Abstract
The aim of this article was to present the treatment method applied to a patient who suffered from a multiple fracture of the right maxilla, as a result of an accident that happened to him at an early age. The main consequence of this injury was an inhibited growth of the maxillary bone segment due to the lack of functional stimulus. The treatment consisted of four phases: the removal of all the teeth in the upper right maxilla, the immediate restoration with bicortical implants, the immediate prosthetic rehabilitation, and closing the oroantral communication.
Keywords: Cortical anchorage, immediate loading, maxillary defect, Strategic Implant®, supporting polygon
INTRODUCTION
The dominant factor for the development of the craniomandibular complex and preservation of alveolar bone is – as in any other bone type – the presence of functional loading.[1,2]
The masticatory function is established symmetrically on both sides because its innervation stems from the same nucleus in the brain. Hanau introduced five factors affecting occlusal balance, and Planas applied some of Hanau's ideas and developed a comprehensive concept of the mechanical feedback given by occlusion and mastication.[3,4] Their work can be summarized in a sentence: if there is no balance in mastication, adaptive changes in jaw bone connected with the distribution of bone mass and mineralization, and changes in temporomandibular joint morphology will occur.[5,6] What is more, such changes may even influence our body posture.[7,8]
The main problem with patients after trauma or surgery of the craniofacial complex is to maintain or restore all those factors with a stable outcome. The treatment possibilities using classic implants are very often limited due to reduced bone base and limited applications of the conventional system itself.
Trauma, surgical defects secondary to malignant tumors, and genetic causes can result in facial disfigurement and dysfunction.[9,10,11,12] Poor quality or insufficient quantity of hard and soft tissues often influence the number of treatment options.[13,14,15] If significant parts of the mandible or the maxilla are missing, treatments with conventional dental implants are often not possible or require tremendous surgical efforts to rebuild the bone foundations for these surgical alternatives. Conventionally, patients with extensive defects of the maxilla are treated with obturator prostheses or undergo extensive bone graft procedures with various results.[16,17,18] Since prosthetic restorations are very important in terms of rehabilitation of those patients, appropriate retention, stability, and support of the prosthesis must be provided to achieve a successful outcome and reasonable life quality.[19,20]
CASE REPORT
A 28-year-old patient in good general health presented to our clinic and requested treatment in the upper and lower jaw. At the age of six, he was accidentally kicked by a horse, and as a result, the upper jaw fractured into multiple pieces. No treatment was provided at that time, and in the following years, the teeth kept growing, but no functional stimulus was exerted into the bone of the upper jaw on the fractured side. As a result, the teeth could not reach the plane of chewing, and they did not reach the normal spatial orientation within the arch. At the age of 28 years, the patient presented for consultation with a radiologic picture as shown in Figure 1. Although he had consulted with an orthodontist before, he was not offered any treatment.
Figure 1.

Preoperative panoramic overview picture. Inhibited growth of the maxillary bone on the injured right side, missing teeth in the lower jaw with tooth 45 being partially retented. Due to the abnormal function, the morphology of the right temporomandibular joint had altered
After a thorough cleaning of all intraoral soft tissue with antiseptic 5% Betadine® solution, the surgical part of the treatment (including extractions) was performed in local anesthesia (Ultracaine® D-S Forte) [Figures 2a, b, and Figure 3]. The teeth 11–19 were removed, and after the extractions, the maxillary sinus was wide open from the tuberosity to the area of the removed tooth 12 with a fully ruptured schneiderian membrane. A direct communication between the oral cavity and the maxillary sinus, which was over 4 cm long and approximately 2 cm wide, had occurred. The teeth had been surrounded only by a thin and splintering bone layer, which was automatically removed with the teeth. In addition, multiple small parts of the palatal process of the maxilla splintered off during the extraction procedure and had to be removed. Before suturing, under the direct access to the caudal stump of the zygomatic bone, the implant bed was prepared with the use of a 2.0 mm drill (30 mm long) mounted on a straight handpiece. Immediately after that, a BCS® (5.5 mmd × 20 mml) implant (Ihde Dental, Germany) was placed into the end of the stump using a handgrip with an adapter insertion tool. A second implant was positioned into the fusion area between the pterygoid plate of the sphenoid bone and the maxillary tuberosity. The cortical floor of the nose was used for the anchorage of the third (anterior) implant. Due to the second and third cortical anchorage achieved with all three implants, we managed to obtain very high primary stability. The soft tissues were sutured with monofilament Silk 3.0. Even though the full closure of the flap was achieved, the suture line was not supported by bone; and hence, the stability of the suturing was at risk from the very beginning. The impression was taken immediately after finishing the surgical part with a silicone following one step, closed tray technique, using transfers which belong to the BCS® system. The three implants were splinted with a fixed, cemented bar on the day of surgery with the use of Fuji IX® cement as shown in Figure 4.
Figure 2.
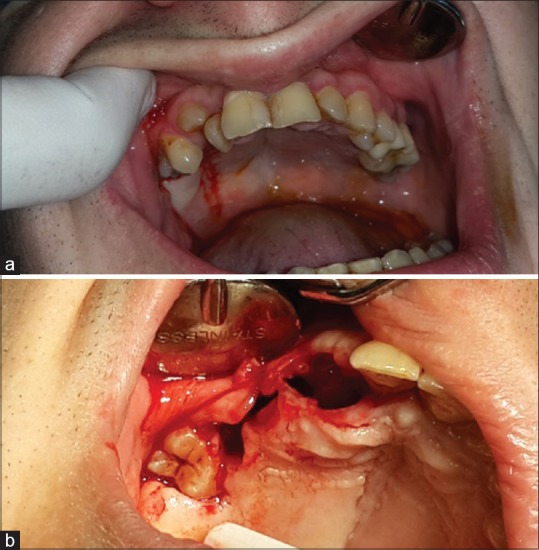
(a) Clinical view on the dentition of the upper jaw before the intervention. The teeth are well in function from 11 to 27. All other upper teeth were in infraocclusion. The molars were hardly erupted and are therefore not visible here. (b) An intraoral clinical picture taken during the first treatment phase. During the extraction not only the teeth came out, but also the minimal rests of cortical bone surrounding them resulting in a large communication between the oral cavity and the maxillary sinus. The bone was partly missing up to the median raphe of the maxilla of the right side
Figure 3.

