Abstract
Hispanic Americans comprise the largest and fastest-growing ethnic minority in the USA. In Houston, Texas, 44% of the population is of Hispanic descent, with the majority being Mexican Americans (78%). This population is under-represented in health-related research despite their high prevalence of obesity and diabetes, which may predispose them to cancer and other chronic conditions. Recognizing the need for a greater research effort into the health risks of Hispanic Americans, the population-based Mexican American (Mano a Mano) Cohort study was launched in 2001. This is an open cohort with enrolment ongoing to 2019, and as of 30 June 2014, 23 606 adult participants from over 16 600 households were enrolled. Bilingual interviewers elicit information in person on demographics, acculturation, lifestyle, occupation, medical history, family cancer history, self-reported and measured height and weight, and other exposures. Urine, blood and saliva samples have been collected at baseline from 43%, 56% and 63% of participants, respectively. DNA samples are available for about 90% of participants. Incident cancers and other chronic diseases are ascertained through annual telephone re-contact and linkage to the Texas Cancer Registry and/or medical records. Molecular data such as genetic ancestry markers, blood telomere length and HbA1c, a marker of impaired glucose tolerance, are available for a substantial proportion of the participants. Data access is provided on request [manoamano@mdanderson.org]. For further information please visit [www.mano-mano.us].
Why was the cohort set up?
By the year 2050, Hispanics are expected to make up almost one-third of the US population.1 Mexican Americans comprise the largest and fastest-growing subgroup among Hispanics.2 In Harris County (metropolitan Houston), Texas, 44% of the population is of Hispanic descent, with the majority being Mexican Americans (78%). Hispanics accounted for half of the population living in poverty and 53% of the uninsured in Harris County.3 This population also has special health needs due to a very high prevalence of obesity and diabetes,4,5 but they are under-represented in health-related research. Despite these conditions, Hispanic Americans tend to have lower overall mortality rates and incidence rates of many diseases, including cancer, than non-Hispanic Whites.6 To date this well-documented and much-debated ‘Hispanic paradox’ remains an enigma,3,7 perhaps due in part to a general dearth of health research focusing on Hispanic Americans. Furthermore, the high prevalence of obesity notwithstanding, cancer has surpassed cardiovascular disease to become the leading cause of death among the US Hispanic population.6 Unlocking the mystery of the Hispanic paradox and identifying reasons for the disparate disease risks among Hispanic Americans may provide new insight to the aetiology of cancer and other chronic diseases. Recognizing both the need for a greater research effort into the health risks of this large segment of population in transition, and the unique research opportunity that this population provides in understanding gene-environment interactions, the Mexican American (Mano a Mano) Cohort was launched in 2001.
The overarching aim of this cohort is to understand cancer and other chronic disease risk and protective factors as they emerge in the Mexican American population undergoing social changes, and to use this information to facilitate the development of population-specific prevention strategies for cancer and cancer-predisposing conditions, such as obesity and diabetes.8 The comprehensive questionnaire data and stored biological samples from cohort participants provide a rich resource and infrastructure to support collaborative multidisciplinary research into genetic, lifestyle and environmental causes of diseases and their interactions. To our knowledge, this study forms the largest longitudinal comprehensive cohort study with biological sample collection from a Mexican American population (reviewed in Appendix 1, available as Supplementary data at IJE online).
There is evidence that immigrating and adopting a new culture (acculturation) can influence behaviours and health status specifically in Hispanic populations. For example, Guendelman and colleagues9 found that US-born Mexican American women were more likely to be obese than women living in Mexico, and Gorman et al.10 showed that greater acculturation leads to deteriorating health over time. Other studies have shown that greater acculturation by Hispanics is associated with higher odds of meeting physical activity recommendations, but also higher levels of drinking alcohol.11,12 In addition, although Mexican Americans exhibit low rates of cancer overall,13 increased duration of residence in the USA is associated with increased risk of common cancers among Hispanics.13,14 These data highlight a population in transition and point to the need to capture the changes in health behaviours and associated disease risks as they adapt to the US culture and lifestyle.
Who is in the cohort?
