Abstract
Background
The tibial tuberosity-trochlear groove (TT-TG) distance is used to determine the necessity of tibial tubercle osteotomy. We conducted this study to determine the extent to which each of the tibial tuberosity lateralization, trochlear groove medialization, and knee rotation angle affects the TT-TG distance in both normal and patella dislocated patients and thereby scrutinize the rationale for tuberosity transfer based on the TT-TG distance.
Methods
Retrospective analysis of rotational profile computed tomography was done for patella dislocated and control group patients. Femoral anteversion, tibial torsion, knee rotation angle, tuberosity lateralization, and trochlear groove medialization were assessed in all patients. Relationship of these parameters with the TT-TG distance was investigated to evaluate their effects on the TT-TG distance.
Results
We observed that the patellar dislocation group, compared to the control group, had increased TT-TG distance (mean, 19.05 mm vs. 9.02 mm) and greater tuberosity lateralization (mean, 64.1% vs. 60.7%) and tibial external rotation in relation to the femur (mean, 7.9° vs. −0.81°).
Conclusions
Tuberosity lateralization and knee rotation were factors affecting patellar dislocation. These factors should be considered in addition to the TT-TG distance to determine the need for tibial tubercle osteotomy in patients with patellar dislocation.
Keywords: Patellar dislocation, Rotation, Tibia/diagnostic imaging
Recurrent patellar dislocation is a result of aberration of normal patellofemoral kinematics.1,2) The anatomical deterrent resulting in malalignment of the knee may be multifactorial.3,4) Problems in both static and dynamic stabilizers of the knee joint may have a role, and therefore it is difficult to find a single treatment protocol that would be applicable for all patients uniformly.5,6) The fact that over 100 procedures have been described for the management of this condition stresses the fact that no single procedure works in all cases.1,2,3,5,6)
Depending on the etiology, both proximal and distal realignment procedures have been described for the treatment of recurrent patellar dislocation. Proximal realignment using lateral release and medial patellofemoral ligament reconstruction has demonstrated good results.6,7) However, the indications and results of distal realignment using tuberosity transfer have been controversial.8,9,10,11) Goutallier et al.12) described the tibial tuberosity-trochlear groove (TT-TG) distance as a quantitative measure of lateralization of the tibial tuberosity on the proximal tibia. Dejour et al.13) concluded 20 mm as a cut-off for tuberosity transfer. However, the literature has not always shown favorable results of tuberosity transfer, and thus we sought to investigate whether the TT-TG alone is an appropriate criterion to determine the transfer of tibial tuberosity.
Since it is important to identify the root cause of malalignment and address the contributing factors,14) tuberosity transfer would be of aid for patients who have severe tuberosity lateralization.15) However, the TT-TG distance is not an exclusive measure of tuberosity lateralization and theoretically an increased value may be a result of trochlear groove medialization on the distal femur, tibial tuberosity lateralization on the proximal tibia, or increased rotation between the distal femur and proximal tibia. Tensho et al.8) investigated retrospectively the TT-TG distance, tibial tubercle, and trochlear groove on computed tomography (CT) in patients with or without patellar dislocation. The authors reported that the TT-TG distance was affected more by knee rotation than by tubercle malposition and its use as an indicator for tibial tubercle transfer may not be appropriate. Besides these three factors described in the study of Tensho et al.,8) we tried to identify other factors that affect patellar dislocation and assess correlation with the TT-TG distance. We hypothesized that there would be another factor influencing the value of TT-TG distance other than tuberosity lateralization.
METHODS
We conducted this study in compliance with the principles of the Declaration of Helsinki. The protocol of this study was reviewed and approved by the Institutional Review Board of Chonnam National University Hwasun Hospital (IRB No. CNUHH-2018-143). Written informed consents were obtained. It was a single center, retrospective, one to two matched case-control study.
Patient Selection
The records of all patients who presented to our center from 2004 to 2015 due to a spontaneous recurrent patellar dislocation with pain were reviewed. Patients with a rotational profile CT scan and a minimum follow-up of 2 years were eligible for the study. Traumatic dislocation and any prior surgery to the knee were used as exclusion criteria. Thirty-one patients formed the study cohort. Twenty-eight patients had a unilateral dislocation and three had a bilateral dislocation. Controls matched for age, sex, body mass index (BMI), and affected side were selected from the records of patients who underwent a rotational profile CT scan for problems other than the knee joint. Sixty-eight control subjects (ratio, 1:2) formed the control cohort.
