Abstract
Background
Tsetse flies are vectors of African trypanosomes, protozoan parasites that cause sleeping sickness (or human African trypanosomosis) in humans and nagana (or animal African trypanosomosis) in livestock. In addition to trypanosomes, four symbiotic bacteria Wigglesworthia glossinidia, Sodalis glossinidius, Wolbachia, Spiroplasma and one pathogen, the salivary gland hypertrophy virus (SGHV), have been reported in different tsetse species. We evaluated the prevalence and coinfection dynamics between Wolbachia, trypanosomes, and SGHV in four tsetse species (Glossina palpalis gambiensis, G. tachinoides, G. morsitans submorsitans, and G. medicorum) that were collected between 2008 and 2015 from 46 geographical locations in West Africa, i.e. Burkina Faso, Mali, Ghana, Guinea, and Senegal.
Results
The results indicated an overall low prevalence of SGHV and Wolbachia and a high prevalence of trypanosomes in the sampled wild tsetse populations. The prevalence of all three infections varied among tsetse species and sample origin. The highest trypanosome prevalence was found in Glossina tachinoides (61.1%) from Ghana and in Glossina palpalis gambiensis (43.7%) from Senegal. The trypanosome prevalence in the four species from Burkina Faso was lower, i.e. 39.6% in Glossina medicorum, 18.08%; in Glossina morsitans submorsitans, 16.8%; in Glossina tachinoides and 10.5% in Glossina palpalis gambiensis. The trypanosome prevalence in Glossina palpalis gambiensis was lowest in Mali (6.9%) and Guinea (2.2%). The prevalence of SGHV and Wolbachia was very low irrespective of location or tsetse species with an average of 1.7% for SGHV and 1.0% for Wolbachia. In some cases, mixed infections with different trypanosome species were detected. The highest prevalence of coinfection was Trypanosoma vivax and other Trypanosoma species (9.5%) followed by coinfection of T. congolense with other trypanosomes (7.5%). The prevalence of coinfection of T. vivax and T. congolense was (1.0%) and no mixed infection of trypanosomes, SGHV and Wolbachia was detected.
Conclusion
The results indicated a high rate of trypanosome infection in tsetse wild populations in West African countries but lower infection rate of both Wolbachia and SGHV. Double or triple mixed trypanosome infections were found. In addition, mixed trypanosome and SGHV infections existed however no mixed infections of trypanosome and/or SGHV with Wolbachia were found.
Electronic supplementary material
The online version of this article (10.1186/s12866-018-1287-4) contains supplementary material, which is available to authorized users.
Keywords: Glossina spp., Trypanosoma spp., Wolbachia spp., SGHV, Microbe infection rate, Interactions
Background
Tsetse flies (Glossina sp.) are obligate blood feeding insects that transmit protozoan parasites (Trypanosoma spp.), the etiological agents of African trypanosomosis that cause sleeping sickness or human African trypanosomosis, (HAT) and nagana or animal African trypanosomosis, (AAT) in livestock [1, 2]. Both diseases cause many direct and indirect losses, which represent a major obstacle for sustainable development in endemic countries [3].
Trypanosomosis is enzootic in an area covering ca. 10 million km2 in sub-Saharan Africa and is transmitted by different species of tsetse flies that vary in their vectorial capacity for the different Trypanosoma species [2]. In West Africa, HAT is caused by Trypanosoma brucei gambiense, that accounts for over 90% of the globally reported HAT cases [4] and is mainly transmitted by tsetse flies from the palpalis group (Glossina tachinoides, G. palpalis gambiensis and G. p. palpalis) [5]. The AAT causative agents (Trypanosoma vivax, T. congolense, T. brucei brucei and T. evansi) are transmitted by a broader range of tsetse fly species which include, in addition to the above-mentioned palpalis group, also flies from the morsitans group (G. morsitans submorsitans and G. longipalpis) [6, 7]. There are 11 different pathogenic trypanosomes that can be characterized by molecular methods using specific or common primers [6–8].
Due to the lack of effective vaccines and inexpensive drugs for HAT and also the development of resistance of the AAT parasites against available trypanocidal drugs [9], vector control remains the most efficient strategy for the sustainable management of these diseases [10]. The sterile insect technique (SIT) is one control tactic that may be used as part of an area-wide integrated pest management (AW-IPM) program against tsetse fly populations [11, 12].
The SIT was successfully used as part of an AW-IPM strategy to sustainably eradicate a population of G. austeni from the Island of Unguja, Zanzibar in the 1990’s [13] and allowed the eradication of tsetse flies from the agro-pastoral land in Sidéradougou, Burkina Faso and in Jos, Nigeria [14, 15]. The latter two programmes were however not sustainable, as they were not implemented following AW-IPM principles, and hence suffered from re-invasion of wild flies from neighbouring areas.
The integration of the SIT in AW-IPM strategies to manage populations of tsetse flies requires the production of large numbers of high quality sterile males that are released in the target area to compete with wild males for matings with wild females of the targeted species. The mass production of the required males will depend on the successful establishment and maintenance of a large, healthy colony of the targeted species in large production facilities. In some tsetse species such as Glossina pallidipes, colonies that are infected with a hytrosavirus, the salivary gland hypertrophy virus (SGHV), suffer from low male and female fertility which makes the maintenance of these colonies very difficult or even impossible [16–18]. This obviously hampers the implementation of AW-IPM programmes that have an SIT component. Tsetse colonies of species that are susceptible to the negative effects of the SGHV require the implementation of some measurements to manage the virus infection to enable colony maintenance and growth [19, 20].
The successful establishment of a large colony of G. pallidipes will not only depend on the virus infection but can also be affected by the tsetse associated symbiotic bacteria. Tsetse flies harbour four main symbiotic bacteria: (i) Wigglesworthia glossinidia, an obligate symbiotic bacterium that is present in all tsetse species. Its removal from a tsetse fly using antibiotic supplements in the tsetse’s diet results in the loss of fertility [21–23], (ii) The commensal Sodalis glossinidius, present in all individuals of laboratory-maintained tsetse lines but not abundant in natural populations. It has been detected in the haemolymph, salivary glands and milk gland of the tsetse fly but also in the midgut where it lives in close proximity with trypanosomes [24–26], (iii) Wolbachia, which is an obligate intracellular and maternally transmitted alpha-proteobacterium that infects many arthropod and filarial nematode species [27, 28]. Wolbachia is responsible for the induction of a number of reproductive alterations and cytoplasmic incompatibility (CI) [27, 28]. Wolbachia infections occur in some tsetse fly species, both in the laboratory and in nature. Available data indicate that Wolbachia infections were heterogeneous in the field, ranging from 0 to 100% in natural populations of G. austeni and G. brevipalpis and from 9.5 to 100% in natural populations of G. m. morsitans [29]. It has been reported that the presence of Wolbachia is associated with reduced prevalence of infections with pathogenic viruses and Plasmodium [30–40]. Therefore, the presence of Wolbachia in tsetse species might also reduce trypanosome and SGHV infections and transmission, and (iv) Spiroplasma that was recently detected in G. fuscipes and G. tachnoides but its impact on tsetse fly performance remains unclear [41].
In support of the potential development of sustainable AW-IPM strategies that might include an SIT component against tsetse species in West Africa, we assessed the prevalence of trypanosomes, SGHV and Wolbachia in a large number of wild specimens from five countries as well as the potential interactions among these three microbes.
Methods
Sampling tsetse
Adult tsetse flies of G. palpalis gambiensis, G. tachinoides, G. morsitans submorsitans, and G. medicorum were collected between 2008 and 2015 in 46 geographical locations from five countries in West Africa (Burkina Faso, Guinea, Ghana, Mali, Senegal) (Tables 1 and 2). The flies were collected using the biconical Challier-Laveissière trap [42] and the monoconical Vavoua trap [43, 44] set as previously described [45]. On average, 20 traps were deployed per location to collect a minimum of 10 adult flies per location that were sorted by species and sex [46]. Collected flies were preserved in 95% ethanol, labeled and shipped to the FAO/IAEA Insect Pest Control Laboratory (IPCL) in Seibersdorf, Austria where they were stored at − 20 °C until further use. Species status was confirmed using molecular identification tools including internal transcribed spacers (ITS), mitochondrial DNA cytochrome oxidase subunit 1 and microsatellites (Augustinos 2018 this special issue).
Table 1.
List of collections of tsetse adults that were analyzed to establish the prevalence of Trypanosomes, Wolbachia and Salivary gland hypertrophy virus (SGHV) in wild tsetse populations in West African countries
| Country | No. of locations | No. of collected flies | Collection year |
|---|---|---|---|
| Burkina Faso | 10 | 2062 | 2008, 2010, 2013, 2015 |
| Mali | 10 | 364 | 2008, 2010, 2011, 2012, 2013 |
| Senegal | 7 | 128 | 2008 |
| Ghana | 11 | 234 | 2008 |
| Guinea | 8 | 314 | 2008, 2009 |
| Total | 46 | 3102 |
Table 2.
