Abstract
Background
In 2003, New York City (NYC) implemented a series of coordinated policies designed to reduce non-communicable disease.
Methods
We used coarsened exact matching (CEM) of individuals living inside and outside NYC between the years of 1992-2000 and 2002-10 to estimate difference-in-difference survival time models, a quasi-experimental approach. We also fitted age-period-cohort (APC) models to explore mortality impacts by gender, race, age, borough and cause of death over this same time period.
Results
Both CEM and APC models show that survival gains were large in the pre-2003 era of health policy reform relative to the rest of the USA, but small afterwards. There is no clear link between any policy and changes in mortality by age, gender, ethnicity, borough, or cause of death.
Conclusions
NYC’s gains in survival relative to the rest of the nation were not linked to the city’s innovative and coordinated health policy efforts.
Keywords: health policy; social policy, ; bloomberg administration, ; urban design, ; urban health
Key Messages
In 2003, the City of New York implemented a large-scale, coordinated public health campaign.
Life expectancy gains in the City of New York have outpaced the rest of the USA.
Using quasi-experimental methods, we find that the overall gains in life expectancy are not due to the city’s coordinated health policies.
Likewise, the specific causes of death in New York City do not mesh with any of the city’s specific health policies.
Introduction
In 1990, New York City (NYC) had a life expectancy at birth that was 4 years behind that of the nation as a whole (68 years), but by 2010, it was 2 years ahead of the rest of the nation with a life expectancy of 78.1 Many, including the mayor’s office, linked this increase in life expectancy to a set of ambitious public health initiatives under Mayor Bloomberg.2–4 These initiatives were widely regarded as highly innovative and unprecedented, requiring coordination and cooperation between city agencies, re-design of the urban landscape, and new regulations on unhealthy foods and drugs.5,6 This coordinated approach has since become a global model for public health action, and has been adopted by many localities.7
The NYC health initiatives included smoking bans, cigarette taxation, trans fat bans, nutrition labelling in restaurants, new green space, active design recommendations for buildings, protected bicycle lanes, bicycle sharing programmes, public transport enhancements and traffic calming measures (among over 100 other interventions).8 These programmes were implemented at remarkably low cost. For instance, stone foundations of unused bridges and inexpensive, portable furniture were used to construct green spaces at a negligible cost to the taxpayer.
These measures were accompanied by sharp declines in smoking prevalence, reductions in accidents and increased public transit use.9,10 However, these changes came on the heels of massive demographic changes in NYC.11–13 Foreign-born and US-born newcomers to NYC live significantly longer and are less likely to smoke than US-born New Yorkers.14,15 To determine whether the story of NYC’s success in risk factor profiles and longevity is simply a story of demographic changes (or other secular, non-local trends), or whether the Bloomberg era health policies actually played a role in the city’s falling mortality rates, we used two datasets and two separate methods to examine the impact these policies might have had on mortality rates in NYC.
Methods
Overview
We used both age-period-cohort analysis (APC) and coarsened exact matching (CEM) in this study. CEM allows for a quasi-experimental (difference-in-difference) estimation of the effect of NYC’s policies on survival16 by matching NYC respondents to other US respondents who share similar demographic characteristics. We analysed these matches both before and after the initiation of Mayor Bloomberg’s coordinated health efforts in 2003 (our exposure of interest), and then compared the overall differences in mortality. However, this quasi-experimental technique relies on a sample, and does not allow for granular visualization of the changes that occurred in NYC between 1990 and the present day. We therefore employed an APC analysis by age, gender, race, ethnicity, borough and cause of death to show period-based trends in mortality between 1990 and 2011.
We first use the National Longitudinal Mortality Survey (NLMS) to match respondents who lived inside and outside NYC at the time of their interview and time of their death using CEM,16 a method that is conceptually similar to propensity score matching. We examine mortality outcomes over two time periods: (i) the pre-exposure period (1992-2000); and (ii) the post-exposure period (2003-10).
Next, we use annual death certificate data and official US population estimates to fit APC models to all deaths (rather than a smaller sample of deaths as in the CEM analysis) to observe if period-based variation in NYC mortality rates corresponds as expected with the city’s policies.17,18 We test these expected policy impacts by stratifying the APC analyses. Our a priori hypotheses across both analyses were that: (i) the 100 or so public health policies implemented under Mayor Bloomberg produced a measurable overall reduction in mortality over a roughly 20-year period of before/after surveillance; (ii) these reductions would be notable after (relative to before) their implementation in comparison with a similarly-matched cohort of Americans; and (iii) specific policies would be powerful enough to produce noticeable reductions in particular types of death, especially: accidents among young survey participants from Manhattan and Brooklyn; homicides city-wide; and cardiovascular-associated mortality among middle-aged participants city-wide.