Data Acquisition
All patients were scanned under supine position with limbs in full extension and 15° external rotation was added for comfort. There were no patients with flexion contracture. The position was maintained during scan using Velcro straps fixed at the middle thigh and middle leg. Axial images at levels of hip, knee, and ankle were reviewed, and the TT-TG distance, tibial tuberosity lateralization, trochlear groove medialization, knee rotation angle, femoral anteversion, and tibial torsion were assessed.
To check the inter- and intraclass correlation coefficient of the measurements, two independent researchers—an orthopedic fellow (HWA) and a radiology consultant (CJI)—not involved directly in decision-making or patient management reviewed all data. The measurements were taken three times 2 weeks apart by each of the observer and the means of measured values were used as the final values.
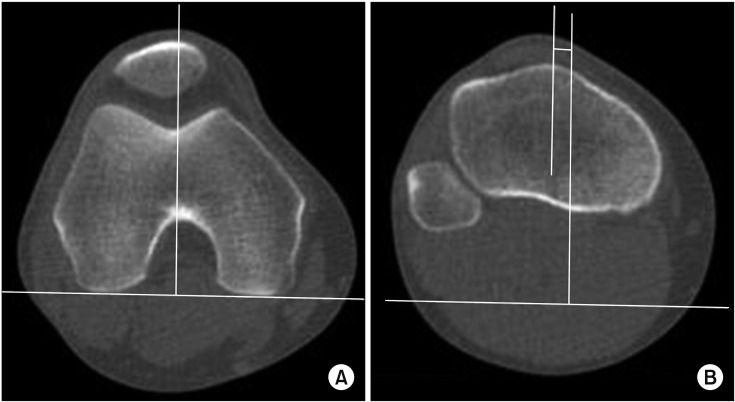
Tibial Tuberosity Trochlear Groove Distance
The trochlear groove position was measured on the axial image of the distal femur where the intercondylar notch takes an appearance of a rounded Roman arch. On this section, a tangent line was drawn to the distal-most portions of posterior condyles (posterior condylar line [PCL]). Then, another line (trochlear groove line) that passes the deepest portion of the trochlea was drawn perpendicular to the PCL. These lines were then copied from this section and pasted on the axial image of the proximal tibia at the most cephalad section of the tuberosity where the patellar tendon is in full contact with it. The distance between the trochlear groove line and a parallel line drawn from the most prominent anterior portion was defined as the TT-TG distance (Fig. 1).16)
Fig. 1. The tibial tuberosity trochlear groove distance was measured as the length between a line drawn from the deepest portion of the trochlear groove perpendicular to the posterior condylar line (A) and a line drawn parallel to this at the most prominent anterior portion of the tibial tuberosity (B).
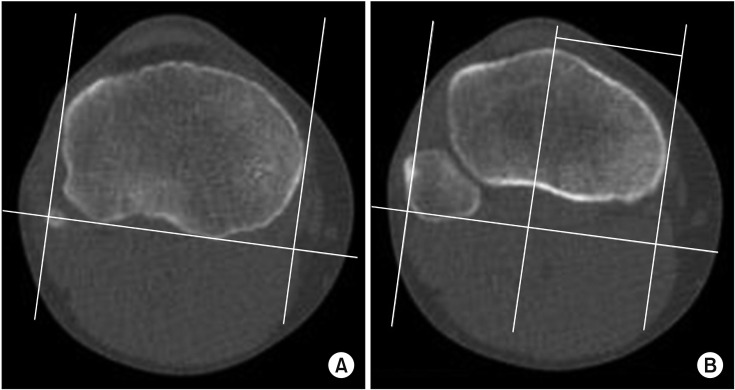
Tibial Tuberosity Lateralization
The width of the tibial plateau was measured on the most cephalic cut that clearly shows the posterior condylar notch of the tibia. A tangent line was drawn from the most posterior points of the plateau on this slice (tPCL). Next, two perpendicular lines were drawn from this line at the most medial and lateral margins of the tibial plateau. The distance between these two perpendicular lines gave the width of the tibia. Lateralization of tuberosity was measured on the axial image of the proximal tibia at the most cephalad section of the tuberosity where the patellar tendon is in full contact with it. The image of the tibial width was copied from this section. The distance between a line drawn at the most anterior part of the tuberosity perpendicular to the tPCL and the medial perpendicular line gave the value of lateralization of the tuberosity and it was presented as a percentage of the total tibial width (Fig. 2).8)
Fig. 2. (A) Tibial tuberosity lateralization was presented as a percentage of the total tibial width. (B) The distance between the most prominent anterior portion of the tibial tuberosity and the medial perpendicular line showed the value of lateralization of tuberosity.
