Abstract
Study objective
To assess the extent to which objective sleep patterns vary among U.S. Hispanics/Latinos.
Methods
We assessed objective sleep patterns in 2087 participants of the Hispanic Community Health Study/Study of Latinos from 6 Hispanic/Latino subgroups aged 18–64 years who underwent 7 days of wrist actigraphy.
Results
The age- and sex-standardized mean (SE) sleep duration was 6.82 (0.05), 6.72 (0.07), 6.61 (0.07), 6.59 (0.06), 6.57 (0.10), and 6.44 (0.09) hr among individuals of Mexican, Cuban, Dominican, Central American, Puerto Rican, and South American heritage, respectively. Sleep maintenance efficiency ranged from 89.2 (0.2)% in Mexicans to 86.5 (0.4)% in Puerto Ricans, while the sleep fragmentation index ranged from 19.7 (0.3)% in Mexicans to 24.2 (0.7)% in Puerto Ricans. In multivariable models adjusted for age, sex, season, socioeconomic status, lifestyle habits, and comorbidities, these differences persisted.
Conclusions
There are important differences in actigraphically measured sleep across U.S. Hispanic/Latino heritages. Individuals of Mexican heritage have longer and more consolidated sleep, while those of Puerto Rican heritage have shorter and more fragmented sleep. These differences may have clinically important effects on health outcomes.
Keywords: Hispanic/Latino, sleep, actigraphy
Statement of Significance
This manuscript reports on one of the largest assessments of objective sleep habits in a working-age population and is one of the first to focus on a diverse group of U.S. Hispanic/Latinos, for whom there is a lack of data on sleep patterns. Based on objective sleep data from wrist actigraphy, significant differences exist by ethnic heritage, and insufficient sleep is highly prevalent. Further research is needed to explore reasons behind these variations in sleep patterns and identify methods to improve the sleep health of U.S. Hispanics/Latinos.
INTRODUCTION
Poor sleep patterns are strongly linked to many adverse health outcomes, including metabolic and cardiovascular disease as well as premature mortality.1–4 Most population-based studies of sleep habits have relied on self-report of habitual sleep duration, which correlates poorly with objective measures.5–7 A focus on duration alone ignores other aspects of sleep such as sleep quality, timing, and regularity, despite growing evidence regarding the multidimensional nature of healthy sleep.8,9 Studies that have utilized an objective assessment of sleep have primarily focused on children and older adults, ignoring working-age populations, although this is often the age at which chronic disease develops. Additionally, this group faces particular challenges such as job and child care responsibilities that adversely impact healthy sleep patterns.10,11
There is also a lack of data on sleep patterns in U.S. Hispanics/Latinos, the largest minority group who represent over 16% of the U.S. population.12 Most of the existing research on sleep habits in U.S. Hispanic Americans has focused solely on those of Mexican heritage, yet it is clear that there are differences in health and behaviors—including self-reported sleep duration—across Hispanic/Latino ethnic backgrounds.13,14 Non-Mexican Hispanics may be at greater risk of short sleep,14,15 and differences in sleep may contribute to disparities between Hispanic/Latino groups in conditions such as diabetes and cardiovascular disease that have been associated with poor sleep patterns.16–18 Therefore, a better understanding of sleep patterns in a heterogeneous Hispanic/Latino population is critical to understanding how sleep may serve as a modifiable risk factor for disease. In this study, we sought to assess the multidimensional aspects of sleep patterns in a diverse group of community-dwelling Hispanics/Latinos using an objective, multinight assessment of sleep.