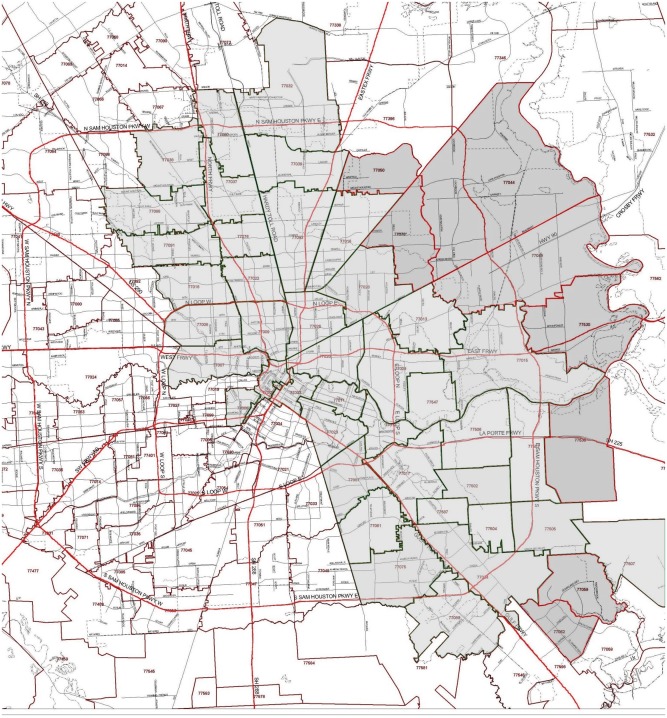
Cohort participants are individuals of self-reported Mexican descent (henceforth referred to as Mexican Americans) who have resided in the metropolitan Houston area for at least 1 year. Up to three individuals were recruited from households with eligible participants. There was no age restriction at the start of the cohort (i.e. 2001); however, as of January 2014, the eligibility criteria were modified to include only men and women ages 35 to 75 years at enrolment, to capture the age groups with increased risk for developing cancer and other chronic diseases. The study catchment area currently includes 50 postal zip code areas along the Interstate Highway 45 (I-45) where the population of under-served Mexican Americans traditionally reside (Figure 1). Compared with Harris County overall, our study catchment area has a higher percentage of Hispanic residents (44% vs 81%) but, of the Hispanic population, a lower proportion of Mexican Americans (68%) than Harris County overall (78%).15 Over the past decade, there has been an out-migration of Mexican Americans from the study area to the outer suburbs of Houston, particularly to areas east of the I-45 corridor. In January 2014, the cohort catchment area was expanded with a goal to further expand recruitment to the entire metropolitan area of Houston in 2015. With this expansion, we expect to broaden the socioeconomic diversity and range of lifestyle and environmental exposures of the cohort participants. Our ultimate goal is to continue recruitment until 2019, reaching an expected cohort size of about 40 000 participants.
Figure 1.
Catchment area of the Mexican American Cohort in the Houston metropolitan area. The lightly-shaded areas show the original catchment area, and the darker-shaded areas include zipcodes expanded beginning in January 2014.
In addition, 1181 children (543 boys and 638 girls) of the adult cohort participants were recruited from 1075 households during 2001–2003, and were followed up in 2005–06, 2008–09 and 2010–11. The children were ages 4 to 17 (mean 11.6 ± 4.1) years at the time of enrolment, and were placed in a separate cohort for studying childhood-related health issues.15–17 Written informed consent was obtained from all adult participants and, for children, an adult parent of each child along with informed assent from the child.
Potential participants are currently recruited at neighbourhood libraries, community centres, health clinics, health fairs and other neighbourhood facilities and events. Interested individuals are then contacted by the Cohort scheduling team to set up an appointment for interview and biological sample collection at the participants’ homes or at other places convenient to them. All field staff are fluent in both English and Spanish and use bilingual questionnaires and consent forms to facilitate communication in the participants’ preferred language. Informed consents are signed prior to interviewing and bio-specimen collection. A small gift card is presented to the participant at the completion of interview as a token of appreciation for his/her time and effort.
As of June 2014, we have enrolled 23 606 adult participants (ages ≥18 years) from over 16 600 households. The majority of the cohort participants are women (79%), reflecting a greater pool of women recruited at neighbourhood facilities and events (Table 1). The average age at enrolment is 40.8 years (±14.2 years), with men being slightly older than women (42.7 vs 40.2 years, respectively). Men were more likely to be married (81.4%) than women (75.0%) at baseline. The majority of participants (60%) did not graduate from high school. Nearly 74% of the participants were born in Mexico, but had lived in the USA for an average of 15.3 years (±11.2 years) at enrolment.
Table 1.