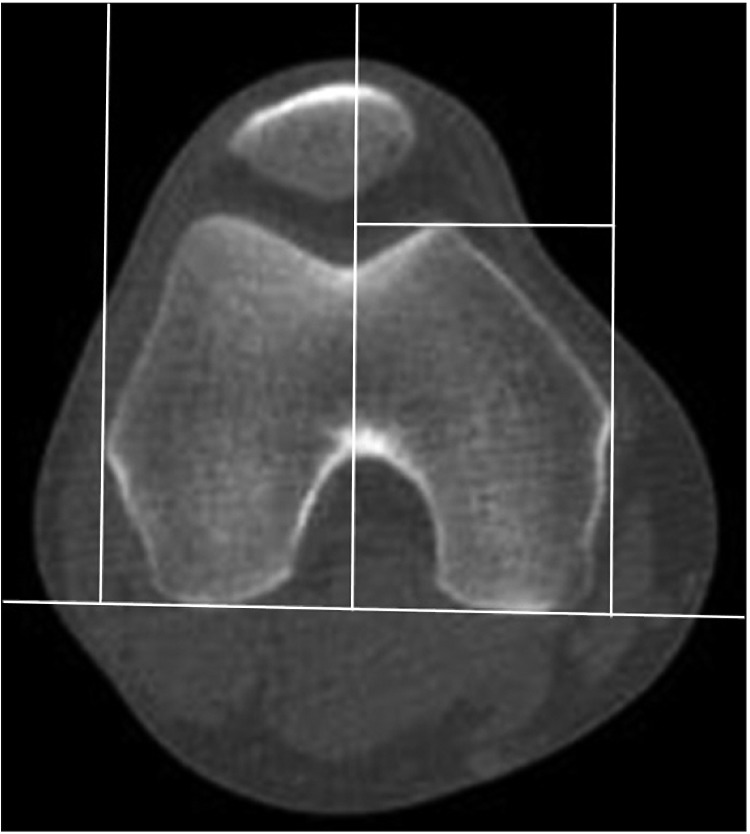
Trochlear Groove Medialization
The slice showing both lateral and medial epicondyles was used to measure the width of the femur. Perpendiculars were drawn from the most medial and lateral margins of the femur to the PCL. The distance between these two lines gave the width of the femur. The distance from the deepest portion of the groove to the medial perpendicular line was measured as the degree of medialization of the groove. The value was presented as a percentage of the femoral width (Fig. 3).8)
Fig. 3. Trochlear groove medialization was presented as a percentage of the total femoral width. The distance from the deepest portion of the groove to the medial perpendicular line showed the degree of medialization of the groove.
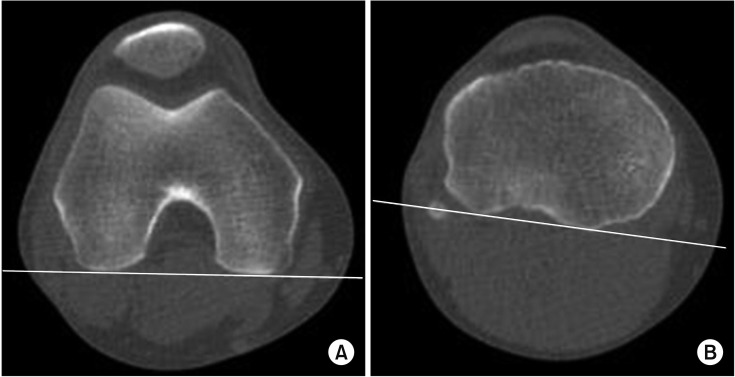
Knee Rotation Angle
This was defined an angle formed by the PCL and the tPCL. It represents relative rotation of the femur and tibia in relation to each other (Fig. 4).8)
Fig. 4. The knee rotation angle was measured by a posterior condylar line of the femur (A) and a tibial posterior condylar line (B).