All teeth in the upper-right jaw were extracted, from 11 to 19(!). It was decided that also the upper right central had to be removed, to make space for a stable, cortically anchored Strategic Implant®. This was necessary to set up a wide supporting polygon with masticatory surfaces in its center
Figure 4.

A clinical picture after wound closure and immediate splinting of the three implants with a casted bar made from CoCrMo. This first construction (without the possibility of masticatory function) was left in place until we were able to place the 4th implant
A full, pressure-proof closure of the maxillary sinus toward the oral cavity was not achieved at the beginning. As BCS® implants have a polished surface and are designed, especially for sinus or transsinus placement; there was no danger of inflammation.
The patient was requested to take a computed tomography (CT) picture to search for other available bone locations, where more implants could be placed [Figure 5]. The CT revealed that one more tubero-pterygoid implant could be positioned anteriorly to the one which had been placed during the first intervention. This was done 4 months later to allow integration of the first three implants [Figure 6].
Figure 5.
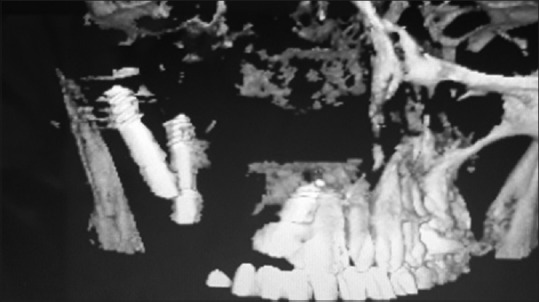
The patient was sent to CT to determine the position of the 1st three implants placed and to search for more bone and determine the spatial relationship between the bone and the implants which were already placed
Figure 6.

Panoramic overview picture after placement of the 4th implant (the 2nd implant in the tubero-pterygoid region)
According to the findings in the postoperative CT, the implant in area 11 seemed not 100% integrated, so we exchanged it with a wider diameter (BCS = 5.5 mmd) implant. All implants were then loaded following the immediate loading protocol with a new prosthetic construction, that is, a first long-term temporary bridge fabricated from CoCrMo with a composite veneering.
RESULTS
The initial treatment phase resulted in an implant borne bridge restoration with masticatory surfaces from tooth 11 to tooth 14, on a fixed, cemented restoration as shown in Figures 7–9.
Figure 7.

Panoramic overview of the first prosthetic construction which allowed real masticatory function on the right side, but with reduced length of the chewing table
Figure 9.

An overview on the first fixed, cemented reconstruction. All occlusal contacts are within the supporting polygon marked by two tubero-pterygoid screw implants, one implant in the caudal stump of the zygomatic bone, and one implant in the area of the right upper central with anchorage in the cortical floor of the nose.
Figure 8.

