Abstract
Aim and Objectives:
The aim and objectives of this study are to investigate the various types of stress-inducing factors, most prevalent etiological factor and to determine the correlation between stress and temporomandibular disorders (TMDs) in Dental students in Modinagar, Ghaziabad, Uttar Pradesh.
Materials and Methods:
A sample of 450 students were selected for the study divided into two groups of undergraduate (UG) and postgraduate (PG) students further subdivided into UG (1st, 2nd, 3rd, and 4th, interns) and PG (1st, 2nd, 3rd year). Study includes clinical evaluation of temporomandibular joint (TMJ) system (TMJ sounds, muscles of mastications, mouth opening, and range of mandibular motion) and questionnaire which covers demographic data (i.e., age, sex, and academic year), TMD symptoms and TMD signs along with standardized scales related to stress dental environmental stress scale and perceived stress scale (PSS).
Results:
Most of the students included into study are mostly of 21–25 years of age (64.3%), males (52.7%), females 47.3% with more number of UGs (91.4%) predominantly 1st year students (23.9%). Headache was found to be the most prevalent TMD symptom (26.2%) followed by clicking (24.9%), pain on clicking (5.5%), jaw lock (3.4), and difficulty in mouth opening (0.9%). Clicking was found to be the most prevalent TMD sign (24.9%) among dental students followed by deviation (16.3%), muscle tenderness (14.3%), and TMJ pain (5.7%). The most prevalent TMD was disc displacement 22.6% followed by myofascial pain dysfunction syndrome (MPDS) with disc displacement (13.5%) and MPDS (3.8%). TMD was higher in UG females students of 21–-25 years of age group, dental environment stress scale score and PSS score shows statistically significant results.
Conclusion:
Stress is a significant etiologic factor involved in initiation and maintenance of TMDs in Dental students.
Keywords: Dental environment stress scale, disc displacement, perceived stress scale, stress, temporomandibular disorders
INTRODUCTION
The temporomandibular joint (TMJ) is synovial compound joint of an ellipsoid variety consisting of the bilateral articulation with condyles of the mandible with the glenoid fossa of the inferior border of the temporal bone, separated by the meniscus or interarticular disc.[1] Thus the TMJ is anatomically made up of two bones but functionally, the articular disc serves as third nonossified component that regulates the complex movements of the joint. Temporomandibular system mainly comprise of two components, the TMJ and the associated neuromuscular system. Any condition that prevents this complex system of muscles, bones and joints from synchronous/harmony working may progress to temporomandibular disorder (TMD). The TMJ and the stomatognathic system are affected by a large variety of pathological conditions with different prognosis.[2,3] TMJ disorders (TMD) are the group of disorders which affects the TMJ, the jaw muscles, or both. Clinically, it presents as pain and tenderness in the masticatory muscles or TMJ, clicking or crepitation of the TMJ during condylar movement, and limitation on mandibular movement (restriction, deviation, or deflection). Involvement of the face, head, or jaw is quite often.[4,5] In TMD, the synovial joint capsule and surrounding musculature are highly vascularized, innervated and are thought to be most common location of pain in TMJ disorders. Symptoms can range from barely noticeable to seriously debilitating. TMJ disorders are very common nowadays and is thought to be self-limiting condition.[6,7]
The exact cause of TMDs is not known but is thought to be multifactorial.[8] Different etiological factors of TMD documented in medical literature are Psychological factors such as personality and behavior, occlusal discrepancies, improper dental treatment, joint laxity, continuous micro trauma to joint, overloading/overusing joint structures, and parafunctional habits. Stress, behavioral, social, and emotional conditions are also considered. Among different etiological factors of TMD, psychosocial factors are most commonly related to TMD patients. Dental school is a highly pressurized, difficult environment for students and has been widely acknowledged as being associated with high levels of stress. Dentistry has grown into a highly demanding and competitive profession. Dental students have to take thorough theoretical knowledge, tough clinical work, and interpersonal skills. 50%–75% of TMJ patients undergone stressful life conditions before the development of TMD symptoms.[9,10]
Keeping all this in mind, a study was designed to investigate the perceived sources of stress, to identify the sources of stress among dental students in D. J Dental College Modinagar, Ghaziabad, Uttar Pradesh, India, to investigate the stress as etiology of TMD. Stress related to year of study or gender and to determine the major source of stress among dental students and to ascertain whether the major stressors varied during the undergraduate (UG) and postgraduate (PG) course and to assess the prevalence of TMJ disorders of dental students and the relation between TMJ disorder syndrome and the emotional condition of the patient.