Femoral Anteversion
The angle between an imaginary transverse line that runs medially to laterally through the knee joint and an imaginary transverse line passing through the center of the femoral head and neck is referred to as the femoral anteversion.17)
Tibial Torsion
Tibial torsion was measured as the angle formed by the tPCL and a tangent line through the bimalleolar axis on the section near the ankle joint at the base of malleoli.18)
Statistical Analysis
All variables are expressed as means and standard deviations. The statistical significance of the difference in means between the two groups was analyzed using Student t-test for continuous distribution variables. Chi-square test was used for categorical variables. The correlation of variables was tested in both groups using Pearson correlation coefficient. All statistics were carried out using IBM SPSS ver. 20.0 (IBM Corp., Armonk, NY, USA). A p-value < 0.05 was regarded as significant. To detect the difference in tuberosity lateralization, trochlear groove medialization, knee rotation, and tibial torsion in the 34 patients of dislocated group, with 80% power and α of 5%, 68 patients were needed in the control group.
RESULTS
Table 1 shows the demographic characteristics of the two groups, which were not significantly different. All parameters showed excellent inter- and intraclass agreement. The intra- and interclass correlation coefficients were 0.9 and 0.82, respectively, for the TT-TG distance; 0.92 and 0.86 for femoral anteversion; 0.96 and 0.91 for knee rotation angle; 0.98 and 0.92 for tibial torsion; 0.87 and 0.81 for tuberosity lateralization; and 0.82 and 0.8 for trochlear medialization.
Table 1. Patient Demographics.
| Variable | Patellar dislocation | Control | p-value |
|---|---|---|---|
| Age (yr) | 21.2 | 21.5 | 0.32* |
| Sex (male:female) | 18:13 | 39:29 | NS† |
| BMI (kg/m2) | 24.5 | 23.9 | 0.65* |
| Laterality (right:left) | 20:14 | 40:28 | NS† |
NS: not significant, BMI: body mass index.
The p-values are the results of *Student t-test for continuous variables and †chi-square for categorical variables.
Table 2 shows the results of Student t-test to evaluate the significance of difference in means between the two groups. It was interesting to find that normally the proximal tibia is in slight internal rotation in relation to the femur (mean, −0.81°; range, −2.1° to 3.4°). By contrast, in the dislocated group, the proximal tibia was in extreme external rotation in relation to the femur (mean, 7.9°; range, 5.9° to 12.2°). In addition, significant lateralization of the tibial tubercle in the patellar dislocation group compared to the normal group was observed (64.1% vs. 60.7%). Other parameters including femoral anteversion, tibial torsion, and trochlear medialization were not statistically different between the two groups. Table 3 shows the Pearson correlation coefficients of all the measured components in relation to the TT-TG distance. The TT-TG distance showed a mild positive correlation (0.578) with the degree of tuberosity lateralization and a moderate positive correlation (0.642) with the knee rotation angle in the dislocated group. In the control group, it showed only mild positive correlation with the degree of tubercle lateralization. It was found to have no significant correlation with any other components in either group.
Table 2. Comparison of Parameters on Computed Tomography between Patellar Dislocation and Control Groups.
| Variable | Patellar dislocation | Control | p-value* |
|---|---|---|---|
| Tibial tuberosity-trochlear groove distance (mm) | 19.05 ± 4.8 | 9.02 ± 5.2 | 0.000 |
| Femoral Anteversion (°) | 15.7 ± 4.4 | 11.4 ± 5.5 | 0.221 |
| Tibial torsion (°) | 30.9 ± 5.7 | 25.2 ± 6.4 | 0.121 |
| Knee rotation angle (°) | 7.9 ± 3.5 | −0.81 ± 1.1 | 0.000 |
| Trochlear medialization (%) | 52.8 ± 2.1 | 52.9 ± 2.3 | 0.958 |
| Tuberosity lateralization (%) | 64.1 ± 2.8 | 60.7 ± 3.1 | 0.016 |
Values are presented as mean ± standard deviation.
*The p-values are the results of Student t-test. Significant p-value is < 0.05.
