Abstract
Ionizing radiation therapy is a common adjuvant therapy for individuals undergoing surgery for breast cancer. There are many well-recognized acute and chronic cutaneous reactions that can vary in severity, course and duration. We present a rare cutaneous manifestation of systemic mastocystosis, in a 59-year-old female who underwent adjuvant radiotherapy following local excision of ductal carcinoma in situ.
INTRODUCTION
Mastocytosis is a diverse group of conditions characterized by the proliferation of a clonal population of mast cells in various tissues such as the liver, spleen, gastrointestinal tract and lymph nodes. Nettleship and Tay originally described mastocytosis in 1869 as a skin condition presenting with maculopapular lesions with an urticaria like response to rubbing or scratching [1].
In 1949, Ellis described systemic mastocytosis (SM) with the involvement of multiple organ systems [2]. The World Health Organisation now recognizes three forms of mastocytosis including mast cell sarcoma, cutaneous mastocytosis (CM) and SM when bone marrow infiltration is present. The exact aetiology of mastocytosis remains unclear. However the diagnosis once established, requires careful surveillance given the potential for leukaemic transformation.
CASE REPORT
A 59-year-old female presented for investigation of a rash located over the left breast, left submammary region and right breast. It consisted of multiple 2–3 mm, red-brown macules that were asymptomatic and non-blanching, however demonstrated dermographism (fig. 1). The eruption developed 9 years after adjuvant radiotherapy of a locally excised breast ductal carcinoma in situ (DCIS), which progressively spread over to the contralateral breast. She had undergone a wide local excision for 20 mm high grade DCIS followed by post-operative radiotherapy delivering 50 Gy in 25 fractions followed by 10 Gy in 5 fractions.
Figure 1:

Rash on the left breast, left submammary area and medial right breast, composed of multiple monomorphic erythematous macules.
A diagnosis of mastocytosis was made by skin biopsy. Histopathology revealed a localized increased concentration of mast cells demonstrated on a toluidine blue stain.
Further investigations demonstrated an elevated serum tryptase of 24.7 mcg/l. Molecular testing was positive for the activating KIT D816V mutation, a mutation which is found in the majority of patients with SM.
A bone marrow aspirate and trephine biopsy demonstrated a diffuse infiltrate of spindle-shaped MCs (Fig. 2). Investigations for other organ involvement were negative. The patient was diagnosed with SM and started on prophylactic anti-histamine therapy and apart from occasional night sweats, remains well.
Figure 2:
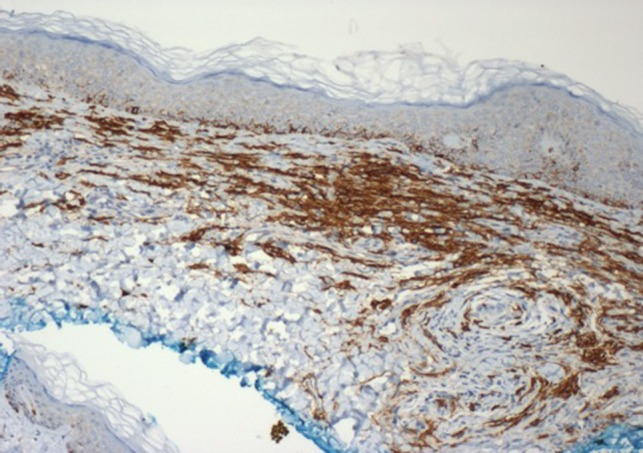
Immunoperoxidase CD117 (c-KIT) stained tissue section of a skin biopsy of the left breast. Mast cell cytoplasmic membrane is stained brown (×10 magnification).
DISCUSSION
CM is divided into four main subtypes including urticaria pigmentosa, solitary mastocytoma, diffuse mastocytosis and telangiectasia macularis eruptive perstans. CM is usually diagnosed in childhood and commonly associated with a good prognosis. In contrast SM has a variable prognosis ranging from a benign disorder with normal life expectancy to a rapidly deteriorating disorder with evolution to leukaemia. This complicates decision making with regards to the choice and timing of interventions [3].