Participant characteristics at enrolment in the Mexican American Mano a Mano Cohort
| Total | Men | Women | |
|---|---|---|---|
| Variable | N (%), or mean (SD) | ||
| Total number | 23 606 | 4886 (20.7) | 18 720 (79.3) |
| Mean age (years) | 40.8 (s.d. ± 14.2) | 42.7 (s.d. ± 15.2) | 40.2 (s.d ± 13.9) |
| < 40 | 12 063 (52.3) | 2563 (48.0) | 10063 (55.1) |
| 40–49 | 4885 (21.2) | 1095 (20.5) | 3790 (20.8) |
| 50–59 | 3274 (14.2) | 834 (15.6) | 2440 (13.4) |
| ≥ 60 | 2821 (12.2) | 851 (15.9) | 1970 (10.8) |
| Marital status | |||
| Married | 18 040 (76.4) | 4351 (81.4) | 13 689 (75.0) |
| Other | 5532 (23.4) | 986 (18.5) | 4546 (24.9) |
| Education | |||
| Elementary school or less | 5440 (23.1) | 1170 (21.9) | 4270 (23.4) |
| Middle school/some high school | 8708 (36.9) | 2004 (37.5) | 6704 (36.7) |
| HS diploma/GED/technical traininga | 6723 (28.6) | 1461 (27.3) | 5262 (28.8) |
| Some college and beyond | 2723 (11.6) | 705 (13.2) | 2018 (11.0) |
| Born in the USA | |||
| Yes | 6194 (26.3) | 1608 (30.1) | 4586 (25.1) |
| No | 17 384 (73.7) | 3728 (69.9) | 16 656 (74.9) |
| Years living in the USA (among non US-born) | |||
| <10 years | 5920 (34.1) | 1010 (27.1) | 4910 (36.0) |
| 10–19 years | 5954 (34.3) | 1129 (30.3) | 4825 (35.3) |
| ≥20 years | 5503 (31.7) | 1586 (42.6) | 3917 (28.7) |
| Alcohol drinking | |||
| Never | 15 411 (66.7) | 1271 (24.5) | 14 140 (78.9) |
| Former | 2380 (10.3) | 1208 (23.3) | 1172 (6.5) |
| Current | 5312 (23.0) | 2703 (52.2) | 2609 (14.6) |
| Cigarette smoking | |||
| Never | 17 021 (72.9) | 2347 (44.6) | 14 674 (81.1) |
| Former | 3436 (14.7) | 1565 (29.7) | 1871 (10.3) |
| Current | 2905 (12.4) | 1349 (25.6) | 1556 (8.6) |
| Body mass index (BMI, kg/m2) | |||
| Normal/underweight (<25) | 3956 (16.8) | 886 (16.7) | 3070 (17.0) |
| Overweight (25–< 30) | 7931 (33.6) | 2188 (41.1) | 5743 (31.8) |
| Obese (30–< 35) | 6461 (27.4) | 1459 (27.4) | 5002 (27.7) |
| Morbidly obese (≥ 35) | 5034 (21.3) | 787 (14.8) | 4247 (23.5) |
aHS: high school; GED: General Education Development.
Approximately 23% of the cohort participants are current alcohol drinkers and 12.4% are current smokers, with more men than women reporting being a current drinker (52.2% vs 14.6%, respectively) and current smoker (25.6% vs 8.6%, respectively) (Table 1). These percentages are generally lower than those reported for the overall national Mexican American population: 76.6% and 54.1% of Mexican American men and women, respectively, are current alcohol drinkers and 27.0% and 13.1% of Mexican American men and women, respectively, are current smokers.18 The prevalence of obesity in the Cohort (48.7%) is much higher than the 32.3% reported in the overall Hispanic population of Texas.19
How often have they been followed up?
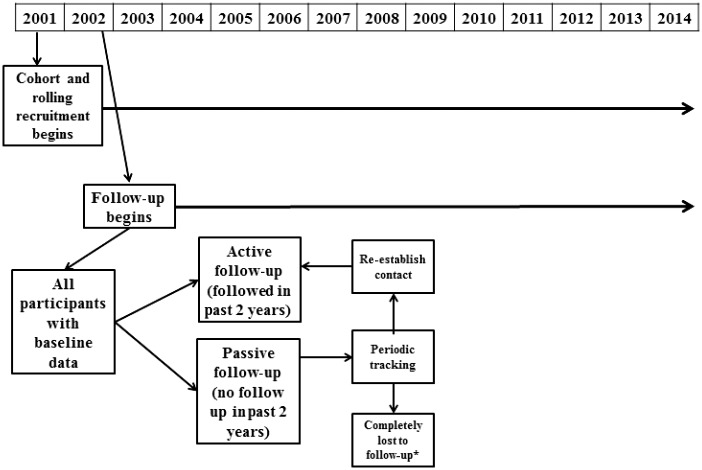
Participants have been actively followed up via annual telephone re-contact to update selected exposures and new diagnosis of selected chronic diseases, including cancer, cardiovascular disease, asthma, chronic obstructive pulmonary disease and diabetes. Ongoing attempts are made to contact all participants at least once per year. Participants who were contacted within the past 2 years are considered to be in active follow-up; participants not directly contacted in the past 2 years are passively followed up. Periodic attempts are made to re-contact passively followed participants (Figure 2) and place them in the actively followed pool as re-contact is made. Recently we reviewed medical records for 126 participants who reported a new diagnosis of diabetes, and confirmed the diagnosis in 123 (98%) of them. We plan to systematically review medical records for a sample of participants who reported other chronic diseases, to assess the accuracy of their reporting.
Figure 2.
Diagram of participant flow in the Mano A Mano Cohort. Asterisk indicates completely lost to follow-up and can include: deceased, refusal to participate in follow-up and participants who have moved away and/or are unable to be located.
