Abstract
Aims and Objectives:
Aims and objectives of the study were to study the effectiveness of Raj-yoga meditation and pranayama in patients with myofascial pain dysfunction syndrome (MPDS) and compared the effects with ongoing conventional noninvasive treatment modalities.
Materials and Methods:
The study comprised 30 patients divided equally (10 each) into 3 group, i.e., control group (conventional, noninvasive treatment), Experimental A group (conventional, noninvasive treatment with raj-yoga meditation therapy and pranayama), and Experimental B group (Raj-yoga meditation therapy and pranayama only). Parameters such as pain, mouth opening, mandibular deviation, inflammation, swelling, clicking, occlusion, and psychologic evaluation such as anxiety, stress, and depression were assessed before the start of the study and at weekly intervals for 3 months.
Results:
Posttreatment pain and inflammation improved both in the control group and Experimental A group, but statistically it is highly significant in the Experimental A group. Furthermore, it is effective immediately as well as for a long period in Experimental A group. Improvement in mouth opening was statistically highly significant in control group but not in the experimental groups. Posttreatment anxiety and stress status was improved with statistically highly significant result in the Experimental A and B. The posttreatment depression status along with mandibular deviation, swelling, clicking, and occlusion has not improved significantly in any of the groups.
Interpretation and Conclusion:
Raj-yoga meditation and pranayama in combination with conventional, noninvasive, treatment modalities showed promising results in MPDS patients as compared to either modalities alone.
Keywords: Myofascial pain dysfunction syndrome, pranayama: Noninvasive therapy, Raj-yoga meditation, transcutaneous electric nerve stimulation
INTRODUCTION
The biomedical approach to disease focuses exclusively on pathophysiologic findings. In chronic pain, as well as in other chronic diseases, the biomedical model is too narrow to explain thoroughly the patient's presentation. The ecologic perspective, referred to as a biopsychosocial model, views pain and pain-related disability as a multifactorial process in which biological factors initiate, maintain, and modulate the transmission of pain-related information in the nervous system (nociception), psychological factors influence the perception and appraisal of pain and social factors shape pain behaviors and social roles for persons in pain. The ecologic model suggests the importance of an integrated treatment approach across biologic, behavioral, and psychosocial domains.[1] Myofascial pain dysfunction syndrome (MPDS) is a condition that can be satisfactorily explained on the basis of a biopsychosocial model. There is a whole gamut of treatment modalities for MPDS, based on the biologic model, (including nonsteroidal anti-inflammatory drugs [NSAIDs], muscle relaxants, therapeutic exercises, and physical medicine) with none of it emerging as a single wholesome therapy. These are effective in transient pain reduction but not successful in treating the patient completely. Besides, the current therapies are not without their share of side effects.
With this background, a project was designed to try to formulate a method of treatment for MPDS, on the basis of the biopsychosocial model, modifying the patient's explanatory models and at the same time being noninvasive, safe, cost effective, without any iatrogenic side effects, and that affords permanent relief to the patient. In this attempt, we explored the effectiveness of raj-yoga meditation and pranayama in patients with MPDS and compared the effects with that afforded by the ongoing conventional noninvasive treatment modalities.