A priori hypotheses surrounding predictable policy mortality impacts relevant to the APC models take into account the important observation that the city’s policy reforms were not uniformly distributed across the city. For example, Manhattan and Brooklyn disproportionately benefited from traffic calming measures, bike lanes and bike sharing programmes and closure of roads to put in public spaces.8,19–21 Some such changes were demand driven and others were only possible in places with business improvement districts (that could move tables and clean spaces at night), limiting most development to more affluent neighbourhoods in Manhattan and Brooklyn.22 These particular types of initiatives would be expected to reduce fatal collisions between pedestrians and bicyclists with motor vehicles. We would expect anti-smoking measures, food regulations and exercise measures to have impacts on heart disease (the most common smoking-, diet- and exercise-associated cause of death) across boroughs, but to mostly affect middle-aged men and older women—groups most at risk of cardiovascular disease.23 Given the relatively short time frame of follow-up though, we would expect to see only modest reductions in lung cancers, which can take years to develop and therefore are most likely to manifest as cohort-based trends.
CEM models and data
CEM is a form of propensity score matching that allows the user to specify plausible levels of each matching variable that the sample must be matched within; i.e. it ensures a minimum degree of balance in the matching procedure. After this initial ‘coarsened’ matching, the uncoarsened variables are used in model estimation.24 CEM is preferable to other matching procedures in terms of producing a balanced sample and reducing model dependence and estimation error.24
CEM maximizes pairings of like-to-like among treated (NYC) and untreated (remainder of the US) samples. We use the NLMS as our data source. Whereas NLMS contains multiple census data sources, the primary source of data is from the March Annual and Social Economic Supplements of the Current Population Survey. This supplement is an annual survey designed to collect detailed data about income, migration and health insurance, as well as a broader range of general economic data for persons aged 15 years and over. Roughly 60 000 households are interviewed annually, and one member of each household provides information for all members of the household. It is weighted and standardized to be reflective of the US population. The NLMS currently consists of approximately 3.8 million records with over 560 000 identified mortality cases up to (but not including) 1 January 2012.25 The NLMS data we employ contain 2.5 million observations of which 27 479 pertain to survey respondents residing within NYC in the years of interest. Of these, 25 830 were successfully matched to 900 242 NLMS participants residing outside NYC. CEM can match multiple individuals in one group to a single individual in another group (to enhance statistical power).
The matching rate is the number of cases that were matched as a percentage of all NLMS cases available for matching (that is, in the appropriate cohorts and with non-missing values for the matching variables) as shown.
The match rate for the 1992--2000 cohort was 77% for the US sample and 93% for the NYC sample. The match rate for the 2002-10 cohort was 73% and 95%, respectively. Cases with missing values were dropped.
The NLMS has geographical location at the time of interview and at the time of death. To select a matched sample of individuals living inside and outside NYC with a similar set of demographic and socioeconomic attributes, we performed CEM across the following variables: race (Black, White, other); Hispanic ethnicity (Puerto Rican, Central/South American/Mexican, other or not Hispanic); age (less than 25 years, 25-34 years, 35-44 years, 45-54 years, 55-64 years, 65-74 years, 75-84 years, greater than 84 years); education (<12 years, high school diploma, some college, college degree, graduate degree); employment status (employed, not employed, not in labour force aged less than 60, not in labour force aged 60 or more); marital status (married, widowed/divorced/separated, never married); veteran status (veteran, non-service); income (less than $25,000, $25,000-$50,000, greater than $50,000); and home ownership status (owns home, rents in cash, non-cash renter).
We used stratified Cox proportional hazard models to compare the likelihood of mortality for our sample before and after the implementation of the Bloomberg administration’s public health initiatives. Individuals were followed using administrative mortality follow-up data for a maximum of 5 years in each cohort to ensure equal follow-up times in each of the period cohorts. The 1992-2000 follow-up period was censored at 31 December 2001, and the 2002-10 period was censored at 31 December 2011. We included an interaction between the indicator variable denoting time period (1992-2000 vs 2002-10) and the indicator denoting residence in NYC. A significant interaction term is an indication of effects of the Bloomberg policies on survival. Difference-in-difference estimates were computed for women and men separately, as well as for the pooled sample. Stata version 13 (College Station, TX) was used for all analyses.
APC models
Population data for the APC models were obtained from the 1990-2011 Bridged-Race Population Estimates.26 Deaths for US residents and those in large cities in high-immigration states of Arizona, California, Florida, Illinois, and Texas between 1999 and 2010 were obtained from an Underlying Cause of Death request via CDC Wonder.26 Counts of death among New York City residents between 1990 and 2004 are made publicly available at the county level by the National Vital Statistics System’s (NVSS) Multiple Cause of Death Files, and NYC deaths between 2005 and 2010 were obtained from the NYC Department of Health and Mental Hygiene Death Master File.
We used the intrinsic estimator (IE) technique to fit APC models on age-specific mortality rates. This is a commonly used approach for parameter estimation in multiple classification APC models.27 Our APC analysis explores trends in age-specific mortality rates for three groups: (i) those within the USA as a whole; (ii) those residing within the five boroughs of NYC; and(iii) those residing in other US cities with large numbers of immigrants. Logged counts of deaths within each APC cell are assumed to follow a Poisson distribution.