In addition to self-report during annual telephone re-contact, newly diagnosed cancers are also identified through annual record linkage to the population-based Texas Cancer Registry (TCR). The completeness of cancer registration among Texas residents is estimated to be more than 95%.20 Self-reported cancer diagnosis not identified in the TCR (e.g. due to a time lag in reporting or diagnosis outsideTexas) are verified through review of medical records. To date, a total of 548 incident cancer cases have been identified; breast cancer is by far the most common cancer among women and prostate cancer is the most common cancer among men (Table 2). In addition, newly diagnosed chronic diseases such as diabetes and hypertension have been reported by 5.0% and 7.0% of cohort participants, respectively.
Table 2.
Chronic disease incidence in the Mano a Mano Cohort as of 30 June 2014
| Chronic disease | N |
|---|---|
| Cancer (total combined) | 548 |
| Breast | 119 |
| Prostate | 40 |
| Lung | 32 |
| Cervical | 25 |
| Heart disease | |
| Hypertension | 1650 |
| Heart attack | 96 |
| Stroke | 86 |
| Diabetes | 1170 |
Several methods are used to track participants with whom contact via telephone (calls made at various times of the day and various days of the week) and mail failed. These methods include contacting friends and relatives reported by the participant at enrolment and last follow-up, visiting non-responders at their last known address and talking with neighbours, and using a commercially available tracking system. The current overall follow-up rate for the cohort is 70.7%, with 64.2% for participants enrolled before 2006 and 79.3% for those enrolled in 2006 and thereafter. With a commercial tracking system, we have increased our rate of success in re-establishing contact with many participants enrolled during the early years of the cohort and anticipate that our response rates will increase over time. Furthermore, participants lost to active follow-up are being passively followed through annual linkage to the TCR for incident cancer diagnosis. At the time of this report, the mean active follow-up time is 5.7 years (SD ±3.2; range <1–13 years), with a total of 114 300 person-years accumulated. Characteristics of cohort participants being actively followed vs those who are passively followed for cancer incidence through linkage to TCR are presented in Table 3. The distributions in demographic characteristics, acculturation, exposures to alcohol and tobacco, and excess body weight are comparable for participants being actively vs passively followed, suggesting that potential bias due to lost to follow-up should be minimal.
Table 3.
Baseline characteristics of participants actively vs passively followed up in the Mano a Mano Cohort
| Variable | Category | Actively followed (as of June 2014) |
Passively followed (as of June 2014) |
||
|---|---|---|---|---|---|
| Number | Percent | Number | Percent | ||
| Total N | 16 685 | 70.7 | 6921 | 29.3 | |
| Gender | Male | 3801 | 22.8 | 1542 | 22.3 |
| Female | 12884 | 77.2 | 5379 | 77.7 | |
| Age (years) | ≤ 39 | 8799 | 52.7 | 3827 | 55.3 |
| 40–49 | 3564 | 21.4 | 1321 | 19.1 | |
| 50–59 | 2354 | 14.1 | 920 | 13.3 | |
| ≥ 60 | 1968 | 11.8 | 853 | 12.3 | |
| Education | ≤ Elementary school | 3859 | 23.1 | 1581 | 22.9 |
| Middle/some high school | 6015 | 36.1 | 2693 | 39.0 | |
| High school diploma/ technical training | 4838 | 29.0 | 1885 | 27.3 | |
| ≥ Some college | 1967 | 11.8 | 756 | 11.0 | |
| Marital status | Married | 12 723 | 76.3 | 5317 | 77.0 |
| Other | 3942 | 23.7 | 1590 | 23.0 | |
| US-born | No | 12 323 | 74.0 | 5056 | 73.2 |
| Yes | 4340 | 26.0 | 1854 | 26.8 | |
| Years lived in USA (among foreign-born) | ≤ 5 | 1524 | 12.4 | 794 | 15.7 |
| 5–9 | 2500 | 20.3 | 1102 | 21.8 | |
| ≥ 10 | 8297 | 67.3 | 3160 | 62.5 | |
| Alcohol drinking | Current | 3748 | 22.9 | 1564 | 23.1 |
| Former | 1661 | 10.2 | 719 | 10.6 | |
| Never | 10 926 | 66.9 | 4485 | 66.3 | |
| Cigarette smoking | Current | 2063 | 12.5 | 842 | 12.3 |
| Former | 2449 | 14.8 | 987 | 14.5 | |
| Never | 12 024 | 72.7 | 4997 | 73.2 | |
| BMI | < 25 | 2761 | 16.7 | 1253 | 18.4 |
| 25–< 30 | 5547 | 33.5 | 2334 | 34.2 | |
| ≥ 30 | 8246 | 49.8 | 3236 | 47.4 | |
What has been collected and measured?
Baseline questionnaire
At cohort enrolment, all participants are administered a questionnaire in person by trained interviewers. A paper form of the questionnaire was used until 2012 when a digital version was developed on laptop computers, with built-in skip patterns and range and logic checks for quality control. Data are immediately transmitted to a secure server and erased from the laptop for security purposes. Table 4 includes the major questionnaire components, as well as modifications made over the years.
