Abstract
Background
Establishing patient safety priorities in psychiatry has received less international attention than in other areas of health care. This study aimed to identify safety issues as described by people in the United Kingdom identifying as mental health service users, carers and professionals.
Methods
A cross‐sectional online survey was distributed via social media. Identified safety issues were mapped onto the Yorkshire Contributory Factors Framework (YCFF) which categorizes factors that contribute to patient safety incidents in general hospital settings. Service user and carer responses were described separately from professional responses using descriptive statistics.
Results
One hundred and eighty‐five responses from 95 service users and carers and 90 professionals were analysed. Seventy different safety issues were identified. These were mapped onto the 17 existing categories of the YCFF and two additional categories created to form the YCFF‐MH. Most frequently identified issues were as follows: “Individual characteristics” (of staff) which included competence and listening skills; “Service process” that contained concerns about waiting times; “Management of staff and staffing levels” dominated by staffing levels; and “External policy context” which included the overall resourcing of services. Professionals identified staffing levels and inadequate community provision more frequently than service users and carers, who in turn identified crisis care more frequently.
Conclusions
This study updates knowledge on stakeholder perceived safety issues across mental health care. It shows a far broader range of issues relating to safety than has previously been described. The YCFF was successfully modified to describe these issues and areas for further coproduced research are suggested.
Keywords: attitude of health personnel, caregivers, health services research, inpatients, mental health services, patient safety, surveys and questionnaires
1. INTRODUCTION
1.1. Patient safety in health care
Improving patient safety has been a priority in health care for nearly two decades1 and the subject of a significant body of research and innovation. Patient safety in health care is a broad area, although typical interventions would be aimed at reducing medication errors, preventing hospital‐acquired infections, reducing falls or pressure sores and improving incident reporting.2 There has been a significant amount of research carried out to this end supporting numerous improvements to practice.3 In the pursuit of safety, the focus is on identifying negative outcomes and reducing the likelihood of their future occurrence; the publication of the Draft Health Service Safety Investigations Bill seeks to create a legal structure for this in England. To this end, researchers have sought to establish, based on the evidence, the factors that contribute to patient safety incidents. The Yorkshire Contributory Factors Framework (YCFF)4 was developed by reviewing 83 empirical studies of the factors causing different types of patient safety incidents, although only two included patient perspectives. It provides a unique and validated framework to describe factors that contribute to safety incidents in general hospital settings (although it has subsequently been adapted for use in primary care5) ranging from proximal, for example individual staff factors; to distal, for example organisational policy. One aim of the framework is to encourage risk managers and incident investigators to move beyond the proximal causes (e.g. violation of a rule or inexperience of the nurse) to a consideration of the local working conditions and the organisational culture in which patient safety incidents are more likely to occur.
Contrary to developments in general hospital care, there has been little parallel research into the identification of safety issues in mental health care services. Research into patient safety in mental health care has been dominated by the process of individual risk assessment with a focus on the prevention of suicide and homicide,6 an approach that can be incompatible with recovery‐orientated mental health care.7 Recent evidence has shown this individual risk assessment frequently does not involve the service user and their families and thus does not take into account their priorities.8 There have been three reviews of broader safety issues in mental health care; all identified similar issues including violence and aggression, suicide and self‐harm, seclusion and restraint, substance misuse and staff retention.9, 10, 11 All recommended further research to better identify and understand the issues so that effective interventions can be developed. A recent Delphi study primarily of professionals reported priorities for further research about safety in mental health care, and these included how service users might contribute to their own safety particularly if they self‐harm, individual safety planning and the reduction in restrictive practices.12
In the past decade, UK mental health services have continued to change at a rapid pace; detentions under the Mental Health Act have increased,13 inpatient beds reduced,14 staff numbers have fallen,15 yet perceptions of safety issues from the perspectives of service users and carers are largely unexplored. There has been little attention paid to this area in the United Kingdom, despite high‐profile failures in service provision,16 for example a mental health trust was the first to be prosecuted by the Care Quality Commission(CQC) after the Francis Report, (a public inquiry into care failures at Mid Staffordshire Foundation Trust17) for failing to provide safe care and treatment.18 In the first quarter of 2016, there were 223 276 patient safety incidents in mental health services,19 13% of all incidents recorded by the UK National Health Service(NHS). Furthermore, the CQC has reported that 40% of NHS core mental health services are either inadequate or require improvement in relation to safety. Key concerns were about physical environments, staffing, coercive practices and access to services including crisis care.20
This study aimed to identify current safety issues in UK mental health care as described by service users, carers and professionals.
2. METHODS
This was a cross‐sectional semi‐structured survey accessed by a web address distributed across the United Kingdom via social media (twitter). Twitter was selected as the primary method for distribution due to its ability for social reach into specific communities of interest, in this case mental health professionals, service users and carers. Using social media has been shown to be a cost‐effective and rapid way in which to recruit people into research, particular those from potentially stigmatised groups, and the peer network structures of platforms such as twitter mean that users can recruit other users.21 An invitation to take part in the survey was tweeted by the authors and retweeted in turn by their networks. No attempts were made to track the tweets, although anonymised traffic to the survey was monitored. Participants were eligible for inclusion if they were aged over 18, had recent experience (within the past two years) of using, caring for someone using, or working in mental health services.