METHODS
Hispanic Community Health Study/Study of Latinos
The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) is a multicenter community-based cohort study examining prevalence and risk factors for chronic disease among Hispanic/Latino individuals. HCHS/SOL used a two-stage random probability-based sampling technique to randomly select household addresses based on census block groups within four cities (Bronx, NY; Miami, FL; Chicago, IL; and San Diego, CA) in order to provide a representative sample of the target population.19,20 A total of 16145 adults aged 18–74 years were recruited between May 2008 and June 2011. Participants provided information on demographics (including self-identified Hispanic/Latino background), socioeconomic status (including highest level of education attained and household income), lifestyle habits (including cigarette and alcohol use), and medical history through questionnaires administered at a study visit in either English or Spanish based on participant preference.19 As part of the baseline HCHS/SOL examination, subjects underwent unattended sleep apnea monitoring (ARES Unicorder 5.2;B-Alert, Carlsbad, CA) at home for one night and the apnea–hypopnea index (AHI) was calculated as a measure of sleep apnea severity.21,22
Sueño Ancillary Study
The Sueño ancillary study recruited 2189 HCHS/SOL participants aged 18–64 years free of severe obstructive sleep apnea (AHI < 50 events/hr and no treatment for sleep apnea) and narcolepsy from December 2010 to December 2013. Recruitment was limited to six Hispanic/Latino backgrounds (Central American, Cuban, Dominican, Puerto Rican, Mexican, and South American) with sampling at each site designed to ensure sufficient subjects from each background to allow comparisons across backgrounds. The study protocol was approved by the Institutional Review Boards at each of the participating sites and all participants provided written informed consent.
Sueño Study Protocol
At the Sueño visit, participants completed a battery of questionnaires including questions about employment status, work schedule, caffeine use, and use of sleep medications. Depressive symptoms were assessed using a 10-item version of the Center for Epidemiological Studies—Depression (CESD-10) questionnaire.23,24 Height and weight were measured and body mass index (BMI) calculated.
Actigraphy Data Collection
An Actiwatch Spectrum (Philips Respironics, Murrysville, PA) wrist actigraph was placed on the nondominant wrist and participants were asked to keep the device on the wrist continuously for 7 days with activity and light data collected in 30-second epochs. Participants also completed a sleep diary upon awakening each day. A centralized reading center in Boston, MA, scored all records. Rest periods where the participant was trying to sleep were identified following a standardized protocol that made use of event markers, sleep diaries, light exposure, and activity levels.25 Sleep–wake status for each 30-second epoch within each rest period was computed using the Actiware 5.59 scoring algorithm with sleep onset defined based on 5 immobile minutes, 0 immobile minutes for sleep offset, and a wake threshold of 40 counts. The scoring algorithm has been validated against polysomnography on an epoch-by-epoch basis.26–28 Participants with at least 5 days of valid actigraphy data were included for the analysis.
Actigraphy Measures
All sleep measures were reported as the mean averaged across all valid days in the recording. Habitual sleep duration was defined as the total amount of time scored as sleep during the main rest period, which was night for most participants, though for shift workers the main rest period may have occurred during the day. Insufficient sleep was defined as a mean of <7 hours of sleep/night in the main rest period.29 Sleep fragmentation index and sleep maintenance efficiency provide measures of sleep quality. The sleep fragmentation index is calculated as the sum of the proportion of all epochs from sleep onset to sleep offset with an activity count of 2 or greater and the proportion of all bouts of immobility (activity count less than 2 in every epoch) that were 1 minute or less in duration.25,30 Sleep maintenance efficiency is calculated as the proportion of time from sleep onset to sleep offset scored as sleep.
The interdaily stability index quantifies the regularity of sleep patterns across days and provides a measure of how stable sleep rhythms are from day to day.31,32 For this analysis, only participants with 7 consecutive days of valid actigraphy data (n = 1694) were used to derive the interdaily stability.
Sleep midpoint was defined as the midpoint between sleep onset and sleep offset. Naps were defined as a self-reported period of sleep (based on event markers or diary) outside the main rest period containing at least 15 minutes of actigraphically scored sleep. Napping was a dichotomous variable indicating whether or not there was >1 nap over the recording period.