We stratified models in the following ways: (i) all-cause age-specific mortality rates; (ii) those among children and adolescents (ages 1-4 through 15-19), younger-aged adults (ages 20-25 through 35-39), middle-aged adults (ages 40-44 through 60-64) and older-aged adults (65-69 through 80-84); (iii) select causes of death that have been targeted by NYC health initiatives (circulatory diseases, diabetes, lung cancer, breast cancer, and other cancers, transport-related accidents, homicides and infectious diseases); (iv) by each NYC borough, in order to explore spatial variation in the period-based trends of NYC mortality; and (v) non-Hispanic White, non-Hispanic Black and Hispanic NYC residents. We stratified trends by borough because Manhattan and Brooklyn received an unusually large share of the Bloomberg administration’s investments. For instance, 100% of the bike-sharing programme and public plaza space went to these boroughs. On the other hand, Queens did receive a large proportion of the city’s immigrant population since 1990 and the Bronx received a good share of HIV prevention funding.2,6 Robustness checks were applied to all APC models. Further details of the APC methods and results are available in the supplementary appendix (available as Supplementary data at IJE online).
The Columbia University institutional review board approved this study, and the NLMS was approved by the Centers for Disease Control and Prevention. Statistical code (modified to remove any potential identifying information) is available from the authors.
Results
CEM analysis
The supplementary appendix (available as Supplementary data at IJE online) describes the selection of a control group through CEM across a set of demographic and socioeconomic variables (race, Hispanic ethnicity, age, education, employment status, marital status, veteran status, income and home ownership).
Table 1 contains the basic demographic profiles of individuals included in the treatment and control groups after CEM. The racial and ethnic makeup of our cohorts changed substantially over time, with White respondents’ share of the matched observations declining over time among both men (falling from 71% of the 1992-2000 cohort to 58% of the 2002-10 cohort) and women (falling from 69% to 55%). The percentage of respondents of Central American, South American or Mexican ethnicity rose from approximately 12% to 20% for both men and women over the same time period. Women in the post-intervention cohort were more likely to be employed (48% vs 43%) and less likely to be widowed, divorced or separated (23% vs 27%). Men in the later cohort were less likely to be veterans (5% vs 11%). Male income was relatively stable across the two cohorts, whereas women’s incomes rose, on average, in the second cohort. Home ownership was slightly more common among both men and women in the post-intervention cohort.
Table 1.
Descriptive data for men and women residing inside and outside New York City (NYC), surveyed before the implementation of the Bloomberg administration’s public health initiatives (1992-2000) and after implementation (2002-10). Values represent the weighted demographics of the matched analytical sample, with unweighted n reported alongside percentages calculated using CEM weights, National Longitudinal Mortality Survey (1992-2011)
| Men, 1992-2000 |
Men, 2002-10 |
Women, 1992-2000 |
Women, 2002-10 |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Outside NYC | Inside NYC | Outside NYC | Inside NYC | Outside NYC | Inside NYC | Outside NYC | Inside NYC | ||
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||
| Age (mean, SD) | 40.7 (18.2) | 40.9 (18.1) | 40.0 (17.5) | 40.2 (17.4) | 42.8 (18.7) | 43.0 (18.7) | 42.4 (18.2) | 42.6 (18.2) | |
| Education, years (mean, SD) | 12.6 (3.9) | 12.7 (3.7)* | 13.0 (3.7) | 13.1 (3.6) | 12.4 (3.8) | 12.4 (3.7) | 13.0 (3.7) | 13.0 (3.7) | |
| Race | |||||||||
| White | 137589 (70.9) | 3778 (70.9) | 209901 (58.3) | 3398 (58.3) | 167329 (68.8) | 4979 (68.8) | 244644 (54.7) | 4065 (54.7) | |
| Black | 10437 (20.0) | 1065 (20.0) | 24709 (27.1) | 1581 (27.1) | 17415 (24.2) | 1751 (24.2) | 39216 (32.0) | 2375 (32.0) | |
| Othera | 5067 (9.1) | 483 (9.1) | 17532 (14.6) | 854 (14.6) | 5909 (7.0) | 510 (7.0) | 20494 (13.3) | 991 (13.3) | |
| Hispanic ethnicity | |||||||||
| Puerto Rican | 1278 (11.0) | 586 (11.0) | 2188 (8.3) | 486 (8.3) | 1796 (14.2) | 1025 (14.2) | 2974 (10.6) | 787 (10.6) | |