Table 4.
Questionnaire components and modifications in the Mano A Mano Cohort
| Variable | 2001-03 | 2004-05 | 2006-11 | 2012- |
|---|---|---|---|---|
| Background/demographics | ||||
| When/where born, marital status, religion, education, self-reported height and weight | • | • | • | • |
| Parents’/spouse’s race | • | |||
| Family history | ||||
| Blood relatives, medical history | • | • | • | • |
| Prostate –specific antigen screening (men) | • | |||
| Reproductive and cancer screening history (women) | • | |||
| Acculturation | ||||
| Years lived in USA, speak/read/watch television/listen to radio in English/Spanish | • | • | • | • |
| Read newspapers/magazines in English/Spanish | • | • | • | |
| Foods eaten at home, ethnicity of spouse/friends, cultural holidays and traditions celebrated | • | • | ||
| Physical activity/sedentary behavior | ||||
| Usual physical activity of past year, sleeping h/day | • | • | • | |
| Sitting h/day | • | • | • | • |
| Activity of past week | • | |||
| Work history | ||||
| 3 longest-held jobs (duties, equipment, years worked; also spouse job and farm work) | • | |||
| Job category for longest-held job (based on North American Classification of Occupations) | • | • | ||
| Details of current/last job held (duties, equipment, farm work) | • | |||
| Job exposures | ||||
| For at least 6 months, including: pesticides, paints, gasoline, dust, exhaust and other fumes, chemicals, oils | • | • | • | • |
| Lifestyle habits | ||||
| Alcohol use (type and amount drank) | • | • | • | • |
| Type of beer, type of wine, binge drinking | • | |||
| Cigarette use (# per day, age when started) | • | • | • | • |
| If quit smoking: why and what method was used | • | |||
| Use of smokeless tobacco, pipes | • | |||
| Access to health care and screening practices | ||||
| Health care coverage and type | • | • | • | |
| Type of health care used (doctor, emergency room, clinic etc.) | • | • | • | |
| Self-rated health | • | • | ||
| Frequency of checkups, weight changes across lifespan, stool test or colonoscopy | • | |||
| Residence | ||||
| Income | • | • | • | |
| Source of drinking water | • | |||
| Own your house/car | • | • | • | |
| Years lived in Texas/Harris County | • | • | • | |
| Media usage | ||||
| Electronic device, cellphone, social media usage | • | |||
| Anthropometrya | ||||
| Self-reported height/weight | • | • | • | • |
| Measured height/weight | • | • | ||
| Blood pressure | • | |||
aIn addition to self-reported height and weight, baseline height and weight are measured by trained field staff since 2006 (n participants = 10 391).
Baseline biological sample collection
At enrolment, participants are invited to consider an optional component of the investigation: biological sample collection. Overall, 90% of participants donated a biological sample, including 56% who donated a blood sample, 63% a saliva sample and 43% a urine sample. The samples are transported in a cooler to the laboratory and processed within 24 h of collection. The processed samples are stored in liquid nitrogen or -80°C freezers. Using these samples, a number of molecular markers have been analysed and the data deposited in the cohort database and made available for future investigations. These markers include telomere length in peripheral blood DNA from about 13 000 cohort participants, genetic ancestry informative markers from about 5000 participants and HbA1c, a marker of impaired glucose tolerance/ long-term glycaemic control, from about 11 000 participants.
Annual follow-up questionnaire
At annual follow-up, a short questionnaire is administered via telephone to update information on current address, additional contact persons, cigarette smoking, current weight and new diagnosis of cancer, diabetes, stroke, and selected other chronic diseases. If a new cancer diagnosis is reported, the type of cancer, age at diagnosis and the physician and hospital names for diagnosis/treatment are ascertained. The participant’s approval is sought and a signed authorization form, to release medical records related to the cancer diagnosis, is requested by mail. Likewise when a new diagnosis of diabetes is reported, additional information is requested on the type of diabetes, type of treatment and names of the physician and hospital/clinic for diagnosis/treatment.
What has been found?
The majority of analyses from the Mexican American Cohort have focused on the relationship between contextual factors (e.g. demographic background, acculturation and socioeconomic status) and health behaviours such as smoking and physical activity, and in turn, how health behaviours may influence physical development and the development of abnormal conditions such as obesity, hypertension, diabetes and cancers. A list of these articles can be found on the Mexican American Cohort website [www.mano-mano.us]. Some of the main findings from those studies are summarized below.
