any age, from six European countries: France, Germany, Italy, Spain, Sweden and the UK (n = 180) | Patient perception of the degree of collaboration between, and relationship with, haemophilia care providers | Not a standardized measurement tool | None |
| del Río‐Lanza 201636 | Information provision and attentive listening as determinants of patient perceptions of shared decision‐making around chronic illnesses | A cross‐sectional survey design, authors used structural equation modelling to describe the pathways of influence of multiple patient‐provider communication variables on patient perceptions of shared decision making | Respondents were adult patients with haemophilia A and B, using regular factor replacement therapy and parents of paediatric patients (n = 181) | Health‐care provider and patient relational communication characteristics, and patient perception of shared decision making | University of Oviedo Surveyb | Validity, reliability, interpretability |
| Lamiani 201739 | Applying a deliberation model to the analysis of consultations in haemophilia: Implications for doctor‐patient communication | Researchers report on the development of an interaction analysis coding scheme using the Theoretical Model of Deliberation Dialogues. The tool was used to analyse shared decision making during a physician encounter | Patients with haemophilia A over the age of 12, using prophylaxis or on‐demand therapy (n = 30) | Shared decision making dialogue | Theoretical Model of Deliberation Dialogues Coding Scheme | None |
| Lock 201238 | The group medical appointment (GMA) in haemophilia and von Willebrand's disease: A new development in outpatient paediatric care | A prospective cohort study of the implementation of a “group medical appointment” care model. Parents or patients' expectations and experiences of the encounter were collected using a self‐report questionnaire | Families with children (mean age of 8 y), mixed inherited bleeding disorders patients in the Netherlands (n = 53) | Patient expectations and perceptions of health‐care provider communication before and after a health encounter | QUOTE‐Communication Questionnaire | None |
| Suarez‐Vazquez 201637 | Empower Me? Yes, Please, But in My Way: Different Patterns of Experiencing Empowerment in Patients with Chronic Conditions. Health Communication, 0(0), 1‐6 | A cross‐sectional survey design, studying the associations between patient and provider communication variables and patients' self‐perception of empowerment were analysed using mixed multiple linear regression modelling | Respondents were adult patients with haemophilia A and B, using regular factor replacement therapy and parents of paediatric patients (n = 181) | Health‐care provider and patient relational communication characteristics and patient empowerment experience | University of Oviedo Survey | Validity, reliability, interpretability |
| Tran 201620 | Physician trust and depression influence adherence to factor replacement: a single‐centre cross‐sectional study | The aim of the study was to explore associations between patient's adherence to factor replacement therapy and demographic, socio‐economic, psychosocial (trust in physician) and health literacy and numeracy variables | Adult patients with moderate or severe haemophilia A or B (n = 91) | Patient's trust in their physician | Wake Forest Trust in Physician Scale | Interpretability |
| Triemstra 199835 | Well‐being of haemophilia patients: A model for direct and indirect effects of medical parameters on the physical and psychosocial functioning | The development and evaluation of a structural equation model for establishing the patient characteristics that impact well‐being in patients with haemophilia | Patients with haemophilia A or B in the Netherlands, aged 15 y or older (n = 980) | Health locus of control, that is, the extent to which individuals perceive health‐care providers to be responsible for their health | Multi‐dimensional health locus of control scale (Dutch adaptation) | Reliability |
| Arranz 200433 | Development of a new disease‐specific quality‐of‐life questionnaire to adults living with haemophilia | Early stages of the development and testing of a haemophilia‐specific quality‐of‐life questionnaire. 75 items were pilot tested, and reduced to 44 items after expert review and pilot testing | Pilot testing of a new questionnaire in adult patients with moderate or severe haemophilia A and B (n = 35) | Patient satisfaction with treatment as a subscale of a disease‐specific health‐related quality of life | Hemofilia‐QoL | Validity, reliability, interpretability |
| Hacker 200634 | A patient satisfaction survey for haemophilia treatment centres | The authors describe the development and testing of a patient‐reported questionnaire to measure satisfaction with the services of their clinic | Paediatric and adult patients with an inherited bleeding disorder from one haemophilia clinic in the United States (n = 271) | Satisfaction with health services including interpersonal skills and quality of care | Mountain States Regional Patient Satisfaction Survey | Validity, reliability, interpretability |
| Jarvinen 199963 | Carrier testing of children for two X‐linked diseases: A retrospective evaluation of experience and satisfaction of subjects and their mothers | The authors used a recall questionnaire to study the experiences of young women who underwent genetic testing as children | Young females from families affected by haemophilia and Duchenne's muscular dystrophy in Finland (n = 23) | Patient perception of their satisfaction and degree of participation in medical decision making | Not a standardized measurement tool | Interpretability |
| Kalnins 201564 | Pain therapy in haemophilia in Germany | A descriptive study based on a questionnaire survey to assess patient's perceptions of pain and pain management | Paediatric and adult patients with haemophilia A or B in Germany (n = 685) | Satisfaction with pain therapy services | Not a standardized measurement tool | None |
| Kirtava 200565 | National haemophilia programme development in the Republic of Georgia | Description of the development of a comprehensive clinic in the Republic of Georgia | Patients with haemophilia A or B from a haemophilia clinic in the Republic of Georgia (n = 104) | Satisfaction with haemophilia treatment centre services | Not a standardized measurement tool | None |
| Page 201666 | Penny wise, pound foolish: an assessment of Canadian haemophilia/inherited bleeding disorder comprehensive care program services and resources | A report on a national survey of Canadian Comprehensive care inherited bleeding disorder programmes and services. Data were collected through interviews with clinicians from haemophilia treatment clinics, and a satisfaction with services survey of Canadian patients | Families and adult patients with any inherited bleeding disorder in Canada (n = 347) | Patient satisfaction with their relationship with their haemophilia treatment centre staff | Not a standardized measurement tool | None |
| Remor 200567 | Psychometric field study of the new haemophilia quality of life questionnaire for adults: The “Hemofilia‐QoL” | A psychometric field study of a newly developed health‐related quality of life questionnaire. The 44‐item draft questionnaire was reduced to 36 items after psychometric evaluation | Patients with haemophilia A and B, mild‐to‐severe disease in Spain (n = 121) | Patient satisfaction with treatment as a subscale of a disease‐specific health‐related quality of life | Hemofilia‐QoL | Validity, reliability, interpretability |
| von Mackenson 201331 | Cross‐cultural adaptation and linguistic validation of age‐group‐specific haemophilia patient‐reported outcome (PRO) instruments for patients and parents | A paper describing the process of translation, and cross‐cultural validation of 3 disease‐specific questionnaires, including one for satisfaction with haemophilia treatment, the Hemo‐SAT | No patients were involved in the language translation study | Satisfaction with haemophilia nurses and specialist services, as a subscale of satisfaction with haemophilia treatment | Hemo‐SAT | Validity, reliability, interpretability |
The measurement properties of the tool which were tested in the study.
This tool was not named in the studies; therefore, in this paper we have referred to it by the institution at which it was developed.
The aims of the studies were grouped into three categories: (a) seeking to explain interpersonal phenomena in patient care, (b) evaluating an intervention and (c) describing health services. Six studies were assigned to category 1, and these explored the associations between patient and provider characteristics, environmental factors and outcomes of treatment. The four studies in category 2 sought to evaluate an intervention, for example, a new application of a technology or service delivery model. Finally, the four studies in category three aimed to describe health services for patients with haemophilia. The remaining six studies aimed to develop a measurement tool. We identified shared decision making and adherence to treatment as two topics that were frequently studied relative to subcomponents of therapeutic relationship. Five studies were conducted for the purpose of understanding elements of shared decision making. Four studies were aimed at understanding the factors related to adherence to treatment in haemophilia.