MATERIALS AND METHODS
For the purpose, a study was designed, in which thirty patients were selected after thorough screening and clinical examination, regardless of age, sex, religion, socioeconomic status, etc., without any debilitating medical illness that was classical cases of MPDS having one or more of the following signs and symptoms:
Diffuse pain in the preauricular region, unilateral, dull, ache, usually constant, often more in the morning time or has a history of progression or worsening during the day and exacerbated by activities of the mandible including eating and talking
Tenderness in the involved muscle of mastication
Limitation of mandibular movements
Absence of clinical and radiographic evidence of any abnormality in the TMJ proper
The presence of joint sounds accompanied by myofascial pain and tenderness in the masticatory musculature that began before the onset of the joint noise. The patients with well-controlled systemic disease were included in the study. All patients were selected and grouped and then the study was started.[2]
From among the patients selected for the study, the total number of patients were divided into three clinical samples randomly and equally (i.e., ten patients in each group), namely the control, Experimental A and B groups. The control group patients were subjected to conventional, noninvasive treatment modalities (including nonnarcotic nonsteroidal anti-inflammatory analgesic, muscle relaxant moist heat, soft diet, rest of jaw, antianxiety agent, gentle stretching exercises [hinge type and lateral border movement exercises without protrusion], avoidance education for painful clicking, occlusal appliance therapy, vapocoolant spray or quick icing of skin, prolonged application of ice packs/heat packs, ultrasound, transcutaneous electric nerve stimulation, soft tissue mobilization, chronic pain therapy, neuropsychiatric consultation/therapy, articulation correction/occlusal rehabilitation, orthodontic consultation). Selectively depending on the requirement of the individual cases in projected order of importance whereas in Experimental A group, in addition to the treatment protocol assigned for the control group, the patients were subjected to raj-yoga meditation therapy and pranayama.
The Experimental B group, on the other hand, was subjected to raj-yoga meditation therapy and pranayama only, without subjecting the patients to any of the other conventional, noninvasive treatment modalities enlisted in the treatment module of the control patients. An expert teacher was asked to supervise the treatment module of the patients to ascertain that the treatment is being properly and regularly administered and to analyze as to what degree the patients are getting benefited from it (through the DASS scale).[3] On the other hand, feedback was taken from the patient's subjective assessment, and the observations and results were cross matched.
All the patients were assessed before the start of the study and at weekly intervals for 3 months on the basis of the following 8 criteria: Pain, mouth opening, mandibular deviation, inflammation, swelling, clicking, occlusion, and psychologic evaluation.
RESULTS
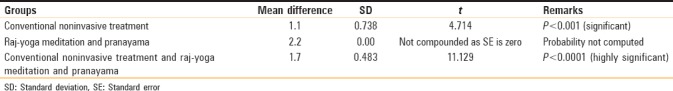
As shown in Tables 1 and 2, the posttreatment pain and inflammation status has improved both in the control and Experimental A groups, but statistically it is highly significant in the Experimental A group. This result could be attributed to the fact that the treatment given in the control group was effective, but for a short duration after which the pain reappeared though at a lower intensity as compared to the previous value, as they were not directed toward the removal of the underlying cause but interfered with the transmission of pain and gave symptomatic relief. On the other hand, the treatment offered in the Experimental A group proved to be effective immediately as well as for a long period as the conventional therapy took care of the acute stage pain and raj-yoga meditation therapy and pranayama were directed toward alleviation of the underlying predisposing stress and anxiety that resulted in prolonged relief from pain.
Table 1.
Comparison between pretreatment and posttreatment pain (n=10)
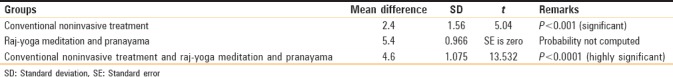
Table 2.
Comparison between pretreatment and posttreatment inflammation (n=10)
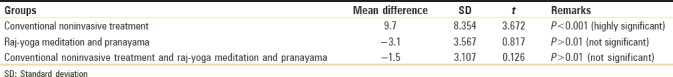
As shown in Table 3, the improvement in mouth opening was statistically highly significant in control group but not statistically significant in the experimental groups. This result could be explained on the basis of the pathogenesis of trismus that occurs in MPDS. Emotional stress results in masticatory muscle clenching, bruxing, over activity and decreased rest, resulting in spasm that leads to reduced mouth opening. In the control group, physical agents (heat, exercises, etc.) and chemical agents (muscle relaxants, NSAIDs) were used to reduce muscle spasm so mouth opening improved significantly in the control as compared to Experimental A and B groups' patients. Besides average pretreatment mouth opening was less in the control group as compared to that in the experimental groups.
Table 3.