Among Mexican American adolescents in our cohort, we investigated longitudinally how psychosocial, behavioural and contextual factors in early life may determine smoking experimentation and maintenance. Adolescents who have experimented with cigarettes report more family conflict, lower subjective social status, greater belief that smoking may provide social benefits and having more concerns about their body image than their peers who have not experimented.21–24 Furthermore, genetic variants in genes involved in dopamine, serotonin and opioid pathways (e.g. HTR2A, DRD2 and SLC6A3) were associated with risk of smoking experimentation.17 In another intervention study of reducing second-hand smoke (SHS), ambient nicotine levels decreased from 1.14 μg/m3 to 0.20 μg/m3 (p < 0.01) after 12 months of follow-up in households receiving experimental intervention, with increased awareness of health effects of SHS, compared with those receiving standard care.26 Consistent with observations in other reports, US-born adults in our cohort were more likely to be obese compared with their Mexican-born counterparts (49% vs 41%, p < 0.001).27 The risk of being overweight doubled in children born to obese mothers and mothers with less than high school education, and in children born in the USA.17 In contrast, moderate and strenuous physical activities were inversely related to the prevalence of obesity, diabetes and hypertension.8 Participation in physical activity, however, varies by gender and is influenced by factors such as parental education, television viewing and linguistic acculturation.28
Another recent effort examining risk of obesity and diabetes in relation to genetic ancestral markers revealed that a 5% increase in African ancestry corresponded to a 12% increased risk of grade 2 obesity [body mass index (BMI) between 35 and 40; p = 0.037] and an 18% increased risk of grade 3 obesity (BMI>40; p = 0.006) whereas native American ancestry was correlated with diabetes risk (p = 0.018).29 Of interest, Mexican-American girls have one of the fastest declining rates in age at menarche.30 In our cohort, an earlier age at menarche was associated with the perception of conflict-prone family life environment [odds ratio (OR)=1.15, 95% confidence interval (CI): 1.02, 1.29] and having a mother who was a single parent (OR=2.22, CI: 1.12, 4.40).15 An elevated risk of breast cancer was observed among women with a family history of cancer (OR=4.3, CI: 2.14, 8.5), with no health insurance (OR=1.6, CI: 1.01, 2.38), and born in Mexico but with high levels of language acculturation (OR=2.5, CI: 1.19, 5.17).31 To further understand the role of genetics vs environment, we are currently investigating the associations of smoking, obesity, physical activity and selected socio-behavioural variables in relation to telomere length in peripheral blood DNA of over 13 000 participants.32
What can be done in the future?
Mano a Mano is a unique and large prospective cohort that provides a tremendous opportunity for future translational research on cancer and other chronic diseases in Mexican Americans. The rich resource of longitudinally collected questionnaire data and banked bio-specimens can be leveraged to address genetic susceptibility, molecular profiles and environmental exposures, as well as lifestyle and behavioural determinants underlying cancer risk relevant to Hispanic populations. Current follow-up allows immediate assessment of risk factors for cancer-predisposing conditions such as diabetes, obesity and insulin resistance syndrome, critically important health issues for this population. Assessment of the impact of acculturation on modifiable risk factors and behaviours such as physical activity and smoking can help inform risk reduction strategies. Recent efforts to explore genetic admixture and genetic susceptibility as they relate to obesity and comorbidities, as well as the inclusion of up to three members from some households, may provide unique opportunities to further disentangle the role of gene vs environment in disease risks. Finally, the Mano a Mano cohort should be an important component of consortium activities that focus on racial/ethnic differences in cancer risk, which would be highly valuable in engaging the broader research community, promoting collaboration and propelling discoveries.
What are the main strengths and weaknesses?
To our knowledge, this is the largest cohort of Mexican Americans with biological samples. The unique focus on first- and subsequent generation Mexican Americans, combined with the availability of biological samples to conduct translational research in this under-represented population, is likely to shed new light on viable targets for prevention of cancer and other chronic diseases. The inclusion of only Mexican Americans further minimizes potential biases from population stratification and from subtle differences in cultural and lifestyle practices even within the Hispanic community. Furthermore, the cohort participants are relatively young at the time of cohort enrolment (average age 40.8 years), providing a rare opportunity for prospectively assessing critical time periods of exposures in relation to subsequent risk of diseases.
Cohort members remain engaged in research efforts through annual telephone contact to update exposure information and to collect new data as needed. Self-reported cancer diagnoses are verified against records from the TCR and the diagnostic/treating hospitals. Additional cases are identified through linkage to the TCR, which allows for a relatively complete follow-up of incident cancers. In addition, we plan to link the cohort with the Texas vital statistics data and the National Death Index for passive follow-up of mortality and causes of death.
Some challenges are posed by the cohort. In an attempt to focus on underserved Mexican Americans, the cohort recruitment has traditionally been conducted in a narrow area of low socioeconomic status (SES). The resulting cohort population, although representative of Mexican Americans in the low SES study areas, is not representative of all Mexican Americans with regard to environmental exposures and lifestyle factors in the entire Houston metropolitan areas. To broaden the range and variation of environmental exposures and lifestyle practices and to enhance the generalizability of study findings, we are expanding cohort recruitment to the entire Houston metropolitan area.
