Introduction
Erosive pustular dermatosis of the scalp (EPDS) is a disease that tends to affect elderly individuals with history of previous surgery, local trauma, actinic damage, burn injuries, and photodynamic therapy at the involved site.1 Diagnosis is typically made clinically. The exact etiology is unknown, but impaired immune and reparative properties associated with ultraviolet light damage have been postulated.1 EPDS is characteristically difficult to treat and has limited therapeutic options that include antibiotics and topical anti-inflammatory agents. The review by Starace et al1 of 20 scalp EPDS cases (mean age, 59 years; range, 18-95 years; male/female ratio, 1.8:1) reported an average disease duration of 53 months, with 35% of patients experiencing relapse after treatment cessation. The predisposing factor for the young patients (ages 18 and 25) was accidental trauma.1
With a prevalence of only 16.2 per million, lamellar ichthyosis (LI) is a rare autosomal recessive genodermatosis2 caused by a transglutaminase-1 mutation. Transglutaminase-1 is a skin barrier enzyme that crosslinks epidermal protein precursors to form impermeable cell envelopes within the stratum corneum.3 Individuals with LI present at birth with a collodion membrane, which later develops into dark, hyperkeratotic, platelike adherent scales.2
Case
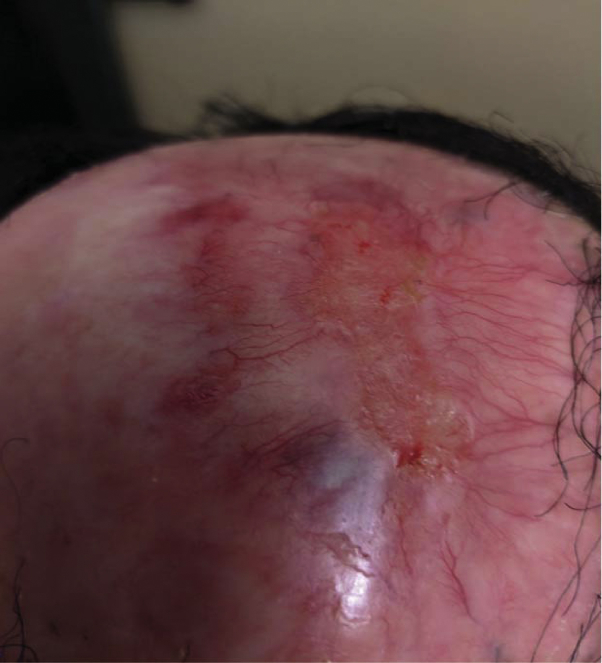
A 20-year-old man with LI and associated scarring alopecia presented for evaluation of a 7-year history of a 4- × 3-cm nonhealing eroded plaque with satellite pustules on the vertex of the scalp (Fig 1, A and B). The wound initially developed from chronic excoriations caused by scalp pruritus secondary to LI, which acutely worsened after a showerhead fell on his scalp. Multiple cultures showed Staphylococcus aureus colonization. Initial treatment before presentation to our service included hydroxyzine, griseofulvin, cephalexin, dapsone, and dilute bleach soaks, all with undulating improvement, but never full epithelialization.
Fig 1.
A, Erosive pustular dermatosis of the scalp at initial presentation: 4- × 3-cm beef-red erosion. Scarring alopecia is associated with lamellar ichthyosis. B, Pustules are associated with EPDS, even after initiation with intralesional triamcinolone treatment.
EPDS was further suspected after positive response to two 5-mg intralesional triamcinolone injections 4 weeks apart with concomitant clobetasol ointment application, resulting in moderate improvement but with persistent residual erosion. Finally, placement of a dehydrated human amnion/chorion membrane allograft (dHACM) (EpiFix; MiMedx, Marietta, GA) resulted in complete re-epithelialization within 12 weeks (Fig 2), without recurrence at 5-month follow-up.
Fig 2.
Three months after dHACM allograft placement. Prior eroded area is completely re-epithelialized. Neoangiogenesis is present at the allograft placement site.