For several months, the patient had to accept a small but disturbing oroantral communication. After three unsuccessful attempts to close the tissue surgically, the condition suddenly healed without any surgery. We observed that the position of the communication gradually moved distally by itself before it finally closed
The treatment plan to follow includes the incorporation of more masticatory surfaces in the upper jaw and replacement of the missing teeth in the lower jaw. At the time point, when this report has been written, the reconstruction in the upper jaw was incorporated uneventfully and stable for ≥2 years, and the oroantral communication remains closed.
DISCUSSION
The conventional approach in this situation would include a multistep surgical protocol with the extraction of all the teeth in the upper jaw, possibly vascularized bone block transplantation and subsequent treatment with endosseous two-stage implants and fixed prosthodontics.[21,22] Due to the severe lack of natural bone (as a foundation for the bone block), this treatment plan seemed extremely uncertain, in fact, an “onlay bone graft” was not possible, because there was no bone up to the median raphe of the right maxilla. In case of failure, a large communication between the oral cavity and the maxillary sinus would appear, and further treatment would quite probably include the incorporation of a removable, soft-tissue borne obturator prosthesis.[23] The goal of any maxillary reconstruction is to avoid oroantral communication.[24] When weighing up pros and cons of a treatment, we had to take into consideration the patient's quality of life, and it was clear that it would have been better to leave him untreated than provide him with a treatment that would leave an oroantral communication and a soft-tissue obturator prosthesis.[25] Therefore, he was offered a treatment with the Strategic Implant® in an immediate load protocol after extraction of all the teeth in the upper right maxilla, but he was also duly warned of the life-long burdens of an obturator prosthesis in case of failure.
In the given preoperative situation also, the option of not treating had to be carefully evaluated. Providing treatment seems only advisable if the patient really urges the treatment provider to perform it and if he is really willing to accept the worst case outcome, i.e., an obturator prosthesis. Our patient was bothered not only by his strongly reduced ability to chew but also by the esthetics. He really sought the solution. We were in a really difficult situation, as we were sure that we could not describe realistically what life with an obturator prosthesis would look like compared to the given situation.[25,26]
The present case seemed perfect for an implant borne reconstruction in an immediate load protocol, because we were able to set up a large supporting polygon and position all masticatory contacts well within that polygon, but in order to set it up, we had to decide for the additional extraction of the only healthy tooth in the right half of the maxilla – the central incisor. Once the decision for implant treatment was taken, there was the urgent need of cortical, osseointegrated anterior support, and no other choice was left.[27,28]
CONCLUSION
The use of cortically anchored Strategic Implant® allowed for the fixed reconstruction of a severe defect after removing all the teeth in the right maxilla and closing a large oroantral communication. This treatment was sufficient to restore masticatory function to some extent, and it has improved the quality of patient's life regarding both function and the esthetics. Before full restoration of the masticatory function can take place, also more (implant borne) teeth in the lower jaw are required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Wolff J. The Law of Bone Remodelling. In: Maquet P, Furlong R, translators. Verlag Von August Hirshwald. Verlag: Springer; 1892. [Google Scholar]
- 2.Frost HM. Wolff's law and bone's structural adaptations to mechanical usage: An overview for clinicians. Angle Orthod. 1994;64:175–88. doi: 10.1043/0003-3219(1994)064<0175:WLABSA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Hanau RL. Articulation defined, analyzed and formulated. J Am Dent Assoc. 1926;13:1694–709. [Google Scholar]
- 4.Planas P. Equilibrium and neuro-occlusal rehabilitation. Orthod Fr. 1992;63(Pt 2):435–41. [PubMed] [Google Scholar]
- 5.Dickerson WG, Chan CA, Carlson J. The human stomatognathic system: A scientific approach to occlusion. Dent Today. 2001;20:100. [PubMed] [Google Scholar]
- 6.Maki K, Miller AJ, Okano T, Hatcher D, Yamaguchi T, Kobayashi H, et al. Cortical bone mineral density in asymmetrical mandibles: A three-dimensional quantitative computed tomography study. Eur J Orthod. 2001;23:217–32. doi: 10.1093/ejo/23.3.217. [DOI] [PubMed] [Google Scholar]