MATERIALS AND METHODS
A sample of 450 students of D. J. College of Dental Science and Research were selected for the study. Their age ranged from 17 to 32 years. Students were divided into two groups: UG students and PG students. These groups were further divided into subgroups according to their academic years: UG (1st, 2nd, 3rd, and 4th, interns) and PG (1st, 2nd, and 3rd year). Students with permanent dentition stage are included into study. Patients with craniofacial anomalies, history of orthodontic treatment, trauma, and surgery of TMJ were excluded from study. Study includes clinical evaluation of TMJ system and questionnaire. TMJ evaluation includes the examination of TMJ sounds [Figure 1], Muscles of mastication [Figure 2], mouth opening [Figure 3], and range of mandibular motion [Figure 4].
Figure 1.

Examination of temporomandibular joint sounds
Figure 2.

Examination of muscles of mastication
Figure 3.
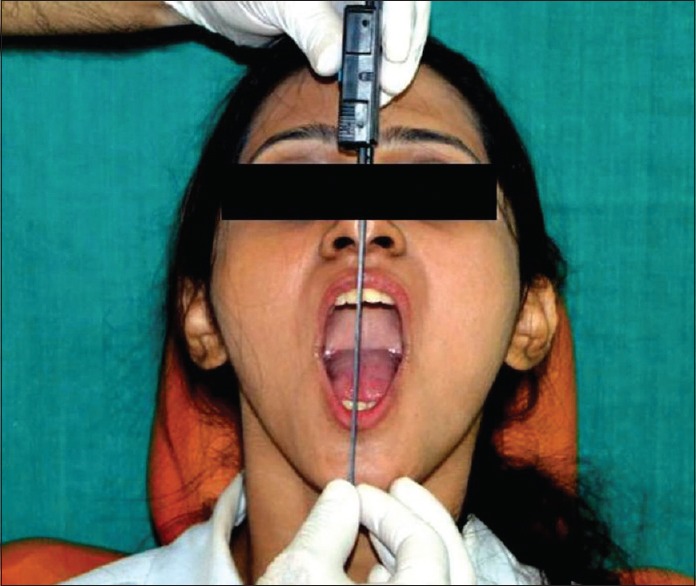
Examination of mouth opening
Figure 4.

Examination of range of mandibular motion
The pretested questionnaire comprised two sections, first part covered the demographic data (i.e., age, sex, and academic year), TMD symptoms, and TMD signs whereas the second part included the standardized scales related to stress dental environmental stress scale (DESS) and perceived stress scale (PSS). The presence of signs and symptoms of TMD was determined using a self-administered modified questionnaire composed of 5 questions regarding common TMD symptoms and 5 questions regarding TMD signs. The PSS comprises of 10 questions. Questions are designed to tap how unpredictable, uncontrollable, and overloaded respondents find their lives.
The questions in the PSS ask about feelings and thoughts during the last month. In each case, respondents are asked how often they felt a certain way. PSS scores are obtained using Likert scale. (0 = never, 1 = almost never, 2 = sometimes, 3 = fairly often, and 4 = very often). Responses are to be reversed (e.g., 0 = 4, 1 = 3, 2 = 2, 3 = 1, and 4 = 0) to the four positively stated items (items 4, 5, 7, and 8) and then summing across all scale items. To assess the sources of stress in dental students, a modified version of the dental environmental stress questionnaire. For clarity of presentation and for the purposes of establishing a theoretical framework for the investigation of the research questions, these items were also grouped into 5 stressor domains: Living accommodation (1–4), personal factors (5–17), education environment (18–22), academic work (23–30), and clinical factor (31–39).
Scores for clinical factors were only computed for the clinical students (3rd year onward) students were clinically examined after filling the questionnaire. The responses to the questionnaire were based on a four-point Likert scale with response options of 1 = not stressful, 2 = slightly stressful, 3 = moderately stressful, and 4 = severely stressful, as well as a fifth possible response of not applicable (0 = not applicable)
RESULTS
The present study evaluates the relationship between various stressful life events and temporomandibular joint disorder (TMD) among dental students. A total of 370 eligible UG and PG students of either sex were selected. The age of all students ranged from 17 to 32 years with mean (±standard deviation) 22.28 ± 2.49 years and median 22 years. The students of our study were mostly of 21–25 years of age (64.3%) predominantly males (52.7%), and females 47.3% with more number of UGs (91.4%) predominantly 1st year students (23.9%) [Graph 1 and Table 1].