Table 3. Results of Pearson Linear Correlation Analysis between Tibial Tubercle-Trochlear Groove Distance and Each Parameter.
| Variable | Patellar dislocation | Control | ||
|---|---|---|---|---|
| Coefficient | p-value | Coefficient | p-value | |
| Femoral anteversion | −0.09 | 0.749 | −0.254 | 0.361 |
| Tibial torsion | 0.09 | 0.750 | −0.070 | 0.805 |
| Knee rotation angle | 0.642 | 0.000 | −0.056 | 0.842 |
| Trochlear medialization | −0.420 | 0.105 | −0.318 | 0.248 |
| Tuberosity lateralization | 0.578 | 0.019 | 0.423 | 0.013 |
DISCUSSION
The study reveals an interesting finding that the TT-TG distance is not exclusively dependent on tuberosity lateralization but also on the relative rotation of the tibia in relation to the femur. This finding questions the validity of the TT-TG distance as a marker for tuberosity lateralization. In addition, the study suggests that apart from the increased TT-TG distance, patellar dislocation patients can present with increased tuberosity lateralization and tibial external rotation in relation to the femur.
The treatment of nontraumatic patellar dislocation poses a challenge for surgeons. The condition is multifactorial and it is challenging to locate clearly the anatomical anomaly that can lead to malfunctioning patellofemoral kinematics.1,2,3,4,5,6) Furthermore, the absence of a clear protocol, ethnic differences in anthropometry of the knee, and a variety of procedures mentioned in the literature complicate the situation. In particular, indications and results of distal realignment procedure have been the subject of controversy. Tibial osteotomy and medialization have been recommended in the literature for TT-TG distance values over 20 mm.13) However, few reports have shown good results with use of this criterion although others reported disagreement.8,9,10,11,19,20,21) Nakagawa et al.10) showed that good results tend to deteriorate with time. The reason for this has not been elucidated, but Tensho et al.8) suggested that since the TT-TG distance depends on the knee rotation angle rather than tubercle lateralization, tubercle osteotomy alone without correction of rotation may alter the patellofemoral kinematics, resulting in the development of late arthritis. We had similar observation with regards to knee rotation angle, but contrary to the results of the authors,8) the patella dislocated group had increased lateralization of the tuberosity. We believe that our findings may better explain why the outcomes of tubercle osteotomy can be favorable in some cases and not in the others. The patients with predominant lateralization of tuberosity would do well with the transfer. However, the patients in whom extreme knee rotation is the cause of increased TT-TG distance may not be perfect candidates for isolated tuberosity transfer. Similarly, Ando22) also concluded that tuberosity lateralization increased in patients with patellar dislocation compared to a control group. Further, in contrast to Tensho et al.,8) we found that the normal control group had no correlation between the knee rotation angle and the TT-TG distance. This further stresses that increased knee rotation angle is a consequence of patellar dislocation and its contribution to the increased TT-TG distance cannot be overlooked.
Various authors have recognized the rotational component in patellar dislocation in the past without specific description of knee rotation angle.23,24,25) In the absence of today's radiological advancement, the decision of derotation tibial osteotomy was based on clinical findings and was attributed to tibial torsion. Paulos et al.26) compared isolated tuberosity transfer to tibial derotation osteotomy in addition to tuberosity transfer in patients with thigh a foot angle of more than 30°. However, with use of the rotational profile CT scan, we recognized that the rotational deformity was not the result of increased tibial torsion. High tibial derotation osteotomy would be helpful only in cases of increased tibial torsion and this may explain that why such procedures are not uniformly helpful.
In our study, patients in both groups had no difference in anteversion or tibial torsion. We believe that the anatomical abnormality causing increased knee rotation angle lies at level of the knee joint, which has not been recognized so far. Although Tensho et al.8) hypothesized that knee rotation angle is the cause of an increased TT-TG distance, their results were based on CT scans of the knee. Theoretically, the knee rotation angle may be changed by either femoral anteversion or tibial torsion. Plain CT of the knee would not be able to reveal if increased knee rotation is due to rotational anomaly of the femur, tibia or knee joint. The present study for the first time provides an objective proof that supports the abovementioned hypothesis. With rotational profile CT, it is possible to rule out other causes of increased knee rotation angle. This finding further demonstrates the inadequacy of the described techniques in management of patellar dislocation. Derotation osteotomy may not be the solution for increased knee rotation angle since the proximal tibia is not the source of deformity. We strongly believe that further studies should be conducted in order to delineate the actual cause of malrotation and the methods to correct it.
Knee rotation angle has been studied rarely for patellar dislocation. We found only two papers mentioning the measurement of this parameter.8,27) Schueda et al.27) found no difference in knee rotation angle between dislocated and normal groups, while Tensho et al.,8) similar to our study, noted that the tibia was in increased degree of external rotation in patellar dislocation patients compared to the control group. This discrepancy may be due to the difference in measurement techniques and the axial cuts used for measurement in the two studies. In addition, it is well known that Asian knees are anthropometrically different from their western counterparts.28) A previous study by Schueda et al.27) involved a Brazilian population, whereas the present study and the study of Tensho et al.8) are based on Asian patients. Thus, we think that the different results could also be due to anthropometric differences; however, this should be backed up by further research involving multicenter data that compare such values in different ethnic groups.