- 7.Šidlauskienė M, Smailienė D, Lopatienė K, Čekanauskas E, Pribuišienė R, Šidlauskas M. Relationships between malocclusion, body posture, and nasopharyngeal pathology in pre-orthodontic children. Med Sci Monit. 2015;21:1765–73. doi: 10.12659/MSM.893395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cuccia A, Caradonna C. The relationship between the stomatognathic system and body posture. Clinics (Sao Paulo) 2009;64:61–6. doi: 10.1590/S1807-59322009000100011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greenberg A, Prein J. Craniomaxillofacial Reconstructive and Corrective Bone Surgery. New York: Springer-Verlag; 2002. [Google Scholar]
- 10.Stewart MG. Head, Face, and Neck Trauma: Comprehensive Management. New York: Thieme; 2005. [Google Scholar]
- 11.Barnes L, Eveson JW, Reichart P, Sidransky D. WHO Classification of Tumours Series. Pathology and Genetics of Head and Neck Tumours. Lyon: IARC Press; 2005. [Google Scholar]
- 12.Kondo A, Kurose M, Obata K, Yamamoto K, Murayama K, Shirasaki H, et al. A clinical study of maxillary sinus squamous cell carcinoma. Adv Otorhinolaryngol. 2016;77:83–7. doi: 10.1159/000441879. [DOI] [PubMed] [Google Scholar]
- 13.Zhang L, Ding Q, Liu C, Sun Y, Xie Q, Zhou Y, et al. Survival, function, and complications of oral implants placed in bone flaps in jaw rehabilitation: A systematic review. Int J Prosthodont. 2016;29:115–25. doi: 10.11607/ijp.4402. [DOI] [PubMed] [Google Scholar]
- 14.Leblebicioglu B, Rawal S, Mariotti A. A review of the functional and esthetic requirements for dental implants. J Am Dent Assoc. 2007;138:321–9. doi: 10.14219/jada.archive.2007.0164. [DOI] [PubMed] [Google Scholar]
- 15.Oh WS, Roumanas E, Beumer J., 3rd Maxillofacial restoration after head and neck tumor therapy. Compend Contin Educ Dent. 2007;28:70–6. [PubMed] [Google Scholar]
- 16.Baj A, Trapella G, Lauritano D, Candotto V, Mancini GE, Giannì AB, et al. An overview on bone reconstruction of atrophic maxilla: Success parameters and critical issues. J Biol Regul Homeost Agents. 2016;30:209–15. [PubMed] [Google Scholar]
- 17.Aghaloo TL, Moy PK. Which hard tissue augmentation techniques are the most successful in furnishing bony support for implant placement. Int J Oral Maxillofac Implants. 2007;227:49–70. [PubMed] [Google Scholar]
- 18.Singh K, Singh SV, Mishra N, Agrawal KK. Management of maxillectomy defect with a hybrid hollow bulb obturator. BMJ Case Rep 2013. 2013:pii: bcr2012007658. doi: 10.1136/bcr-2012-007658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dholam KP, Bachher GK, Yadav PS, Quazi GA, Pusalkar HA. Assessment of quality of life after implant-retained prosthetically reconstructed maxillae and mandibles postcancer treatments. Implant Dent. 2011;20:85–94. doi: 10.1097/ID.0b013e31820031ab. [DOI] [PubMed] [Google Scholar]
- 20.Chigurupati R, Aloor N, Salas R, Schmidt BL. Quality of life after maxillectomy and prosthetic obturator rehabilitation. J Oral Maxillofac Surg. 2013;71:1471–8. doi: 10.1016/j.joms.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 21.Cha HS, Kim JW, Hwang JH, Ahn KM. Frequency of bone graft in implant surgery. Maxillofac Plast Reconstr Surg. 2016;38:19. doi: 10.1186/s40902-016-0064-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ribeiro Filho SA, Francischone CE, de Oliveira JC, Ribeiro LZ, do Prado FZ, Sotto-Maior BS, et al. Bone augmentation of the atrophic anterior maxilla for dental implants using rhBMP-2 and titanium mesh: Histological and tomographic analysis. Int J Oral Maxillofac Surg. 2015;44:1492–8. doi: 10.1016/j.ijom.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 23.Ali A, Fardy MJ, Patton DW. Maxillectomy – To reconstruct or obturate? Results of a UK survey of oral and maxillofacial surgeons. Br J Oral Maxillofac Surg. 1995;33:207–10. doi: 10.1016/0266-4356(95)90001-2. [DOI] [PubMed] [Google Scholar]
- 24.Okay DJ, Genden E, Buchbinder D, Urken M. Prosthodontic guidelines for surgical reconstruction of the maxilla: A classification system of defects. J Prosthet Dent. 2001;86:352–63. doi: 10.1067/mpr.2001.119524. [DOI] [PubMed] [Google Scholar]
- 25.Andrades P, Militsakh O, Hanasono MM, Rieger J, Rosenthal EL. Current strategies in reconstruction of maxillectomy defects. Arch Otolaryngol Head Neck Surg. 2011;137:806–12. doi: 10.1001/archoto.2011.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Murphy J, Isaiah A, Wolf JS, Lubek JE. Quality of life factors and survival after total or extended maxillectomy for sinonasal malignancies. J Oral Maxillofac Surg. 2015;73:759–63. doi: 10.1016/j.joms.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 27.Kornblith AB, Zlotolow IM, Gooen J, Huryn JM, Lerner T, Strong EW, et al. Quality of life of maxillectomy patients using an obturator prosthesis. Head Neck. 1996;18:323–34. doi: 10.1002/(SICI)1097-0347(199607/08)18:4<323::AID-HED3>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 28.Ihde S, Ihde A, Lysenko V, Konstantinovic V, Palka L. New systematic Terminolog of cortical bone areals for osseo-fixated implants in strategic oral implantology. J Anat. 2016;1:7. [Google Scholar]