3.2. Description of measurement tools
Thirteen of the twenty articles described a standardized measurement tool. Ten unique tools were identified: the “Specialist/Nurses” subscale of Hemo‐SAT, 31 the “treatment satisfaction” domain of Hemofilia‐QoL, 32, 33 Mountain States Regional Haemophilia and Thrombosis Center Patient Satisfaction Survey, 34 Multi‐dimensional Health Locus of Control Scale, 35 University of Oviedo Survey 36, 37 (UOvS), QUOTE‐Communication Questionnaire 38 (QUOTE), Theoretical Model of Deliberation Dialogues 39 (TMDD), the “Communication” subscale of the Veritas‐PRO, 40, 41 the Wake Forest Trust in Physician Scale 20 (WFTPS) and the Working Alliance Inventory for Chronic Conditions 42 (WAI‐CC).
An additional 27 articles were found that reported on a tool's development or testing. Within the associated literature, we found evidence for all tools regarding content validity and interpretability. Additionally, we found that internal consistency (coefficient alpha) had been reported for all the self‐report questionnaires. The measurement properties of six tools were tested in a haemophilia patient population. Key characteristics of the tools and their associated literature are described in Table 3.
Table 3.
Description of the measurement tools identified from studies involving patients with haemophilia
| Measurement tool | Description | Disciplinea | Measurement constructb | Subscales or domains | Number of items and response scale |
|---|---|---|---|---|---|
| Hemofilia‐QoL32, 33 | A disease‐specific quality of life questionnaire, with a “treatment satisfaction” subscale | Haemophilia health‐care providers | 2‐item subscale measuring satisfaction with care | Eight domains: physical health, physical role, joint damage, pain, treatment satisfaction, emotional functioning, mental health and social support | 2 items, 5‐point Likert scale |
| Hemo‐SAT specialist/nurses subscale31 | The Hemo‐SAT was developed to assess patient satisfaction with haemophilia treatment. It contains a subscale, “satisfaction with specialist/nurses” | Physicians and nurses | Satisfaction with care from haemophilia specialists and nurse | Seven domains: ease/convenience, efficacy, burden, side‐effects, specialist/nurse, centre/hospital, general satisfaction | 7 items, 5‐point Likert scale |
| Mountain States Patient Satisfaction Survey34 | A questionnaire survey designed to measure patient satisfaction with the care provided by a haemophilia treatment centre | Haemophilia health‐care providers | Patient satisfaction services of a haemophilia treatment centre | Four domains: technical competence, interpersonal skills, quality of care and access | 37 items, 5‐point Likert scale |
| Multi‐dimensional health locus of control scale35 | Measures the degree to which a person perceives others (health‐care professionals) to have control over their health own health | Physician | Patient's health locus of control | Three dimensions: self, others, luck; “Other” measures the extent to which an individual perceives others to be responsible for his or her health | 18 items, 6‐point Likert scale |
| QUOTE‐Communication Questionnaire38 | A patient‐reported satisfaction questionnaire, based on the theory that patient satisfaction is a function of patient expectations and experiences | Health‐care providers | Patient satisfaction with communication during a health‐care encounter | Two subscales (previsit and postvisit) each with two domains (biomedical and psychosocial) | 2 sets of 10 items, 5‐point Likert scale |
| Theoretical Model of Deliberation Dialogues coding scheme39 | An observer‐rated coding scheme to analyse shared decision making between patient and physician during a consultation | Physicians | Patient and physician interactions | Codes based on three stages in shared decision making: opening stage (topic or problem introduced), argumentation stage (solutions proposed, arguments for or against a proposal), closing stage (explicit agreement by one or both participants) | A rating scale of Complete or Incomplete; codes describe qualities of an incomplete dialogue |
| University of Oviedo Survey36, 37 | A patient‐reported questionnaire developed for the purpose of developing statistical models to describe relationships between patient‐provider communication variables | Haemophilia health‐care providers | Patient‐provider communication, patient perceptions of shared decision making and empowerment experiences | Eight subscales: patient participation, patient impact, meaning, health‐care professionals' information provision, emotional support, attentive listening, trust;' patients' collaboration | 29 items, 5‐point Likert scale |
| Veritas‐PRO communication subscale40, 62 | A patient‐reported questionnaire to assess patient adherence to prophylaxis regiment. It includes six subscales, one of which is “communication” | Haemophilia health‐care providers | Communication behaviours of the patient and their haemophilia treatment centre | 6 subscales: time, dose, plan, remember, skip, communicate | 4 items, 5‐point Likert scale |
| Wake Forest Trust in Physician Scale20 | A patient‐reported questionnaire to assess trust in physician | Physicians | Interpersonal Trust | Four domains: fidelity, competence, honesty, global trust | 10 items, 5‐point Likert scale |
| Working Alliance Inventory—Chronic Conditions42 | A tool to assess patient‐provider relationships in paediatric haematology. 20 forms were designed to assess from the perspective of adolescents, children, their parents, the physician and nurse practitioner | Physicians, nurse practitioners | Working Alliance | Three subscales: bonds, goals, tasks | 36 items, 7‐point Likert (adolescent and parent)12 items, 5‐point Likert scale (child) |
| Measurement tool | Related literature | Theoretical foundation of the tool | Internal consistency | Reliability | Measurement error | Content validity | Structural validity | Hypothesis testing | Cross‐cultural validity | Criterion Validity | Responsiveness | Interpretability |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hemofilia‐QoL32, 33 | von Mackensen68 | Based on the results of qualitative research on the factors that are considered important in quality of life | x | x | x | x | x | x | x | |||
| Hemo‐SAT specialist/nurses subscale31 | von Mackensen,69, 70 Gringeri71 | Based on the definition of Weave72r: Treatment satisfaction as the individual rating of important attributes of the process and outcomes of his treatment experience | x | x | x | x | ||||||
| Mountain States Patient Satisfaction Survey34 | NA | Four domains of interest based on literature review of patient satisfaction | x | x | x | |||||||
| Multi‐dimensional health locus of control scale35 | Wallston73 | Based on the theory that a person's locus of control has three dimensions, which are independent of one another: internal, external, and luck or chance | x | x | x | |||||||
| QUOTE‐Communication Questionnaire38 | Sixma,74 van den Brink‐Muinen,75 Valorie76 | Based on the conceptual framework for patient satisfaction of Sixma et al74 This scale included items from the “Patient Requests Form” of Valorie et al76 | x | x | x | x | x | x | ||||
| Theoretical Model of Deliberation Dialogues coding scheme39 | Bigi47 | The 3 stages in the “Theoretical Model of Deliberation Dialogues”—opening stage (topic or problem introduced); argumentation stage (solutions proposed, arguments for or against a proposal), closing stage (explicit agreement by one or both participants) | x | x | x | |||||||
| University of Oviedo Survey36, 37 | Chen,77 Lee & Lin,78 Warren‐Findlow,79 Fassaert,80 Briggs,81 Kriston82 | Authors considered relational dimensions of communication to design the survey, using items from validated measurement tools: “Diabetes Empowerment Process Scale”,77 “Trust in Physician Scale”,78, 83 “Active Listening Observation Scale”,77, 80 “Health Literacy Measurement Scale”,81 “9‐item Shared Decision Making Questionnaire” 82 | x | x | x | x | x | x | ||||
| Veritas‐PRO communication subscale40, 62 | Duncan,84 Lock,85 Rubén,86 Tran20 | Development was informed by data gathered from health‐care providers and patient focus groups | x | x | x | x | x | x | x | |||
| Wake Forest Trust in Physician Scale20 | Muller,87 Hall,88 Bachinger,89 Donnelly90 | Hall et al88 conceptualized model focused on interpersonal trust from a patient to a known primary care provider based on a review of theoretical and empirical literature from medical and nonmedical settings | x | x | x | x | x | x | x | |||
| Working Alliance Inventory—Chronic Conditions42 | Besley,45 Hall,43 Burns,44 Morris,46 Horvath and Greenberg60 | This tool was adapted from the “Working Alliance Inventory” in collaboration with its author. The original tool was developed using Bordin's Theory of Working Alliance in psychotherapy, which has three constituent components: bonds (feelings between), goals (valuing the outcomes that are targeted) and tasks (behaviours within the clinical encounter) | x | x | x | x | x | x | x | x | x |
The health‐care discipline for which the tool was developed.