The limitations of our study are the small sample size and retrospective nature of the work. Even though we observed that both femur and tibia had normal rotations, we could not objectively identify the true anatomical location of the rotational deformity. It would be important to know whether the extreme knee rotation is the cause or result of disrupted patellofemoral alignment. This would further help to formulate the procedure that would be suited for the patients with rotational abnormality. We believe that these answers may can be obtained by collective efforts of the scientific community. Despite these shortcomings, we hope this preliminary attempt will encourage researchers to improve the understanding of the true pathoanatomy of patellar dislocation.
Tuberosity lateralization as well as knee rotation in relation to the femur was factors affecting patellar dislocation and correlated with the TT-TG distance. Therefore, tibial tubercle osteotomy in nontraumatic patellar dislocation should be carefully determined based on the consideration of the TT-TG distance, tubercle lateralization, and knee rotation, rather than the TT-TG distance alone.
References
- 1.Aglietti P, Buzzi R, Insall JN. Disorders of the patellofemoral joint. In: Insall JN, Scott WN, editors. Surgery of the Knee. 3rd ed. New York, NY: Churchill Livingstone; 2001. pp. 592–623. [Google Scholar]
- 2.Aulisa AG, Falciglia F, Giordano M, Savignoni P, Guzzanti V. Galeazzi's modified technique for recurrent patella dislocation in skeletally immature patients. J Orthop Sci. 2012;17(2):148–155. doi: 10.1007/s00776-011-0189-1. [DOI] [PubMed] [Google Scholar]
- 3.Biedert RM, Bachmann M. Anterior-posterior trochlear measurements of normal and dysplastic trochlea by axial magnetic resonance imaging. Knee Surg Sports Traumatol Arthrosc. 2009;17(10):1225–1230. doi: 10.1007/s00167-009-0824-y. [DOI] [PubMed] [Google Scholar]
- 4.Blumensaat C, Ergenbn D. Patellofemoral disorders: physical and radiographic evaluation. Chir U Orthop. 1938;31:149–223. [Google Scholar]
- 5.Colvin AC, West RV. Patellar instability. J Bone Joint Surg Am. 2008;90(12):2751–2762. doi: 10.2106/JBJS.H.00211. [DOI] [PubMed] [Google Scholar]
- 6.Conlan T, Garth WP, Jr, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75(5):682–693. doi: 10.2106/00004623-199305000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Camanho GL, Bitar AC, Hernandez AJ, Olivi R. Medial patellofemoral ligament reconstruction: a novel technique using the patellar ligament. Arthroscopy. 2007;23(1):108.e1–108.e4. doi: 10.1016/j.arthro.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 8.Tensho K, Akaoka Y, Shimodaira H, et al. What components comprise the measurement of the tibial tuberosity-trochlear groove distance in a patellar dislocation population? J Bone Joint Surg Am. 2015;97(17):1441–1448. doi: 10.2106/JBJS.N.01313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuroda R, Kambic H, Valdevit A, Andrish JT. Articular cartilage contact pressure after tibial tuberosity transfer: a cadaveric study. Am J Sports Med. 2001;29(4):403–409. doi: 10.1177/03635465010290040301. [DOI] [PubMed] [Google Scholar]
- 10.Nakagawa K, Wada Y, Minamide M, Tsuchiya A, Moriya H. Deterioration of long-term clinical results after the Elmslie-Trillat procedure for dislocation of the patella. J Bone Joint Surg Br. 2002;84(6):861–864. doi: 10.1302/0301-620x.84b6.12804. [DOI] [PubMed] [Google Scholar]
- 11.Parikh S, Noyes FR. Patellofemoral disorders: role of computed tomography and magnetic resonance imaging in defining abnormal rotational lower limb alignment. Sports Health. 2011;3(2):158–169. doi: 10.1177/1941738111399372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goutallier D, Bernageau J, Lecudonnec B. The measurement of the tibial tuberosity: patella groove distanced technique and results (author's transl) Rev Chir Orthop Reparatrice Appar Mot. 1978;64(5):423–428. [PubMed] [Google Scholar]
