Abstract
Background
Anhydrous ethanol, for its part, has been successfully used to treat renal cyst, hepatocellular carcinoma and ovarian chocolate cyst et al. However, in spite of the high frequency of tuberculous purulent pleural effusion, we found that only a few very early studies that attempted to assess the use of intrapleural anhydrous ethanol in tuberculous effusions with signs of empyema. We report a patient who was injected anhydrous ethanol into pleural cavity to treat chronic tuberculous empyema.
Case presentation
A 23-year old male was admitted in the hospital because of chronic tuberculous empyema. Ultra-sonography guided thoracentesis and thoracic close drainages were done, but had no effect. However, the patient refused Video-assisted Thoracoscopic Surgery (VATS) and traditional thoracotomy. Therefore, we injected anhydrous ethanol into the pleural cavity after getting the patient's consent. Pyothorax was quickly controlled and the patient finally recovered fully.
Conclusion
Surgical operation is the main treatment of chronic tuberculous empyema, which has a high cost and large injury, and many patients do not accept this treatment. In this study, intrapleural injection of anhydrous ethanol could achieve the purpose of eliminating the pus cavity, which is particularly suitable for patients who cannot tolerate surgery or are unwilling to undergo surgical treatment.
Keywords: Tuberculous, Chronic empyema, Anhydrous ethanol
1. Background
China is still one of the high burden TB countries [1]. Therefore, China also has a relatively high prevalence of tuberculous empyema. Tuberculous empyema is caused by Mycobacterium tuberculosis infection. Chronic empyema can seriously affect the heart and lung function of patients because it causes pleural fibrosis, calcification, intercostal space narrowing, chest deformity and mediastinal shift. The treatment principle of chronic empyema is eliminating infection and pus cavity, recovering pulmonary function. Eradicating pus cavity is essential for treatment [2]. The efficacy of video-assisted thoracic surgery (VATS) in empyema management have been evaluated in several studies showing favourable results [[3], [4], [5]], less is known about the role of intrapleural anhydrous ethanol, which appears to be safe and successful in tuberculous empyema treatment. It is also lower in cost and better tolerated in frail patients than VATS which has a relatively greater trauma.
2. Case report
A 23-year-old man was admitted in a local general hospital on Dec. 12, 2015, because of complaints of chest tightness, shortness of breath, and dyspnea starting a week prior. He was diagnosed as bilateral tuberculous pleural effusion. Anti-tuberculosis treatment with four drugs (rifampin, isoniazid, pyrazinamide, and ethambutol) and thoracentesis therapy were given, and the specific volume of fluid was unknown. After a month the patient stopped pyrazinamide by himself. The left pleural effusion was controlled, but the right pleural effusion recurred repeatedly. Because of chest tightness and wheezing, the patient was referred to our hospital on March 29, 2016. Pyrazinamide rejoined the anti-TB regimen. On the day of admission and April 3, about 500 ml and 300 ml of pyogenic pleural effusion were respectively removed from the right pleural cavity, and operations were forced to stop because of severe chest pain. Ultra-sonography guided thoracentesis and thoracic close drainages were done, but there was no effect. Chest CT still showed right thoracic pleural effusion (Fig. 1) and pleural purulent fluid grew Mycobacterium tuberculosis until June 2016. However, the patient refused VATS and traditional thoracotomy. Therefore, we injected anhydrous ethanol into pleural cavity after getting the patient's consent on July 5, 2016. Pyothorax was controlled after 6 intrapleural injections of anhydrous ethanol. Table 1 shows volumes, methods of draining and characteristics of pleural effusion.
Fig. 1.
CT-scan images of right pleural effusion on Jun 28, 2016.
Table 1.
Vol, methods of draining and characteristics of pleural effusion.
| Date | Volume of pleural effusion (mL) | Method of draining pleural effusion | Characteristics of pleural effusion |
|---|---|---|---|
| Mar. 29, 2016 | 500 | Thoracentesis | Purulent |
| Apr. 3, 2016 | 300 | Thoracentesis | Purulent |
| Apr. 8, 2016 | 150 | Thoracentesis | Purulent |
| Apr. 11- Jun. 10, 2016 | 100-200/Day | catheter drainage | Purulent |
| Jun. 15, 2016 | 120 | Thoracentesis | Purulent |
| Jun. 17, 2016 | 110 | Thoracentesis | Purulent+Bloody |
| Jun. 30, 2016 | 150 | Thoracentesis | Purulent+Bloody |
| Jul. 5, 2016a | 120 | Thoracentesis | Purulent |
| Jul. 20, 2016a | 100 | Thoracentesis | Purulent |
| Aug. 5, 2016a | 60 | Thoracentesis | Purulent |
| Sep. 3, 2016a | 30 | Thoracentesis | Purulent |
| Oct. 8, 2016a | 20 | Thoracentesis | Purulent |
| Nov. 1, 2016a | 15 | Thoracentesis | Purulent |
| Dec. 12, 2016 | 10 | Thoracentesis | Purulent |
Anhydrous ethanol was retained in the pleural cavity, waiting for the next fluid extraction.