The interpersonal construct measured by the tool.
3.3. Content comparison of the tools
We did not identify any tools that comprehensively measured the full scope of therapeutic relationship. Based on item content analysis, we distinguished six tools that measure a relationship construct as a primary domain: WAI‐CC, WFTPS, QUOTE, Veritas‐PRO, TMDD and UOvS. Three of the four other tools measured satisfaction with care.
The results of our item content analysis showed the WAI‐CC most comprehensively covers the components of therapeutic relationship framework, with 9 of 11 subcomponents represented, missing the subcomponents of “body as a pivot point” and “present.” The scope of the UOvS content was broad as well, capturing 7 of the 11 subcomponents. The WFTPS measured elements of the bond (trust, caring) and the conditions of engagement (receptive, genuine, committed). The items in the Veritas‐PRO, TMDD and QUOTE tools measured subcomponents of ways of establishing connections.
In terms of the three themes of therapeutic relationship, five of the six tools addressed the relationship as a mutual endeavour, and four of six tools addressed the body is central theme. A single tool attended to the personal aspect of therapeutic relationship (UOvS), while all tools examined professional aspects of therapeutic relationship. We compare the six relational tools in terms of functionality, content and measurement properties in Table 4.
Table 4.
A comparison of the relational tools from the haemophilia literature
| Measurement tool | Target population | Purpose of the tool | Content of the toola | Measurement propertiesb | Language |
|---|---|---|---|---|---|
| QUOTE‐Communication | Adult and paediatric patients before and after health‐care encounter | To evaluate patient satisfaction with relational communication during an encounter with a health‐care provider, by comparing patient communication expectations and experiences during encounter | “Establishing connections” (acknowledging the individual, body as a pivot point). Themes covered: professional dimension and body is central | Measurement properties have not been reported for a haemophilia population. Evidence of content and construct validity in medical outpatient populations | Dutch, French, Spanish, Flemish, German, English |
| Theoretical model of deliberation dialogues | Adult patients with haemophilia and health‐care providers | To describe shared decision making during an encounter between a health‐care provider and patient, using an interaction analysis coding scheme | “Establishing connections” (acknowledging the individual). Themes covered: mutuality professional | Content validity, inter‐rater reliability testing, coding scheme was developed in the haemophilia population | Italian |
| University of Oviedo Survey | Adult patients with haemophilia and health‐care providers | To discriminate between groups of patients with varying levels of different factors related to patient‐provider communication, shared decision making, and empowerment experience | “Establishing connections” (body as a pivot point, giving‐of‐self, acknowledging the individual), “elements of the bond” (trust), and “conditions of engagement” (receptive, committed). Themes covered: mutuality, professional, personal, body is central | Developed and tested in a haemophilia population. Shows evidence of reliability, content and construct validity | Spanish, English (translation not tested) |
| Veritas‐PRO—”Communication” subscale | Adult and paediatric patients with haemophilia on prophylaxis factor replacement therapy | To evaluate patient‐reported communication behaviours with respect to haemophilia treatment, and quantify change in adherence over time | “Establishing connections” (body as a pivot point). Themes covered: body is central | Developed and tested in a haemophilia population. Evidence of internal consistency, reliability and content validity | English, Dutch, German, Spanish |
| Wake Forest Trust in physician | Adult patients in medical outpatient and primary care settings and known health‐care provider | To discriminate between patients with varying levels of interpersonal trust towards a known health‐care provider | “Elements of the bond” (trust, caring), and “conditions of engagement” (receptive, genuine, committed). Themes covered: mutuality, professional, body is central | Measurement properties have not been reported for a haemophilia population. Internal consistency, reliability, content and construct validity have been tested in outpatient settings | English, Dutch, German, Spanish |
| Working Alliance Inventory—Chronic Conditionsc | Paediatric patients with chronic haematological conditions | To discriminate between patients with varying quality of working alliance with a known physician or nurse practitioner | “Establishing connections” (giving‐of‐self, acknowledging the individual), “Elements of the bond” (trust, caring, respect, rapport), and “conditions of engagement” (receptive, committed, authentic). Themes covered: mutuality, professional | The reliability and usability of this tool were tested in a general paediatric haematology clinic. The measurement properties of the original tool have been tested in the care of adults with diabetes and chronic low back pain | English |
Component(s) of the framework of therapeutic relationship measured by the items in the tool and the themes of therapeutic relationship covered by the tool.
Measurement properties tested and reported in the literature associated with the tool.
Content analysis was carried out on the original Working Alliance Inventory—long form because the adapted version was not available.
3.4. Outcomes of PPIE
PPIE impacted the study in two specific ways: (a) deciding to use the framework of therapeutic relationship; and (b) informing decisions about the scope of the study. In the design stage, the patient partner considered his experiences during clinical encounters to help us establish the applicability of a framework developed from research in a different patient population to patient‐provider relationships in haemophilia. Also, in early stages, the patient partner was involved in determining the scope of the study. The patient partner actively contributed to writing the project proposal as well as the final manuscript. He supported knowledge dissemination activities by attending scientific conferences where the project was presented and through discussions with peers in his network regarding the project. The patient partner also connected the researchers with other relevant health‐care providers in the community, creating opportunities for future collaboration.
The conception and design of the study and the scope of our research question were guided by informal discussions with health‐care providers working in HTCs. In addition, a peer‐review panel consisting mainly of clinicians from HTCs reviewed the project at the proposal stage, and we incorporated their feedback into the project design.
4. DISCUSSION
The purpose of this study was to provide an overview of the measurement of therapeutic relationship in the care of patients with haemophilia. We did not find any studies that measured the full scope of therapeutic relationship. From this, we concluded that no tool for the measurement of therapeutic relationship has been validated in this population.
Knowledge of the performance of a tool in the population of interest is necessary to inform the selection of outcome measures for research applications. The six tools identified in this review show promise as tools to measure subcomponents of therapeutic relationship in haemophilia. However, there is little evidence of the tools' measurement properties from haemophilia patient populations; therefore, further validation of these tools will be required to ensure the results from studies using these tools are valid.
We identified six tools that measure constructs that are part of therapeutic relationship. The features of each tool must be considered when selecting a tool for use in research. The WFTPS may be useful to researchers seeking to measure patient trust in their health‐care provider. It has performed well in studies in outpatient medical settings in both English and Dutch. Similarly, the QUOTE‐communication questionnaire could be used to measure patient satisfaction in studies of relationship‐focused models of care.
The WAI‐CC may be a useful tool to quantify working alliance between health‐care providers and patients with haemophilia. It has been used in the original form in studies of patients with chronic conditions such as low back pain and diabetes.43, 44, 45, 46 However, we identified two areas where the content of the tool is incomplete with respect to therapeutic relationship. The first relates to how patients and health‐care providers connect over the body—for example, how physical symptoms are assessed or addressed. This gap in the content of the tool may have significant implications in the care of patients with haemophilia, as a primary concern of patients and health‐care providers is to manage the musculoskeletal manifestations of the condition. The second gap in the content of the WAI‐CC relates to the “personal” theme in therapeutic relationship. The study of Vegni et al15 revealed a deep personal and professional involvement of haemophilia physicians with their patients,15 suggesting that the WAI, which does not address the personal dimensions of therapeutic relationship, may not adequately capture therapeutic relationship in haemophilia. Researchers43, 45 studying the content of the WAI in physical medicine and rehabilitation have also identified these two limitations.