Geographic coordinates of tsetse collected samples
| Glossina species | Country (area) | Longitude | Latitude |
|---|---|---|---|
| G. tachinoides | Burkina Faso (Folonzo) | − 4.60801757 | 9.92967851 |
| Burkina Faso (Sissili) | −2.098178 | 11.09447 | |
| Burkina Faso (Comoe) | − 4.58976269 | 9.89106718 | |
| Burkina Faso (Arly) | −1.289104 | 11.612917 | |
| Ghana (Bougouhiba) | −0,719,172,226 | 10,23,885,694 | |
| Ghana (Walewale) | −0.79846 | 10.351613 | |
| Ghana (Mortani) | −0,714,119,074 | 10,23,479,058 | |
| Ghana (Fumbissi) | −1,386,834,989 | 10,47,282,856 | |
| Ghana (Sissili Bridge) | −1,319,208,122 | 10,33,035,865 | |
| Ghana (Grogro) | −1.883133222 | 10.08224767 | |
| Ghana(Kumpole) | −1,270,183,374 | 10,25,432,141 | |
| Ghana (Nabogo) | −0,979,001,606 | 9,692,628,234 | |
| Ghana (Psikpé) | −1,081506423 | 10,44,471,897 | |
| G. palpalis gambiensis | Burkina Faso (Kénédougou) | −4.80305222 | 10.98166737 |
| Burkina Faso (Moussodougou) | −4.95 | 10.833333 | |
| Burkina Faso (Folonzo) | −4.60801757 | 9.92967851 | |
| Burkina Faso (Comoé) | −4.58976269 | 9.89106718 | |
| Burkina Faso (Kartasso) | −5.253033 | 11.141786 | |
| Burkina Faso (Bama) | −4.4 | 12.033333 | |
| Sénégal (Tambacounda) | −13.667222 | 13.7768889 | |
| Sénégal (Fleuve Gambi) | −13,23,552,282 | 13,02433926 | |
| Sénégal (Mako) | −13,27,338,336 | 12,85,430,818 | |
| Sénégal (Niokolo) | −13,16,964,933 | 13,06555831 | |
| Sénégal (Fleuève Gambi) | −12,35,811,122 | 12,84,670,702 | |
| Sénégal (Diaguiri) | −12,09137828 | 12,62,932,251 | |
| Sénégal (Moussalla) | −17,37,981,432 | 12,9,297,035 | |
| Mali (Baoule) | −8.62 | 12.88 | |
| Mali (Banko) | −6.516667 | 12.1 | |
| Mali (Siby) | −8.32664 | 12.377685 | |
| Mali (Système Sénégal) | −11.103663 | 13.416551 | |
| Mali (Système Niger) | −4.201945 | 14.466284 | |
| Mali (Bani) | −4,202,017 | 14,466,353 | |
| Mali (Bougouni) | −7.483333 | 11.416667 | |
| Mali (Sikasso) | −5.666667 | 11.316667 | |
| Mali (Kita) | −9.484723 | 13.04114 | |
| Mali (Baguineda) | −7.776667 | 12.615278” | |
| Guinea (Kangoliya) | −13.65584 | 9.96084 | |
| Guinea (Dekonkore) | −10.016667 | 9.85 | |
| Guinea (Bafing) | −7.524724 | 8.325205 | |
| Guinea (Lemonako) | −11.566667 | 11.733333 | |
| Guinea (Kerfala) | −9.461194 | 11.343966 | |
| Guinea (Mimi) | −9.053083 | 10.400434 | |
| G. morsitans submorsitans | Burkina Faso (Folonzo) | −4.60801757 | 9.92967851 |
| Burkina Faso (Sissili) | −2.098178 | 11.09447 | |
| Burkina Faso (Comoe) | −4.58976269 | 9.89106718 | |
| G. medicorum | Burkina Faso (Comoe) | −4.58976269 | 9.89106718 |
| Burkina Faso (Folonzo) | −4.60801757 | 9.92967851 |
DNA extraction
The flies were removed from ethanol and rehydrated in distilled water. The wings and legs were removed for other studies. The total DNA was extracted from the remaining fly body using the DNeasy tissue kit (QIAGEN Inc., Valencia, CA) following the supplier’s instructions and was eluted in 200 μl elution buffer. All the extracted DNA samples from these locations were tested for a tsetse-specific sequence to confirm the quality.
PCR amplification and prevalence analysis
SGHV prevalence
Polymerase chain reactions (PCR) were used to amplify the partial coding regions of two conserved putative ORFs, odv-e66 and dnapol (GenBank accession numbers: EF568108) using Glossina pallidipes Salivary Hypertrophy Virus (GpSGHV)-specific primers [47]. These primers were used in a multiplex PCR, and all the samples included a set of specific primers amplifying the G. pallidipes microsatellite GpCAG133 sequence to control the quality of the extracted DNA [48]. For all PCR amplifications, 22.5 μl of 1.1× Pre-Aliquoted PCR Master Mix (ABgene, UK) was used. A final volume of 25 μl of this mix contained: 0.625 units Thermoprime Plus DNA Polymerase, 75 mM Tris–HCl (pH 8.8 at 25 °C), 20 mM (NH4)2SO4, 2.0 mM MgCl2, 0.01% (v/v) Tween-20 and 0.2 mM each of the dNTPs. To the mix, 1.5 μl of template DNA plus forward and reverse primers were added to a final concentration of 0.2 mM per primer. Samples were considered virus-infected if any of the expected viral PCR product amplicons were detected. Data were accepted only if the control gene GpCAG133 sequence was amplified.
Trypanosome prevalence and genotyping
For trypanosome detection, PCR was used according to Njiru et al., [8], using trypanosome specific primers to amplify the internal transcribed spacer 1 (ITS-1). PCR conditions were: 25 μl volume containing 12.5 μl of Taq PCR Master Mix kit (Qiagen) (with 0.8 Units of Taq DNA polymerase, 1.5 mM MgCl2, 200 μM dNTP), 0.8 μM each of the ITS-1 forward (5’-CCGGAAGTTCACCGATATTG-3′) and reverse (5’-TGCTGC GTTCTTCAACGAA- 3′) primers (VBC, Biotech, Austria), 9 μl of sterile water and 2.5 μl of genomic DNA. Cycling conditions were: 94 °C for 15 min, 94 °C for 30 s, 60 °C for 30s, 72 °C for 30s, 40 cycles following by 72 °C for 5 min; PCR products were detected by agarose (2%) gel electrophoresis and ethidium bromide staining. The sample was considered infected with trypanosome by detecting single, double or triple bands ranging from 200 bp to 700 bp (see below). DNA from T. congolense savannah was used as positive control which gives a PCR amplicon of 650 bp.
To have better specific and sub-specific identification of the detected trypanosomes, positive samples from the first screen were amplified with ITS-1 forward (5’-TGTAGGTGAACCTGCAGCTGGATC-3′) and ITS-1 reverse (5’-CCAAGTCATCCATCGCGACACGTT- 3′) primers following Fikru et al. [49]. The detection of different trypanosomes was based on the length of the amplicon, i.e., T. vivax (200 bp), T. equiperdum, T. evansi and T. brucei (350 bp), T. theileri (450 bp) and T. congolense savannah type (650 bp). DNA from T. congolense savannah type, T. vivax, T. theileri, T. brucei gambiense, T. brucei rhodesiense, T. brucei brucei, T. evansi and T. equiperdum provided by Dr. Stijn Deborggraeve were used as positive control.
Wolbachia prevalence
PCR reaction with Wolbachia specific primers was used to screen the DNA of the wild tsetse flies for the presence of Wolbachia. The detection was based on the Wolbachia 16S rRNA gene and results in the amplification of a 438 base-pair long DNA fragment with the Wolbachia specific primers wspecF and wspecR [29]. The PCR conditions used were as described above for the trypanosome detection and the cycling conditions were: 94 °C for 2 min, 94 °C for 30 s, 55 °C for 30s, 72 °C for 30s, 36 cycles following by 72 °C for 5 min. As a positive control for Wolbachia, DNA extracted from the Mediterranean fruit fly, Ceratitis capitata strain S 10.3 was used. This strain is transinfected with the wCer4 Wolbachia strain of Rhagoletis cerasi [50].
Data analysis
The data were analyzed with the software package R, using a generalized linear model (GLM) with the package stat [51]. Trypanosome, virus and Wolbachia prevalence in tsetse were respectively considered as response variables, while tsetse species, sex, countries and their interactions were used as explicative variables. The best model was selected on the basis of the lowest corrected Akaike information criterion (AICc), and the significance of fixed effects was tested using the likelihood test ratio [52, 53]. Then, for each country, GLM were used to assess differences in trypanosome, virus and Wolbachia prevalence between localities and species. Trypanosome prevalence was compared between species by a pairwise comparison of proportions with a Bonferroni correction (package stats). Correlations between the prevalence of trypanosome species, salivary gland hypertrophy virus and Wolbachia were tested using the “rcorr” function of the Hmisc (Harrel miscellaneous package version 4.03, 2017).