Comparison between pre- and post-treatment mouth opening (n=10)
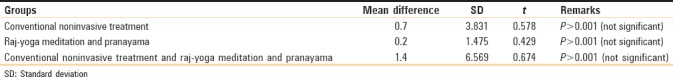
The posttreatment anxiety and stress status has improved in the experimental A and B groups, where the results are statistically highly significant [Tables 4 and 5]. The posttreatment depression status has not improved significantly in any of the groups [Table 6], as the other criteria of mandibular deviation, swelling, clicking, and occlusion.
Table 4.
Comparison between pretreatment and posttreatment anxiety (n=10)
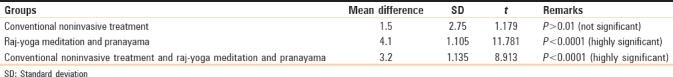
Table 5.
Comparison between pretreatment and posttreatment stress (n=10)
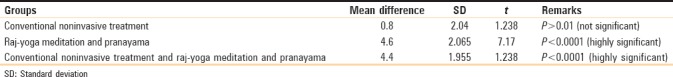
Table 6.
Comparison between pretreatment and posttreatment depression (n=10)
Our results coincide with the study conducted by Morone et al., in which they attempted to identify the effects of mindfulness meditation in older adults with chronic low back pain.
Our study is in correlation with the study of Kabat-Zinn who showed that 65% of the patients having chronic pain, not improved with conventional medical treatment, showed lesser pain after practicing mind and heartfulness meditation for 10 weeks.[4]
DISCUSSION
Yoga is a general term given for physical, mental, and spiritual practices originated early in ancient era of India with a view to gain state of permanent peace. It consists of yogic exercises related to all the parts of the body. It is composed of systematic pattern of exercises, meant to be followed regularly. Yoga consists of exercises which forms the basis of all the other forms of exercises. Pranayama means extension of breath or extension of the life force originated in the yogic desciplines of India. It is considered as “the yoga of breathe.” One can get out of stress through simple practice of yogic breathing techniques. Breathing loads your blood with oxygen which maintains your health at the most desirable level. Shallow breathing does not oxygenate your blood efficiently.
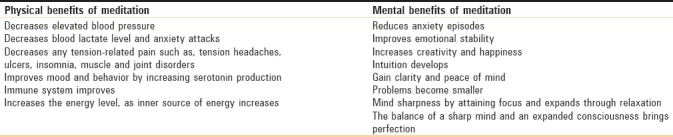
Consequently, toxins pile up in the cells before you know it, you feel sluggish and down, eventually organs begin to malfunction. One will get all benefits of pranayama through practicing different pranayama exercise [Table 7].
Table 7.
Physical and mental benefits of meditation
Kapalabhathi pranayama (cleansing breath)
Brain cells are revived, gives brightness to face, balances and strengthens the nervous system and removes drowsiness, massages the abdominal organs, benefits and cleanses respiratory tract, removes the spasm in bronchial tubes, carbon dioxide is eliminated on a large scale, purifies the blood and strengthens the heart, tones digestive system. Prepares mind for meditation.
Sectional breathing (Vibhagiya Savasana)
Corrects the breathing pattern and increases the vital capacity of lungs. Even 10 min of sectional breathing practice daily can bring more power and vitality, calmness in daily activities, clarity in thinking, calms your mind and revitalizes it.
Surya Anuloma Viloma/Chandra Anuloma Viloma pranayama
Clears the nasal passages, useful for nasal allergy and deviated nasal septum. Helps in maintaining normal weight.
Nadishuddhi pranayama/Anuloma Viloma pranayama
Balance between two nostrils, increases vitality, and increases appetite. Lowers stress and anxiety, beneficial for respiratory disorders such as nasal allergy, asthma, and bronchitis. Gives clarity to thought and leads to deep states of meditation and spiritual awakening.
Cooling pranayama – Sitali, Sitkari, Sadanta
Induces muscular relaxation and overall cooling effect. Soothens eyes, ears and purify blood, quench thirst, appease hunger, sensitizes taste buds and mouth and generate a feeling of satisfaction. Reduces tension, stress and induce mental tranquility. Sitkari and Sadanta keep the teeth and gums healthy. Reduces blood pressure and acidity in stomach, cure chronic dyspepsia, chronic skin disease, and releases subtle tensions.