2.1. Data collection
The electronic survey was created by the authors using the Bristol Online Survey platform which collates responses into a database and records IP addresses to prevent multiple responses from any one internet connection. The study was open between September and December 2016. The survey consisted of 18 questions specifically designed for this study. The questions about safety issues were consciously open and exploratory due to the broad range of potential safety issues identified both in the literature and during initial consultations with stakeholders. Participants were routed in one of three different ways depending on whether they primarily identified as a service user, carer or professional. The survey asked about demographic characteristics (age, gender, location), and asked for free‐text responses to the question: “Please tell me what you think are the things that affect safety in mental health care?” The full survey is published at https://doi.org/10.6084/m9.figshare.6300800.v1.
Approval for the study was granted by the University of Leeds, School of Healthcare Research Ethics Committee (ref. HREC15‐059). Information was provided about both the survey and sources of support at the beginning and consent was implied by completion and submission of the survey.
2.2. Data analysis
All the individual safety issues identified by participants were read and then coded by two researchers (KB and JB). Initial codes were generated, for example: “poor crisis support” or “alcohol on wards” resulting in 70 codes that accounted for all responses. These codes were then mapped onto the Yorkshire Contributory Factors Framework (YCFF) to aid interpretation. The decision to use the YCCF was made as it is theoretically based, there was no similar framework specific to mental health care available and it was not possible to develop one in the same way as there is not the primary research to draw upon. The framework consists of latent external factors (government policy), organisational factors (scheduling and bed management), local working conditions (staff workload), situational factors (individual staff) and active failures (mistakes), along with two cross‐cutting themes of communication and safety culture. The mapping of codes onto the YCCF was initially carried out by KB and JB and discrepancies discussed with RL (the original author of the YCCF), before amendments were made (described below) and consensus gained. The free‐text responses were coded using the modified YCCF (supported by Microsoft Excel) to provide illustration of individual issues.
The survey findings were numerically coded for analysis using SPSS 22,22 and descriptive statistics were used to describe the sample characteristics. Comparisons of service user and carer and professionals groups were conducted using chi‐square tests; further comparisons were carried out between those service users who had recently experienced inpatient treatment and those who had not, and between those staff whose recent employment was in inpatient services or community services.
2.3. Patient involvement in the design and conduct of the study
Mental health service user and carer representatives and other stakeholders (e.g. collective advocacy organisations, mental health professionals and policymakers) were involved throughout this study. The research aims arose from social media discussions with a range of people, including (ex)service users, family members, carers and professionals in a range of roles about improving and understanding key safety issues in mental health services. The subsequent survey was developed following discussions with (ex)service users about patient safety in mental health settings. A number of active social media campaigners, including (ex)service users, were contacted about the specific design and content of the survey. They provided feedback on the questions and participant information resulting in adaptations being made to the wording of the survey, and this continued when the survey was launched after feedback from respondents, for example the additional of an employment category. These individuals assisted with maximising response rates using their substantial networks to actively promote the distribution of the survey. Author MB is mental health design researcher, writer and consultant. MB has direct lived experience of mental health difficulty and 12 years of experience in developing and delivering mental health projects with a strong participatory element. He has been involved for the duration of the study having been part of the initial application for funding, codesigned the survey, led the distribution through social media and subsequently provided input into the analysis and reporting of this study.
3. FINDINGS
The survey received 188 responses from across the United Kingdom although three were excluded from the analysis as they were less than 50% complete. The analysed sample of 185 consisted of 90 professionals (48.6%), 77 service users (41.6%) and 18 carers (9.7%). For the purpose of analysis service, users’ and carers’ views were combined and presented separately from professionals. The demographic characteristics of the respondents are shown in Table 1.
Table 1.
Sample characteristics
| Service users and carers | Professionals | |||
|---|---|---|---|---|
| % | n | % | n | |
| Age | ||||
| 18‐25 | 15 | 14 | 1 | 1 |
| 26‐35 | 20 | 19 | 18 | 16 |
| 36‐45 | 19 | 18 | 31 | 28 |
| 46‐55 | 32 | 30 | 37 | 33 |
| 56‐65 | 13 | 12 | 13 | 12 |
| >65 | 1 | 1 | 0 | 0 |
| Gender | ||||
| Male | 23 | 22 | 29 | 26 |
| Female | 75 | 71 | 71 | 64 |
| Ethnicity | ||||
| White British | 76 | 72 | 72 | 65 |
| British Asian | 2 | 2 | 4 | 4 |
| White Other | 7 | 7 | 13 | 12 |
| Other | 4 | 4 | 2 | 2 |
| UK region | ||||
| North West | 11 | 10 | 18 | 16 |
| N. Yorks & Humber | 12 | 11 | 20 | 18 |
| South West | 7 | 7 | 8 | 7 |
| South East | 16 | 15 | 9 | 8 |
| London | 16 | 15 | 14 | 13 |
| East of England | 6 | 6 | 3 | 3 |
| East Midlands | 8 | 8 | 9 | 8 |
| West Midlands | 8 | 8 | 4 | 4 |
| Wales | 4 | 4 | 3 | 3 |
| Scotland | 8 | 8 | 7 | 6 |
| North East | 2 | 2 | 4 | 4 |
| Contact with services | ||||
| 2‐5 y | 33 | 31 | 16 | 14 |
| 6‐10 | 27 | 26 | 14 | 13 |
| 11‐15 | 19 | 18 | 19 | 17 |
| 16‐20 | 4 | 4 | 16 | 14 |
| >20 | 14 | 13 | 35 | 32 |
| Type of service contact in past 2 y | ||||
| CMHT inpatient services | 47 | 45 | 23 | 21 |
| GP | 17 | 16 | 31 | 28 |
| Voluntary | 25 | 24 | 6 | 5 |
| Organisation | 6 | 6 | 7 | 6 |
| Other | 3 | 3 | 29 | 26 |
There were more women than men in both groups and the majority of respondents described themselves as White British. The largest percentage of service users and carers (33%) had been in contact with services for five years or less with most of their contact over the previous two years with Community Mental Health Teams (CMHT) (48%), although 40% had experienced compulsory treatment in the past. Registered nurses were the largest professional group (n = 20; 22%), 17 respondents described themselves as managerial (18%) rather than by professional orientation. Service users and carers were asked to describe their mental health problem in their own words; many provided diagnoses but others used non‐diagnostic terms such as “severe and enduring” (21%). Nearly half said they experienced depression and anxiety (n = 38; 44%); 17% PTSD, 16% personality disorder, 10% schizophrenia and psychosis and 9% bipolar disorder.