Results
Global trypanosome prevalence
The trypanosome prevalence varied significantly from one country to another and from one species to another. Overall, 18.4% of the examined tsetse flies (n = 3102) were positive for trypanosomes, irrespective of tsetse species or country (Table 3). Trypanosomes were detected in G. tachinoides in Burkina Faso and Ghana; G. p. gambiensis in Burkina Faso, Guinea, Mali, and Senegal; G. m. submorsitans and G. medicorum in the Comoé forest in the south of Burkina Faso at the border with Côte d’Ivoire. The best model (lowest AICc) selected for the overall trypanosome prevalence retained the tsetse species and countries as variables that fitted well the data with no interaction. For tsetse species, G. medicorum (only caught in Folonzo village, and a protected area belonging to the village in Southern Burkina Faso) had the highest mean infection rate of 39.6% (Fig. 1A), which was significantly higher than the mean infection rate in G. p. gambiensis (P < 0.001). The mean trypanosome infection rate in G. tachinoides was also significantly higher as compared with G. m. submorsitans (P = 0.008; Fig. 1A; Additional file 1).
Table 3.
Prevalence of trypanosomes, salivary gland hypertrophy virus and Wolbachia in tsetse tested samples
| Species | Country | Trypanosomes | Virus | Wolbachia |
|---|---|---|---|---|
| G. tachinoides | Burkina Faso | (140/834) 16.79% | (25/834) 3% | (2/834) 0.24% |
| Ghana | (143/234) 61.11% | (0/234) 0% | (0/234) 0% | |
| G.p.gambiensis | Burkina Faso | (77/731) 10,53% | (14/731) 1,92% | (1/731) 0,14% |
| Mali | (25/364) 6,87% | (15/364) 4,12% | (16/364) 4,40% | |
| Guinea | (7/314) 2,23% | (0/314) 0% | (13/314) 4,14% | |
| Senegal | (58/128) 43,75% | (0/128) 0% | (0/128) 0% | |
| G. m. submorsitans | Burkina Faso | (62/343) 18.08% | (4/343) 1,17% | (1/343) 0,29% |
| G. medicorum | Burkina Faso | (61/154) 39.61% | (1/154) 0,65% | (1/154) 0,65% |
| Total | (570/3102) 18,38% | (54/3102) 1,74% | (30/3102) 0,96% | |
Fig. 1.
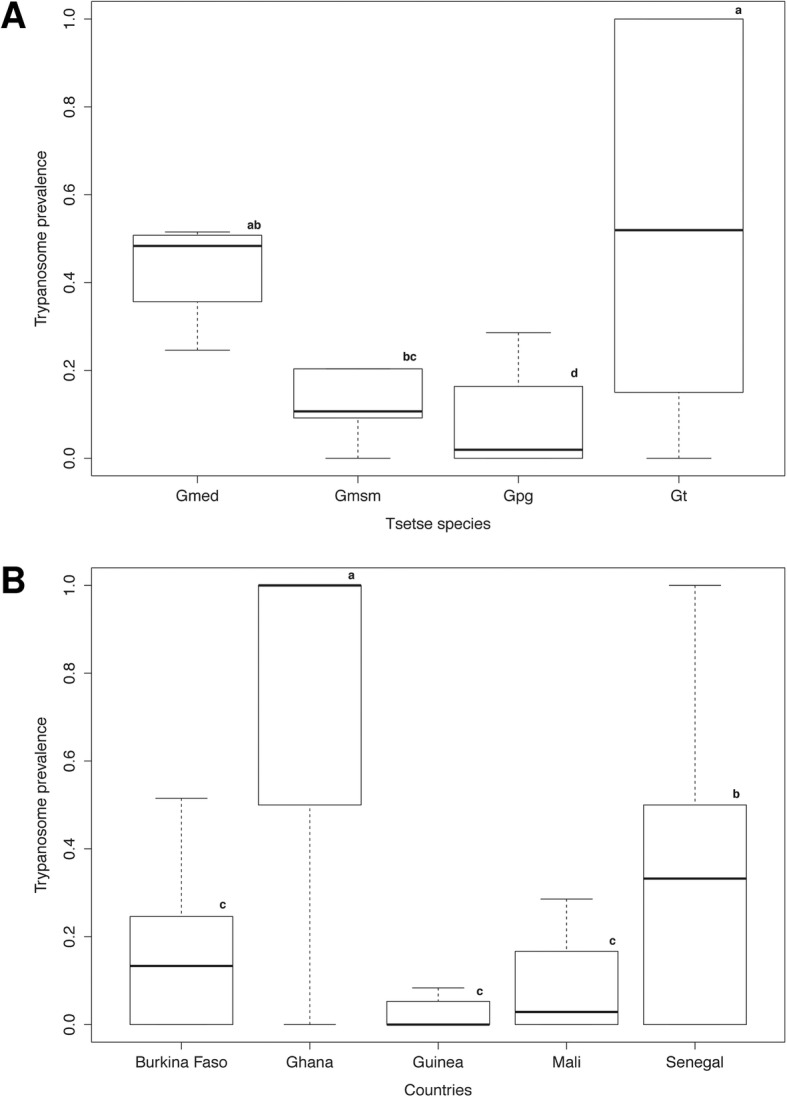
Global prevalence of trypanosomes according to tsetse species (A) and country (B). Boxes extend between the 25th and 75th percentile. A thick line denotes the median. The whiskers extend up to the most extreme values. Gmed: Glossina medicorum, Gmsm: G. morsitans submositans, Gpg: G. palpalis gambiensis and Gt: G. tachinoides. Different letters indicate significant difference. Different letters indicate significant difference
Trypanosome prevalence by country was low in Guinea (2.2%) and Mali (6.9%) but high in Senegal (43.7%) and Ghana (61.1%) (Table 3). The result showed no significant difference between the trypanosome prevalence in Burkina Faso, Guinea and Mali but the prevalence of these three countries was significantly different from that of Senegal and Ghana (P < 0.05) (Fig. 1B and Additional file 1). The sex effect was not retained in the model highlighting no difference in the mean prevalence of male and female flies. All G. tachinoides flies collected from Fumbissi (n = 15), Grogro (n = 11), Kumpole (n = 7), Psikpé (n = 2) and Sissili Bridge (n = 6) in Ghana were infected with trypanosomes, and the overall prevalence in seven out of nine locations was relatively > 53% (Table 4). Trypanosome prevalence in the other tsetse species fluctuated greatly with location, i.e., from 0% in the G. p. gambiensis flies collected in Comoé, Kenedougou and Bama to 34.5% in Moussodougou in Burkina Faso (Table 5). A similar trend was found in G. p. gambiensis flies collected in Mali and Guinea.
Table 4.
Trypanosome prevalence in natural populations of Glossina tachinoides collected from Ghana
| Location | Sample size | Prevalence |
|---|---|---|
| Bougouhiya | 19 | (3/19) 15.78% |
| Fumbissi | 15 | (15/15) 100% |
| Grogro | 11 | (11/11) 100% |
| Kumpole | 7 | (7/7) 100% |
| Mortani | 41 | (22/41) 53.65% |
| Nabogo | 2 | (0/2) 0% |
| Psikpé | 2 | (2/2) 100% |
| Sissili Bridge | 6 | (6/6) 100% |
| Walewale | 131 | (77/131) 58.77% |
| Total | 234 | (143/234) 61.11% |
Table 5.
Trypanosome prevalence in natural populations of Glossina palpalis gambiensis collected from Burkina Faso
| Location | Sample size | Prevalence |
|---|---|---|
| Bama | 77 | (0/77) 0% |
| Comoé | 123 | (3/123) 2.43% |
| Folonzo | 237 | (27/237) 11.39% |
| Kartasso | 136 | (0/136) 0% |
| Kenedougou | 41 | (0/41) 0% |
| Moussodougou | 142 | (49/142) 34.50% |
| Total | 731 | (77/731) 10.53% |
Prevalence of different trypanosome species in wild populations of tsetse in Western Africa
The results indicate that tsetse flies in West Africa could be infected with different species of trypanosomes in single or multiple infections. For T. vivax prevalence the best model retained countries as variable that fitted well the data indicating that the prevalence of T. vivax alone, did not differ significantly among tsetse fly species and sex (Additional file 1) but the mean infection rate of T. vivax in Senegal was significantly higher as compared to other countries (P < 0.05), also the prevalence in Ghana was significantly higher as compared to Guinea (P = 0.030; Fig. 2; Additional file 1).
Fig. 2.