| Mexican | 9651 (13.0) | 693 (13.0) | 26195 (19.2) | 1122 (19.2) | 9100 (12.0) | 872 (12.0) | 25721 (19.5) | 1452 (19.5) | |
| Not Hispanic | 142164 (76.0) | 4047 (76.0) | 223759 (72.4) | 4225 (72.4) | 179757 (73.8) | 5343 (73.8) | 275659 (69.9) | 5192 (69.9) | |
| Employment status | |||||||||
| Employed | 110676 (59.2) | 3155 (59.2) | 182964 (60.4) | 3524 (60.4) | 105379 (42.6) | 3081 (42.6) | 180836 (48.5) | 3602 (48.2) | |
| Not employed | 8457 (12.0) | 637 (12.0) | 15243 (11.9) | 694 (11.9) | 11343 (11.0) | 797 (11.0) | 17697 (10.5) | 783 (10.5) | |
| Not in labuor force, age < 60 | 16337 (16.3) | 868 (16.3) | 35503 (18.0) | 1050 (18.0) | 40700 (30.0) | 2175 (30.0) | 67977 (27.2) | 2018 (27.2) | |
| Not in labour force, age > = 60 | 17623 (12.5) | 666 (12.5) | 18432 (9.7) | 565 (9.7) | 33231 (16.4) | 1187 (16.4) | 37844 (13.8) | 1028 (13.8) | |
| Marital status | |||||||||
| Married | 95388 (49.9) | 2656 (49.9) | 152263 (48.8) | 2849 (48.8) | 105299 (38.0) | 2750 (38.0) | 164171 (39.3) | 2923 (39.3) | |
| Not married | 9662 (11.0) | 588 (11.0) | 13196 (9.3) | 545 (9.3) | 39186 (27.5) | 1990 (27.5) | 54560 (23.2) | 1721 (23.2) | |
| Never married | 48043 (39.1) | 2082 (39.1) | 86683 (41.8) | 2439 (41.8) | 46168 (34.5) | 2500 (34.5) | 85623 (37.5) | 2787 (37.5) | |
| Veteran status | |||||||||
| Veteran | 28394 (11.1) | 589 (11.1) | 21236 (5.4) | 315 (5.4) | 57 (0.2) | 12 (0.2)* | 58 (0.2) | 14 (0.2) | |
| Non-service | 124699 (88.9) | 4737 (88.9) | 230906 (94.6) | 5518 (94.6) | 190596 (99.8) | 7228 (99.8) | 304296 (99.8) | 7417 (99.8) | |
| Income (1990 US$) | |||||||||
| < $25,000 | 49656 (46.4) | 2473 (46.4) | 74527 (43.1) | 2511 (43.1) | 80158 (57.6) | 4173 (57.6) | 113108 (51.5) | 3828 (51.5) | |
| $25,000-$50,000 | 50704 (28.9) | 1540 (28.9) | 75110 (29.4) | 1714 (29.4) | 57225 (23.8) | 1723 (23.8) | 88929 (26.8) | 1990 (26.78) | |
| > $50,000 | 52824 (24.7) | 1313 (24.7) | 102505 (27.6) | 1608 (27.6) | 53270 (18.6) | 1344 (18.6) | 102317 (21.7) | 1613 (21.71) | |
| Home ownership | |||||||||
| Owns home | 107705 (32.2) | 1715 (32.2) | 180722 (35.3) | 2056 (35.3) | 130271 (29.3) | 2119 (29.3) | 212305 (32.3) | 2398 (32.3) | |
| Rents in cash | 44862 (66.7) | 3552 (66.7) | 70870 (63.4) | 3698 (63.4) | 159644 (69.8) | 5054 (69.8) | 91485 (66.8) | 4963 (66.8) | |
| Renter, non-cash | 526 (1.1) | 59 (1.1) | 550 (1.4) | 79 (1.4) | 738 (0.9) | 67 (0.9) | 564 (0.9) | 70 (0.9) | |
| N (all) | 210527 | 5799 | 363246 | 6188 | 234739 | 7719 | 399624 | 7773 | |
| N (matched) | 153093 | 5326 | 252142 | 5833 | 190653 | 7240 | 304354 | 7431 | |
| N (unmatched) | 57434 | 473 | 111104 | 355 | 44086 | 479 | 95270 | 342 | |
Asian/Pacific Islander, Native American/American Indian etc.
Statistically significant at P < 0.05 using t tests for continuous variables and chi2 tests for categorical variables.
Stratified Cox proportional hazard models indicate that male and female NYC residents in the 1992-2000 cohort faced a markedly lower hazard of mortality relative to non-NYC residents [Table 2; hazard ratio (HR) = 0.74; 95% confidence interval (CI) = 0.67, 0.82]. This was true for men (HR = 0.73; 95% CI = 0.63, 0.84), and for women (HR = 0.76; 95% CI = 0.66, 0.87).
Table 2.
Results of Cox proportional hazards models examining relative likelihood of death of New York City (NYC) residents compared with non-NYC residents, before and after the implementation of Bloomberg's public health policies. National Longitudinal Mortality Survey (1992-2011)
| NYC residents, 1992-2000 |
NYC residents, 2002-10 |
Difference-in-differences |
||||
|---|---|---|---|---|---|---|
| Hazard ratioa | 95% CI (high, low) | Hazard ratioa | 95% CI (high, low) | Coefficient differenceb | 95% CI (high, low) | |
| All | 0.74 | (0.67, 0.82) | 0.80 | (0.70, 0.91) | 0.08 | (-0.09, 0.24) |
| Men | 0.73 | (0.63, 0.84) | 0.82 | (0.67, 1.00) | 0.12 | (-0.13, 0.37) |
| Women | 0.76 | (0.66, 0.87) | 0.78 | (0.65, 0.94) | 0.03 | (-0.19, 0.26) |
Mortality hazard ratios for New York City residents compared with non-NYC residents using coarsened exact matching based on race, Hispanic ethnicity, age, education, employment status, marital status, veteran status, income and home ownership.
The value represents the difference of the beta coefficient for the 1992-2010 period and the 2002-10 period, and the associated P-value. LCL; lower confidence limit, UCL; upper confidence limit.