The items in the UOvS have the potential to be useful in a comprehensive measure of therapeutic relationship. The content of the UOvS subscales is broad, and their measurement properties have been tested in the haemophilia population in Spain. Additionally, there are English and Mandarin translations of most items, which have been tested in populations with chronic conditions. Further measurement studies are needed to adapt the tool to assess therapeutic relationship quality or evaluate change over time.
The reliability and validity of the Veritas‐PRO have been tested in populations of patients with haemophilia. The usefulness of the communication subscale as a measure of therapeutic relationship is uncertain, in part because of the narrow focus of the four items in the scale.
There was one observer‐rating scale identified in this review, a coding schema based on the Theoretic Model of Deliberation Dialogues.47 Lamiani et al39 reported on the early development and testing stages of an interaction analysis coding for shared decision‐making communication between patients and physicians. The authors anticipate using the tool in a study of factors influencing adherence to treatment in haemophilia.39 The coding scheme may be useful in future studies requiring an objective measure of shared decision making during clinical encounters.
4.1. Gaps in knowledge and directions for future research
With this scoping review, we identified a need for a valid measure of therapeutic relationship in haemophilia. The first step will be to establish an understanding of the main elements of therapeutic relationship (ie a conceptual model) in the care of patients with haemophilia. This would provide a clear definition and scope of the relational construct being measured by a tool, and would provide a basis for deciding to use an existing tool, from another patient population (ie if the content of an existing tool adequately represents the conceptualization of therapeutic relationship). If an existing tool is not available, the conceptual model would provide a foundation for the development of a new tool.
There are measurement tools developed in other patient populations that could be useful in research with patients with haemophilia. A well‐known tool is the Caring and Relational Empathy (CARE) measure, a 10‐item measure developed for the evaluation of the “human aspects” of the quality of consultations (ie the ability of the health‐care provider to communicate an understanding of the patient's world and to act on that understanding in a therapeutic way).48 It has shown good measurement properties in various outpatient settings.49 The Healing Encounters and Attitudes Lists (HEAL) is a 57‐item measure of the “patient‐provider connection”.50 The HEAL measure has the advantage of being developed using item response theory, which offers greater flexibility and efficiency of measurement.50 Eveleigh et al provide an overview of 19 measurement tools that have been used to measure doctor‐patient relationships, but none of these have been tested in patients with haemophilia.24
Other considerations for future research include increasing efforts to test and report measurement properties in patients with haemophilia, and studying therapeutic relationship in developing countries. Researchers could make a more informed selection of measurement tools if measurement properties of existing relational tools used in haemophilia populations were known. Also, given the majority of studies we identified were completed in western Europe and North America, studying therapeutic relationship in developing countries should be considered.
This work is important because a validated measurement tool will improve research quality into the processes and mechanisms by which aspects of therapeutic relationship impact outcomes, such as pain, joint health and quality of life for patients with haemophilia. Given that therapeutic relationship is associated with adherence to treatment in haemophilia and that adherence impacts outcomes such as pain and joint health,19, 51 this a potential area of inquiry that could meaningfully improve the outcomes of care for patients with haemophilia.
4.2. Strengths and limitations of this study
We presented a robust overview of research and measurement tools and situate measurement of therapeutic relationship within the broader context of health service research in haemophilia. Also, we identified the knowledge gaps and directions for future research. Some key strengths of our study are that we used a systematic and reproducible search and selection strategy, and we assembled a research team with content and methodological expertise. Further, we clearly reported our approach to data analysis using a robust theoretical framework of therapeutic relationship.
There were two main advantages to using the framework. First, it added structure and transparency to the analysis of the tools' content. The framework was justified given the rigorous methods with which the framework was developed and that therapeutic relationship has not been conceptualized in the care of patients with haemophilia. Second, the framework helped identify a clear distinction between patient‐reported relationship scales and patient satisfaction scales. In an effort to include all available evidence of evaluation of therapeutic relationship, we included patient satisfaction with care as a measurement construct in this scoping study. It was important that we used a method that could distinguish the two constructs, because the use of patient satisfaction questionnaires to evaluate the quality of therapeutic relationships is generally not supported.52 In part, this is because general satisfaction questionnaires often fail to include items that assess emotional constructs in the proportions that reflect patients' true priorities in their care.52
A potential limitation of the study is that the framework of therapeutic relationship was developed in the context of physiotherapy for patients with musculoskeletal impairments, and the generalizability of the framework from physiotherapy to other health‐care disciplines has not been established. Physiotherapists typically focus on the body and physical condition, and parts of the framework might be more pertinent to physiotherapists (eg “body as pivot point”). However, haemophilia is a haematologic condition that often manifests in the musculoskeletal system. During clinical encounters, health‐care providers from all disciplines will be concerned with asking about physical symptoms, addressing issues related to the physical condition (eg experience of pain, joint bleeding), and how the patient experiences and is impacted by these physical problems. Therefore, the therapeutic relationship framework used is likely relevant to the care of patients with haemophilia by health‐care providers from all disciplines. Furthermore, the framework converges with the therapeutic relationship literature in haemophilia. Qualitative studies in haemophilia addressing a patient‐centred care model12 and haematologists' internal representations of difficult encounters with patients15 mirror Miciak's27 relationship components, as well as the framework's personal and professional theme.
Another potential limitation is the method of appraisal of the content of the items. The process involved the subjective judgement of the researchers, and it is possible that items in each measure would be classified differently by a different set of researchers. In addition, the choice of therapeutic relationship framework could impact the results of the content analysis of the measurement tools. Therapeutic relationship is a complex construct that can be conceptualized and organized differently, thereby impacting the classification of tools as relational. For instance, some frameworks are focused on concepts such as bonding,53 empathy,54 trust,55 or communication,56 and working alliance,30 while others are more broad, including contextual factors such as the health‐care environment,57 patient or health‐care provider factors such as the prerequisite knowledge and qualities of the health‐care provider, or patient expectations for care.58, 59 Despite these limitations, the results of the content analysis suggest that our method was suitable as there was a clear delineation between the tools classified as relational (proportion of relational items was 0.84 and above) and nonrelational tools (0.38 or lower). A final limitation is that one single researcher conducted the data extraction and content analysis steps; however, these were verified by another researcher.
4.3. Reflections on PPIE
The degree of PPIE in health research can range from a consultation‐type involvement to research that is completely led by the public. We engaged a single patient partner who is a graduate student at our institution, who was involved in the early stages (conception, design) and late stages (dissemination). The study could have been enriched by partnering with patients that represent a diversity of backgrounds and experiences or by involving patient partners at all stages of the research process. Despite this limitation, PPIE was an important component of this project, informing principal aspects and leading to a positive learning experience for all involved. The researchers had supportive and open attitudes towards partnering with a patient; however, they were not experienced in the implementation of PPI in practice. We attribute part of the success of PPI in this project to the patient partner's familiarity with research processes, which likely facilitated collaboration. The researchers recognize that a formal mentorship relationship between our research team and a patient‐oriented research organization would be useful in designing and conducting future projects. The aim of the mentorship would be to add structure to the involvement of patient partners, allowing patients who are not already part of the research community to be fully involved in research and to ensure the experience is meaningful for all involved.
5. CONCLUSIONS
In this scoping review, we sought to answer the question: “What validated measurement tool(s) exist for measuring the therapeutic relationship in the care of patients with haemophilia?” We did not find any measurement tools that have sufficient validity evidence to be used to measure therapeutic relationship in haemophilia care. We identified six tools that were used to measure aspects of therapeutic relationship, but were not comprehensive in scope. There is a need for a conceptually sound measurement tool of the therapeutic relationship to be validated in the care of patients with haemophilia.