3.1. Safety issues identified in mental health care
There were 796 individual responses identifying safety issues which after coding resulted in 70 first‐level categories. The majority of these codes fitted well within the YCCF but 20% did not. Following scrutiny of these codes by the author team, a decision was made to add two new categories. These were termed “Social environment” which took into account concerns about the social aspects of the service environment, for example other patients’ behaviour on mental health wards; and “Service process” which took into account both gaining access to and discharge from services, for example, not being able to access crisis care or being discharged from hospital before feeling suitably recovered. These were factors that the original YCCF did not address as it was derived exclusively from general hospital studies4 and this survey asked about experiences across all mental health services in both hospital and community because there can be regular transitions between both. The 70 categories were subsequently mapped onto the amended YCCF‐Mental Health (MH) (frequencies of category responses shown in Figure 1). Table 2 shows the full list of safety issues under all the YCCF‐MH headings and Table 3 the most frequently cited safety issues.
Figure 1.
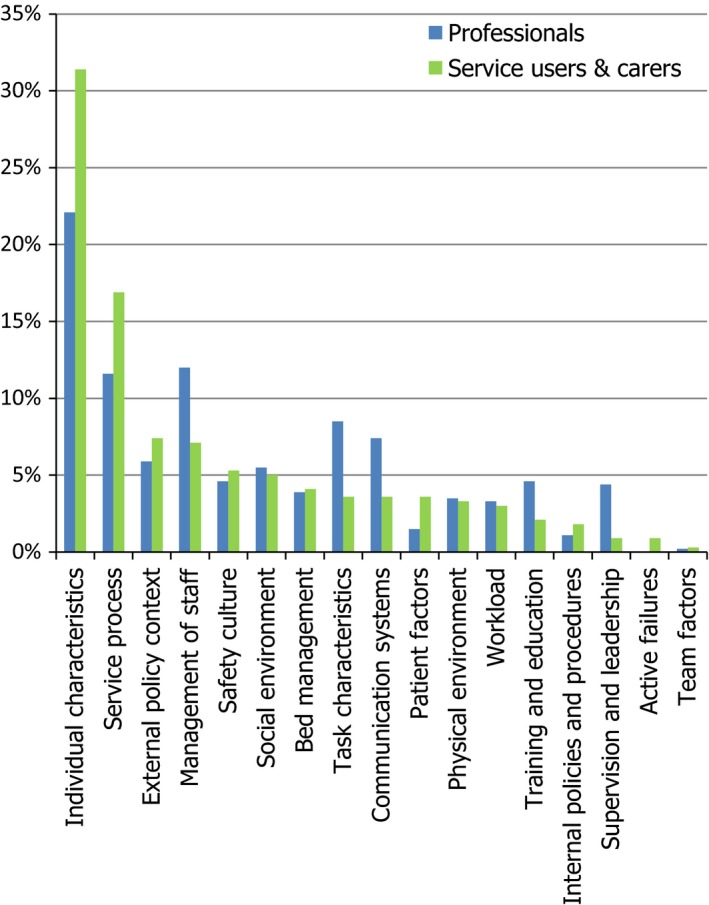
Summary of responses by YCCF‐MH category
Table 2.