Graph 1.
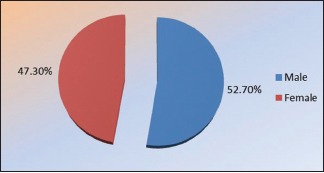
Gender distribution of study subjects
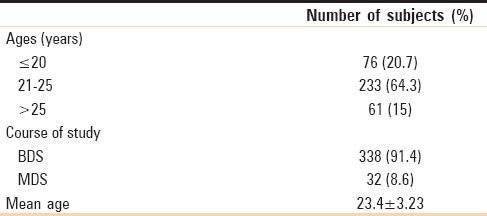
Table 1.
Age-wise and academic course-wise distribution of subjects
Temporomandibular disorder symptoms
Among dental students, headache was found to be the most prevalent TMD symptom (26.2%) followed by clicking (24.9%), pain on clicking (5.5%), jaw lock (3.4), and difficulty in mouth opening (0.9%) [Graph 2].
Graph 2.
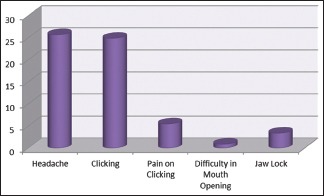
Temporomandibular disorder symptoms in study subjects
Temporomandibular disorder signs
The frequency distribution of TMD signs among dental students shows clicking was found to be the most prevalent TMD sign (24.9%) among dental students followed by deviation (16.3%), muscle tenderness (14.3%), and TMJ pain (5.7%) [Graph 3].
Graph 3.
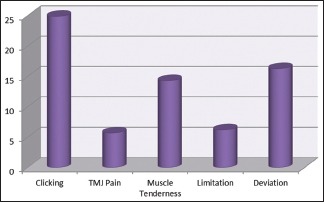
Temporomandibular disorder signs in study subjects
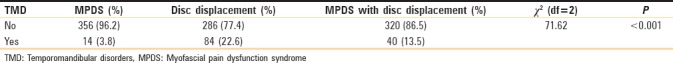
The TMD prevalent in dental students shows the most prevalent TMD was disc displacement 22.6% followed by myofascial pain dysfunction syndrome (MPDS) with disc displacement (13.5%) and MPDS (3.8%) in dental students [Table 2].
Table 2.
Frequency distribution of temporomandibular disorders among dental students
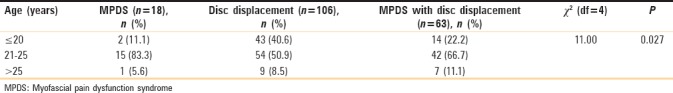
Among dental students, the TMDs were found to be most prevalent in 21–25 years of age group with predominance of MPDS (83.3%). Comparing the TMDs between different age groups, χ2 test revealed significant (P > 0.05) difference between the groups and higher prevalence of TMD disorders was found among 21–25 years of age group as compared to both ≤20 years and >25 years(χ2= 11.00, P = 0.027) [Table 3].
Table 3.
Age-wise distribution of temporomandibular disorders among dental students
Among dental students, the prevalence of TMDs was found to be higher in females than males with highest frequency of disc displacement in females (66.0%). However, the TMDs did not differed (P > 0.05) between the two genders (χ2= 0.61, P = 0.736) i.e., found to be statistically the same [Graph 4].
Graph 4.
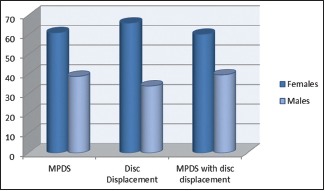
Gender distribution of temporomandibular disorders among dental students
Among dental students, the prevalence of TMD disorders was comparatively higher in UG students than in PG students with the highest frequency of MPDS with disc displacement in UG (95.2%) and disc displacement in PG (11.3%) students. However, the TMD disorders did not differed (P > 0.05) between the two academics (χ2= 2.40, P = 0.301) i.e., found to be statistically similar [Graph 5].
Graph 5.