CONFLICT OF INTEREST
The authors have no conflict of interests to declare.
AUTHOR CONTRIBUTIONS
E. McCabe, M. Miciak, D. Gross and L. Dennett conducted the literature search; E. McCabe, M. Miciak, D. Gross, L. Dennett, J. Hall, C. Guptill and T. Manns designed the research study; E. McCabe, M. Miciak and D. Gross analysed the data; E. McCabe, M. Miciak and D. Gross contributed to the drafting of the manuscript. All authors critically reviewed and approved the final version of the manuscript.
DISCLOSURE STATEMENT
EM received financial support for this project through a fellowship grant from the Canadian Hemophilia Society and Shire as well as an operating grant from Bayer Pharmaceuticals, Inc. EM holds a Bayer Hemophilia Awards Program research grant from Bayer Pharmaceuticals, Inc., and has served on advisory boards for Novo Nordisk and Pfizer. MM and DG have research funding from Bayer Hemophilia Awards Program. JH has participated in a leadership programme sponsored by Bayer Pharmaceuticals, Inc. TM, CG and LD have stated that they had no interests that might be perceived as posing a conflict or bias.
ACKNOWLEDGEMENTS
Thank‐you to Maria Tan, health research librarian, for her help conducting the search.
APPENDIX 1.
MEDLINE search strategy
| Topic | Population | Measurement instruments |
|---|---|---|
| 1. professional‐patient relations/ or nurse‐patient relations/ | 4. exp blood coagulation disorders, inherited/ | 6. (survey* or tool* or index or test* or instrument* or questionnaire* or scale* or psychometric* or validation or validity or factor analy* or health measurement or health measure or outcome measure or outcome assess* or evaluation).mp |
| 2. ((professional* or doctor* or physician* or nurs* or physiotherap* or physical therap* or social work* or caregiver* or care‐provider* or haemophilia treater* or provider* or hemophilia treater*) adj12 (patient* or client* or consumer* or haemophiliac* or hemophiliac*) adj8 (relation* or relationship* or alliance* or bond or communicat* or encounter* or interaction* or collaboration or trust or empathy or compassion* or responsiveness or caring)).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] | 5. (hemophilia* or haemophilia*).mp | 7. “weights and measures”/ or psychometrics/ or questionnaires/ |
| 3. (therapeutic alliance* or working alliance* or helping alliance or physiotherapeutic relationship* or therapeutic encounter* or therapeutic process* or patient‐centred* or patient‐centered* or shared decision making or patient satisfaction or quality of care or context* factor*).mp | 8. (1 or 2 or 3) and (4 or 5) and (6 or 7) |
APPENDIX 2.
Examples of item content appraisal
| Item | Component | Subcomponent | Reasoning |
|---|---|---|---|
| “You have no worries about putting your life in your doctor's hands” [WFTPS] | Elements of the Bond | Trust | The patient trusts the doctor's professional capabilities |
| “Your doctor will do whatever it takes to get you all the care you need” [WFTPS] | Conditions of Engagement | Committed | The patient believes the health‐care provider to be committed to taking action to help the patient |
| “I feel our doctor understands us and our problems” [Hemo‐SAT] | Conditions of Engagement | Receptive | The conditions created by the doctor are such that the patient feels understood |
| “Healthcare professionals help me improve my skills to deal with my illness” [UOv] | Ways of Establishing Connections | Using the body as a pivot point | Describes the information exchange between providers and patients having to do with the illness (physical body) |
| “The doctor gave me some help with my emotional problems” [QUOTE‐Communication] | Ways of Establishing Connections | Acknowledging the individual | The patient feels that their problems were acknowledged |
| “I always call the treatment center when I have questions about hemophilia or treatment.” [Veritas‐PRO] | Ways of Establishing Connections | Using the body as a pivot point | Describes accessing/communicating with providers about the disease |
| “We feel comfortable at the treatment center/hospital” [Hemo‐SAT] | Did not map | ‐ | Not an interpersonal concept |
| “I am satisfied with the physiotherapy services” [MSPSS] | Satisfaction with care | ‐ | Satisfaction with a service |
| “If I am lucky, my condition will improve” [MHLC] | Did not map | ‐ | Not an interpersonal concept |
| “I am genuinely concerned about how (the patient) feels.” [WAI‐CC] | Elements of the Bond | Caring | Describes an emotional investment in the patient's health on the part of the health‐care provider |
APPENDIX 3.
Content analysis of the tools. Results of item appraisal in reference to the components of the therapeutic relationship framework, or “satisfaction with care”
| Mapped to the framework (number of items) | Wake Forest Trust in Physician Scale | University of Oviedo survey | Mountain States Patient Satisfaction Survey | QUOTE Questionnaire | Multi‐dimensional health locus of control scale | Veritas‐PRO (communication subscale) | Theoretical model of deliberation dialogues | Hemofilia‐QoLa | Hemo‐SAT (physician/nurse subscale) | Working Alliance Inventory—Chronic Conditionsb |
|---|---|---|---|---|---|---|---|---|---|---|
| Ways of Establishing Connections | 0 | 10 | 4 | 10 | 4 | 4 | 1 | 0 | 17 | |
| Acknowledging the individual | 6 | 4 | 4 | 1 | 1 | 15 | ||||
| Giving‐of‐self | 1 | 2 | ||||||||
| Using the body as a pivot point | 3 | 6 | 4 | 3 | ||||||
| Elements of the Bond | 6 | 5 | 4 | 0 | 0 | 0 | 0 | 1 | 11 | |
| Respect | 4 | 4 | ||||||||
| Trust | 5 | 5 | 1 | 3 | ||||||
| Caring | 1 | 2 | ||||||||
| Nature of the rapport | 2 | |||||||||
| Conditions of Engagement | 4 | 9 | 6 | 0 | 0 | 0 | 0 | 1 | 10 | |
| Present | 4 | 0 | ||||||||
| Receptive | 1 | 3 | 2 | 1 | 7 | |||||
| Genuine | 2 | 1 | ||||||||
| Committed | 1 | 6 | 2 | |||||||
| Number of items that fitc | 10 | 24 | 14 | 10 | 4 | 4 | 1 | NA | 2 | 32 |
| Number of items in tool | 10 | 29 | 37 | 10 | 18 | 4 | 1 | NA | 7 | 36 |
| Comprehensiveness | ||||||||||
| Proportion of relationship itemse | 1.00 | 0.83 | 0.38 | 1.00 | 0.22 | 1.00 | 1.00 | NA | 0.29 | 0.89 |
| Components covered (of 3) | 2 | 3 | 3 | 1 | 2 | 1 | 1 | NA | 1 | 3 |
| Subcomponents covered (of 11) | 5 | 7 | 2 | 2 | 2 | 2 | 1 | NA | 3 | 9 |
| Component most often covered | Elements of the bond | Establish connections | NA | Establish connections | NA | Establish connections | Establish connections | NA | NA | Establish connections |
| Presence of themesd | ||||||||||
| Mutuality Y/N | Yes | Yes | No | No | Yes | No | Yes | NA | Yes | Yes |
| Professional Y/N | Yes | Yes | Yes | Yes | Yes | No | Yes | NA | Yes | Yes |
| Personal Y/N | No | No | No | No | No | No | No | NA | No | No |
| Body is central Y/N | Yes | Yes | No | Yes | Yes | Yes | No | NA | Yes | No |
Test items not available, item analysis not possible.
Item analysis carried out using the original long form of the Working Alliance Inventory, because the adapted version was not available.
Number of items coded to a component in the framework.
Determined by whether the content of the tool covers the themes in therapeutic relationship framework.