When comparing the 2002-10 cohorts, NYC residents still faced a lower relative risk of mortality compared with non-NYC residents (HR = 0.80; 95% CI = 0.70, 0.91 overall; and HR = 0.82; 95% CI = 0.67, 1.0, HR = 0.78; 95% CI = 0.65, 0.94, for men and women, respectively). However, the magnitude of this difference is diminished somewhat compared with the 1992-2000 cohort. The HR for NYC residents relative to the rest of the USA increased by 0.08 overall, 0.12 for men and 0.03 for women. There was no statistically significant interaction between time and residence in proportional hazard models.
APC models
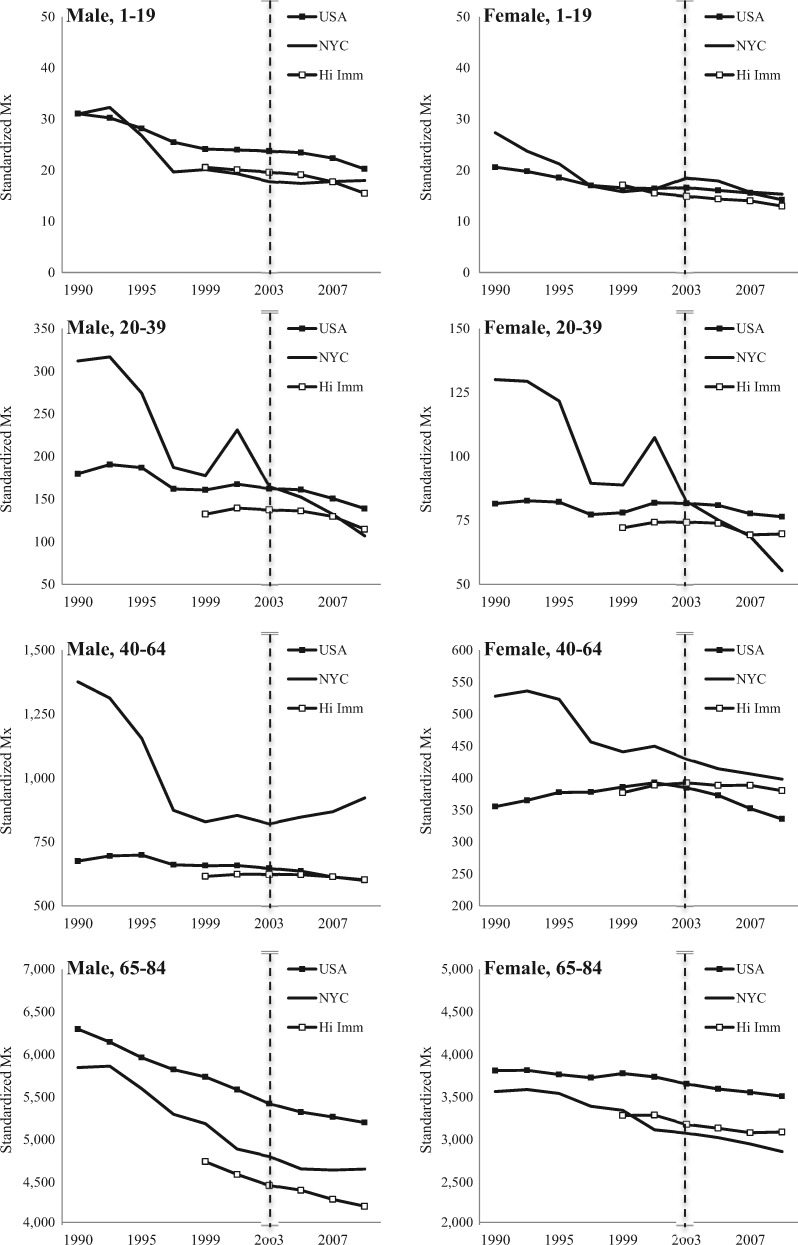
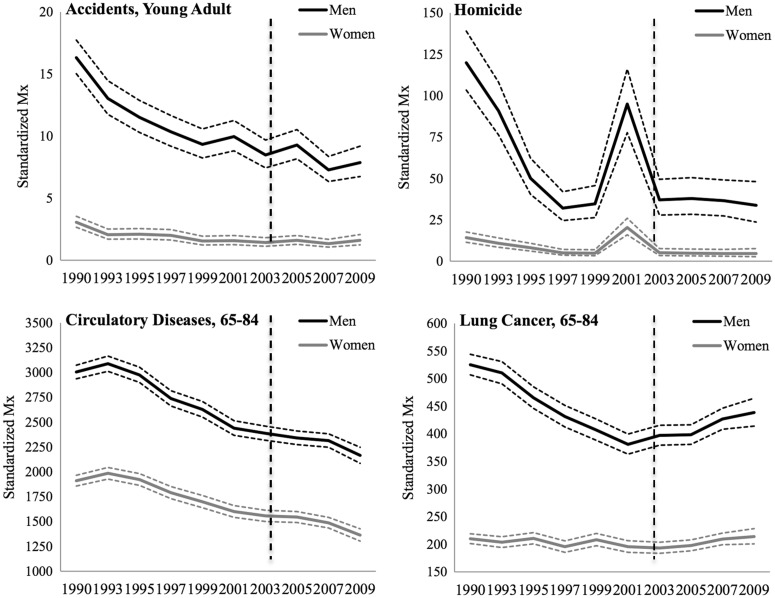
Figure 1 presents estimates of period-based trends in age-specific standardized mortality rates for NYC women and men and for all US men and women between 1990 and 2010, as well as for men and women in US cities with high proportions of foreign-born residents. These cities were selected as useful cities to compare with NYC, as the large foreign-born population in NYC is one of its defining characteristics. The largest investments made by the Bloomberg administration were in traffic safety (accident reduction), smoking (reduction of heart disease, stroke and cancer), food content (reductions in heart disease via trans fat bans and food labelling) and HIV prevention (e.g. free condom distribution).6 ‘Accidents’ (now called ‘crashes’ in NYC) are among the most common cause of death among younger people. Heart disease and cancers are more common causes of death among older people. Furthermore, we should see reductions in lung cancer (preventable via smoking cessation), but not breast cancer (no major primary prevention programme). Were Bloomberg era policies responsible for period-based reduction in mortality relative to the rest of the country, we would expect to see falls in accident deaths among young people and falls in heart disease (and possibly lung cancer) among older people in NYC relative to the comparison groups after 2003.