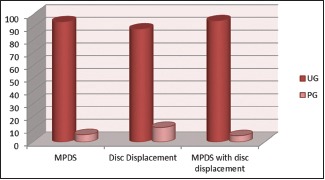
Academic course-wise distribution of temporomandibular disorders among dental students
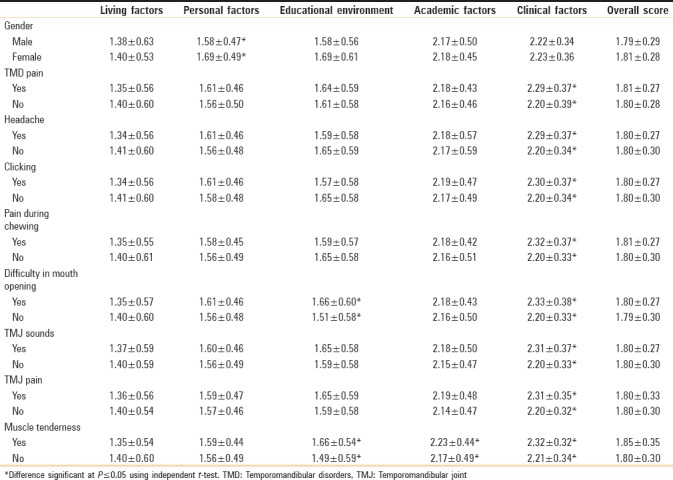
Dental environment stress scale
Result of questionnaire in DESS shows statistically significant result in both males and females in personal factors. Among clinical factors TMD pain, headache, clicking sound in TMJ, Pain during chewing, difficulty in mouth opening, TMJ sounds, TMJ pain and muscle tenderness shows statistically significant results. There is statistically significant result of difficulty in mouth opening and muscle tenderness in education environment. In addition, significant results of muscle tenderness in academic factors [Table 4].
Table 4.
Dental environment stress score based on different temporomandibular joint symptoms
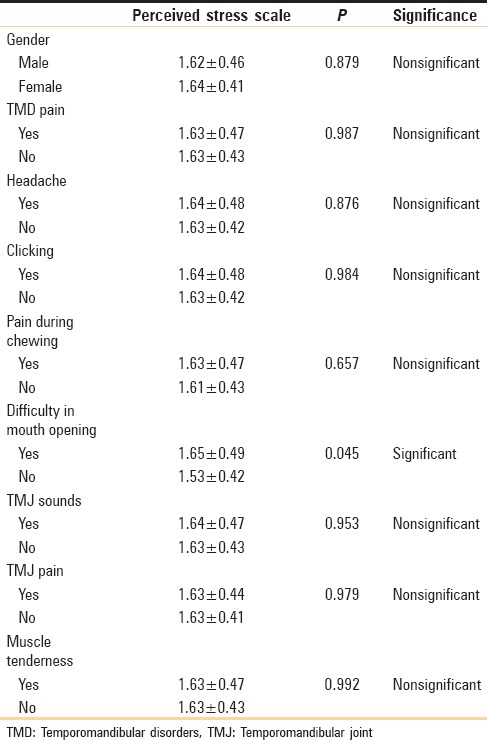
PSS score according to TMD symptoms shows statistically significant results in difficulty in mouth opening only [Table 5].
Table 5.
Perceived stress score according to temporomandibular disorders symptoms
DISCUSSION
Temporomandibular disorders (TMJ disorders), TMJ dysfunction, and TMJ syndrome are the common synonyms associated with problems of the jaw, TMJ itself, and surrounding facial muscles. It is commonly occurs in 2nd to 4th decade with female predominance. Clinical features of TMJ disorders are clicking, poping, or grating sounds, tenderness of TM joint, reduced mouth opening, stiff or tender neck and shoulders region, pain in ears and preauricular region while opening/closing jaw or chewing. Other symptoms include tired face, difficulty in chewing, swelling on the side of the face, toothache, headache, dizziness, hearing problems, and ringing in the ears (tinnitus).
The exact cause of TMJ disorders is not clear and is thought to be multifactorial. Among all of the factors that have been studied as potential causes for TMD, behavioral and psychologic factors are believed to be one of the most significant etiologies. Stress related with dentistry is time and scheduling pressures (study, clinical, and laboratory works), management of uncooperative patients in clinics, and the highly technique sensitive/intensive nature of work. The resulting stress can lead to depression, anxiety, and reduce efficacy. The aim of present study is to identify the probable sources of stress among dental students DJ Dental College, Modinagar, Ghaziabad, India, to investigate whether specific stressor was related to age, gender, or year of study and to further evaluate the relationship various stressful life events and TMDs among dental students.