List of 70 safety issues under YCCF‐MH headings
| YCCF‐MH and subcategories | Total | Service users and carers | Professionals | |||
|---|---|---|---|---|---|---|
| N of cases | % of cases | N of cases | % of cases | N of cases | % of cases | |
| Individual characteristicsa | 111 | 60 | 52 | 58 | 59 | 62 |
| Staff incompetence | 36 | 20 | 18 | 20 | 18 | 19 |
| Poor staff attitudes | 23 | 13 | 10 | 11 | 13 | 14 |
| Staff not listening | 20 | 11 | 5 | 6 | 15 | 16 |
| Staff not understanding | 20 | 11 | 7 | 8 | 13 | 14 |
| Staff lack of compassion | 17 | 9 | 7 | 8 | 10 | 11 |
| Staff burnout | 16 | 9 | 11 | 12 | 5 | 5 |
| Low quality of care | 15 | 8 | 6 | 7 | 9 | 10 |
| Lack of therapeutic relationships | 12 | 7 | 9 | 10 | 3 | 3 |
| Stigma from staff | 11 | 6 | 5 | 6 | 6 | 7 |
| Staff inexperience | 9 | 5 | 8 | 9 | 1 | 1 |
| Untrustworthy staff | 8 | 4 | 3 | 3 | 5 | 5 |
| Staff morale | 6 | 3 | 3 | 3 | 3 | 3 |
| Staff disbelieving | 2 | 1 | 1 | 1 | 1 | 1 |
| Staff having poor English | 2 | 1 | 1 | 1 | 1 | 1 |
| Service processa (New category for YCCF‐MH) | 70 | 38 | 32 | 36 | 38 | 40 |
| Waiting times | 33 | 18 | 12 | 13 | 21 | 23 |
| High threshold for support | 19 | 10 | 11 | 12 | 8 | 9 |
| Poor community provision | 15 | 8 | 10 | 11 | 5 | 5 |
| Poor crisis support | 11 | 6 | 1 | 1 | 10 | 11 |
| Poor continuity of care | 10 | 6 | 7 | 8 | 3 | 3 |
| Poor access to psychological therapies | 9 | 5 | 5 | 6 | 4 | 4 |
| No early intervention provision | 6 | 3 | 2 | 2 | 4 | 4 |
| Premature discharge from hospital | 6 | 3 | 5 | 6 | 1 | 1 |
| Poor transition from CAMHS | 1 | 1 | 0 | 0 | 1 | 1 |
| Management of staff and staffing levelsa | 69 | 37 | 47 | 52 | 22 | 23 |
| Low staffing levels | 65 | 36 | 47 | 52 | 18 | 19 |
| High use of agency/bank staff | 7 | 4 | 4 | 4 | 3 | 3 |
| High number of staff vacancies | 4 | 2 | 3 | 3 | 1 | 1 |
| No visible staff on wards | 3 | 2 | 1 | 1 | 2 | 2 |
| External policy contexta | 49 | 27 | 24 | 29 | 23 | 24 |
| Underfunding of mental health care | 36 | 20 | 15 | 17 | 21 | 23 |
| Societal stigma | 10 | 6 | 7 | 8 | 3 | 3 |
| Wider social problems | 7 | 4 | 5 | 6 | 2 | 2 |
| NHS targets | 4 | 2 | 3 | 3 | 1 | 1 |
| NHS policies | 3 | 2 | 3 | 3 | 0 | 0 |
| Legal issues | 2 | 1 | 1 | 1 | 1 | 1 |
| Task characteristicsa | 40 | 22 | 30 | 33 | 10 | 11 |
| Poor risk assessment | 31 | 17 | 23 | 26 | 8 | 9 |
| Poor care planning | 17 | 9 | 13 | 14 | 4 | 4 |
| Staff only able to “firefight” | 3 | 2 | 3 | 3 | 0 | 0 |
| Communication systemsa | 34 | 18 | 23 | 26 | 11 | 12 |
| Poor communication | 28 | 15 | 21 | 23 | 7 | 8 |
| Inaccurate information | 5 | 3 | 2 | 2 | 3 | 3 |
| Ineffective use of technology | 5 | 3 | 5 | 6 | 0 | 0 |
| Administration burden | 5 | 3 | 5 | 6 | 0 | 0 |
| Confidentiality | 2 | 1 | 0 | 2 | 2 | |
| Poor feedback mechanisms | 1 | 1 | 1 | 1 | 0 | 0 |
| Social environmenta (New category for YCCF‐MH) | 34 | 18 | 20 | 22 | 14 | 15 |
| Substance misuse | 11 | 6 | 9 | 10 | 2 | 2 |
| Patient acuity | 11 | 6 | 8 | 9 | 3 | 3 |
| Threats from other patients | 10 | 6 | 1 | 1 | 9 | 10 |
| Other patients boredom | 5 | 3 | 3 | 3 | 2 | 2 |
| Other patients self‐harming | 3 | 2 | 2 | 2 | 1 | 1 |
| Violence from other patients | 2 | 1 | 2 | 2 | 0 | 0 |
| Safety culturea | 29 | 16 | 15 | 17 | 14 | 15 |
| Service culture | 18 | 10 | 14 | 16 | 4 | 4 |
| Coercion by staff | 13 | 7 | 4 | 4 | 9 | 10 |
| Lack of coproduction | 4 | 2 | 2 | 2 | 2 | 2 |
| Poor complaints and whistleblowing procedures | 3 | 2 | 1 | 1 | 2 | 2 |
| Disregard for psychological safety | 1 | 1 | 0 | 0 | 1 | 1 |
| Bed managementa | 30 | 16 | 16 | 18 | 14 | 15 |
| Lack of inpatient beds | 26 | 14 | 14 | 16 | 12 | 13 |
| Use of out of area treatment | 5 | 3 | 4 | 4 | 1 | 1 |
| Placing children on adult wards | 1 | 1 | 0 | 0 | 1 | 1 |
| Physical environmenta | 23 | 12 | 15 | 17 | 8 | 8 |
| Unsafe environment | 22 | 12 | 15 | 17 | 7 | 8 |