Covariates
Covariates considered for inclusion were factors known to impact sleep based on prior large-scale research studies.15,25,33–35 Education level was dichotomized as <high school versus ≥high school diploma. Employment status was categorized as daytime worker/student, shift worker, homemaker/unemployed, and retired/disabled. Shift worker was defined as any participant regularly working at night, rotating, split, or irregular/on call shift. Annual household income was categorized as: <$20000, ≥$20000, and missing. BMI was categorized as <30.0 kg/m2, 30.0–39.9 kg/m2, and ≥40.0 kg/m2. Sleep apnea was categorized as AHI <5 events/hr, 5–14.9 events/hr, 15–29.9 events/hr, and 30–49.9 events/hr.36,37 A CESD-10 score ≥10 was used to define elevated depressive symptoms. Tobacco use was classified as current smoker, former smoker, or nonsmoker. Excessive alcohol use was defined as ≥7 drinks/week for women or ≥14 drinks/week for men based on the National Institute on Alcohol Abuse and Alcoholism definition of problem drinking.38,39 Caffeine intake was dichotomized as <3 cups/day versus ≥3 cups of caffeinated beverages consumed/day. Sleep medication was defined as any over-the-counter, herbal, or prescription medication used to aid with sleep and was categorized as <1, 1–2, 3–4, and ≥5 nights/week. Season of actigraphy collection was categorized into winter (January–March), spring (April–June), summer (July–September), and fall (October–December).
Model Building
Ethnic background was the exposure of interest in all models, and six sleep outcomes were modeled: nightly sleep duration, sleep fragmentation index, sleep maintenance efficiency, interdaily stability, sleep midpoint, and napping. For each of the six sleep outcomes, age- and sex-adjusted means were calculated, standardized to 2010 U.S. Census data. Multivariable models were then built for each of the six sleep outcomes using survey linear regression and including age, sex, educational level, employment status, income, obesity, sleep apnea, depressive symptoms, tobacco use, alcohol use, caffeine intake, sleeping medication use, and season as covariates. All analyses used complex survey procedures to account for cluster sampling, stratification, and sampling weights.11 Analysis of variance was used to test for differences among means and prevalences by ethnic background. If the null hypothesis of a common mean was rejected at p < .05, pairwise comparisons were performed using the Tukey–Kramer method to account for the multiple comparisons.
Because site and ethnic background are highly correlated, steps were taken to ensure site did not confound any differences in sleep outcomes attributed to ethnic background. We evaluated the potential for site to be a confounder by determining whether (1) site was associated with the sleep outcome (p for site ≤.15) in the multivariable model or (2) the inclusion of site in the multivariable model changed the beta coefficients for Hispanic/Latino background by ≥10%. This was done for each of the six sleep outcomes. If neither criterion was met, site was not considered a confounder and so not included as a covariate.
If either criterion was met, analyses were stratified by site to compute age- and sex-adjusted means. For multivariable analyses, a 10-level variable combining Hispanic/Latino background with site (Bronx-Dominican, Bronx-Puerto Rican, Chicago-Mexican, Chicago-Central American, Chicago-Puerto Rican, Chicago-South American, Miami-Central American, Miami-Cuban, Miami-South American, and San Diego-Mexican) was included in the models. A global F statistic was used to test the null hypothesis that all 10 levels had the same mean or prevalence. If this null hypothesis was rejected at p < .05, pairwise comparisons were performed within each site using the Tukey–Kramer method to account for multiple comparisons.
We tested for a sex by ethnic background interaction for all sleep outcomes in order to evaluate for effect modification by sex. In sensitivity analyses, we repeated all models after excluding shift workers (n = 297).
All p values were based on two-tailed testing. All analyses were completed using SAS v. 9.3 (SAS Institute, Cary, NC).
RESULTS
Of the 2189 participants in the Sueño ancillary study meeting eligibility criteria, 2156 (98%) had ≥5 days of valid actigraphy data. Covariate data were missing in 69 participants resulting in a sample size of 2087 for this analysis. Among the participants analyzed, the unweighted mean age (SD) was 46.9 (11.6) years, and 64.6% were women (Table 1). As expected, based on recruitment techniques, individuals of Mexican heritage comprised a smaller percentage of the study sample when compared to the overall HCHS/SOL cohort (26.9% vs. 40.5%), while all other ethnic backgrounds had increased representation (Supplemental Table 1).
Table 1.