In the present study, TMJ pain the most prevalent TMD symptom (26.2%) followed by headache (25.7%) pain on chewing (23.2%), lock jaw (3.4%), and difficulty in opening (6.2%) and clicking was also the most prevalent TMD sign (31.2%) noted in our sample followed by deviation (16.3%), muscle tenderness (14.3%), between TMJ pain (5.7%) and limitation (6.2%) which is in accordance to the study by Feteih[11] wherein the prevalence of Joint sounds were the most prevalent sign (13.5%) followed by restricted opening (6.2%) and opening deviation (16.9%). Basafa and Shahabee[12] and Miyake et al.[13] in their study have shown that joint noises were the predominant sign and symptom.
In dental students, among the three groups, the most prevalent TMD was disc displacement (22.6%) followed by MPDS with disc displacement (13.5%) and MPDS (3.8%). This was contrary to the statement by LeResche[14] wherein the most common subtypes of TMDs in clinic populations appear to be myofascial pain and arthralgia, followed by disc displacements with reduction.
The prevalence of TMDs was found to be higher among females than males with highest frequency of Disc displacement in Females (66.0%) in dental students. This observation is in line with the study done by Basafa and Shahabee[12] wherein women were found to be more prone to TMDs than men (1.6:1). A strong female preponderance (9:1) observed by Milam[4] and by Manfredini et al.[15] where in the reported females:males ratio is about 3–4:1 and by Bonjardim et al.[16] which showed that the percentage of women (57.43%) with TMD is higher than that of men (42.11%). However, these are in contrast to the findings reported by Acharya[10] wherein overall, males perceived more stress than female students.
Twenty-one–25 years of age group was most common one with the prevalence of TMDs with predominance of MPDS (83.3%) among dental students. This is in accordance with the article by Manfredini et al.[15] with a peak in the age range between 20 and 40 years and a lower prevalence in the young and the old people. Maydana et al.[17] illustrated typically limiting nature of the symptoms and deduced that most cases occurs in young adults aged between 20 and 40 years.
TMD disorders were found to have comparatively higher prevalence in UG students than PG students with highest frequency of MPDS with disc displacement in UG (95.2%) and disc displacement in PG (11.3%) students. However, the TMD disorders did not differed (P > 0.05) between the two groups (P = 0.301), i.e., found to be statistically similar. This has not been observed in any other study and literature is not available regarding the prevalence of TMD among UG and postgraduate dental students.
The stress levels (PSS and DESS) were found to be higher in Females than Males except in DESS domains like personal factors and clinical factors. However, the gender difference was not statistically significant. This is also seen in study conducted by Yamaguchi et al.[18] wherein the female TMD patients showed a higher degree of stress. This is in contrast to the study by Naidu et al.[19] wherein female students are found to be more stressful for the domains of Academic work and Clinical factors whereas in our study, the clinical factor domains are more stressful in males.
The stress levels were found to be highest in >25 years age group specially in domains such as personal factors and clinical factors. However, the age difference was not statistically significant. This is due thought that student phase is most critical phase in life. Further, future career decisions, financial stability, social responsibilities, and family pressure are running back of the minds. Hence, this age group is quiet prone to stress, anxiety, and depression. Literature regarding stress in dental students in different age groups cannot be found.
In the present study, the stress levels (PSS and DESS) were found to be higher in Postgraduate students than UG students with higher level of stress regarding personal factors and clinical factors in PG students as compared to UG students. This can be attributed to the fact postgraduate students are burdened with academic load (dissertations work, preclinical exercises, and clinical work). Lack of time for relaxation, uncertainty about dental career, difficulty of coursework, criticism about academic or clinical work, expectation versus reality of dental school, financial responsibilities etc., are source of stress all through the tenure of the course. We have searched but did not find any relevant literature comparing the stress level among postgraduate students and UG students.
Stress regarding Living Accommodation was found to be highest in MDS 1st year followed by MDS 3rd year and BDS 2nd year. This may be attributed to the fact that students are exposed to a new stressful environment in initial years of UG and postgraduate courses and the increasing load will make it difficult for them to accommodate and adjust to the hostel atmosphere. No study has been reported regarding stress among academic years related to living accommodation yet.