| Access to ligature points | 5 | 3 | 1 | 1 | 4 | 4 |
| Staff workloada | 22 | 12 | 14 | 16 | 8 | 8 |
| Inadequate time with staff | 16 | 9 | 12 | 13 | 4 | 4 |
| Adequate monitoring on wards | 7 | 4 | 3 | 3 | 4 | 4 |
| Caseload size | 2 | 1 | 0 | 0 | 2 | 2 |
| Traininga | 26 | 14 | 19 | 21 | 7 | 7 |
| Inadequate staff training | 24 | 13 | 18 | 20 | 6 | 7 |
| Poor staff physical health training | 4 | 2 | 3 | 3 | 1 | 1 |
| Supervision and leadershipa | 20 | 11 | 17 | 19 | 3 | 3 |
| Poor supervision | 14 | 8 | 14 | 16 | 0 | 0 |
| Poor leadership | 9 | 5 | 6 | 7 | 3 | 3 |
| Patient factorsa | 17 | 9 | 6 | 7 | 11 | 12 |
| Medication issues | 16 | 9 | 6 | 7 | 10 | 11 |
| Increased MHA detentions | 3 | 2 | 1 | 1 | 2 | 2 |
| Policies and proceduresa | 11 | 6 | 5 | 6 | 6 | 6 |
| Poor carer support/involvement | 7 | 4 | 3 | 3 | 4 | 4 |
| Poor legal advice/advocacy | 4 | 2 | 2 | 2 | 2 | 2 |
| Active failuresa | 3 | 2 | 0 | 0 | 3 | 3 |
| Abuse from staff | 3 | 2 | 0 | 0 | 3 | 3 |
| Team factorsa | 2 | 1 | 1 | 1 | 1 | 1 |
| Poor teamwork | 2 | 1 | 1 | 1 | 1 | 1 |
Total number of cases referring to factor at least once.
Table 3.
Frequently identified safety issues
| YCCF | Total | Service users & carers | Professionals | |||
|---|---|---|---|---|---|---|
| N | % of cases) | N | % of cases) | N | % of cases) | |
| Individual factorsa | 111 | 60 | 59 | 62 | 52 | 58 |
| Staff competence | 36 | 19 | 18 | 20 | 18 | 19 |
| Staff attitudes | 23 | 13 | 13 | 14 | 10 | 11 |
| Staff not listening* | 20 | 10 | 15 | 16 | 5 | 6 |
| Staff not understanding | 20 | 10 | 13 | 14 | 7 | 8 |
| Staff lack of compassion | 17 | 9 | 10 | 11 | 7 | 8 |
| Staff burnout | 16 | 9 | 5 | 5 | 11 | 12 |
| Service processa | 70 | 38 | 38 | 40 | 32 | 36 |
| Waiting times | 33 | 18 | 21 | 23 | 12 | 13 |
| High threshold for support | 19 | 10 | 8 | 9 | 11 | 12 |
| Poor community provision | 15 | 8 | 5 | 5 | 10 | 11 |
| Poor crisis support** | 11 | 6 | 10 | 11 | 1 | 0 |
| Poor continuity of care | 10 | 6 | 3 | 3 | 7 | 8 |
| Management of staff & staffing levelsa | 69 | 37 | 22 | 23 | 47 | 52 |
| Poor staffing levels*** | 65 | 36 | 18 | 19 | 47 | 52 |
| External policy contexta | 49 | 27 | 23 | 24 | 26 | 29 |
| Underfunding of mental health care | 36 | 20 | 21 | 23 | 15 | 17 |
Total number of cases referring to factor at least once.
*95 CI 0.2404‐19.7624; χ2 = 4.645; P = .0311; **95 CI 2.6706‐18.1389; χ2 = 7.982; P = .0047; ***95 CI 18.7287‐45.9289; χ2 = 21.988; P < .0001.
“Individual (staff) factors” was the most frequently cited YCCF‐MH category of both service user and carers and professionals. The second YCCF‐MH categories differed between groups with service users describing “Service process” followed by “External policy context.” Professionals cited “Management of staff and staffing levels” as the second with “Service process” coming third.
Within the “Individual (staff) factors” category, both groups most frequently referred to staff competence followed by poor attitudes. Staff competence was often illustrated by respondents describing specific issues such as staff not being able to respond to service user distress:
Lack of skills, confidence, and knowledge of staff to deal with challenging behaviour and risk. Professional #159
Significantly more service users than professionals thought staff not listening was a safety issue (P < .05, see Table 1), some respondents described their views being dismissed:
Truly listening to service user/carers views rather than [saying] ‘well that's your perspective’. Service user #36
There were differences between the safety issues identified by staff depending on whether they worked in community or inpatient services. Significantly fewer inpatient staff gave responses related to individual staff characteristics as a safety issue (Difference 25; 95 CI 27.8169 to 65.4693; χ2 = 19.250; df 1; P < .0001).