Proportion of relationship items over the total number of items in the tool.
McCabe E, Miciak M, Dennett L, et al. Measuring therapeutic relationship in the care of patients with haemophilia: A scoping review. Health Expect. 2018;21:1208–1230. 10.1111/hex.12827
Funding information
This study was financially supported by the Canadian Hemophilia Society, Shire, and Bayer Pharmaceuticals Inc.
This work was carried out in the Faculty of Rehabilitation Medicine at the University of Alberta. Department of Rehabilitation Science, 3‐48 Corbett Hall, Edmonton, Canada.
REFERENCES
- 1. Berntorp E, Piitulainen E, Lethagen S, Mattson E, Tengborn L, Matzsch T. Experience with a new percutaneous port system, Percuseal, for intravenous injection in patients with haemophilia, von Willebrand disease and severe alpha1‐antitrypsin deficiency. Haemophilia. 2003;9(2):173‐178. [DOI] [PubMed] [Google Scholar]
- 2. Pai M, Key NS, Skinner M, et al. NHF‐McMaster guideline on care models for haemophilia management. Haemophilia. 2016;22:6‐16. 10.1111/hae.13008. [DOI] [PubMed] [Google Scholar]
- 3. Griffin SJ. Effect on health‐related outcomes of interventions to alter the interaction between patients and practitioners: a systematic review of trials. Ann Fam Med. 2004;2(6):595‐608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kelley JM, Kraft‐Todd G, Schapira L, Kossowsky J, Riess H. The influence of the patient‐clinician relationship on healthcare outcomes: a systematic review and meta‐analysis of randomized controlled trials. PLoS ONE. 2014;9(4):e94207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Street RL, Makoul G, Arora NK, Epstein RM. How does communication heal? Pathways linking clinician‐patient communication to health outcomes. Patient Educ Couns. 2009;74(3):295‐301. [DOI] [PubMed] [Google Scholar]
- 6. Babatunde F, Macdermid J, Macintyre N. Characteristics of therapeutic alliance in musculoskeletal physiotherapy and occupational therapy practice: a scoping review of the literature. BMC Health Serv Res. 2017;17:1‐23. 10.1186/s12913-017-2311-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Srivastava A, Brewer AK, Mauser‐Bunschoten EP, et al. Guidelines for the management of hemophilia. Haemophilia. 2013;19(1):e1‐e47. [DOI] [PubMed] [Google Scholar]
- 8. Hermans C, Klamroth R, Richards M, et al. Outcome measures in European patients with haemophilia: survey of implementation in routine clinical practice, perception of relevance and recommendations by European treaters in the EHTSB. Haemophilia. 2017;23(2):222‐229. [DOI] [PubMed] [Google Scholar]
- 9. Steinhart B. Patient autonomy: evolution of the doctor‐patient relationship. Haemophilia. 2002;8(3):441‐446. [DOI] [PubMed] [Google Scholar]
- 10. HellÍn T. The physician‐patient relationship: recent developments and changes. Haemophilia. 2002;8(3):450‐454. [DOI] [PubMed] [Google Scholar]
- 11. Torres‐Ortuno A, Cid‐Sabatel R, Barbero J, et al. Life experience of the adult and ageing patient with haemophilia. Practical aspects for psychological support. Vox Sang. 2017;112(4):301‐309. [DOI] [PubMed] [Google Scholar]
- 12. Gue D, Squire S, McIntosh K, et al. Joining the patient on the path to customized prophylaxis: one hemophilia team explores the tools of engagement. J Multidiscip Healthc. 2015;8:527‐534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Grogan A, Coughlan M, O' Mahony B, Mckee G. The development of a patient partnership programme and its impact on quality improvements in a comprehensive haemophilia care service. Haemophilia. 2012;18(6):875‐880. [DOI] [PubMed] [Google Scholar]
- 14. Nilson J, Schachter C, Mulder K, et al. A qualitative study identifying the knowledge, attitudes and behaviours of young men with mild haemophilia. Haemophilia. 2012;18(3):e120‐e125. [DOI] [PubMed] [Google Scholar]
- 15. Vegni E, Leone D, Biasoli C, Moja EA. Difficult encounters with a hemophilic patient: the inner perspective of physicians. J Health Psychol. 2014;19(12):1499‐1507. [DOI] [PubMed] [Google Scholar]
- 16. Fillion E. How is medical decision‐making shared? The case of haemophilia patients and doctors: the aftermath of the infected blood affair in France. Health Expect. 2003;6(3):228‐241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fillion E. Clinical relationships tested by iatrogenicity: the case of haemophiliac patients faced with the epidemic of transfusional AIDS. Soc Sci Med. 2008;67(9):1400‐1409. [DOI] [PubMed] [Google Scholar]
- 18. Manco‐Johnson MJ, Sanders J, Ewing N, Rodriguez N, Tarantino M, Humphries T. Consequences of switching from prophylactic treatment to on‐demand treatment in late teens and early adults with severe haemophilia A: the TEEN/TWEN study. Haemophilia. 2013;19(5):727‐735. [DOI] [PubMed] [Google Scholar]
- 19. Mclaughlin JM, Witkop ML, Lambing A, Anderson TL, Munn J, Tortella B. Better adherence to prescribed treatment regimen is related to less chronic pain among adolescents and young adults with moderate or severe haemophilia. Haemophilia. 2014;20(4):506‐512. [DOI] [PubMed] [Google Scholar]
- 20. Tran DQ, Barry V, Antun A, Ribeiro M, Stein S, Kempton CL. Physician trust and depression influence adherence to factor replacement: a single‐centre cross‐sectional study. Haemophilia. 2016;23:98‐104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. de Moerloose P, Urbancik W, Van Den Berg HM, Richards M. A survey of adherence to haemophilia therapy in six European countries: results and recommendations. Haemophilia. 2008;14(5):931‐938. [DOI] [PubMed] [Google Scholar]
- 22. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19‐32. [Google Scholar]
- 23. Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Eveleigh RM, Muskens E, Van Ravesteijn H, Van Dijk I, Van Rijswijk E, Lucassen P. An overview of 19 instruments assessing the doctor‐patient relationship: different models or concepts are used. J Clin Epidemiol. 2012;65(1):10‐15. [DOI] [PubMed] [Google Scholar]
- 25. Streiner DL, Norman GR, Cairney J. Health Measurement Scales : A Practical Guide to Their Development and Use, 5th ed New York, NY: Oxford University Press; 2015. [Google Scholar]
- 26. Mokkink LB, Terwee CB, Patrick DL, et al. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health‐related patient‐reported outcomes. J Clin Epidemiol. 2010;63(7):737‐745. [DOI] [PubMed] [Google Scholar]
- 27. Miciak MA. Bedside matters: a conceptual framework of the therapeutic relationship in physiotherapy. 2015. https://era.library.ualberta.ca/files/9z903246q#.WEWHhmQrIfE. Accessed September 3, 2016.