Stress regarding personal factors was found to be highest in MDS 2nd year followed by MDS 1st year and BDS 4th year. Stress among BDS 4th year may be due to lack of time for relaxation due to extensive academic, preclinical, and clinical work. This is in line with the study by Kumar et al.[20]
Stress regarding Educational Environment was found to be highest in MDS 3rd year followed by MDS 2nd year and BDS 2nd year. Stress regarding educational environment such as stress because of expectation versus reality of dental school was found to be more in MDS 3rd year, MDS 2nd year in Postgraduates and BDS 2nd year students in UG students. This may be due to heavy work in second year with academic, preclinical work and fear of entering clinic. This is in line with the study by Kumar et al.[20] according to which the educational environment associated stress was more in BDS 2nd year students in UGs.
Stress regarding academic work was found to be highest in BDS 2nd year followed by BDS I year and MDS 2nd year This may be due to the sudden change in curriculum and subject, which the new students find difficult to cope with initially and due to problem-based learning in the second year produces considerable stress and contact with clinical faculty during preclinical laboratory perhaps increase their perceived stress. Similar findings were noted by Kumar et al.[20] where in stress related to academic work is found to be more in BDS 2nd year students than other academic years. However, these are in contrast to the findings reported by Acharya,[10] who studied that stress due to academic factors was found to be high in the first year, then decreased in the second year. Naidu et al.[19] revealed that for the educational stress, the 2nd year students have significantly less stress than other academic years.
Stress regarding clinical factors was found to be highest in MDS 2nd year followed by MDS 3rd year and BDS 4th year. The increase in stress level related to clinical problems in the BDS final year student might be due differences in opinion between clinical staff concerning patient's treatment and shortage of allocated clinical time and due to criticism by staff. This increase in stress was due to that students were required to complete clinical patient quotas in order to be eligible to appear for the final examinations. This was also seen in study by Kumar et al.[20] and Acharya.[10]
The present study showed that individuals with TMDs (Group I-MPDS, Group II-disc displacement, and Group III-MPDS with disc displacement) are found to be significantly (P > 0.05) associated with higher level of stress (PSS) as compared to subjects without TMD (18.93 ± 6.01 vs. 20.28 ± 5.38, t = 2.49; P = 0.301). According to the psychological theory, the emotional disturbances results in muscular hyperactivity. Muscle hyperactivity is mediated by the extrapyramidal gamma-motoric system, which is closely linked to the limbic system and thus very susceptible to emotional influences. With sustained muscular hyperactivity, pain develops as a consequence of local ischemic hypoxia due to accumulation of lactic acid. Bonjardim et al.[16] studied that anxiety plays an important role in TMD. Anxiety acts as a predisposing or aggravating factor and has a significant relationship with stress and degree of TMD. Liao et al.[21] wherein it was derived that the incidence of TMD was 2.65 times higher in the depression cohort than in the nondepression cohort.
Although the etiology of TMD has not been established, psychological factors have been implicated in the predisposition, initiation, and perpetuation of TMD. The overall value of this kind of research is to identify the sources of dental student stress and relationship among stress levels and TMDs which may shed more light on diagnostic and therapeutic aspects of TMDs.