a Prevalence of Trypanosoma vivax, Trypanosoma congolense and Trypanosoma spp single infection according to country (a) and tsetse species (b). Boxes extend between the 25th and 75th percentile. A thick line denotes the median. The whiskers extend up to the most extreme values. Gmed: Glossina medicorum, Gmsm: G. morsitans submositans, Gpg: G. palpalis gambiensis and Gt: G. tachinoides. Different letters indicate significant difference of trypanosome infection prevalence between counties (A) and tsetse species (B)
GLM results for single infections with T. congolense selected for species as variable that fitted well the data indicated that the prevalence of T. congolense alone did not differ significantly among countries and sex (Fig. 2). The T. congolense infection rate in G. medicorum was significantly higher as compared to G. tachinoides, G. p. gambiensis and G. m. submorsitans (P < 0.05); Additional file 1). T. congolense infection rate in G. p. gambiensis was significantly lower as compared to G. m. submorsitans (Fig. 2B; Additional file 1).
Non-specific detection of Trypanosoma spp. (Tz) (including T. brucei, T. evansi, T. equiperdum and T. theileri) based on the primer detection was recorded in 19.4% of the samples (Fig. 3). Results model selected for countries as variable that fitted well the data indicating that the prevalence of Trypanosoma spp. did not differ significantly among countries and sex. The Trypanosoma spp. prevalence in Ghana was significantly higher than the other countries (P < 0.001; Fig. 4A; Additional file 1).
Fig. 3.
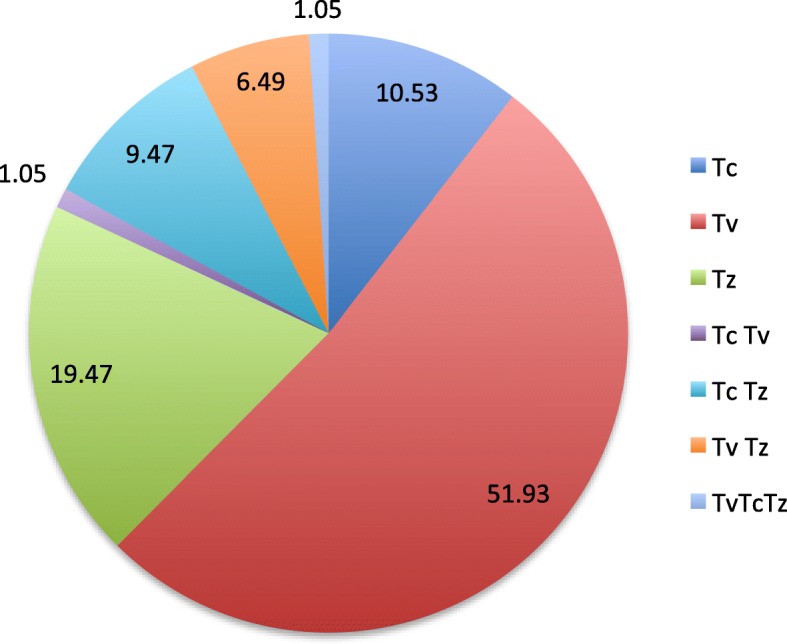
Prevalence of Trypanosome single and mixed infection if different tsetse species collected from west Africa
Fig. 4.
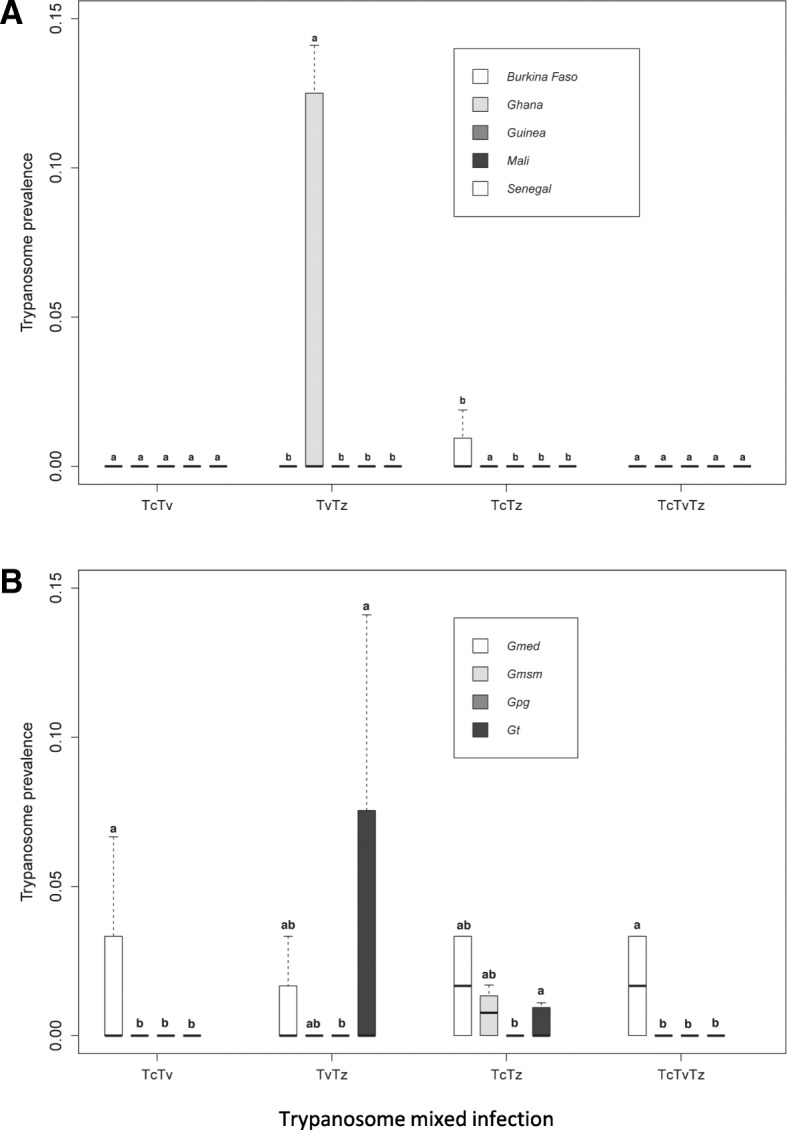
Prevalence of Trypanosome coinfection according to the country (A) and tsetse species (B). Boxes extend between the 25th and 75th percentile. A thick line denotes the median. The whiskers extend up to the most extreme values. Gmed: Glossina medicorum, Gmsm: G. morsitans submositans, Gpg: G. palpalis gambiensis and Gt: G. tachinoides. Tv: Trypanosoma vivax, Tc: Trypanosoma congolensis and Tz: Trypanosoma spp (T. brucei, T. evansi, T. equiperdum and T. theileri). Different letters indicate significant difference of trypanosome mixed infection prevalence between counties (A) and tsetse species (B)
Analysis of the data with the well fitted model indicated that the coinfection of T. congolense with T. vivax did not differ between countries and sex. However, T. congolense and T. vivax coinfection was significantly higher in G. medicorum (1.1%) as compared with the other tsetse species (P = 0.001; Fig. 4B; Additional file 1). The coinfection rate of T. vivax and other Trypanosoma spp in Ghana was significantly higher than all other countries (P < 0.01, Fig. 4A; Additional file 1). Analysis of coinfection of T. congolense and other Trypanosoma spp (7.5%) indicated that the infection rate in Ghana was significantly higher than Burkina Faso (P < 0.01, Fig. 4A; Additional file 1).
Analysis of triple infection of T. vivax, T. congolense with other Trypanosoma spp selected for species as variable that fitted well the data indicating that the prevalence of Trypanosoma spp. did not differ significantly among countries and sex. The infection rate in G. medicorum (1.1%) was significantly higher than in the other tsetse species (0%) (P < 0.001; Additional file 1).
SGHV prevalence
Based on the PCR screen used in the present study, the average prevalence of SGHV in all collected flies was 1.7% (n = 54) (Table 2). The prevalence varied from 0% in G. tachinoides samples from Ghana and G. p. gambiensis samples from Senegal and Guinea to 4.1% in G. p. gambiensis flies from Mali (Fig. 5). The result indicated that the SGHV prevalence did not differ significantly among species and sex. However, the virus prevalence was significantly higher in Mali compared with the other countries (P = 0.001; Additional file 1).
Fig. 5.
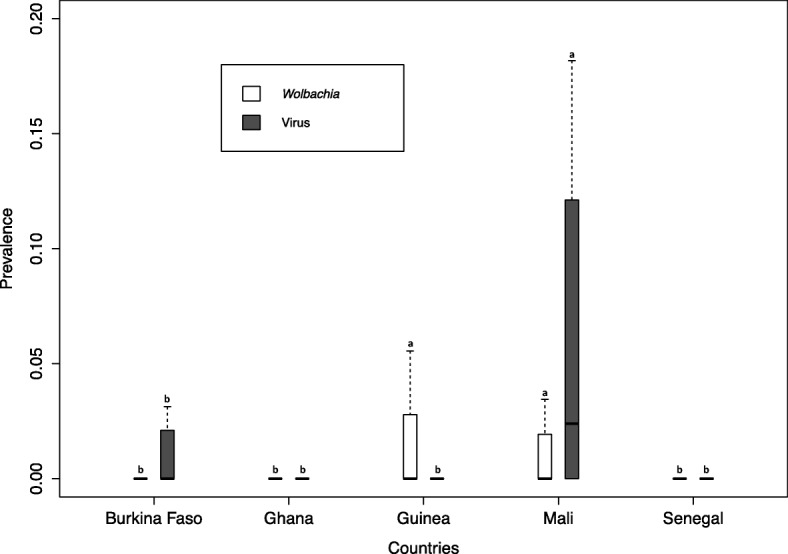
Prevalence of Salivary gland hypertrophy virus (SGHV) and Wolbachia according to the country (A) and tsetse species (B). Boxes extend between the 25th and 75th percentile. A thick line denotes the median. The whiskers extend up to the most extreme values. Gmed: Glossina medicorum, Gmsm: G. morsitans submositans, Gpg: G. palpalis gambiensis and Gt: G. tachinoides. Different letters indicate significant difference
Prevalence of Wolbachia
The prevalence of Wolbachia was low in all tested species and averaged at 1.0% (Table 3). The prevalence did not differ significantly among species and sex. The Wolbachia prevalence in Mali was significantly higher as compared to Senegal, Ghana and Burkina Faso (P < 0.05; Additional file 1). No other significant difference was observed (Fig. 4).
