Abstract
Transmesenteric hernia is a rare cause of small bowel strangulation in adults and, to our knowledge, no one has reported the existence of two mesenteric defects in an adult. Our patient was a 73-year-old Japanese woman who presented to our emergency department complaining of abdominal pain and nausea. Computed tomography with contrast enhancement revealed a closed loop obstruction in the pelvis, suggesting small bowel strangulation due to an internal hernia. The emergency exploratory laparotomy indicated a small bowel strangulation caused by a transmesenteric hernia. With the examination across whole parts of the mesentery, we identified another small defect. Both defects were closed by suture intraoperatively, and the patient’s postoperative course was satisfactory. Searching for whole parts of the mesentery after the reduction of a hernia can help prevent the recurrence of internal hernias.
INTRODUCTION
A transmesenteric hernia is a rare cause of small bowel strangulation in adults [1]. This clinical state is usually diagnosed intraoperatively; few critical imaging findings have been reported [2]. Although the sizes of the mesenteric defects reported to date varied significantly, all of the reported adult cases showed only one defect. We experienced an adult case of a transmesenteric hernia with two mesenteric defects. We closed both of the defects intraoperatively.
CASE REPORT
A 73-year-old Japanese woman presented to our emergency department with a 72-hr history of abdominal pain and nausea. Her surgical history included appendectomy and total hysterectomy. Her vital signs on admission were as follows: blood pressure 141/89 mmHg, pulse 76 bpm, temperature 36.9°C. The physical examination revealed lower abdominal tenderness without any peritoneal irritation signs. Laboratory tests included a slightly elevated white blood cells count (9.0 × 103/μl) and C-reactive protein (2.14 mg/dl). Abdominal X-ray showed distended loops of small bowel (Fig. 1).
Figure 1:

The abdominal X-ray showing distended loops of small bowel.
Computed tomography (CT) with contrast enhancement revealed a closed loop obstruction located in the pelvis (Fig. 2). In addition, the slightly decreased bowel wall enhancement of the closed loop and the moderate volume of ascites indicated bowel ischemia (Fig. 2). As these findings suggested small bowel strangulation due to an internal hernia, we performed an emergency exploratory laparoscopy.
Figure 2:
(a) Contrast-enhanced coronal CT image showing a closed loop obstruction located in the pelvis (arrowheads), a slightly decreased bowel wall enhancement of the closed loop, and a moderate volume of ascites. (b) Another coronal slice of CT revealing the change in caliber (arrow) and a whirl sign.
At the laparoscopy, the view was too narrow to identify the strangulated bowel due to dilated small bowel, which forced us to convert the procedure to a laparotomy. Through a lower midline incision, we observed that approximately 25 cm of the small bowel had gone through a 2.5-cm defect located in the distal ileal mesentery (Fig. 3). By enlarging the defect to 3.0 cm, the affected bowel was successfully reduced. We confirmed the preserved bowel viability and averted bowel resection.