Demographic and Lifestyle Characteristics of Participants in the Sueño Study.
| Overall, N = 2087 | Central American, N = 285 | Cuban, N = 378 | Dominican N = 261 | Mexican, N = 561 | Puerto Rican, N = 431 | South American, N = 171 | |
|---|---|---|---|---|---|---|---|
| Age, years | 46.9 (11.6) | 46.1 (11.3) | 48.1 (10.8) | 46.5 (12.1) | 45.7 (11.6) | 48.2 (11.8) | 47.0 (11.9) |
| Female | 64.6% | 66.0% | 57.9% | 71.3% | 65.2% | 64.3% | 66.1% |
| High school diploma | 70.6% | 69.2% | 83.2% | 65.3% | 63.7% | 71.9% | 86.6% |
| Employed | 63.0% | 77.1% | 67.7% | 51.2% | 70.9% | 44.0% | 77.9% |
| Household yearly income <$20000 | 43.5% | 45.9% | 44.6% | 54.8% | 34.9% | 51.5% | 35.9% |
| Body mass index ≥30.0 kg/m2 | 41.4% | 37.9% | 34.0% | 42.0% | 38.7% | 56.7% | 30.0% |
| Apnea hypopnea index ≥5.0 events/hr | 22.6% | 21.4% | 21.7% | 22.5% | 25.1% | 19.2% | 22.0% |
| Depressive symptomsa | 28.2% | 20.7% | 27.3% | 32.9% | 24.0% | 36.7% | 25.3% |
| Current/former tobacco use | 17.7% | 11.8% | 16.9% | 14.1% | 22.3% | 14.0% | 18.6% |
| High level of alcohol useb | 5.9% | 9.1% | 4.9% | 7.1% | 4.7% | 7.3% | 5.7% |
| Caffeine, drinks/day ≥3 | 35.0% | 36.2% | 41.0% | 34.3% | 29.1% | 39.7% | 35.8% |
| Sleep aids use, nights/week ≥1 | 13.4% | 11.2% | 18.9% | 11.7% | 7.6% | 21.4% | 6.5% |
All shown as mean (SD) or percentage, adjusted for age and sex standardized to the 2010 U.S. Census distributions (except age and sex).
Depressive symptoms defined as a score of 10 or greater on the 10-item Center for Epidemiological Studies—Depressive questionnaire.
High level of alcohol use defined as ≥7 drinks/week for women or ≥14 drinks/week for men based on the National Institute on Alcohol Abuse and Alcoholism definition of problem drinking.
Overall, the prevalence of insufficient sleep, classified as <7 hours per night, was high. The age- and sex-adjusted prevalence varied by background: 63.2% in individuals of Central American heritage, 60.1% in individuals of Cuban heritage, 69.5% in individuals of Dominican heritage, 54.6% in individuals of Mexican heritage, 61.7% in individuals of Puerto Rican heritage, and 67.0% in individuals of South American heritage.
For nightly sleep duration, sleep fragmentation index, sleep maintenance efficiency, and interdaily stability, there was no evidence of confounding by site. In age- and sex-adjusted analyses, mean nightly sleep duration differed by as much as 23 minutes across Hispanic/Latino backgrounds (global p < .01). Individuals of Mexican heritage had the longest habitual sleep duration with a mean (SE) of 6.82 (0.05) hours, while those of South American heritage had the shortest sleep duration of 6.44 (0.09) hours followed by those of Puerto Rican heritage at 6.57 (0.10) hours and those of Central American heritage at 6.59 (0.06) hours (Table 2). In multivariable analyses, these differences persisted (Table 3). Compared to individuals of Mexican heritage, sleep duration was 19 minutes (95% confidence interval [CI] = 6 to 33) shorter per night in those of South American heritage, 13 minutes (95% CI = 3 to 23) shorter in those of Central American heritage, and 12 minutes (95% CI = −1 to 26) shorter in those of Puerto Rican heritage.
Table 2.
Age- and Sex-Adjusted Sleep Outcomes by Hispanic/Latino Heritage, Sueño Study (N = 2087).