Notwithstanding the rich data that we have collected, we have not yet collected comprehensive information on dietary practices. The lack of nutritional data limits our ability to assess the role of shifting dietary practices and energy balance in relation to disease risks. We have recently implemented a brief diet questionnaire (∼10–15 min) to be administered during usual telephone follow-up interviews. We are also piloting more comprehensive, web-based and self-administered assessments that can be completed by new cohort enrollees at baseline. These steps will bring us closer to eventually reaching the goal of characterizing dietary practices and obtaining reasonable estimates of total energy intake in cohort participants.
Can I get hold of data and where can I find more?
More details, including procedures to request data and biological samples for collaborative research, can be found at [www.mano-mano.us] or by e-mail to [manoamano@ MDAnderson.org].
Supplementary Data
Supplementary data are available at IJE online.
Funding
The Cohort receives funds collected pursuant to the Comprehensive Tobacco Settlement of 1998 and appropriated by the 76th Legislature to the University of Texas MD Anderson Cancer Center; from the Caroline W Law Fund for Cancer Prevention; and from the Dan Duncan Family Institute for Risk Assessment and Cancer Prevention. The funders did not contribute to the design or conduct of the study; the collection, analysis or interpretation of the data; or the preparation, review or approval of the manuscript.
Key Messages
This large Mexican American Cohort study, with detailed questionnaire and biological sample collection from first, second and subsequent generations of immigrants, provides a unique opportunity to shed light on the health issues of a minority US population in transition.
An important cohort finding is that increased acculturation (adoption of US lifestyle) is associated with health-related risk behaviours such as smoking, alcohol consumption and level of physical activity. Individuals with high acculturation scores, compared with those with low acculturation scores, had increased risk of obesity, diabetes and hypertension.
This cohort of relatively young adults (average age 40.8 years) provides an unparalleled opportunity to examine the role of early adulthood exposures and life-course events on subsequent disease risk. High participation rate in biological sample donation enhances opportunities for assessing the role of genetic susceptibility and gene-environment interactions in disease risk.
Supplementary Material
Acknowledgements
This study would not be possible without the generous support and cooperation of the participants, as well as the dedication of the Cohort study team. Their continued support is critical to the success of the study. The authors express their deep appreciation to Drs Margaret Spitz and Melissa Bondy of Baylor College of Medicine, for their early efforts on the cohort.
Conflict of interest: None declared.
References
- 1. US Census Bureau. US Census Bureau Projections Show a Slower Growing, Older, More Diverse Nation a Half Century from Now .2012. https://www.census.gov/newsroom/releases/archives/population/cb12-243.html(18 June 2014, date last accessed). [Google Scholar]
- 2. Ennis SR, Rios-Vargas M, Albert NG. The Hispanic Population: 2010. US Census Bureau; 2011. http://www.census.gov/prod/cen2010/briefs/c2010br-04.pdf (6 November 2014, date last accessed). [Google Scholar]
- 3. Houston Department of Health and Human Services. Hispanic Health Profile Houston/Harris County: Population Growth, Demographics, Chronic Disease and Health Disparities .2013. http://www.houstontx.gov/health/chs/HispanicHealthDep Booklet.pdf(6 November 2014, date last accessed). [Google Scholar]
- 4. Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA 2010;303:235–41. [DOI] [PubMed] [Google Scholar]
- 5. Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2014 .Atlanta, GA: US Department of Health and Human Services, 2014. [Google Scholar]
- 6. American Cancer Society. Cancer Facts & Figures for Hispanics/Latinos 2012-2014. 2012. http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-034778.pdf(28 July 2014, date last accessed). [Google Scholar]
- 7. Markides KS, Eschbach K. Ageing, migration, and mortality: current status of research on the Hispanic paradox. J Gerontol B Psychol Sci Soc Sci 2005;60:68–75. [DOI] [PubMed] [Google Scholar]
- 8. de, Heer HD, Wilkinson AV, Strong LL, Bondy ML, Koehly LM. Sitting time and health outcomes among Mexican origin adults: obesity as a mediator. BMC Public Health 2012;12:896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Guendelman SD, Ritterman-Weintraub ML, Fernald LCH, Kaufer-Horwitz M. Weight status of Mexican immigrant women: a comparison with women in Mexico and with US-born Mexican American women. Am J Public Health 2013;103:1634–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gorman BK, Read JG, Krueger PM. Gender, acculturation, and health among Mexican Americans. J Health Soc Behav 2010;51:440–57. [DOI] [PubMed] [Google Scholar]