Figure 3:
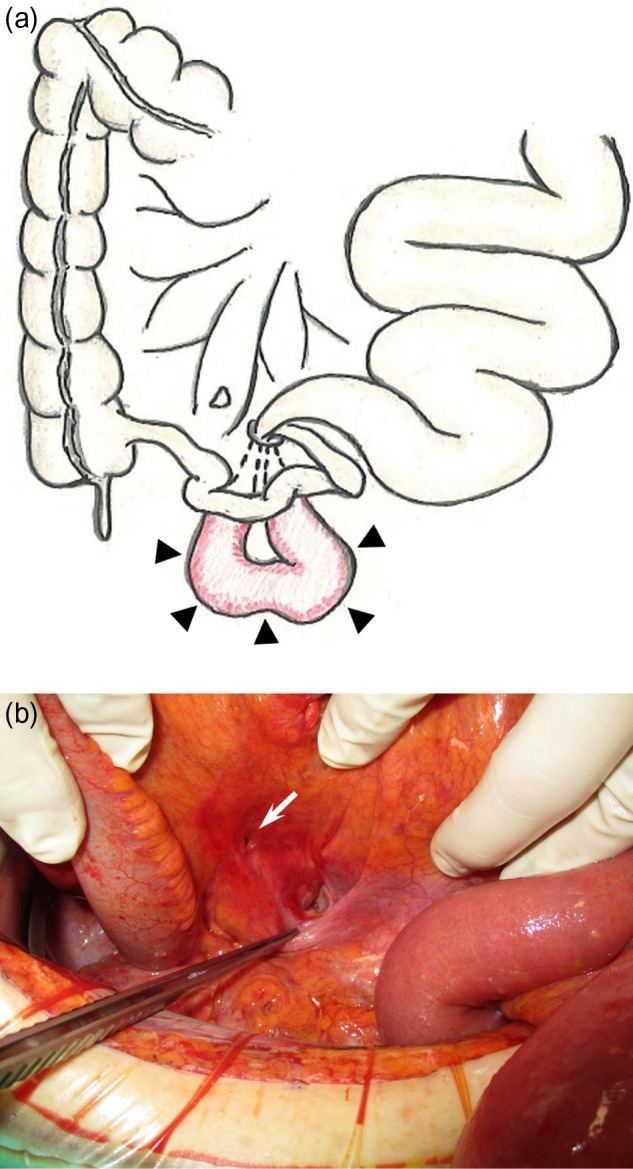
(a) Schema showing strangulated herniation (25 cm long) observed 210 cm from the ligament of Treitz (arrowheads). (b) Intraoperative photograph after reduction. The herniated small bowel had been reduced from the mesenteric defect (2.5 cm), which is pointed to by the forceps. Another defect (1.0 cm, arrow) just distal to the previously identified defect. Both defects had no adhesion around them, and the serous membrane fully covered the marginal lines of the defects.
Based on the examination across whole parts of the mesentery, we identified another small defect (1.0 cm) just distal to the previously identified defect (Fig. 3). The two mesenteric defects had very smooth marginal lines and no adhesion around them. Both defects were closed with 3.0 non-absorbable sutures. After the recovery of her bowel movements was confirmed, the patient resumed oral intake on postoperative Day 6. She was discharged uneventfully 21 days after the operation.
DISCUSSION
A transmesenteric hernia is one of the types of narrowly defined internal hernias that are known to be a relatively uncommon cause of small bowel obstruction [1]. Mesenteric defects are observed in approximately 0.5% of all autopsies [3]. Some cases of transmesenteric hernias have been reported in pediatric patients, whereas adult cases have rarely been reported [1]. Transmesenteric hernias in adult patients occur more frequently after a surgery such as gastro-intestinal reconstruction [4]. Congenital mesenteric defects are very rare in adults but can cause an internal hernia followed by an incarceration or strangulation of small intestines [1].
A transmesenteric hernia can occur based on congenital factors or acquired factors [5]. One of the hypotheses regarding congenital causes of mesenteric defects was described by Treves in 1885. He noted a part of the mesentery near the terminal ileum which was circumscribed by the junction of the ileocolic artery and the last branch of the ileal artery. This area, later named Treves’ field, was reported to contain no fat, no visible blood vessels, and no lymph nodes, making it highly susceptible to injury during development [6].
The reported acquired causes of mesenteric defects are blunt abdominal trauma and surgical manipulation of the bowel and mesentery [5]. In our patient’s case, although she denied any history of trauma, her past surgical histories indicated a possibility of iatrogenic pathogenesis. However, a congenital pathogenesis of the defects in her case seemed much more likely, for the following two reasons: (i) the operative findings revealed that no adhesion existed around the two mesenteric defects, and the serous membrane fully covered the marginal lines of the defects and (ii) both defects were located in the mesentery near the terminal ileum where congenital defects often appear.