Figure 1.
Period-based variation in all-cause age-specific mortality rates in New York City, the US population and US cities with large foreign-born populations (‘Hi Imm’), 1990-2010. National Vital Statistics Survey System and New York City Department of Health and Mental Hygiene Death Master File. (The Y-axis, ‘Standardized Mx’ refers to the standardized mortality rate per 100 000 persons and the X-axis refers to the year of the analysis).
In the early 1990s, virtually all groups within NYC realized large reductions in standardized mortality rates relative to the USA as a whole or other urban areas see Figures 1 and 2; the spike in 2001 seen in most younger and middle-age groups and in the homicide cause of death represents September 11-associated deaths.) For NYC women and men aged 20-39 and for NYC girls aged 1-19, period-based mortality reductions continued across the 2000s. The steepest reductions were seen before the Bloomberg era, but it is plausible that Bloomberg era policies contributed to these reductions for these groups.
Figure 2.
Period-based variation age-specific mortality rates for selected causes of death in New York City, the US population and US cities with large foreign-born populations (Hi Imm), 1990-2010. National Vital Statistics Survey System and New York City Department of Health and Mental Hygiene Death Master File. (The Y-axis, ‘Standardized Mx’ refers to the standardized mortality rate per 100,000 persons and the X-axis refers to the year of the analysis).
For other age groups, the fall in standardized mortality rates seen in the 1990s in NYC relative to comparison groups slowed (e.g. women aged 40-64), stalled (e.g, male populations aged 1-19 and 65-84) or even increased relative to comparison groups (e.g. male population aged 40-64).
Period-based trends in NYC men’s and women’s mortality rates from homicides and transport-related accidents among young adults (top panels) and circulatory diseases and lung cancer (bottom panels) are shown in Figure 2. Period-based reductions in these causes of death occurred across the 1990s and 2000s, with the largest mortality reductions pre-dating the Bloomberg era policy reforms. More detailed figures, along with period-based data by race, ethnicity and borough, are included in the supplementary appendix (available as Supplementary data at IJE online). These additional analyses in the supplementary appendix show that non-preventable causes of death, such as breast cancer, fell and rose in tandem with preventable causes of death, and do not support hypothesized patterns of mortality that might be linked to Bloomberg era policies after 2003. An exception is the set of results showing that the largest period-based reductions in NYC mortality occurred in Manhattan, especially for mortality among younger-aged men and women (e.g. ages 1-39). However, the results also suggest that the period-based reductions in Manhattan mortality began before the Bloomberg era policies.
Discussion
Could NYC’s exceptional gains in life expectancy be attributed to its innovative public health agenda? We find that New Yorkers had survival advantages relative to other Americans that pre-dated NYC's aggressive health policy campaign. In both the quasi-experimental CEM and the descriptive APC models, we noted some convergence between the USA and the rest of the nation in the post-2003 period. Moreover, the APC models showed no clear link between a priori hypothesized mortality impacts and specific policies for any specific cause of death. Nor do the APC models show linkages between the geographical implementation of a policy and outcomes within a specific geographical region (e.g. protected bike lane construction in Manhattan and Brooklyn and traffic fatalities in these boroughs).
Although our findings do not support the hypothesis that the Bloomberg era policies improved health, they also do not refute them. Rather, any such gains might have been overwhelmed by factors that began to reduce mortality rates at rates that were greater in NYC than in the rest of the nation at least as early as the 1990s. This may have left less room for further reductions in the 2000s.