- 11. Vermeesch AL, Stommel M. Physical activity and acculturation among U.S. Latinas of childbearing age. West J Nurs Res 2014;36:495–511. [DOI] [PubMed] [Google Scholar]
- 12. Zemore SE. Acculturation and alcohol among Latino adults in the United States: A comprehensive review. Alcohol Clin Exp Res 2007;31:1968–90. [DOI] [PubMed] [Google Scholar]
- 13. Pinheiro PS, Sherman RL, Trapido EJ et al. Cancer incidence in first generation U.S. Hispanics: Cubans, Mexicans, Puerto Ricans, and New Latinos. Cancer Epidemiol Biomarkers Prev 2009;18:2162–69. [DOI] [PubMed] [Google Scholar]
- 14. Siegel R, Naishadham D, Jemal A. Cancer statistics for Hispanics/Latinos, 2012. CA Cancer J Clin 2012;62:283–98. [DOI] [PubMed] [Google Scholar]
- 15. Jean RT, Wilkinson AV, Spitz MR, Prokhorov A, Bondy M, Forman MR. Psychosocial risk and correlates of early menarche in Mexican-American girls. Am J Epidemiol 2011;173:1203–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wilkinson AV, Shete S, Spitz MR, Swann AC. Sensation seeking, risk behaviours, and alcohol consumption among Mexican origin youth. J Adolesc Health 2011;48:65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hernández-Valero MA, Wilkinson AV, Forman MR et al. Maternal BMI and country of birth as indicators of childhood obesity in children of Mexican origin. Obesity (Silver Spring) 2007;15:2512–19. [DOI] [PubMed] [Google Scholar]
- 18. Fryar C, Hirsch R, Porter K, Kottiri B, Brody D, Louis T. Smoking and alcohol behaviours reported by adults, United States, 1999–2002. Adv Data Vital Health Stat. 2006;378 http://www.cdc.gov/nchs/data/ad/ad378.pdf(12 September 2014, date last accessed). [PubMed] [Google Scholar]
- 19. Centers for Disease Control and Prevention. Differences in prevalence of obesity among Black, White, and Hispanic Adults - United States, 2006-2008. MMWR 2009;58:740–44. [PubMed] [Google Scholar]
- 20. North American Association of Central Cancer Registries. US Registries Certified in 2013 for 2010 Incidence Data .2014. http://www.naaccr.org/Certification/USCert2010.aspx(7 August 2014, date last accessed). [Google Scholar]
- 21. Wilkinson AV, Waters AJ, Vasudevan V, Bondy ML, Prokhorov AV, Spitz MR. Correlates of susceptibility to smoking among Mexican origin youth residing in Houston, Texas: a cross-sectional analysis. BMC Public Health. 2008;8:337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wilkinson AV, Shete S, Vasudevan V, Prokhorov AV, Bondy ML, Spitz MR. Influence of subjective social status on the relationship between positive outcome expectations and experimentation with cigarettes. J Adolesc Health 2009;44:342–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Spelman AR, Spitz MR, Kelder SH et al. Cognitive susceptibility to smoking: Two paths to experimenting among Mexican origin youth.Cancer Epidemiol Biomarkers Prev 2009;18:3459–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wilkinson AV, Spitz MR, Prokhorov AV, Bondy ML, Shete S, Sargent JD. Exposure to smoking imagery in the movies and experimenting with cigarettes among Mexican heritage youth. Cancer Epidemiol Biomarkers Prev 2009;18:3435–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wilkinson AV, Bondy ML, Wu X et al. Cigarette experimentation in Mexican origin youth: psychosocial and genetic determinants. Cancer Epidemiol Biomarkers Prev 2012;21:228–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Prokhorov AV, Hudmon KS, Marani SK et al. Eliminating second-hand smoke from Mexican-American households: outcomes from Project Clean Air-Safe Air (CASA). Addict Behav 2013;38:1485–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Barcenas CH, Wilkinson AV, Strom SS et al. Birthplace, years of residence in the United States, and obesity among Mexican-American adults. Obesity (Silver Spring) 2007;15:1043–52. [DOI] [PubMed] [Google Scholar]
- 28. Strong LL, Anderson CB, Miranda PY et al. Gender differences in sociodemographic and behavioural influences of physical activity in Mexican-origin adolescents. J Phys Act Health 2012;9:829–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hu H, Huff C, Yamamura Y, Wu X, Strom X. Genetic Ancestry Associated With Obesity and Diabetes Risks in a Mexican-American Population From Houston, Texas. In: Proceedings of the 2014 American Society of Human Genetics Annual Conference; San Diego, CA: 2014. [Google Scholar]
- 30. Thelus JR, Bondy ML, Wilkinson AV, Forman MR. Pubertal development in Mexican American girls: the family's perspective. Qual Health Res 2009;19:1210–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Miranda PY, Wilkinson AV, Etzel CJ et al. Policy implications of early onset breast cancer among Mexican-origin women.Cancer 2011;117:390–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Han L, Zhao H, Strom S et al. Telomere length linking social contexts and cancer risk in Mexican Americans. American Association for Cancer Research Annual Meeting, San Diego, CA, 9 April 2014. Philadelphia, PA: AACR, 2014. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.