| Central American, Mean (SE) | Cuban, Mean (SE) | Dominican, Mean (SE) | Mexican, Mean (SE) | Puerto Rican, Mean (SE) | South American, Mean (SE) | p | |
|---|---|---|---|---|---|---|---|
| Sleep duration, hours | 6.59 (0.06)a | 6.72 (0.07)b | 6.61 (0.07)a | 6.82 (0.05)b,c,d,e | 6.57 (0.10)a | 6.44 (0.09)a,f | <.01 |
| Sleep fragmentation index, % | 21.8 (0.6)a,e | 22.4 (0.6)a,e | 23.0 (0.5)a,b | 19.7 (0.3)c,d,e,f | 24.2 (0.7)a,b,c,f | 21.0 (0.8)d,e | <.01 |
| Sleep maintenance efficiency, % | 88.3 (0.3)a,e | 88.4 (0.4)a,e | 87.5 (0.4)a | 89.2 (0.2)c,d,e,f | 86.5 (0.4)a,b,c,f | 88.3 (0.5)e | <.01 |
| Inter-daily stabilityg | 0.54 (0.01)e | 0.55 (0.01)d | 0.52 (0.01)f | 0.54 (0.01)e | 0.50 (0.01)a,b,c,f | 0.54 (0.01)e | <.01 |
Mean and standard error are shown adjusted for age and sex, standardized to the 2010 U.S. Census distributions and accounting for sampling methods; P is for global F statistic. Subscript letters a–f indicate significant differences in means, by Tukey–Kramer pairwise comparison (p < .05).
Significantly different from Mexican.
Significantly different from South American.
Significantly different from Central American.
Significantly different from Dominican.
Significantly different from Puerto Rican.
Significantly different from Cuban.
N = 1694 for interdaily stability analyses.
Table 3.
Regression Coefficients for Sleep Outcomes by Hispanic/Latino Heritage, Sueño Study (N = 2087).
| Central American, beta (SE) | Cuban, beta (SE) | Dominican, beta (SE) | Mexican, beta (SE) | Puerto Rican, beta (SE) | South American, beta (SE) | p value | |
|---|---|---|---|---|---|---|---|
| Sleep duration, minutes | −13.2 (5.2)a | −5.2 (4.9) | −10.5 (5.1)a | 0.0 (0.0)b,c,d | −12.4 (6.7) | −19.3 (6.7)a | .02 |
| Sleep fragmentation index, % | 2.1 (0.7)a | 2.5 (0.7)a | 2.5 (0.6)a | 0.0 (0.0)c,d,e,f | 3.4 (0.7)a | 1.7 (0.9) | <.01 |
| Sleep maintenance efficiency, % | −1.0 (0.4)a | −0.7 (0.4)e | −1.2 (0.4)a | 0.0 (0.0)b,c,d,e | −2.0 (0.5)a,f | −1.3 (0.6)a | <.01 |
| Inter-daily stability, %* | −0.01 (0.01) | 0.01 (0.01)d,e | −0.02 (0.01)f | 0.0 (0.0)e | −0.03 (0.01)a,b,f | 0.00 (0.01)e | .048 |
Regression coefficients are taken from a multivariable model with Mexicans serving as the reference group, including age, sex, education, employment, income, body mass index, apnea–hypopnea index, depressive symptoms, tobacco use, alcohol use, caffeine intake, sleep medication usage, and season as covariates and accounting for sampling methods. p Value is for testing the null hypothesis of a common mean across groups. Subscript letters a–e indicate significant differences in means, by Tukey–Kramer pairwise comparison (p < .05).
Significantly different from Mexican.
Significantly different from South American.
Significantly different from Central American.
Significantly different from Dominican.
Significantly different from Puerto Rican.
Significantly different from Cuban.
N = 1694 for inter-daily stability analyses.
The mean sleep fragmentation index was lowest among individuals of Mexican heritage at 19.7% (0.3%) and highest among those of Puerto Rican heritage at 24.2% (0.7%). In multivariable analyses, the sleep fragmentation index remained 3.4% (95% CI = 2.0% to 4.8%) greater in those of Puerto Rican compared to Mexican heritage. A similar pattern was seen for sleep maintenance efficiency, where individuals of Mexican heritage had the highest mean sleep maintenance efficiency at 89.2% (0.2%) and those of Puerto Rican heritage had the lowest sleep maintenance efficiency at 86.5% (0.4%). In multivariable analyses, the difference in mean sleep maintenance efficiency was 2.0% (95% CI = 1.0% to 2.9%) between those of Mexican and Puerto Rican heritages. Inter-daily stability was lowest among individuals of Puerto Rican heritage at 0.50 (0.01) when contrasted to individuals of Central American, Cuban, Mexican, and South American heritages for which mean (SE) was 0.54 (0.01), 0.55 (0.01), 0.54 (0.01), and 0.54 (0.01), respectively. In multivariable analyses, a similar pattern to other sleep measures of quality was observed, with the largest contrast of 0.03 (95% CI = −0.07 to 0.01) between individuals of Mexican and Puerto Rican heritage.