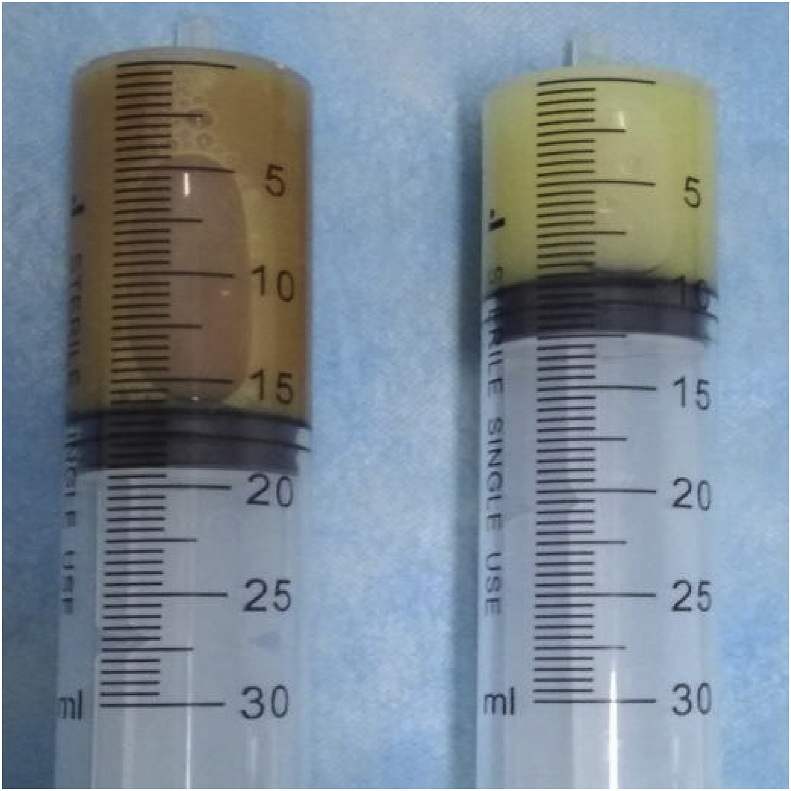
Intrapleural injection of anhydrous ethanol: After obtaining the patient's consent, centesis of pleural effusion guided by color Doppler ultrasound was performed. The first step: drain pleural fluid as much as possible; The second step: normal saline was injected into and drawn away from the pleural cavity. The amount of normal saline used for irrigation of the pleural cavity was the same volume as pus removed (For example, if we draw out 100ml pus, we should inject 100ml normal saline into the pleural cavity). We washed the pleural cavity with normal saline in order to determine whether the patient had bronchopleural fistula. The third step: 10–15 ml of anhydrous ethanol was injected every time, rinsing the pleural cavity repeatedly (Fig. 2), until the liquid was clear. No normal saline was used in this process. Finally: 10–15 ml of anhydrous ethanol was retained in the pleural cavity, waiting for the next fluid extraction.
Fig. 2.
Liquid drawn out from pleural cavity after anhydrous ethanol was injected.
We repeated the procedure every 1–2 weeks in the first month and every 2–4 weeks in the following months until color Doppler ultrasound showed no pleural effusion. It should be stressed in particular that we must observe whether the patient has a severe cough while washing the pleural cavity with normal saline. If the patient coughs out salty liquid, it suggests that the patient may have bronchopleural fistula, and we should stop washing the pleural cavity and the injection of anhydrous ethanol. If necessary, intrapleural injections of methylene blue will further confirm whether there is bronchopleural fistula or not. Of course, it is best to ask patients if they have any history of alcohol allergy before intrapleural injection of anhydrous ethanol.
The patient stopped antituberculous treatment in June 2017 and finally recovered fully. Re-examination of lung CT showed that the patient's right pyothorax was significantly improved on February 23, 2018 (Fig. 3). Meanwhile, color Doppler showed only pleural thickening without pleural effusion.
Fig. 3.
CT-scan images showed that the pyothorax was significantly improved on Feb. 23, 2018.
3. Discussion
Tuberculous pleural effusion is the most common pleural disease in China. If treatment is not timely and chemotherapy is not standardized, the complications such as chronic encapsulated effusion and tuberculous empyema can form. Tuberculous empyema is a chronic pleural cavity infection with pleural thickening and adhesions, poor drug penetration, easy to form dead cavity, and hard to cure. The course of chronic empyema is more than 3 months when pleural pus become viscous and difficult to be extracted. We report our success in injecting anhydrous ethanol into the pleural space in order to cure and prevent the recurrence of tuberculous empyema.