SM is a rare entity. The diagnosis is based on the presence of one major criterion and one minor criterion or three minor criteria. Major criteria include the presence of multifocal infiltrates of greater than 15 mast cells in aggregates in bone marrow. Minor criteria include:
The presence of elevated serum alpha tryptase levels >20 ng/ml
The expression of CD2 and CD25 surface markers in c-kit positive mast cells from bone marrow or other organs
The presence of c-kit mutations in bone marrow and/or other tissue mast cells
The presence of >25% abnormal mast spindle-shaped cells in bone marrow and/or tissue [4]
A systematic literature search was conducted using the databases of Pubmed, Medline, EMBASE and Cochrane library databases for articles between 1946 and 2018. Searches were performed using medical subject heading terms and the free keywords (‘Mastocystosis’) AND (‘Breast Cancer’ OR ‘Breast Carcinoma’ OR ‘Breast Tumour’) AND (‘Radiotherapy’ OR ‘Radiation Therapy’ OR ‘Radiation Field’). The reference lists of retrieved articles were manually scrutinized to identify potentially relevant articles. Our search revealed that mastocytosis associated with a radiotherapy field after breast surgery, has only been reported in six cases in the literature [5–9]. All occurred in female patients who had breast cancer and were treated with surgery and adjuvant radiotherapy. All were presentations of CM in patients aged between 43 and 62. The clinical presentations were similar to our patient with multiple red-brown macules predominantly confined to skin overlying the radiation field. A positive Darier’s sign was elicited in two out of six patients. All demonstrated skin histology revealing a focal accumulation of mast cells. The interval between radiotherapy and the development of skin changes consistent with mastocytosis ranged from 3 to 24 months. The management of CM is comprised of avoiding triggers of mast cell degranulation and pharmacotherapy centred on antihistamines and leukotriene modifying agents. Short duration topical corticosteroids and narrow band UVB phototherapy have been used in refractory cases with anecdotal evidence also existing to support the use of topical cromoglycate ointments [10]. To our knowledge, this is the first case of SM in an individual with CM presenting after surgery and radiotherapy for breast cancer.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Nettleship E, Tay W. Rare forms of urticaria. Br Med J 1869;2:323–4. [Google Scholar]
- 2. Ellis JM. Urticaria pigmentosa. A report of a case with autopsy. AMA Arch Pathol 1949;48:426–9. [PubMed] [Google Scholar]
- 3. Lim K, Tefferi A, Lasho TL, Finke CM, Patnaik MS, Butterfield JH, et al. Systemic mastocytosis in 342 consecutive adults: survival studies and prognostic factors. Blood 2009;113:5727–36. [DOI] [PubMed] [Google Scholar]
- 4. Valent P, Akin C, Metcalfe DD. Mastocytosis: 2016 updated WHO classification and novel emerging treatment concepts. Blood 2017;129:1420–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Soilleux EJ, Brown VL, Bowling J. Cutaneous mastocytosis localized to a radiotherapy field. Clin Exp Dermatol 2008;34:111–2. [DOI] [PubMed] [Google Scholar]
- 6. Comte C, Bessis D, Dereure O, Guillot B. Urticaria pigmentosa localized on radiation field. Eur J Dermatol 2003;13:408–9. [PubMed] [Google Scholar]
- 7. MacDonald A. Cutaneous mastocytosis: an unusual radiation dermatitis. Proc R Soc Med 1971;64:29–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Davidson S. Cutaneous mastocytosis extending beyond a radiotherapy site: a form of radiodermatitis or a neoplastic phenomenon? Australas J Dermatol 2013;54:e85–7. [DOI] [PubMed] [Google Scholar]
- 9. Dalmasso C, Tournier E, De Lafontan B, Modesto A, Dalenc F, Chantalat E, et al. Uncommon dermatologic disorders triggered by radiation therapy of breast cancer: a case-series. Cancer Radiother 2017;21:216–21. [DOI] [PubMed] [Google Scholar]
- 10. Alvarez-Twose I, Vañó-Galván S, Sánchez-Muñoz L, Morgado JM, Matito A, Torrelo A, et al. Increased serum baseline tryptase levels and extensive skin involvement are predictors for the severity of mast cell activation episodes in children with mastocytosis. Allergy 2012;67:813–21. [DOI] [PMC free article] [PubMed] [Google Scholar]