The issue of burnout was more frequently identified by professionals; this was seen as undermining their ability to provide safe care:
Staff should be supported with adequate supervision, training and manageable case loads so that they do not experience burnout which can impact on patient safety. Professional #49
The new YCCF‐MH category of “Service process” had agreement between the two groups about waiting times and high thresholds for accessing support as being the main threats to service user safety within this category. Some service users reported being told their needs were not severe enough to receive a service and others of having to wait longer for more intensive support:
[I] was also told if my risk/need was lower I'd wait [a] much shorter [time] as more staff [would be] available. Service user #77
Significantly more service users were concerned about difficulties in accessing specific crisis support when in the community (P < .005, see Table 1), although professionals also identified lack of community services in general as a threat to safety, particularly for people moving back to the community from inpatient care:
Lack of resources result in service users being discharged from inpatient settings to community services that are unable to manage risk safely and provide continuity of care. Professional #116
A larger proportion of service users and carers with recent experience of community‐based services had identified issues relating to service process as a safety issue (Difference 35; 95 CI 4.4066 to 58.6881; χ2 = 6.476; df 1; P < .05).
The category of “Management of staff and staffing levels” was dominated by staffing numbers; the second commonest safety concern for professionals, identified significantly more frequently than by service users (P < .005, see Table 1):
Due to shortage of staff inpatients are not observed or interacted with… community patients are not seen enough resulting in care being delivered in crisis situation rather than planned work. Patients are being placed miles from home so staff have no previous knowledge and people are placed in inadequate community placements due to lack of alternatives. Professional #43
The service users and carers with recent experience of inpatient services were more likely to have identified short staffing as a safety issue (Difference 19; 95 CI‐1.8193 to 47.8663; χ2 = 4.544; df 1; P < .05). Correspondingly, a greater proportion of professionals currently employed in inpatient services also reported staffing levels to be a safety issue when compared with those working in the community (Difference 38; 95 CI 15.2331 to 54.7176; χ2 = 11.265; df 1; P < .05).
The category “External policy context” was dominated by concern about the safety implications of overall resourcing of mental health services. Both groups most frequently described this in terms of government cuts affecting mental health funding at local levels:
Inadequate services (as a result of poor funding and pressures caused by other service cuts) Professional #101
Overall, the defining feature of the majority of the safety issues raised by participants was their reference to staff characteristics:
…the risks are more caused by people/human error (quality of staffing and management) than broken equipment. Service user #124
4. DISCUSSION
This paper reports mental health service users’, carers’ and professionals’ views of current safety issues in UK mental health services, across both inpatient and community settings. The safety focus in mental health has been confined to risk, homicide, suicide and deaths. Broader research which considers systemic safety issues does not appear to have been as prolific as in other areas of health care in the last ten years.9, 10, 11 During this decade, there have been continuing constraints on services as a result of austerity measures13, 14, 15 and the issue of safety has dramatically increased in prominence after inquiries into care failures in the NHS in both general medicine and mental health care.17, 18
The data we present update the issues and demonstrate there is a far broader range of safety issues identified in mental health care services than the threat to self and others that underlies the dominant risk‐management approach within mental health services. These issues range from the distal such as under‐resourcing of NHS services, to the proximal such as interaction with the individual practitioner. Previous research reporting safety issues in mental health services has referred to only a small number of concerns, whereas we identified 70 different issues. The majority of those previously reported in a safety context locate the risk within the service user, for example, self‐harm, suicide and violence.11 These did feature but were not mentioned with any great frequency by this sample whose responses were dominated by staff factors such as incompetence, negative attitudes and poor listening skills. Locating the risk within the service user leads to a focus on physical safety, often managed through use of seclusion or restraint in inpatient settings, or detention under the Mental Health Act for those in the community. However, locating the threat within individual staff runs the risk of individualising a systemic problem. An under‐resourced system greatly increases the risk of burnout in individual staff, features of which include emotional exhaustion, detachment and poor mental health leading to poor care.23 Locating risk within a broader system context allows a broader consideration of safety issues, not limited to physical safety and carries with it the potential to promote positive outcomes.
These data identify that patients feel their safety is at greater risk from service failures such as poor interaction with staff and the impact of short staffing than they are from self‐harm or suicide. This might reflect service users’ perceived lack of influence over the care they receive, of the power imbalance between service providers and those who want or need to use them.24 Staff also spoke of poor attitudes and behaviours amongst their number, although this was often in the context of severe staff shortages making it almost impossible to give individual service users the time and attention they need. Significantly, fewer professionals working in inpatient services reported staff attitudes as a safety issue when compared with service user and carer perspectives. This finding is resonant of research comparing service user and staff ratings of the quality of therapeutic relationships where staff rated the quality higher than service users.25 This might suggest that professionals have a tendency to be overly optimistic about the nature of their interactions, an issue that might benefit from more reflexive practice or further investigation. Previous research about the triggers of incidents of aggression shows that interactions with staff are a primary cause.26 The disparity between service users’ and professionals’ perceptions of attitude as a safety issue may reflect why these encounters frequently trigger incidents. That both service users and professionals with experience of inpatient environments were more likely to report staffing levels as a safety issue implies that this is a particular concern in this setting, which is where the most severely ill service users are likely to be.
The inadequacy of community services as a safety issue was highlighted with service users reporting particular difficulties accessing crisis services and professionals perceiving all community provision as lacking, for example access to CMHTs, specialist teams and day services. There was a clearly perceived threat from the broader climate of reduced public spending that has led to cuts in overall mental health service provision, benefit entitlement and valued community services.