Mixed infection of trypanosomes, SGHV and Wolbachia
The prevalence data indicate that the mean trypanosome infection rate was higher as compared with the prevalence of the SGHV and Wolbachia. Most of the flies (99.94%) that were infected with trypanosomes were negative for Wolbachia. In G. tachinoides and G. m. submorsitans, double infection with SGHV and trypanosomes was observed at a low prevalence, i. e. 0.5% and 0.4% respectively. No double infection of SGHV and trypanosome was detected in G. p. gambiensis. The Trypanosoma spp. infection rate was significantly positively correlated with that of the virus (P < 0.001), although the correlation was weak (r = 0.45). No significant correlation was observed between Wolbachia and SGHV.
Impact of tsetse fly gender on trypanosomes, SGHV and Wolbachia prevalence
There was no significant difference between male and female infection by trypanosomes (P = 0.377), SGHV (P = 0.739) or Wolbachia (P = 0.362).
Trypanosomes, SGHV and Wolbachia distribution per countries
Burkina Faso showed the highest species diversity with four tsetse species collected: G. p. gambiensis, G. tachinoïdes, G. m. submorsitans and G. medicorum. Among the ten localities sampled, these four species were found together in Folonzo and Comoe. G. p. gambiensis flies were found in four other localities: Bama, Kartasso, Kenedougou and Mousodougou. G. tachinoïdes and G. m. submorsitans flies were found together in Sissili, however, in Arly G. tachinoïdes only was found (Table 2). Flies infected with trypanosomes were found in five localities. Trypanosoma vivax prevalence was not different between localities and species (Additional file 1). For T. congolense no differences between localities were highlighted. However, significant differences were observed between tsetse species. G. medicorum was the most infected species (9%) and was different from all other species (G. m. submorsitans 5.2%; G. tachinoïdes 2.4% and G. p. gambiensis 0.4%; Additional file 1). For Trypanosoma spp., significant differences were observed between tsetse species in Comoe and Folonzo. In both localities, G. medicorum (3.2% and 30% respectively) was significantly more infected than G. m. submorsitans (0.4% and 0.7% respectively) and G. tachinoïdes (0.2% and 1.5%) (Additional file 1). Flies infected with SGHV were found in four localities. No difference between tsetse species and localities was observed (Additional file 1). Wolbachia prevalence was not different between species. Tsetse flies (G. tachinoïdes, G. p. gambiensis, G. medicorum and G. m. submorsitans) from two localities were infected with Wolbachia. Wolbachia prevalence in tsetse flies from Kenedougou was significantly more important than Comoe (2.4% and 0.5% respectively).
In Mali, flies from only one tsetse species (G. p. gambiensis) were collected in the ten localities sampled. T. vivax infection was found in seven localities and the prevalence in Baoule (42.8%) was significantly higher than the others (Bagnuineda 16.6%, Banko 21.9%, Bani 1.4%, Kita 16.6%, Système Niger 1.1%, Système Sénégal 2%; Additional file 1). T. congolense was only found in Système Niger (1.1%) and Trypanosoma spp. in Sikasso (3.4%) and Système Niger (2.3%) with no differences. SGHV was found in the ten localities of Mali and Wolbachia in four without any differences (Additional file 1).
In Senegal, only G. p. gambiensis were found between the seven localities sampled. T. congolense infection was not found, however T. vivax infection was found in five localities (Mako, Fleuve G, Fleuve Gambie, Niokolo and Tambacounda) and Trypanosoma sp in two (Diaguiri and Tambacounda). No significant differences in trypanosome prevalence were found between different localities (Additional file 1). No SGHV and Wolbachia were found in tsetse flies analysed.
In Ghana, G. tachinoides was the only species caught among the eleven localities sampled and eight of them were found positive for trypanosomes. For T. vivax, significant differences in trypanosome prevalence were found between localities. The locality of Grogro showed the highest prevalence (36%) and was significantly different from all localities except Fumbissi. On the contrary, the locality of Bougouhiya showed the lowest prevalence (0.05%) and was significantly different from Fumbissi, Grogro and Kumpole. Fumbissi was also different from Mortani, Sissili bridge and Walewale (Additional file 1). T. congolense was only found in one locality: Walewale. Trypanosoma spp. was found in the eight positive localities. Among these, flies collected at the localities of Kandiaga and Sissili bridge were the most infected (100% and 83% respectively) and were significantly different from all others but not between them. No virus and Wolbachia were found.
In Guinea, G. tachinoides was the only species caught from all localities. Out of eight localities sampled, tsetse flies collected from six of them were found positive for trypanosomes. T. congolense and Trypanosoma spp. were not found and no significant difference in trypanosome prevalence for T. vivax was observed (Additional file 1). SGHV was absent and Wolbachia was found in three localities but no difference in prevalence was observed (Additional file 1).
Discussion
The results of this study indicate an overall low prevalence of SGHV and Wolbachia and a high prevalence of trypanosomes in the sampled wild tsetse populations. The prevalence of all three microbes varied between species and between locations but there was no significant difference between male and female flies. All flies sampled in Kimpole (100%), Grogro (100%), Fumbissi (100%), Sissili Bridge (100%) and Psikpe (100%) of Ghana were infected with trypanosomes, an infection rate that was significantly higher as compared to other locations. In some cases, mixed infections with different trypanosome species were detected, as well as mixed infections of trypanosomes and SGHV. However, no mixed infection of trypanosomes or SGHV with Wolbachia was detected.
The method of detection and characterization of the type of trypanosome infection using the ribosomal internal transcribed spacer (ITS) is known to be sensitive and it provides quick information about the trypanosome type circulating in the infected area. However, these identified trypanosomes may not be the only ones circulating within the different areas as was observed in Guinea. Other types of trypanosome species may also be circulating but due to the lack of PCR primers cannot be identified [54]. In addition, Pagabeleguem et al. [55] noted that the trypanosome infection rate in tsetse flies was always higher by microscopy than PCR and suggested that almost half of the flies were infected by trypanosome species non-pathogenic for cattle.
The relatively high frequency of pathogenic trypanosomes in tsetse was previously linked to high AAT prevalence in cattle, especially in the locality of Folonzo in Burkina Faso [55]. It has therefore been suggested that the detection of trypanosome infection in tsetse flies might provide indirect information about the AAT prevalence in livestock in the selected area and hence the potential risk of uninfected animals to become infected. This may not be so relevant for HAT as the link between tsetse infection and disease prevalence is considered to be weak. In Guinea, for example, T. brucei gambiense is the pathogenic trypanosome identified in humans, while no T. brucei gambiense infection has been found in tsetse confirming the usual very low (0.1%) mature infection rates of T. brucei gambiense in tsetse, even in active sleeping sickness foci [56].
The SGHV was reported in G. p. palpalis in Côte d’Ivoire in 1978 at a very low prevalence (0.3%) [57]. Although the prevalence of SGHV based on fly dissection was generaly low in wild tsetse populations (0.5–5%) [58], the prevalence detected by PCR can be very high (100%) [47]. These results clearly indicate that the SGHV prevalence in tsetse species in West Africa is significantly lower than the SGHV prevalence in G. pallidipes in eastern and southern Africa previously reported [47], where the virus prevalence varied from 2 to 100%, depending on the location. However, the low virus prevalence in West African tsetse populations might be underestimated due to the primer specificity and the sensitivity of the PCR, as all primers were based on the nucleotide sequence of G. pallidipes SGHV. A different virus sequence in other tsetse species in West Africa would then result in a lower detection rate. To overcome this problem, it is suggested to have the entire genome sequenced of each virus detected in each tsetse species to enable the selection of more specific and sensitive primers for virus detection.