CONCLUSION
The conclusion drawn from the findings of this study clearly indicates stress to be significantly involved in initiation and maintenance of TMDs and in dental students there are some factors predominantly leading to stressful situations exposing them to TMDs. These derivations will be of great help in diagnosing this complicated group of diseases (TMDs). Main limitation of the study is small sample size and further studies with larger sample size are required to validate the prevalence of TMDs in dental students and their association with stress.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Baskan S, Zengingul A. Temporomandibular joint, disorders and approaches. Biotechnol Biotechnol. 2006;20:151–5. [Google Scholar]
- 2.Jerjes W, Upile T, Abbas S, Kafas P, Vourvachis M, Rob J, et al. Muscle disorders and dentition-related aspects in temporomandibular disorders: Controversies in the most commonly used treatment modalities. Int Arch Med. 2008;1:23. doi: 10.1186/1755-7682-1-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhat S. Etiology of temporomandibular disorders: The journey so far. Int Dent SA. 2010;12:88–99. [Google Scholar]
- 4.Milam SB. Pathophysiology and epidemiology of TMJ. J Musculoskelet Neuronal Interact. 2003;3:382–90. [PubMed] [Google Scholar]
- 5.Poveda Roda R, Bagan JV, Díaz Fernández JM, Hernández Bazán S, Jiménez Soriano Y. Review of temporomandibular joint pathology. Part I: Classification, epidemiology and risk factors. Med Oral Patol Oral Cir Bucal. 2007;12:E292–8. [PubMed] [Google Scholar]
- 6.Buescher JJ. Temporomandibular joint disorders. Am Fam Physician. 2007;76:1477–82. [PubMed] [Google Scholar]
- 7.Knight J. Diagnosis and treatment of temporomandibular disorders in primary care. Hosp Phys. 1999;35:55–8. [Google Scholar]
- 8.Fantoni F, Salvetti G, Manfredini D, Bosco M. Current concepts on the functional somatic syndromes and temporomandibular disorders. Stomatologija. 2007;9:3–9. [PubMed] [Google Scholar]
- 9.Prashant VK, Dodamani A. Perceived sources of stress among Indian dental students. J Indian Assoc Public Health Dent. 2012;17:171–7. [Google Scholar]
- 10.Acharya S. Factors affecting stress among Indian dental students. J Dent Educ. 2003;67:1140–8. [PubMed] [Google Scholar]
- 11.Feteih RM. Signs and symptoms of temporomandibular disorders and oral parafunctions in urban Saudi Arabian adolescents: A research report. Head Face Med. 2006;2:25. doi: 10.1186/1746-160X-2-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Basafa M, Shahabee M. Prevalence of TMJ disorders among students and it relation to malocclusion. Iran J Otorhinolaryngol. 2006;18:53–9. [Google Scholar]
- 13.Miyake R, Ohkubo R, Takehara J, Morita M. Oral parafunctions and association with symptoms of temporomandibular disorders in Japanese university students. J Oral Rehabil. 2004;31:518–23. doi: 10.1111/j.1365-2842.2004.01269.x. [DOI] [PubMed] [Google Scholar]
- 14.LeResche L. Epidemiology of temporomandibular disorders: Implications for the investigation of etiologic factors. Crit Rev Oral Biol Med. 1997;8:291–305. doi: 10.1177/10454411970080030401. [DOI] [PubMed] [Google Scholar]
- 15.Manfredini D, Guarda-Nardini L, Winocur E, Piccotti F, Ahlberg J, Lobbezoo F, et al. Research diagnostic criteria for temporomandibular disorders: A systematic review of axis I epidemiologic findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:453–62. doi: 10.1016/j.tripleo.2011.04.021. [DOI] [PubMed] [Google Scholar]
- 16.Bonjardim LR, Lopes-Filho RJ, Amado G, Albuquerque RL, Jr, Goncalves SR. Association between symptoms of temporomandibular disorders and gender, morphological occlusion, and psychological factors in a group of university students. Indian J Dent Res. 2009;20:190–4. doi: 10.4103/0970-9290.52901. [DOI] [PubMed] [Google Scholar]
- 17.Maydana AV, Tesch RS, Denardin OV, Ursi WJ, Dworkin SF. Possible etiological factors in temporomandibular disorders of articular origin with implications for diagnosis and treatment. Dent Press J Orthod. 2010;15:78–86. [Google Scholar]
- 18.Yamaguchi D, Motegi E, Nomura M, Narimiya Y, Katsumura S, Miyazaki H, et al. Evaluation of psychological factors in orthodontic patients with TMD as applied to the “TMJ scale”. Bull Tokyo Dent Coll. 2002;43:83–7. doi: 10.2209/tdcpublication.43.83. [DOI] [PubMed] [Google Scholar]
- 19.Naidu RS, Adams JS, Simeon D, Persad S. Sources of stress and psychological disturbance among dental students in the West Indies. J Dent Educ. 2002;66:1021–30. [PubMed] [Google Scholar]
- 20.Kumar P, Dodamani A, Kerudi V, Shirahatti R, Telka S. Perceived sources of stress among Indian dental students. J Indian Assoc Public Health Dent. 2011;9:171–7. [Google Scholar]
- 21.Liao CH, Chang CS, Chang SN, Lane HY, Lyu SY, Morisky DE, et al. The risk of temporomandibular disorder in patients with depression: A population-based cohort study. Community Dent Oral Epidemiol. 2011;39:525–31. doi: 10.1111/j.1600-0528.2011.00621.x. [DOI] [PubMed] [Google Scholar]