Mapping the responses onto the YCCF clarifies these priorities showing both groups concerns about individual staff factors, staffing levels and the related problems with service process. The amendments made to broaden the scope of the YCFF to include community services and take account of the importance of social as well as physical environment in mental health care provide a framework within which further research and interventions can be developed. One way in which it is feasible to involve patients in safety improvements is by encouraging them to provide feedback on the safety of the care they are receiving. One such tool that uses the YCFF as an underpinning framework is the Patient Measure of Safety now validated for use amongst all general hospital patients.27, 28 Similar work in mental health care using the YCCF‐MH may provide an opportunity for improving the safety of these services.
4.1. Recommendations for practice
This survey identified a wide range of concerns held by service users and professionals but they mostly fell into three categories: individual staff characteristics, service process and staffing levels, and there is a fundamental tension between them. Understaffed services will inevitably struggle to respond to service users’ needs due to constraints on professionals’ time and personal resources. This is not to say that all professionals have skills to deliver care in a compassionate and considerate manner, but that many that do are likely to be hampered by the circumstances in which they are working. That these individual staff characteristics were identified as safety issues is not something that has featured in the literature previously. Not being listened to, believed or feeling able to trust staff can make service users feel unsafe. This suggests these are important aspects of positive relationships and highlights the importance of professionals being able to develop them with service users and carers, but crucially that services are adequately resourced to make this possible. To make improvements to practice, it is recommended that direct collaboration takes place with service users to address the safety needs they have identified.
4.2. Limitations
There are limitations to using an opt‐in survey although it was widely publicised using twitter and resulted in a large number of respondents reporting experiences and perspectives. As with all surveys, there was little potential for verifying responses, particularly in a novel area such as this where there are no other data sets that might have been used for comparison. Using twitter as a recruitment mechanism runs the risk of reaching people with the same interests and views, an “echo chamber” effect which has been found to occur with political affiliations.29 However, social media users with interests in mental health care are by no means a homogenous group, the advantage of social media being that it provides an equal platform for people to participate in discussion from many different perspectives, including those often deemed “hard to reach” in traditional research sampling. Use of the internet allowed people to participate anonymously, which is of particular relevance to participants who may feel unable to publically state their concerns. The sample was also, of course, limited to those with internet access and the demographics showed that men, black, Asian and minority ethnic (BAME) groups were under‐represented. Additionally, the relatively low number of carer participants prevented separate analysis of this group who might have different needs to service users, as has been reported in research about suicide.30We used the term “carer” as we consider this a broad term that can include whoever identifies with this role. However, we appreciate that some family members or friends might not identify as carers despite still having significant involvement and therefore might not have responded to this survey. Further research should be targeted at these specific groups, particularly BAME service users as research has shown they are more likely to experience coercive measures and it may be that their experiences paint a starker picture still.
4.3. Future research
Future coproduced research should aim to explore these numerous safety issues in greater depth. Qualitative data would illuminate many of the issues and in turn inform the development of interventions to address systemic safety issues such as optimum staffing levels as well as individual staff factors such as burnout.
5. CONCLUSION
This study updates knowledge on patient safety issues in mental health care for the first time in over a decade. It shows that service users, carers and professionals have considerable concerns about the manner in which staff interact with service users, access to support and inadequate staffing levels. Future research should focus on coproducing interventions with service users and carers to improve safety in mental health carer services by focusing on these areas of concern.
COMPETING INTERESTS
The authors declare they have no competing interests.
ACKNOWLEDGEMENTS
We would like to thank all the people who participated in this study by sharing their views and experiences.
Berzins K, Baker J, Brown M, Lawton R. A cross‐sectional survey of mental health service users’, carers’ and professionals’ priorities for patient safety in the United Kingdom. Health Expect. 2018;21:1085–1094. 10.1111/hex.12805
Funding information
This study was funded by a grant awarded by the School of Healthcare Research Pump Priming Fund, University of Leeds. This research was supported by the National Institute for Health Research (NIHR) CLAHRC Yorkshire and Humber http://www.clahrc-yh.nihr.ac.uk and the NIHR Yorkshire and Humber Patient Safety Translational Research Centre (NIHR YH PSTRC). The views expressed in this article are those of the author(s) and not necessarily those of the University of Leeds School of Healthcare, the NHS, the NIHR, or the Department of Health and Social Care.
REFERENCES
- 1. Institute of Medicine . To Err is Human: Building a Safer Health System. Washington, DC: The National Academies Press; 2000. [PubMed] [Google Scholar]
- 2. World Health Organization . World Alliance for Patient Safety Progress Report 2006‐2007. 2008.