Wolbachia is known to be present in wild tsetse populations [29, 59], and using standard PCR assays, it was detected in G. m. morsitans, G. m. centralis and G. austeni populations, but not in G. tachinoides. Using alternative assays Wolbachia was also detected at low infection rates in G. fuscipes and G. morsitans subspecies [59, 60]. The prevalence of Wolbachia in G. p. gambiensis from Burkina Faso was very low (~ 0.14%) In G. m. morsitans the prevalence of Wolbachia was higher and varied between 10 and 100% depending on the location [51]. In G. f. fuscipes collected from Uganda, the prevalence of Wolbachia varied between 26 and 55%, which is higher than the prevalence reported in this study [29]. It is important to note that in the study of Alam and colleagues the detection method used for screening the Wolbachia infection was the sequential PCR method (high sensitivity but low specificity). In this study and in the study of Doudoumis and colleagues, a traditional one step PCR was used for the detection [29, 59] to avoid any non-specific detection and to detect only high level Wolbachia infections that might interfere with the virus and trypanosome infection. We also tried to avoid detecting Wolbachia chromosomal insertions by using primers specific for active Wolbachia in the cytoplasm [29, 61]. Presence of extensive Wolbachia insertions was discovered in the genome of its host G. m morsitans [61]. The low prevalence of Wolbachia detected in wild tsetse populations in this study might be due to (i) the absence of Wolbachia infection, (ii) the low titer of Wolbachia infection or (iii) the presence of another Wolbachia strain that cannot be detected with the primers used in this study.
Mixed infections of trypanosomes, SGHV and Wolbachia have been previously reported [59] and this was also the case in our study, although the correlation was low (r = 0.45; P < 0.001). In the study of Alam et al. [59], the author mentioned the potential negative relationship between Wolbachia and SGHV infection, which was also observed in our study. Trypanosome infection was found in flies that were also infected with the SGHV but no flies that were infected with Wolbachia showed a trypanosome infection. This suggests that the presence of Wolbachia might mediate the presence of different pathogens and parasites, as previously described [36, 62, 63]. Due to the low prevalence of Wolbachia, no possible correlation between the Wolbachia infection and the trypanosomes and/or SGHV could be found. On the other hand, a negative impact of trypanosome infection on Wolbachia presence cannot be excluded. However, these antagonistic relationships need further investigation and statistical analysis. If the assumption that Wolbachia might block trypanosome transmission is correct, these novel insights could be useful for the development and implementation of sterile insect technique-based population control strategies, e.g. releasing Wolbachia-infected males that both induce cytoplasmic incompatibility when mated with wild Wolbachia–free females and being refractory for trypanosome infection and transmission in a way similar to that recently developed for mosquitoes [64–67].
Conclusion
The results of this study indicate a high rate of trypanosome infection in tsetse wild populations but lower infection rate of both Wolbachia and SGHV. Mixed infections with different trypanosome species or trypanosome with SGHV were found. The high rate of trypanosome infection in tsetse populations might be used as an indicator of the presence of trypanosomiosis in both human and animal by determining the different trypanosomes circulation in the targeted area. The low prevalence of Wolbachia in tsetse flies in West Africa and the lack of mixed infection of Trypanosoma spp., and Wolbachia, which might indicate an antagonistic relationship, require further investigation. The low prevalence of SGHV in the field population is encouraging for SIT programmes as it might exclude the SGHV outbreaks in tsetse mass-rearing established from such low infected populations; however, it encourages the implementation of the virus management strategies to control the virus infection to avoid such problem.
Additional file
Generalized linear model (GLM) fixed effect statistical results. (DOC 269 kb)
Acknowledgements
We thank Dr. Stijn Deborggraeve and Dr. Jan van den Abbeele from the Institute of Tropical Medicine, Antwerp, Belgium for providing reference trypanosome DNA. We thank Abdul Hasim Mohammed, Edgardo Lapiz, Henry Adun and Carmen Marin for their technical assistance, the field teams that helped in the tsetse sampling within the different countries.
Funding
This work and the publication fees were funded by the Joint FAO/IAEA Division of Nuclear Techniques in Food and Agriculture, IAEA (CRP No.: D4.20.15 and Technical cooperation Project (BKF 5070) funding fellowship BKF 16016) Vienna, Austria.
Availability of data and materials
Materials described in the manuscript, including all relevant raw data, are available in this link https://dataverse.harvard.edu/dataset.xhtml?persistentId=doi:10.7910/DVN/X38X5B.
About this supplement
This article has been published as part of BMC Microbiology Volume 18 Supplement 1, 2018: Enhancing Vector Refractoriness to Trypanosome Infection. The full contents of the supplement are available online at https://bmcmicrobiol.biomedcentral.com/articles/supplements/volume-18-supplement-1.
Abbreviations
- AAT
Animal African trypanosomosis
- AICc
Akaike information criterion
- AW-IPC
Area-wide integrated pest management programs
- GpSGHV
Glossina pallidipes salivary gland hypertrophy virus
- HAT
Human African trypanosomosis
- IPCL
Insect Pest Control Laboratory
- ITS
Internal transcribed spacers
- PBS
Phosphate Buffer Saline
- qPCR
Quantitative polymerase chain reaction
- SGHV
Salivary gland hypertrophy virus
- SIT
Sterile Insect Technique
- T
Trypanosoma
Authors’ contributions
AMMA, AGP, BB, TA, SI, OAG: designed and supervised the research. OGMS, GDU, AA, AGP, AMMA: conducted the experiments. GG, OGMS, AGP, collected and analyzed data and prepared the figures. OGMS, ATC, PT, AGP, RJB: Provided live material for experiments. OGMS, GDU, AGP, MJBV, BK, RJB, GG, BB, TA, SI: participated in the writing of the manuscript. All authors have read and agreed to its content and that the manuscript conforms to the journal’s policies. All authors have read and agreed on the final version on the manuscript.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Steelman CD. Effects of external and internal arthropod parasites on domestic livestock production. Annu Rev Entomol. 1976;21:155–178. doi: 10.1146/annurev.en.21.010176.001103. [DOI] [PubMed] [Google Scholar]
- 2.WHO . Report of the Scientific Working Group meeting on African trypanosomiasis, Geneva, 4–8 June, 2001. Geneva: World Health Organization; 2003. [Google Scholar]
- 3.Jordan AM. Trypanosomiasis control and African rural development. London: Longman; 1986. [Google Scholar]
- 4.Simarro PP, Jannin J, Cattand P. Eliminating human African trypanosomiasis: where do we stand and what comes next? PLoS Med. 2008;5:e55. doi: 10.1371/journal.pmed.0050055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Solano P, Jamonneau V, N'guessan P, N'dri L, Dje NN, Miezan TW, Lejon V, Büscher P, Garcia A. Comparison of different DNA preparation protocols for PCR diagnosis of human African trypanosomosis in cote d'Ivoire. Acta Trop. 2002;82:349–356. doi: 10.1016/S0001-706X(02)00029-3. [DOI] [PubMed] [Google Scholar]
- 6.Nakayima J, Nakao R, Alhassan A, Mahama C, Afakye K, Sugimoto C. Molecular epidemiological studies on animal trypanosomiases in Ghana. Parasit Vectors. 2012;5:217. doi: 10.1186/1756-3305-5-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Takeet MI, Fagbemi BO, De DM, Yakubu A, Rodulfo HE, Peters SO, Wheto M, Imumorin IG. Molecular survey of pathogenic trypanosomes in naturally infected Nigerian cattle. Res Vet Sci. 2013;94:555–561. doi: 10.1016/j.rvsc.2012.10.018. [DOI] [PubMed] [Google Scholar]
- 8.Njiru ZK, Constantine CC, Guya S, Crowther J, Kiragu JM, Thompson RCA, Davila AMR. The use of ITS1 rDNA PCR in detecting pathogenic African trypanosomes. Parasitology. 2005;95:186–192. doi: 10.1007/s00436-004-1267-5. [DOI] [PubMed] [Google Scholar]
- 9.Aksoy S, Rio RVM. Interactions among multiple genomes: tsetse, its symbionts and trypanosomes. Insect Biochem Mol Biol. 2005;35:691–698. doi: 10.1016/j.ibmb.2005.02.012. [DOI] [PubMed] [Google Scholar]
- 10.Leak SGA. Tsetse biology and ecology: their role in the epidemiology and control of trypanosomosis. Wallingford: CABI Publishing; 1998. [Google Scholar]