There are few reports on application of anhydrous ethanol in treatment of tuberculous chronic empyema in China and abroad [6,7]. The treatment of chronic tuberculous empyema with anhydrous ethanol may be related to the following mechanisms. First, anhydrous ethanol can solidify the protein in order to reduce the viscosity of pus, which make pus easy to be extracted. In vitro, we also confirmed this by adding anhydrous ethanol to the pus (Fig. 4). Secondly, anhydrous ethanol can kill bacteria and prevent the continuous generation of pus. Finally, anhydrous ethanol stimulates the purulent cavity, producing a wide range of aseptic inflammatory reactions, promoting pleural adhesion and purulent cavity closure. But it should be emphasized that the indication of ethanol injection is purulent cavity without bronchopleural fistula which needs surgical or bronchial stent treatment [8].
Fig. 4.
Pus drawn out from pleural cavity (A); Added anhydrous ethanol in vitro (B).
Why tPA and DNAase combination was not used? it has shown to improve drainage and also decrease the viscosity at the same time in an infected pleural space. We use anhydrous ethanol to solve two problems: 1. decrease the viscosity in order to improve drainage; 2. kill bacteria and prevent the continuous generation of pus. The tPA and DNAase combination can only deal with the first problem, and the process needs to wait for several hours or even 24 hours, but no need to wait after injection of anhydrous ethanol. It has significant curative effects to injecting tPA and DNAase combination into encapsulated pleural effusion and early empyema, but it does not work well for this stubborn chronic empyema. We also treated tuberculous empyema by intrapleural injection of normal saline, urokinase and sodium bicarbonate injection. These methods are only effective in the treatment of early empyema. We have treated more than ten cases of chronic tuberculous empyema by intrapleural injection of anhydrous ethanol. These patients had very good short-term effects, but no long-term curative effects were observed, or had no complete data. We report this case because the information is complete. We think it is a safe, effective and cheap treatment which is worth promoting.
Conflicts of interest
There are no conflicts of interest for any of the above authors.
Funding
Medical research projects of Health and Family Planning Commission of Wuhan Municipality. Project number: WX17Q28.
Contributions
Initial idea, drafting and finalising manuscript: Qi Nie, Li-xuan Tao, Sheng-jin Tu, Yuan Wei, Ge Yao, Cai-hong Li, Wen-juan Wu, Ding-yu Zhang.
Final approval
Qi Nie, Li-xuan Tao, Sheng-jin Tu, Yuan Wei, Ge Yao, Cai-hong Li, Wen-juan Wu, Ding-yu Zhang.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rmcr.2018.11.001.
Contributor Information
Li-xuan Tao, Email: nieqitlx@163.com.
Ding-yu Zhang, Email: 3180001668@qq.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.World Health Organization . World Health Organization; Geneva, Switzerland: 2018. Global Tuberculosis Report 2018 [Internet]http://www.who.int/tb/publications/global_report/en/ c, [cited 2018 Sep 18]. Available from: [Google Scholar]
- 2.Koh M., Yoshioka Y., Yoshikawa K. Spontaneous esophageal rupture treated with staged operations. Jpn. J. Thorac. Cardiovasc. Surg. Aug, 2003;51(8):390–392. doi: 10.1007/BF02719475. [DOI] [PubMed] [Google Scholar]
- 3.Elsayed H.H., Mostafa A., Fathy E., Diab H.S., Nofal I.M., AbdelHamid O.A., El-Bawab H.Y., ElNori A.A. Thoracoscopic management of early stages of empyema: is this the golden standard? J. Vis. Surg. 2018;4:114. doi: 10.21037/jovs.2018.05.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bilgin M., Akcali Y., Oguzkaya F. Benefits of early aggressive management of empyema thoracis. ANZ J. Surg. 2006;76:120–122. doi: 10.1111/j.1445-2197.2006.03666.x. [DOI] [PubMed] [Google Scholar]
- 5.Chambers A., Routledge T., Dunning J. Is videoassisted thoracoscopic surgical decortication superior to open surgery in the management of adults with primary empyema? Interact. Cardiovasc. Thorac. Surg. 2010;11:171–177. doi: 10.1510/icvts.2010.240408. [DOI] [PubMed] [Google Scholar]
- 6.EPSTEIN I.G., LOBAIDO F., NAIR K.G., SCHLOSS J. Ethyl alcohol lavage treatment of tuberculous empyema. Sea View Hosp. Bull. 1956 Jul;16(2):52–61. [PubMed] [Google Scholar]
- 7.Zhu Zao-rong, Chen Dian-he. Alcohol washing and retention for tuberculous empyema [J] J. Chin. Antituberc. Assoc. 1966;7(2):105–106. 131. [Google Scholar]
- 8.Chan Brian YO., Chan Canon KO. Retrievable endoscopic stenting for tuberculous oesophagopleural fistula with empyema. Hong Kong Med. J. 2017;23:89–92. doi: 10.12809/hkmj154670. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.