- 3. Shekelle PG, Pronovost PJ, Wachter RM, et al. The top patient safety strategies that can be encouraged for adoption now. Ann Intern Med. 2013;158:365‐368. [DOI] [PubMed] [Google Scholar]
- 4. Lawton R, McEachan RR, Giles SJ, Sirriyeh R, Watt IS, Wright J. Development of an evidence‐based framework of factors contributing to patient safety incidents in hospital settings: a systematic review. BMJ Qual Saf. 2012;21:369‐380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hernan AL, Giles SJ, Fuller J, Johnson JK, Walker C, Dunbar JA. Patient and carer identified factors which contribute to safety incidents in primary care: a qualitative study. BMJ Qual Saf. 2015;24:583‐593. [DOI] [PubMed] [Google Scholar]
- 6. Appleby L, Hunt IM, Kapur N. New policy and evidence on suicide prevention. Lancet Psychiatry. 2017;4:658‐660. [DOI] [PubMed] [Google Scholar]
- 7. Felton A, Stickley T. Rethinking risk: a narrative approach. J Ment Health Train Educ Pract. 2018;13:54‐62. [Google Scholar]
- 8. Coffey M, Cohen R, Faulkner A, Hannigan B, Simpson A, Barlow S. Ordinary risks and accepted fictions: how contrasting and competing priorities work in risk assessment and mental health care planning. Health Expect. 2017;20:471‐483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nath SB, Marcus SC. Medical errors in psychiatry. Harv Rev Psychiatry. 2006;14:204‐211. [DOI] [PubMed] [Google Scholar]
- 10. Brickell TA, Nicholls TL, Procyshyn RM, et al. Patient safety in mental health. Edmonton, Alberta: Canadian Patient Safety Institute and Ontario Hospital Association; 2009. [Google Scholar]
- 11. Hill K. Improving acute psychiatric services ‐ what is the NPSA contributing? Ment Health Rev J. 2006;11:27‐30. [Google Scholar]
- 12. NHS Digital . Inpatients Formally Detained in Hospitals Under the Mental Health Act 1983 and Patients Subject to Supervised Community Treatment, England ‐ 2014–2015, Annual figures. Leeds, UK: NHS Digital; 2015. [Google Scholar]
- 13. Dewa LH, Murray K, Thibaut B, et al. Identifying research priorities for patient safety in mental health: an international expert Delphi study. BMJ Open. 2018;8:e021361 10.1136/bmjopen-2017-021361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bell A, Hardie A, Morris Z, Ramanuj P, Watkins S. Briefing 52: Adult and older adult mental health services 2012–2016 An analysis of Mental Health NHS Benchmarking Network data for England and Wales. London: Centre for Mental Health; 2017. [Google Scholar]
- 15. The King's Fund . Mental Health under Pressure. London, UK: The King's Fund; 2015. [Google Scholar]
- 16. Care Quality Commission : CQC tells Southern Health NHS Foundation Trust to take urgent action to improve governance arrangements to ensure patient safety. http://www.cqc.org.uk/content/cqc-tells-southern-health-nhs-foundation-trust-take-urgent-action-improve-governance (2016). Accessed 10 October 2017.
- 17. Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. London, UK: The Stationery Office; 2013. [Google Scholar]
- 18. Care Quality Commission: Southern Health prosecution. https://www.cqc.org.uk/news/releases/southern-health-prosecution (2017). Accessed 10 October 2017.
- 19. NHS Improvement : National quarterly data on patient safety incident reports: March 2017. https://improvement.nhs.uk/resources/national-quarterly-data-patient-safety-incident-reports-march-2017/ (2017). Accessed 10 October 2017.
- 20. Care Quality Commission : The state of care in mental health services 2014 to 2017. http://www.cqc.org.uk/sites/default/files/20170720_stateofmh_report.pdf (2017). Accessed 10 October 2017.
- 21. Pedersen ER, Helmuth ED, Marshall GN, Schell TL, PunKay M, Kurz J. Using facebook to recruit young adult veterans: online mental health research. JMIR Res Protoc. 2015;4:e63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. IBM Corp . Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp. [Google Scholar]
- 23. Hannigan B, Edwards D, Coyle D, Fothergill A, Burnard P. Burnout in community mental health nurses: findings from the all‐Wales stress study. J Psychiatr Ment Health Nurs. 2000;7:127‐134. [DOI] [PubMed] [Google Scholar]
- 24. Farrelly S, Lester H, Rose D, et al. Barriers to shared decision making in mental health care: qualitative study of the Joint Crisis Plan for psychosis. Health Expect. 2016;19:448‐458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Simpson A, Coffey M, Hannigan B, et al. Cross‐national mixed methods comparative case study of recovery‐focused mental health care planning and coordination in acute inpatient mental health settings (COCAPP‐A). Health Serv Deliv Res. 2017;5:1‐234. [PubMed] [Google Scholar]
- 26. Bowers L. Safewards: a new model of conflict and containment on psychiatric wards: Safewards: description of the model. J Psychiatr Ment Health Nurs. 2014;21:499‐508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Giles SJ, Lawton RJ, Din I, McEachan RR. Developing a patient measure of safety (PMOS). BMJ Qual Saf. 2013;22:554‐562. [DOI] [PubMed] [Google Scholar]
- 28. McEachan RR, Lawton RJ, O'Hara JK, et al. Developing a reliable and valid patient measure of safety in hospitals (PMOS): a validation study. BMJ Qual Saf. 2014;23:565‐573. [DOI] [PubMed] [Google Scholar]
- 29. Krasodomski‐Jones A. Talking To Ourselves? Political Debate Online and the Echo Chamber Effect. London: Demos; 2016. [Google Scholar]
- 30. Fogarty AS, Spurrier M, Player MJ, et al. Tensions in perspectives on suicide prevention between men who have attempted suicide and their support networks: Secondary analysis of qualitative data. Health Expect. 2018;21:261‐269. [DOI] [PMC free article] [PubMed] [Google Scholar]