- 13.Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 14.Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am. 1994;25(3):425–465. [PubMed] [Google Scholar]
- 15.Stephen JM, Lumpaopong P, Dodds AL, Williams A, Amis AA. The effect of tibial tuberosity medialization and lateralization on patellofemoral joint kinematics, contact mechanics, and stability. Am J Sports Med. 2015;43(1):186–194. doi: 10.1177/0363546514554553. [DOI] [PubMed] [Google Scholar]
- 16.Schoettle PB, Zanetti M, Seifert B, Pfirrmann CW, Fucentese SF, Romero J. The tibial tuberosity-trochlear groove distance; a comparative study between CT and MRI scanning. Knee. 2006;13(1):26–31. doi: 10.1016/j.knee.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 17.Cibulka MT. Determination and significance of femoral neck anteversion. Phys Ther. 2004;84(6):550–558. [PubMed] [Google Scholar]
- 18.Goutallier D, Van Driessche S, Manicom O, Sariali E, Bernageau J, Radier C. Influence of lower-limb torsion on long-term outcomes of tibial valgus osteotomy for medial compartment knee osteoarthritis. J Bone Joint Surg Am. 2006;88(11):2439–2447. doi: 10.2106/JBJS.E.01130. [DOI] [PubMed] [Google Scholar]
- 19.Balcarek P, Jung K, Ammon J, et al. Anatomy of lateral patellar instability: trochlear dysplasia and tibial tubercle-trochlear groove distance is more pronounced in women who dislocate the patella. Am J Sports Med. 2010;38(11):2320–2327. doi: 10.1177/0363546510373887. [DOI] [PubMed] [Google Scholar]
- 20.Balcarek P, Jung K, Frosch KH, Sturmer KM. Value of the tibial tuberosity-trochlear groove distance in patellar instability in the young athlete. Am J Sports Med. 2011;39(8):1756–1761. doi: 10.1177/0363546511404883. [DOI] [PubMed] [Google Scholar]
- 21.Dickens AJ, Morrell NT, Doering A, Tandberg D, Treme G. Tibial tubercle-trochlear groove distance: defining normal in a pediatric population. J Bone Joint Surg Am. 2014;96(4):318–324. doi: 10.2106/JBJS.M.00688. [DOI] [PubMed] [Google Scholar]
- 22.Ando T. Factors affecting the rectus femoris-patellar tendon Q-angle, measured using a computed tomographic scan. J Orthop Sci. 1999;4(2):73–77. doi: 10.1007/s007760050077. [DOI] [PubMed] [Google Scholar]
- 23.Cameron JC, Saha S. External tibial torsion: an underrecognized cause of recurrent patellar dislocation. Clin Orthop Relat Res. 1996;(328):177–184. [PubMed] [Google Scholar]
- 24.Drexler M, Dwyer T, Dolkart O, et al. Tibial rotational osteotomy and distal tuberosity transfer for patella subluxation secondary to excessive external tibial torsion: surgical technique and clinical outcome. Knee Surg Sports Traumatol Arthrosc. 2014;22(11):2682–2689. doi: 10.1007/s00167-013-2561-5. [DOI] [PubMed] [Google Scholar]
- 25.Sanfridsson J, Arnbjornsson A, Friden T, Ryd L, Svahn G, Jonsson K. Femorotibial rotation and the Q-angle related to the dislocating patella. Acta Radiol. 2001;42(2):218–224. [PubMed] [Google Scholar]
- 26.Paulos L, Swanson SC, Stoddard GJ, Barber-Westin S. Surgical correction of limb malalignment for instability of the patella: a comparison of 2 techniques. Am J Sports Med. 2009;37(7):1288–1300. doi: 10.1177/0363546509334223. [DOI] [PubMed] [Google Scholar]
- 27.Schueda MA, Astur DC, Bier RS, Bier DS, Astur N, Cohen M. Use of computed tomography to determine the risk of patellar dislocation in 921 patients with patellar instability. Open Access J Sports Med. 2015;6:55–62. doi: 10.2147/OAJSM.S75243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim DK, Seo MC, Song SJ, Kim KI. Are Korean patients different from other ethnic groups in total knee arthroplasty? Knee Surg Relat Res. 2015;27(4):199–206. doi: 10.5792/ksrr.2015.27.4.199. [DOI] [PMC free article] [PubMed] [Google Scholar]