- 11.Klassen W, Curtis CF. History of the sterile insect technique. In: Dyck VA, Hendrichs J, Robinson AS, editors. Sterile Insect Technique: Principles and Practice in Area-Wide Integrated Pest Management. Dordrecht: Springer; 2005. pp. 1–34. [Google Scholar]
- 12.Vreysen MJB, Robinson AS, Hendrichs JP. Area-wide control of insect pests: from research to field implementation. Dordrecht: Springer; 2007. [Google Scholar]
- 13.Msangi AR, Saleh KM, Kiwia N, Malele II, Mussa WA, Mramba F, Juma KG, Dyck VA, Vreysen MJB, Parker AG, Feldmann U, Zhu Z-R, Pan H. Success in Zanzibar: Eradication of tsetse. In: Tan K-H, editor. Area-wide Control of Fruit Flies and other Insect Pests. Penang: Penerbit Universiti Sains Malaysia; 2000. pp. 57–66. [Google Scholar]
- 14.Cuisance D, Politzar H, Merot P, Tamboura I. Les lachers de males irradies dans la campagne de lutte integree contre les glossines dans la zone pastorale de sideradougou (Burkina Faso) Rev Elev Med Vet Pays Trop. 1984;37:449–467. [PubMed] [Google Scholar]
- 15.Oladunmade MA, Feldmann U, Takken W, Tenabe SO, Hamann HJ, Onah JA, Dengwat L, Van der Vloedt AMV, Gingrich RE. Sterile insect technique for tsetse control and eradication, STI/PUB/830. Vienna: International Atomic Energy Agency; 1990. Eradication of Glossina palpalis palpalis (Robineau-Desvoidy) (Diptera: Glossinidae) from agropastoral land in Central Nigeria by means of the sterile insect technique; pp. 5–23. [Google Scholar]
- 16.Abd-Alla AMM, Vlak JM, Bergoin M, Maruniak JE, Parker AG, Burand JP, Jehle JA, Boucias DG. Hytrosaviridae: a proposal for classification and nomenclature of a new insect virus family. Arch Virol. 2009;154:909–918. doi: 10.1007/s00705-009-0398-5. [DOI] [PubMed] [Google Scholar]
- 17.Abd-Alla AMM, Parker AG, Vreysen MJB, Bergoin M. Tsetse salivary gland hypertrophy virus: Hope or hindrance for tsetse control? PLoS Negl Trop Dis. 2011;5:e1220. doi: 10.1371/journal.pntd.0001220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lietze VU, Abd-Alla AMM, Vreysen MJB, Geden CJ, Boucias DG. Salivary gland hypertrophy viruses: a novel group of insect pathogenic viruses. Annu Rev Entomol. 2010;56:63–80. doi: 10.1146/annurev-ento-120709-144841. [DOI] [PubMed] [Google Scholar]
- 19.Abd-Alla AMM, Kariithi HM, Mohamed AH, Lapiz E, Parker AG, Vreysen MJB. Managing hytrosavirus infections in Glossina pallidipes colonies: feeding regime affects the prevalence of salivary gland hypertrophy syndrome. PLoS One. 2013;8:e61875. doi: 10.1371/journal.pone.0061875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abd-Alla AMM, Marin C, Parker A, Vreysen M. Antiviral drug valacyclovir treatment combined with a clean feeding system enhances the suppression of salivary gland hypertrophy in laboratory colonies of Glossina pallidipes. Parasit Vectors. 2014;7:214. doi: 10.1186/1756-3305-7-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aksoy S. Tsetse- a haven for microorganisms. Parasitol Today. 2000;16:114–118. doi: 10.1016/S0169-4758(99)01606-3. [DOI] [PubMed] [Google Scholar]
- 22.Nogge G. Sterility in tsetse flies (Glossina morsitans Westwood) caused by loss of symbionts. Experientia. 1976;32:995–996. doi: 10.1007/BF01933932. [DOI] [PubMed] [Google Scholar]
- 23.Pais R, Lohs C, Wu Y, Wang JW, Aksoy S. The obligate mutualist Wigglesworthia glossinidia influences reproduction, digestion, and immunity processes of its host, the tsetse fly. Appl Environ Microbiol. 2008;74:5965–5974. doi: 10.1128/AEM.00741-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aksoy S, Chen X, Hypsa V. Phylogeny and potential transmission routes of midgut-associated endosymbionts of tsetse (Diptera: Glossinidae) Insect Mol Biol. 1997;6:183–190. doi: 10.1111/j.1365-2583.1997.tb00086.x. [DOI] [PubMed] [Google Scholar]
- 25.Cheng Q, Aksoy S. Tissue tropism, transmission and expression of foreign genes in vivo in midgut symbionts of tsetse flies. Insect Mol Biol. 1999;8:125–132. doi: 10.1046/j.1365-2583.1999.810125.x. [DOI] [PubMed] [Google Scholar]
- 26.Dale C, Maudlin I. Sodalis gen. nov. and Sodalis glossinidius sp. nov., a microaerophilic secondary endosymbiont of the tsetse fly Glossina morsitans morsitans. Int J Syst Bacteriol. 1999;49(Pt 1):267–275. doi: 10.1099/00207713-49-1-267. [DOI] [PubMed] [Google Scholar]
- 27.Saridaki A, Bourtzis K. Wolbachia: more than just a bug in insects' genitals. Curr Opin Microbiol. 2010;13:67–72. doi: 10.1016/j.mib.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 28.Werren JH, Baldo L, Clark ME. Wolbachia: master manipulators of invertebrate biology. Nat Rev Microbiol. 2008;6:741–751. doi: 10.1038/nrmicro1969. [DOI] [PubMed] [Google Scholar]
- 29.Doudoumis V, Tsiamis G, Wamwiri F, Brelsfoard C, Alam U, Aksoy E, Dalaperas S, Abd-Alla A, Ouma J, Takac P, Aksoy S, Bourtzis K. Detection and characterization of Wolbachia infections in laboratory and natural populations of different species of tsetse flies (genus Glossina) BMC Micobiology. 2012;12:S3. doi: 10.1186/1471-2180-12-S1-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bian G, Xu Y, Lu P, Xie Y, Xi Z. The endosymbiotic bacterium Wolbachia induces resistance to dengue virus in Aedes aegypti. PLoS Pathog. 2010;6:e1000833. doi: 10.1371/journal.ppat.1000833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bian G, Joshi D, Dong Y, Lu P, Zhou G, Pan X, Xu Y, Dimopoulos G, Xi Z. Wolbachia invades Anopheles stephensi populations and induces refractoriness to plasmodium infection. Science. 2013;340:748–751. doi: 10.1126/science.1236192. [DOI] [PubMed] [Google Scholar]
- 32.Frentiu FD, Robinson J, Young PR, McGraw EA, O'Neill SL. Wolbachia-mediated resistance to dengue virus infection and death at the cellular level. PLoS One. 2010;5:e13398. doi: 10.1371/journal.pone.0013398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Glaser RL, Meola MA. The native Wolbachia endosymbionts of Drosophila melanogaster and Culex quinquefasciatus increase host resistance to West Nile virus infection. PLoS One. 2010;5:e11977. doi: 10.1371/journal.pone.0011977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hedges LM, Brownlie JC, O'Neill SL, Johnson KN. Wolbachia and virus protection in insects. Science. 2008;322:702. doi: 10.1126/science.1162418. [DOI] [PubMed] [Google Scholar]
- 35.Lu P, Bian G, Pan X, Xi Z. Wolbachia induces density-dependent inhibition to dengue virus in mosquito cells. PLoS Negl Trop Dis. 2012;6:e1754. doi: 10.1371/journal.pntd.0001754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Moreira LA, Iturbe-Ormaetxe I, Jeffery JA, Lu G, Pyke AT, Hedges LM, Rocha BC, Hall-Mendelin S, Day A, Riegler M, Hugo LE, Johnson KN, Kay BH, McGraw EA, van den Hurk AF, Ryan PA, O'Neill SL. A Wolbachia symbiont in Aedes aegypti limits infection with dengue, Chikunguya, and Plasmodium. Cell. 2009;139:1268–1278. doi: 10.1016/j.cell.2009.11.042. [DOI] [PubMed] [Google Scholar]
- 37.Pan X, Zhou G, Wu J, Bian G, Lu P, Raikhel AS, Xi Z. Wolbachia induces reactive oxygen species (ROS)-dependent activation of the toll pathway to control dengue virus in the mosquito Aedes aegypti. Proc Natl Acad Sci U S A. 2012;109:E23–E31. doi: 10.1073/pnas.1116932108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tsai KH, Huang CG, Wu WJ, Chuang CK, Lin CC, Chen WJ. Parallel infection of Japanese encephalitis virus and Wolbachia within cells of mosquito salivary glands. J Med Entomol. 2006;43:752–756. doi: 10.1093/jmedent/43.4.752. [DOI] [PubMed] [Google Scholar]
- 39.van den Hurk AF, Hall-Mendelin S, Pyke AT, Frentiu FD, McElroy K, Day A, Higgs S, O'Neill SL. Impact of Wolbachia on infection with chikungunya and yellow fever viruses in the mosquito vector Aedes aegypti. PLoS Negl Trop Dis. 2012;6:e1892. doi: 10.1371/journal.pntd.0001892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Walker T, Johnson PH, Moreira LA, Iturbe-Ormaetxe I, Frentiu FD, McMeniman CJ, Leong YS, Dong Y, Axford J, Kriesner P, Lloyd AL, Ritchie SA, O'Neill SL, Hoffmann AA. The wMel Wolbachia strain blocks dengue and invades caged Aedes aegypti populations. Nature. 2011;476:450–453. doi: 10.1038/nature10355. [DOI] [PubMed] [Google Scholar]
- 41.Doudoumis V, Blow F, Saridaki A, Augustinos A, Dyer NA, Goodhead I, Solano P, Rayaisse JB, Takac P, Mekonnen S, Parker AG, Abd-Alla AMM, Darby A, Bourtzis K, Tsiamis G. Challenging the Wigglesworthia, Sodalis, Wolbachia symbiosis dogma in tsetse flies: Spiroplasma is present in both laboratory and natural populations. Sci Rep. 2017;7:4699. doi: 10.1038/s41598-017-04740-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Challier A, Laveissiere C: Un nouveau piege pour la capture des glossines (Glossina: Diptera, Muscidae): description et essais sur le terrain. Cah ORSTOM, Sér Ent Méd Parasitol 1973, XI:251–262.