- 28. Miciak M, Mayan M, Brown C, Joyce AS, Gross DP. The necessary conditions of engagement for the therapeutic relationship in physiotherapy: an interpretive description study. Arch Physiother. 2018;8(3):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Miciak M, Mayan M, Brown C, Joyce AS, Gross DP. A framework for establishing connections in physiotherapy practice. Physiother Theory Pract. In press. 10.1080/09593985.2018.1434707. [DOI] [PubMed] [Google Scholar]
- 30. Bordin ES. The generalizability of the psychoanalytic concept of the working alliance. Psychother Theory Res Pract. 1979;16(3):252‐260. https://doi.org/doi:10.1037/h0085885. [Google Scholar]
- 31. von Mackensen S, Campos IG, Acquadro C, Strandberg‐Larsen M. Cross‐cultural adaptation and linguistic validation of age‐group‐specific haemophilia patient‐reported outcome (PRO) instruments for patients and parents. Haemophilia. 2013;19(2):e73‐e83. 10.1111/hae.12054. [DOI] [PubMed] [Google Scholar]
- 32. Remor E, Arranz P, Quintana M, et al. Psychometric field study of the new haemophilia quality of life questionnaire for adults: the “Hemofilia‐QoL”. Haemophilia. 2005;11(6):603‐610. 10.1111/j.1365-2516.2005.01144.x. [DOI] [PubMed] [Google Scholar]
- 33. Arranz P, Remor E, Quintana M, et al. Development of a new disease‐specific quality‐of‐life questionnaire to adults living with haemophilia. Haemophilia. 2004;10(4):376‐382. 10.1111/j.1365-2516.2004.00918.x. [DOI] [PubMed] [Google Scholar]
- 34. Hacker MR, Primeaux J, Manco‐Johnson MJ. A patient satisfaction survey for haemophilia treatment centres. Haemophilia. 2006;12(2):163‐168. 10.1111/j.1365-2516.2006.01199.x. [DOI] [PubMed] [Google Scholar]
- 35. Triemstra AHM, Van der Ploeg HM, Smit C, Briet E, Ader HJ, Rosendaal FR. Well‐being of haemophilia patients: a model for direct and indirect effects of medical parameters on the physical and psychosocial functioning. Soc Sci Med. 1998;47(5):581‐593. [DOI] [PubMed] [Google Scholar]
- 36. del Río‐Lanza A‐BB, Suárez‐Álvarez L, Suárez‐Vázquez A, Vázquez‐Casielles R. Information provision and attentive listening as determinants of patient perceptions of shared decision‐making around chronic illnesses. Springerplus. 2016;5(1):1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Suárez Vázquez A, Del Río Lanza AB, Suárez Álvarez L, Vázquez Casielles R. Empower me? Yes, please, but in my way: different patterns of experiencing empowerment in patients with chronic conditions. Health Commun. 2017;32(7):910‐915. [DOI] [PubMed] [Google Scholar]
- 38. Lock J, De Bruin A, Scholten M, et al. The group medical appointment (GMA) in haemophilia and von Willebrand's disease: a new development in outpatient paediatric care. Haemophilia. 2012;18(5):766‐772. [DOI] [PubMed] [Google Scholar]
- 39. Lamiani G, Bigi S, Mancuso ME, Coppola A, Vegni E. Applying a deliberation model to the analysis of consultations in haemophilia: implications for doctor‐patient communication. Patient Educ Couns. 2017;100(4):690‐695. [DOI] [PubMed] [Google Scholar]
- 40. Miesbach W, Kalnins W. Adherence to prophylactic treatment in patients with haemophilia in Germany. Haemophilia. 2016;22(5):e367‐e374. [DOI] [PubMed] [Google Scholar]
- 41. Jacobson K, Hooke MC. Telehealth videoconferencing for children with hemophilia and their families: a clinical project. J Pediatr Oncol Nurs. 2016;33(4):282‐288. [DOI] [PubMed] [Google Scholar]
- 42. Ely B, Alexander LB, Reed M. The working alliance in pediatric chronic disease management: a pilot study of instrument reliability and feasibility. J Pediatr Nurs. 2005;20(3):190‐200. [DOI] [PubMed] [Google Scholar]
- 43. Hall AM, Ferreira ML, Clemson L, Ferreira P, Latimer J, Maher CG. Assessment of the therapeutic alliance in physical rehabilitation: a RASCH analysis. Disabil Rehabil. 2012;34(3):257‐266. [DOI] [PubMed] [Google Scholar]
- 44. Burns JW, Evon D. Common and specific process factors in cardiac rehabilitation: independent and interactive effects of the working alliance and self‐efficacy. Health Psychol. 2007;26(6):684‐692. [DOI] [PubMed] [Google Scholar]
- 45. Besley J, Kayes NM, McPherson KM. Assessing the measurement properties of two commonly used measures of therapeutic relationship in physiotherapy. N Z J Physiother. 2011;39(1):75‐80. [Google Scholar]
- 46. Morris L, Berry K, Wearden AJ, Jackson N, Dornan T, Davies R. Attachment style and alliance in patients with diabetes and healthcare professionals. Psychol Health Med. 2009;14(5):585‐590. [DOI] [PubMed] [Google Scholar]
- 47. Bigi S. The deliberation dialogue as a model to analyze shared decision making In: Communicating (with) Care: A Linguistic Approach to the Study of Doctor‐Patient Interactions. Amsterdam: IOS Press BV; 2016:59‐81. https://books.google.ca/books?id=uBfpDAAAQBAJ&pg=PA81&lpg=PA81&dq=The+power+of+words:+Deliberation+dialogue+as+a+model+to+favor+patient+engagement+in+chronic+care&source=bl&ots=VviaI385k2&sig=_-ik76Wnrfs2odAMi5NihZEXo_M&hl=en&sa=X-&ved=0ahUKEwiE9JK3krvUAhU. Accessed May 12, 2017. [Google Scholar]
- 48. Mercer SW, McConnachie A, Maxwell M, Heaney D, Watt GCM. Relevance and practical use of the Consultation and Relational Empathy (CARE) Measure in general practice. Fam Pract. 2005;22(3):328‐334. [DOI] [PubMed] [Google Scholar]
- 49. Kersten P, White PJ, Tennant A. The consultation and relational empathy measure: an investigation of its scaling structure. Disabil Rehabil. August 2011;2012(34):503‐509. [DOI] [PubMed] [Google Scholar]
- 50. Greco CM, Yu L, Johnston KL, et al. Measuring nonspecific factors in treatment: item banks that assess the healthcare experience and attitudes from the patient's perspective. Qual Life Res. 2016;25(7):1625‐1634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Manco‐Johnson M, Clark WM, Brooks W, et al. Prophylaxis versus episodic treatment to prevent joint disease in boys with severe hemophilia. N Engl J Med. 2007;357(6):535‐544. [DOI] [PubMed] [Google Scholar]
- 52. Greenhalgh T, Heath I. Measuring quality in the therapeutic relationship ‐ part 1: objective approaches. Qual Saf Health Care. 2010;19(6):475‐478. [DOI] [PubMed] [Google Scholar]
- 53. Tejero LMS. Development and validation of an instrument to measure nurse‐patient bonding. Int J Nurs Stud. 2010;47(5):608‐615. [DOI] [PubMed] [Google Scholar]
- 54. Mercer SW, Maxwell M, Heaney D, Watt GCM. The consultation and relational empathy (CARE) measure: development and preliminary validation and reliability of an empathy‐based consultation process measure. Fam Pract. 2004;21(6):699‐705. [DOI] [PubMed] [Google Scholar]
- 55. Hall MA, Zheng B, Dugan E, et al. Measuring patients' trust in their primary care providers. Med Care Res Rev. 2002;59(3):293‐318. [DOI] [PubMed] [Google Scholar]
- 56. Hovey R, Massfeller H. Exploring the relational aspects of patient and doctor communication. J Med Person. 2012;10(2):81‐86. 10.1007/s12682-012-0123-0. [DOI] [Google Scholar]
- 57. Greco CM, Glick RM, Morone NE, Schneider MJ. Addressing the “it is just placebo” pitfall in CAM: methodology of a project to develop patient‐reported measures of nonspecific factors in healing. Evid Based Complement Alternat Med. 2013;2013:1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Besley J, Kayes MN, McPherson MK. Assessing therapeutic relationships in physiotherapy: literature review. N Z J Physiother. 2011;39(2):81‐91. [Google Scholar]