The preoperative diagnosis of a transmesenteric hernia is often challenging due to the non-specific symptoms and to the poor sensitivity and specificity of imaging devices including CT [7]. Blachar et al. described the characteristic findings of a transmesenteric hernia as small bowel dilation, a cluster of small bowel loops, central displacement of colon, and a lack of omental fat overlying the cluster and displacement of the mesenteric trunk [8]. From a retrospective point of view, however, we could confirm only the former two findings in our patients case, and we failed to reach the correct diagnosis preoperatively, which suggests the difficulty of an accurate preoperative diagnosis of transmesenteric hernia. When patients with a bowel obstruction are encountered, clinicians should be aware of the possibility of a transmesenteric hernia, because surgical intervention performed as early as possible is necessary in such patients to avert bowel resection and provide a good clinical course [5].
The operative management for a transmesenteric hernia consists of timely laparotomy, reduction of the hernia, resection of bowel if necrotized and closure of the defect [5]. When the bowel is incarcerated too tightly to reduce as was observed in our patient’s case, it may be necessary to enlarge the defect to avoid bowel injuries [9].
We were unable to find any report of the existence of two transmesenteric defects in an adult. In our patient, we examined the whole mesentery after the reduction of the hernia and incidentally detected another mesenteric defect just distal to the defect which caused the small bowel incarceration. Thereafter, both mesenteric defects could be closed by suture. A detailed search of the entire mesentery contributes to the detection of other mesenteric defects and thus contributes to the prevention of the recurrence of internal hernias.
CONCLUSION
A transmesenteric hernia is a rare cause of small bowel obstruction in adults. Though the preoperative diagnosis of a transmesenteric hernia remains challenging, immediate decision-making based on surgical exploration is important to avoid bowel resection. Searching the whole mesentery after the reduction of a hernia will help prevent the recurrence of internal hernias.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Katagiri H, Okumura K, Machi J. Internal hernia due to mesenteric defect. J Surg Case Rep 2013;2013:doi:10.1093/jscr/rjt037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Alhayo S, Gosal P, Shakeshaft A. Incarcerated congenital transmesenteric hernia in an adult: a case report. J Surg Case Rep 2017;2017:doi:10.1093/jscr/rjx112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Vallumsetla R, Govind Rao N. Congenital transmesenteric internal hernia—a case report with literature review. Indian J Surg 2010;72:268–70. doi:10.1007/s12262-010-0065-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kalaycı O, Yazıcı A, Yandı M, Topaloğlu S. Strangulated congenital mesenteric hernia: a case report. Ulus Travma Acil Cerrahi Derg 2015;21:410–3. doi:10.5505/tjtes.2015.44957. [DOI] [PubMed] [Google Scholar]
- 5. ur Rehman Z, Khan S. Large congenital mesenteric defect presenting in an adult. Saudi J Gastroentero 2010;16:223–5. doi:10.4103/1319-3767.65193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Treves F. Lectures on the anatomy of the intestinal canal and peritoneum in man. Br Med J 1885;1:470–4. doi:10.1136/bmj.1.1262.470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Edwards HM, Al-Tayar H. A transmesenteric congenital internal hernia presenting in an adult. J Surg Case Rep 2013;2013:doi:10.1093/jscr/rjt099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Blachar A, Federle MP, Brancatelli G, Peterson MS, Oliver JH 3rd, Li W. Radiologist performance in the diagnosis of internal hernia by using specific CT findings with emphasis on transmesenteric hernia. Radiology 2001;221:422–8. doi:10.1148/radiol.2212010126. [DOI] [PubMed] [Google Scholar]
- 9. Benyamini P, Lopez S, Cooper M, Mohamad O, Maldini G. Congenital mesenteric defect: an uncommon cause of bowel obstruction. Hawaii J Med Public Health 2016;75:46–7. [PMC free article] [PubMed] [Google Scholar]