The leading hypothesis is that mortality rates in NYC fell due to higher migration rates to and from NYC relative to the rest of the nation.1 Previous work has suggested that newcomers to NYC (whether wealthy Americans or foreign-born people) are less likely to smoke, to drive cars, to commit violent crimes or to eat unhealthy foods.15,28
However, we find that NYC is a place that is healthier than other parts of the country even when immigration and migration of wealthier US-born people are taken into consideration in the analysis. (The CEM analysis matches for characteristics of those inside and outside NYC over two periods, for example, and the APC analysis compares NYC with other high-immigration cities.) However, it may also be that migration indirectly produces health among native New Yorkers by normalizing safe driving and a healthy lifestyle, and by driving demand for healthy foods in markets. If these spill-over effects are the driver of the better health outcomes we observe in the 1990s, then the city’s pro-immigration policies may have done more for its average health gains than its public health policies.
Together, our two analyses form a complementary and remarkably consistent picture of what happened in NYC relative to the rest of the country (or other high-immigration urban areas) since 1990. Whereas the CEM analysis provides a causal estimate of the impact of the policies on mortality overall, the APC analysis provides a more granular view of mortality trends in NYC—showing who was affected, where they were affected and of what they died.
However, it is not a complete picture. These combined approaches do not include measures of morbidity and have limited follow-up, and the CEM analyses do not allow for analyses across more than two points in time (somewhat increasing the chance of unobserved bias). Whereas the CEM models do account for all migration effects, the APC models only account for migration indirectly (via comparisons with other urban areas that are largely affected by healthy immigrant biases) and are subject to stronger assumptions.29 CEM models, on the other hand, can only measure whether mortality fell, not why.
The mortality reductions in the 1990s (seen in both the APC and CEM models) produced a much healthier city, and it is possible that mortality rates would have stabilized or even increased without the package of over 100 public health policies. These limitations should not be taken lightly, because the study could be perceived to have deep implications for public health policy. We do not find evidence that any given policy was successful. Surveillance data show that there were dramatic decreases in smoking rates observed in the 2000s and also increases in exercise.9 If these gains were due policy rather than migration, we should have observed a large reduction in circulatory diseases among middle-aged and older New Yorkers.30 However, standardized mortality rates for these causes (and for lung cancer) among older New Yorkers increased in the post-2003 era (Figures 1 and 2).Finally, mortality from diseases that should not have been influenced by any policies (e.g., breast cancer) showed declines in the 1990s in perfect parallel with those diseases that were preventable (see supplementary appendix).
These findings underscore a stronger political reality—even with a committed mayor who efficiently coordinates policies across city agencies, politics get in the way of health. Many scholars of this era argue that very little was actually accomplished because many or most of the initiatives met with political resistance.6 Bike lanes required lengthy community board fights. Congestion pricing was defeated. Those programmes that were implemented were unquestionably innovative, but the monetary investments in health that were made under Bloomberg were modest.
Whereas our findings do not support the notion that coordinated public health efforts in NYC were responsible for the observed gains in life expectancy, they also do not refute the claim. NYC is by its nature very similar to the public health ‘ideal’ seen in many European cities and has been so for a long time, and this ideal improved under the Bloomberg administration. Low-rise buildings with ample public transport and shopfront space mean that New Yorkers have many more opportunities to shop and work within their own communities, thereby increasing exercise while reducing exposure to automobile pollution and traffic accidents.31,32 In this respect, New York has been on a steady upward improvement since its boom in public transport ridership, seen after investments in its subway lines and policing starting in 1989.21 Indeed, the gains in life expectancy within New York have paralleled those of Australia, Canada, the UK, Sweden, France, Japan and The Netherlands—countries with very similar urban infrastructure to NYC—at the same time as the rest of the USA is falling far behind these nations with respect to changes in life expectancy.33 In this sense, New York City might not be so exceptional after all. It might simply be that the rest of the nation is falling behind.
Supplementary Data
Supplementary data are available at IJE online.
Funding and acknowledgements
We would like to thank the Robert Wood Johnson Foundation for primarily supporting this research and the U.S. Census Bureau for their support of the National Longitudinal Mortality Survey component of the paper. The opinions expressed are those of the authors, and do not necessarily reflect those of the U.S. Census Bureau.
Author Contributions
P.M. conceived of the analysis and wrote the manuscript; D.V., S.H., R.M. and J.H. made significant contributions to the methodological approach and the development of the manuscript.
Supplementary Material
References
- 1. Preston SH, Elo IT.. Anatomy of a municipal triumph: New York City's upsurge in life expectancy. Popul Dev Rev 2013;40:1-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. City of New York, Office of the Mayor. Mayor Bloomberg, Deputy Mayor Gibbs, Health Commissioner Farley announce New Yorkers living longer than ever, outpacing national trend. Press Release No. 453. 27 December 2011.
- 3. Wang H, Schumacher AE, Levitz CE, Mokdad AH, Murray CJ.. Left behind: widening disparities for males and females in US county life expectancy, 1985-2010. Popul Health Metr 2013;11:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. New York City Department of Health and Mental Hygiene. Take Care New York2012. http://www.nyc.gov/html/doh/downloads/pdf/tcny/tcny-2012.pdf (1 October 2012, date last accessed).