- 59. Registered Nurses' Association of Ontario . Establishing Therapeutic Relationships. Toronto, ON: Registered Nurses' Association of Ontario; 2002. [Google Scholar]
- 60. Horvath AO, Greenberg LS. Development and validation of the working alliance inventory. J Couns Psychol. 1989;36(2):223‐233. [Google Scholar]
- 61. Carl F, Gribble TJ. HealthDesk for Hemophilia: an interactive computer and communications system for chronic illness self‐management. Proc Annu Symp Comput Appl Med Care. 1995:829‐833. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=medc&NEWS=N&AN=8563408. [PMC free article] [PubMed] [Google Scholar]
- 62. Lock J, Raat H, Peters M, et al. Optimization of home treatment in haemophilia: effects of transmural support by a haemophilia nurse on adherence and quality of life. Haemophilia. 2016;22(6):841‐851. [DOI] [PubMed] [Google Scholar]
- 63. Jarvinen O, Lehesjoki A‐EAA‐EA, Lindlof M, et al. Carrier testing of children for two X‐linked diseases: a retrospective evaluation of experience and satisfaction of subjects and their mothers. Genet Test. 1999;3(4):347‐355. [DOI] [PubMed] [Google Scholar]
- 64. Kalnins W, Schelle G, Jost K, Eberl W, Tiede A. Pain therapy in haemophilia in Germany. Hämostaseologie. 2015;35:167‐173. [DOI] [PubMed] [Google Scholar]
- 65. Kirtava A, Soucie M, Evatt B, et al. National haemophilia programme development in the Republic of Georgia. Haemophilia. 2005;11(5):529‐534. [DOI] [PubMed] [Google Scholar]
- 66. Page D, Crymble S, Lawday K, et al. Penny wise, pound foolish: an assessment of Canadian Hemophilia/inherited bleeding disorder comprehensive care program services and resources. Haemophilia. 2016;22(4):531‐536. [DOI] [PubMed] [Google Scholar]
- 67. Remor E. Development and psychometric testing of the hemophilia well‐being index. Int J Behav Med. 2013;20(4):609‐617. [DOI] [PubMed] [Google Scholar]
- 68. vonMackensen S , Gringeri A. Quality of life in hemophilia In: Preedy VR, Watson RR, eds. Handbook of Disease Burdens and Quality of Life Measures. Vol 2010 Springer Science & Business Media B.V.; 2010:1896 https://link-springer-com.login.ezproxy.library.ualberta.ca/content/pdf/10.1007%2F978-0-387-78665-0_112.pdf. Accessed August 8, 2017. [Google Scholar]
- 69. von Mackensen S, Gringeri AML. Development and validation of the first treatment satisfaction scale for adult haemophiliacs (Hemo‐SatA). Haemophilia. 2004;10(Suppl 3):126.15479385 [Google Scholar]
- 70. Dekoven M, Wisniewski T, Petrilla A, et al. Health‐related quality of life in haemophilia patients with inhibitors and their caregivers. Haemophilia. 2013;19(2):287‐293. [DOI] [PubMed] [Google Scholar]
- 71. Gringeri A, Mantovani L, Mackensen SV, et al. Quality of life assessment in clinical practice in haemophilia treatment. Haemophilia. 2006;12(Suppl 3):22‐29. [DOI] [PubMed] [Google Scholar]
- 72. Weaver M, Patrick DL, Markson LE, Martin D, Frederic I, Berger M. Issues in the measurement of satisfaction with treatment. Am J Manag Care. 1997;3(4):579‐594. [PubMed] [Google Scholar]
- 73. Wallston KA, Strudler Wallston B, DeVellis R. Development of the multidimensional health locus of control scales. Health Educ Monogr. 1978;6(2):160‐170. [DOI] [PubMed] [Google Scholar]
- 74. Sixma HJ, Kerssens JJ, van Campen C, Peters L. Quality of care from the patients' perspective: from theoretical concept to a new measuring instrument. Health Expect. 1998;1(2):82‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. van den Brink‐Muinen A, Verhaak PFM, Bensing JM, et al. Doctor–patient communication in different European health care systems: relevance and performance from the patients' perspective. Patient Educ Couns. 2000;39(1):115‐127. [DOI] [PubMed] [Google Scholar]
- 76. Valori R, Woloshynowych M, Bellenger N, Aluvihare V, Salmon P. The Patient Requests Form: a way of measuring what patients want from their general practitioner. J Psychosom Res. 1996;40(1):87‐94. 10.1016/0022-3999(95)00548-X. [DOI] [PubMed] [Google Scholar]
- 77. Chen M, Wang R, Cheng C, et al. Diabetes empowerment process scale: development and psychometric testing of the Chinese version. J Adv Nurs. 2011;67:204‐214. [DOI] [PubMed] [Google Scholar]
- 78. Lee YY, Lin JL. The effects of trust in physician on self‐efficacy, adherence and diabetes outcomes. Soc Sci Med. 2009;68(6):1060‐1068. [DOI] [PubMed] [Google Scholar]
- 79. Warren‐Findlow J, Seymour R, Huber L. The association between self‐efficacy and hypertension self‐care activities among African American adults. J Community Health. 2012;37:15‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Fassaert T, van Dulmen S, Schellevis F, Bensing J. Active listening in medical consultations: development of the Active Listening Observation Scale (ALOS‐global). Patient Educ Couns. 2007;68(3):258‐264. [DOI] [PubMed] [Google Scholar]
- 81. Briggs A, Jordan J, O'Sullivan P, et al. Individuals with chronic low back pain have greater difficulty in engaging in positive lifestyle behaviours than those without back pain: an assessment of health literacy. BMC Musculoskelet Disord. 2011;12:161‐171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Kriston L, Scholl I, Hölzel L, Simon D, Loh A, Härter M. The 9‐item Shared Decision Making Questionnaire (SDM‐Q‐9). Development and psychometric properties in a primary care sample. Patient Educ Couns. 2010;80(1):94‐99. [DOI] [PubMed] [Google Scholar]
- 83. Anderson LA, Dedrick RF. Development of the trust in physician scale: a measure to assess interpersonal trust in patient‐physician relationships. Psychol Rep. 1990;67:1091‐1100. [DOI] [PubMed] [Google Scholar]
- 84. Duncan NA, Shapiro AD, Ye X, Epstein J. Adherence to therapy among hemophilia patients in the U.S. Haemophilia. 2010;16:137. [Google Scholar]
- 85. Lock J, Raat H, Duncan N, et al. Adherence to treatment in a Western European paediatric population with haemophilia: reliability and validity of the VERITAS‐Pro scale. Haemophilia. 2014;20(5):616‐623. [DOI] [PubMed] [Google Scholar]
- 86. Cuesta‐Barriuso R, Torres‐Ortuño A, Galindo‐Piñana P, Nieto‐Munuera J, Duncan N, López‐Pina J. Validation of the VERITAS‐Pro treatment adherence scale in a Spanish sample population with hemophilia. Dovepress. 2017;11:653‐660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Müller E, Zill JM, Dirmaier J, Härter M, Scholl I. Assessment of trust in physician: a systematic review of measures. PLoS ONE. 2014;9(9):e106844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Hall MA, Camacho F, Dugan E, Balkrishnan R. Trust in the medical profession: conceptual and measurement issues. Health Serv Res. 2002;37(5):1419‐1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Bachinger SM, Kolk AM, Smets EM. Patients' trust in their physician‐Psychometric properties of the Dutch version of the “Wake Forest Physician Trust Scale”. Patient Educ Couns. 2009;76(1):126‐131. [DOI] [PubMed] [Google Scholar]
- 90. Donnelly V, Lynch A, Devlin C, et al. Therapeutic alliance in forensic mental health: coercion, consent and recovery. Ir J Psychol Med. 2011;28(1):21‐28. [DOI] [PubMed] [Google Scholar]