Discussion
EPD and LI are both rare disorders, and concomitant EPD and LI makes this case exceedingly rare. To the best of our knowledge, there has been no prior report of EPD presenting in the context of LI. PubMed and Embase searches of “erosive pustular dermatosis” AND “lamellar ichthyosis” yielded zero results.
Although autologous skin grafting has long been a mainstay for full- and partial-thickness skin wounds, it is associated with significant donor site morbidity and has even instigated development of EPD at graft donor sites.1
The dHACM graft is an allograft composed of dehydrated human amnion and chorion membranes that modulates inflammation and acts as a barrier membrane to enhance healing.4 Fibroblast growth factor, epidermal growth factor, and transforming growth factor-α are released from the graft to regulate inflammation and to promote angiogenesis, cell proliferation, and extracellular matrix deposition.4 Although silicone gel wound dressing has shown anti-inflammatory and bacteriostatic properties in cases of recalcitrant erosive pustular dermatosis, complete re-epithelialization was expedited with the dHACM graft (3 months versus 5 months).5
The recalcitrant and chronic nature of this wound is owing to the impaired skin barrier and increased inflammatory marker profile observed in EPD and LI, with increased expression of tumor necrosis factor-α and interleukin-17 in the latter.6 These inflammatory mediators may contribute directly to impaired skin barrier function and increased transepidermal water loss in LI, predisposing LI patients to skin breakdown.6 Matrix metalloproteinases have been implicated in chronic wounds, and have been cited sparingly with EPDS.7 Reports of successful treatment with infliximab for superficial granulomatous pyoderma, a similar trauma-induced chronic wound condition, suggest a possible role of tumor necrosis factor in chronic scalp wound pathogenesis.7 Additionally, follicular destruction caused by this patient's LI likely prevented stem cell production, resulting in impaired wound healing. Future investigations are warranted to explore the role inflammatory mediators have on wound repair defects and cutaneous appendages in EPDS.7
Footnotes
Kempton and Maarouf contributed equally to this article.
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Starace M., Loi C., Bruni F. Erosive pustular dermatosis of the scalp: Clinical, trichoscopic, and histopathologic features of 20 cases. J Am Acad Dermatol. 2017;76(6):1109–1114.e1102. doi: 10.1016/j.jaad.2016.12.016. [DOI] [PubMed] [Google Scholar]
- 2.Hernandez-Martin A., Garcia-Doval I., Aranegui B. Prevalence of autosomal recessive congenital ichthyosis: a population-based study using the capture-recapture method in Spain. J Am Acad Dermatol. 2012;67(2):240–244. doi: 10.1016/j.jaad.2011.07.033. [DOI] [PubMed] [Google Scholar]
- 3.Boeshans K.M., Mueser T.C., Ahvazi B. A three-dimensional model of the human transglutaminase 1: insights into the understanding of lamellar ichthyosis. J Mol Model. 2007;13(1):233–246. doi: 10.1007/s00894-006-0144-9. [DOI] [PubMed] [Google Scholar]
- 4.Koob T.J., Rennert R., Zabek N. Biological properties of dehydrated human amnion/chorion composite graft: implications for chronic wound healing. Int Wound J. 2013;10(5):493–500. doi: 10.1111/iwj.12140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Uva L., Aphale A.N., Kehdy J., Benedetto A.V. Erosive pustular dermatosis successfully treated with a novel silicone gel. Int J Dermatol. 2016;55(1):89–91. doi: 10.1111/ijd.13066. [DOI] [PubMed] [Google Scholar]
- 6.Paller A.S., Renert-Yuval Y., Suprun M. An IL-17-dominant immune profile is shared across the major orphan forms of ichthyosis. J Allergy Clin Immunol. 2017;139(1):152–165. doi: 10.1016/j.jaci.2016.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ibrahim O., Arndt K.A., Dover J.S. Pathophysiology and Treatment Considerations for Erosive Pustular Dermatosis. JAMA Dermatol. 2017;153(10):971–972. doi: 10.1001/jamadermatol.2017.2897. [DOI] [PubMed] [Google Scholar]