- 43.Laveissiere C, Grébaut P. Recherches sur les pièges à glossines (Diptera: Glossinidae). Mise au point d' un modèle èconomique: Le piège >> Vavoua <<. Trop Med Parasitol. 1990;41:185–192. [PubMed] [Google Scholar]
- 44.Laveissiere C, Eouzan JP, Pascal G, Lemasson JJ. The control of riverine tsetse. Insect Sci Appl. 1990;11:427–441. [Google Scholar]
- 45.Rayaisse JB, Krober T, McMullin A, Solano P, Mihok S, Guerra CA. Standardizing visual control devices for tsetse flies: west African species Glossina tachinoides, G palpalis gambiensis and G morsitans submorsitans. PLoS Negl Trop Dis. 2012;6:e1491. doi: 10.1371/journal.pntd.0001491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Potts WH. Glossinidae (tsetse-flies) In: Kenneth GV, KGV S, editors. Insects and other arthropods of medical importance. London: The British Museum; 1973. pp. 209–249. [Google Scholar]
- 47.Kariithi HM, Ahmadi M, Parker AG, Franz G, Ros VID, Haq I, Elashry AM, Vlak JM, Bergoin M, Vreysen MJB, Abd-Alla AMM. Prevalence and genetic variation of salivary gland hypertrophy virus in wild populations of the tsetse fly Glossina pallidipes from southern and eastern Africa. J Invertebr Pathol. 2013;112:S123–S132. doi: 10.1016/j.jip.2012.04.016. [DOI] [PubMed] [Google Scholar]
- 48.Baker MD, Krafsur ES. Identification and properties of microsatellite markers in tsetse flies Glossina morsitans lato (Diptera: Glossinidae) Mol Ecol. 2001;1:234–236. doi: 10.1046/j.1471-8278.2001.00087.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fikru R, Goddeeris BM, Delespaux V, Moti Y, Tadesse A, Bekana M, Claes F, De Deken R, Buscher P. Widespread occurrence of Trypanosoma vivax in bovines of tsetse- as well as non-tsetse-infested regions of Ethiopia: a reason for concern? Vet Parasitol. 2012;190:355–361. doi: 10.1016/j.vetpar.2012.07.010. [DOI] [PubMed] [Google Scholar]
- 50.Zabalou S, Riegler M, Theodorakopoulou M, Stauffer C, Savakis C, Bourtzis K. Wolbachia-induced cytoplasmic incompatibility as a means for insect pest population control. Proc Natl Acad Sci U S A. 2004;101:15042–15045. doi: 10.1073/pnas.0403853101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.R Development Core Team . R: a language and environment for statistical computing. Vienna: R Foundation for statistical Computing; 2010. [Google Scholar]
- 52.Burnham KP, Anderson DR. Model selection and multimodel inference: A practical information-theoretic approach. 2nd ed. edition. New-York: Springer-Verlag; 2002. [Google Scholar]
- 53.Hurvich CM, Tsai CL. Model selection for extended quasi-likelihood models in small samples. Biometrics. 1995;51:1077–1084. doi: 10.2307/2533006. [DOI] [PubMed] [Google Scholar]
- 54.Kagbadouno MS, Camara M, Rouamba J, Rayaisse JB, Traore IS, Camara O, Onikoyamou MF, Courtin F, Ravel S, De Meeûs T, Bucheton B, Jamonneau V, Solano P. Epidemiology of sleeping sickness in Boffa (Guinea): where are the trypanosomes? PLoS Negl Trop Dis. 2012;6:e1949. doi: 10.1371/journal.pntd.0001949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pagabeleguem S, Sangare M, Bengaly Z, Akoudjin M, Belem AM, Bouyer J. Climate, cattle rearing systems and African animal Trypanosomosis risk in Burkina Faso. PLoS One. 2012;7:e49762. doi: 10.1371/journal.pone.0049762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jamonneau V, Ravel S, Koffi M, Kaba D, Zeze DG, Ndri L, Sane B, Coulibaly B, Cuny G, Solano P. Mixed infections of trypanosomes in tsetse and pigs and their epidemiological significance in a sleeping sickness focus of cote d'Ivoire. Parasitology. 2004;129:693–702. doi: 10.1017/S0031182004005876. [DOI] [PubMed] [Google Scholar]
- 57.Gouteux J-P. Prevalence of enlarged salivary glands in Glossina palpalis, G. pallicera, and G. nigrofusca (Diptera: Glossinidae) from the Vavoua area, Ivory Coast. J Med Entomol. 1987;24:268. doi: 10.1093/jmedent/24.2.268. [DOI] [PubMed] [Google Scholar]
- 58.Otieno LH, Kokwaro ED, Chimtawi M, Onyango P. Prevalence of enlarged salivary glands in wild populations of Glossina pallidipes in Kenya, with a note on the ultrastructure of the affected organ. J Invertebr Pathol. 1980;36:113–118. doi: 10.1016/0022-2011(80)90142-1. [DOI] [Google Scholar]
- 59.Alam U, Hyseni C, Symula RE, Brelsfoard C, Wu Y, Kruglov O, Wang J, Echodu R, Alioni V, Okedi LM, Caccone A, Aksoy S. Implications of microfauna-host interactions for trypanosome transmission dynamics in Glossina fuscipes fuscipes in Uganda. Appl Environ Microbiol. 2012;78:4627–4637. doi: 10.1128/AEM.00806-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Schneider DI, Garschall KI, Parker AG, Abd-Alla AMM, Miller WJ. Global Wolbachia prevalence, titer fluctuations and their potential of causing cytoplasmic incompatibilities in tsetse flies and hybrids of Glossina morsitans subgroup species. J Invertebr Pathol. 2013;112:S104–S115. doi: 10.1016/j.jip.2012.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Brelsfoard C, Tsiamis G, Falchetto M, Gomulski LM, Telleria E, Alam U, Doudoumis V, Scolari F, Benoit JB, Swain M, Takac P, Malacrida AR, Bourtzis K, Aksoy S. Presence of extensive Wolbachia symbiont insertions discovered in the genome of its host Glossina morsitans morsitans. PLoS Negl Trop Dis. 2014;8:e2728. doi: 10.1371/journal.pntd.0002728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kambris Z, Cook PE, Phuc HK, Sinkins SP. Immune activation by life-shortening Wolbachia and reduced filarial competence in mosquitoes. Science. 2009;326:134–136. doi: 10.1126/science.1177531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kambris Z, Blagborough AM, Pinto SB, Blagrove MS, Godfray HC, Sinden RE, Sinkins SP. Wolbachia stimulates immune gene expression and inhibits plasmodium development in Anopheles gambiae. PLoS Pathog. 2010;6:e1001143. doi: 10.1371/journal.ppat.1001143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhang D, Zheng X, Xi Z, Bourtzis K, Gilles JRL. Combining the sterile insect technique with the incompatible insect technique: I-impact of Wolbachia infection on the fitness of triple-and double-infected strains of Aedes albopictus. PLoS One. 2015;10:e0121126. doi: 10.1371/journal.pone.0121126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhang D, Lees RS, Xi Z, Gilles JRL, Bourtzis K. Combining the sterile insect technique with Wolbachia-based approaches: II-A safer approach to Aedes albopictus population suppression programmes, designed to minimize the consequences of inadvertent female release. PLoS One. 2015;10:e0135194. doi: 10.1371/journal.pone.0135194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhang D, Lees RS, Xi Z, Bourtzis K, Gilles JRL. Combining the sterile insect technique with the incompatible insect technique: III-robust mating competitiveness of irradiated triple Wolbachia-infected Aedes albopictus males under semi-field conditions. PLoS One. 2016;11:e0151864. doi: 10.1371/journal.pone.0151864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bourtzis K, Lees RS, Hendrichs J, Vreysen MJB. More than one rabbit out of the hat: radiation, transgenic and symbiont-based approaches for sustainable management of mosquito and tsetse fly populations. Acta Trop. 2016;157:115–130. doi: 10.1016/j.actatropica.2016.01.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Generalized linear model (GLM) fixed effect statistical results. (DOC 269 kb)
Data Availability Statement
Materials described in the manuscript, including all relevant raw data, are available in this link https://dataverse.harvard.edu/dataset.xhtml?persistentId=doi:10.7910/DVN/X38X5B.