Bhramari pranayama
To chant Bhramari, touch the tip of your tongue to the top of the palate. Close your ears with thumb finger and rest of your fingers on the face with eyes closed. Close your mouth and chant M-Kara, gives a humming sound of the female bee or bhramari. It creates soothing effect on the nervous system, cultures voice and increases melody. It can be practiced at any time to relieve mental tension, anger, anxiety, insomnia, increases tissue healing, decreases blood pressure, throat aliments, good for psychosomatic problems as it reduces stress and tension.
Yoga nidra
Strengthens and tones up the entire system. All muscles and joints get relaxed. It is extremely useful in managing the psychosomatic aliments such as hypertension and headaches.
Meditation and pranayama have both been found to be helpful in improving management of pain.[5,6] Meditation and pranayama techniques included in this study have increased the patients mindfulness. The patients practice yoga learned about mental focus, which in turn helps them to increase their awareness of non-optimal ways of moving and positioning their head, neck, and body. They also learn to relax tensed muscles and to relieve emotional and mental stress.[7,8]
Hurtfulness and mindfulness meditation helps in the pain reduction, improving physical function and the quality of life.[9,10]
Meditation and yoga themes help in pain reduction, improved attention and sleep and also achieving well-being. Mindfulness meditation is having promising results as a nonpharmacologic management of chronic pain for adults.[6]
CONCLUSION
Raj-yoga meditation and pranayama in combination with conventional, noninvasive, treatment modalities showed promising results in MPDS patients as compared to either modalities alone. Raj-yoga meditation and pranayama can emerge as a sole means of therapy in MPDS but needs further research based on a larger sample size and longer duration of treatment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Gatchel R, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: Scientific advances and future directions. Psychol Bull. 2007;133:581–624. doi: 10.1037/0033-2909.133.4.581. [DOI] [PubMed] [Google Scholar]
- 2.Sanford L. Block: Differential diagnosis of masticatory muscle pain and dysfunction. Oral Maxillofac Surg Clin North Am. 1995;7:29. [Google Scholar]
- 3.Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. 2nd ed. Sydney: Psychology Foundation; 1995. ISBN 7334-1423-0. [Google Scholar]
- 4.Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. Gen Hosp Psychiatry. 1982;4:33–47. doi: 10.1016/0163-8343(82)90026-3. [DOI] [PubMed] [Google Scholar]
- 5.Vallath N. Perspectives on yoga inputs in the management of chronic pain. Indian J Palliat Care. 2010;16:1–7. doi: 10.4103/0973-1075.63127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morone NE, Lynch CS, Greco CM, Tindle HA, Weiner DK. ‘I felt like a new person’ the effects of mindfulness meditation on older adults with chronic pain: Qualitative narrative analysis of diary entries. J Pain. 2008;9:841–8. doi: 10.1016/j.jpain.2008.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mehling WE, Hamel KA, Acree M, Byl N, Hecht FM. Randomized, controlled trial of breath therapy for patients with chronic low-back pain. Altern Ther Health Med. 2005;11:44–52. [PubMed] [Google Scholar]
- 8.Sherman KJ, Cherkin DC, Erro J, Miglioretti DL, Deyo RA. Comparing yoga, exercise, and a self-care book for chronic low back pain: A randomized, controlled trial. Ann Intern Med. 2005;143:849–56. doi: 10.7326/0003-4819-143-12-200512200-00003. [DOI] [PubMed] [Google Scholar]
- 9.Morone NE, Greco CM, Weiner DK. Mindfulness meditation for the treatment of chronic low back pain in older adults: A randomized controlled pilot study. Pain. 2008;134:310–9. doi: 10.1016/j.pain.2007.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morone NE, Rollman BL, Moore CG, Li Q, Weiner DK. A mind-body program for older adults with chronic low back pain: Results of a pilot study. Pain Med. 2009;10:1395–407. doi: 10.1111/j.1526-4637.2009.00746.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