- 5. Li W MG, Begier EM.. Life Expectancy in New York City:What Accounts for the Gains? New York City, NY: Department of Health and Mental Hygiene, 2013. [Google Scholar]
- 6. Isett KR, Laugesen MJ, Cloud DH.. Learning from New York City: a case study of public health policy practice in the Bloomberg administration. J Public Health Manag Pract 2015;21:313-22. [DOI] [PubMed] [Google Scholar]
- 7. 2X2 Project. What Public Health Legacy Does Bloomberg Leave Behind?2013. http://the2x2project.org/what-public-health-legacy-does-bloomberg-leave-behind/ (4 October 2015, date last accessed).
- 8. New York City Department of Health and Mental Hygiene. Take Care New York.http://www.nyc.gov/html/doh/html/about/tcny.shtml (21 October 2016, date last accessed).
- 9. Centers for Disease Control and Prevention. Decline in smoking prevalence - New York City, 2002-2006. MMWR Morb Mortal Wkly Rep 2007;56:604. [PubMed] [Google Scholar]
- 10. Muennig PA, Epstein M, Li G, DiMaggio C.. The cost-effectiveness of New York City's Safe Routes to School Programme. Am J Public Health 2014;104:1294-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Barton MS. Gentrification and violent crime in New York City. Crime & Delinquency 2014:0011128714549652. [Google Scholar]
- 12. Huynh M, Maroko A.. Gentrification and preterm birth in New York City, 2008–2010. J Urban Health 2014;91:211-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Foner N. New Immigrants in New York. New York, NY: Columbia University Press, 2001. [Google Scholar]
- 14. Muennig P, Fahs MC.. Health status and hospital utilization of recent immigrants to New York City. Prev Med 2002;35:225-31. [DOI] [PubMed] [Google Scholar]
- 15. Muennig P, Wang Y, Jacubowski A.. The health of immigrants to New York City from Mainland China: Evidence from the New York Health Examination and Nutrition Survey. Journal of Immigrant and Refugee Studies 2012;10:1-7. [Google Scholar]
- 16. Blackwell M, Iacus S, King G, Porro G.. cem:Coarsened Exact Matching in Stata. Stata J 2009;9:524-46 [Google Scholar]
- 17. Kupper LL, Janis JM, Karmous A, Greenberg BG.. Statistical age-period-cohort analysis: a review and critique. J Chronic Dis 1985;38:811-30. [DOI] [PubMed] [Google Scholar]
- 18. Clayton D, Schifflers E.. Models for temporal variation in cancer rates. II: age–period–cohort models. Stat Med 1987;6:469-81. [DOI] [PubMed] [Google Scholar]
- 19. New York City Department of Transportation. Safety Programmes: Safe Routes to Schools http://www.nyc.gov/html/dot/html/safety/saferoutes.shtml (15 December 2012, date last accessed).
- 20. New York City Department of Transportation. 2013 NYC In-Season Cycling Indicator http://www.nyc.gov/html/dot/downloads/pdf/2013-isci-2-25-14.pdf (27 August 2014, date last accessed).
- 21. Metropolitan Transit Authority. New York City Transit - History and Chronology http://web.mta.info/nyct/facts/ffhist.htm (16 August 2015, date last accessed).
- 22. New York City Plaza Program Sites. New York City Department of Transportation. http://www.nyc.gov/html/dot/html/pedestrians/nyc-plaza-program.shtml (21 October, 2016, date last accessed).
- 23. Centers for Disease Control and Prevention. Annual smoking attributable mortality, years of potential life lost and economic costs - United States, 1995-1999. JAMA 2002;287:2355-56. [PubMed] [Google Scholar]
- 24. Iacus SM, King G, Porro G.. Causal inference without balance checking: Coarsened exact matching. Pol itical analysis 2011:mpr013. [Google Scholar]
- 25. Naitonal Longitudinal Mortality Survey. Variable Reference Manual.https://www.census.gov/did/www/nlms/publications/docs/referenceManual_v4.pdf (15 May 2016, date last accessed).
- 26. Wonder C. Bridged-Race Population Estimates. Atlanta, GA: Centers for Disease Control and Prevention, 2016. [Google Scholar]
- 27. Yang Y, Schulhofer‐Wohl S, Fu WJ, Land KC.. The intrinsic estimator for age‐period‐cohort analysis: what it is and how to use it. Am J Sociol 2008;113:1697-736. [Google Scholar]
- 28. Rundle A, Neckerman KM, Freeman L. et al . Neighborhood food environment and walkability predict obesity in New York City. Environ Health Perspect 2009;117:442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Luo L. Assessing validity and application scope of the intrinsic estimator approach to the age-period-cohort problem. Demography 2013;50:1945-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mokdad AH, Marks JS, Stroup DF, Gerberding JL.. Actual causes of death in the United States, 2000. JAMA 2004;291:1238-45. [DOI] [PubMed] [Google Scholar]
- 31. Diez-Roux AV. Neighborhood environments and coronary heart disease: a multilevel analysis. Am J Epidemiol 1997;146:48-63. [DOI] [PubMed] [Google Scholar]
- 32. Kawachi I, Berkman LF.. Neighborhoods and Health. New York, NY: Oxford University Press, 2003. [Google Scholar]
- 33. Muennig PA, Glied SA.. What changes in survival rates tell us about us health care. Health Aff (Millwood) 2010;29:2105-13. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.