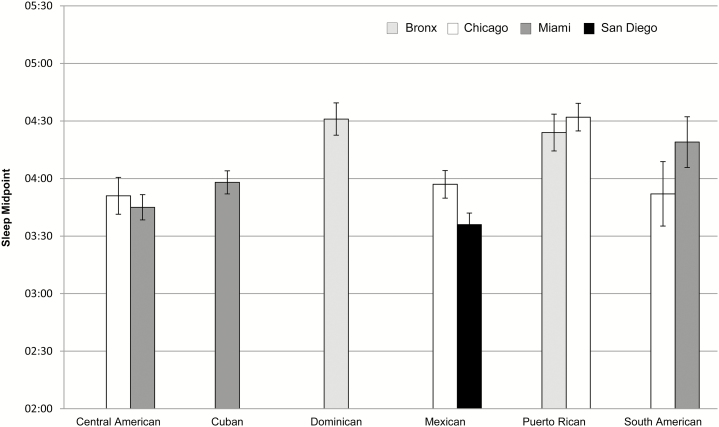
Because site was found to potentially confound the ethnicity associations with sleep midpoint (Figure 1) and napping, analyses were stratified by site. Within the Chicago site, mean sleep midpoint was later in individuals of Puerto Rican heritage (04:32) when compared to individuals of Central American (03:51) and Mexican heritage (03:57). In Miami, the sleep midpoint for individuals of Central American heritage (04:19) was later than individuals of South American heritage (03:45). In multivariable analyses, the sleep midpoint for individuals of Puerto Rican heritage in Chicago remained 29 (95% CI = 5 to 53) minutes later than those of Mexican heritage and 35 (95% CI = 9 to 61) minutes later than those of Central American heritage at that site. The overall prevalence of napping ranged from 19.0% (<0.01%) among individuals of Mexican heritage in San Diego to 34.7% (0.1%) among individuals of Central American heritage in Chicago. There were no differences across ethnic heritages (global p value >.05).
Figure 1.
Age- and sex-adjusted sleep midpoint by Hispanic/Latino heritage, Sueño Study (N = 2087). Mean and standard error (bars) are shown adjusted for age and sex, standardized to the 2010 U.S. Census and accounting for sampling methods. In Miami, there was a mean (95% confidence interval) 34 (15, 82)-minute difference between individuals of Central and South American heritage. In Chicago, there was a 42 (4, 87)-minute difference between midpoints of individuals of Puerto Rican and Central American heritage and 35 (4, 73)-minute difference between midpoints of individuals of Puerto Rican and Mexican heritage.
There was no evidence for heterogeneity by sex in ethnic differences for any of the six sleep outcomes. In addition, sensitivity analyses excluding shift workers did not substantially change any of the reported findings.
DISCUSSION
This work represents one of the largest assessments to date of objective sleep habits in a working-age population. The factors that determine sleep in this age-group are distinctly different from those of children and older adults. In particular, competing time demands from job, child care, and family responsibilities can contribute to sleep insufficiency.10,11 This is also one of the first studies to focus on objective sleep in Hispanic/Latino individuals, a population at high risk of diseases linked to poor sleep.
We found that mean sleep duration was over 30 minutes longer than in non-Hispanic whites and blacks participating in the Coronary Artery Risk Development in Young Adults (CARDIA) study, which used similar actigraphy software, although the protocol was not identical.40 While we are unable to comment on a direct comparison to non-Hispanic groups, our results are consistent with a lower prevalence of self-reported insufficient sleep among U.S. Hispanics/Latinos.41,42 However, of note, insufficient sleep was still highly prevalent. A majority of working-age U.S. Hispanic/Latino adults sleep less than the recommended 7 hours per night,29 ranging from 54.6% in individuals of Mexican heritage to 69.5% among individuals of Dominican heritage. Napping was also relatively common at roughly 25%. In addition, the sleep midpoint data, with group means ranging from 3:36 a.m. to 4:32 a.m., suggest a relatively late bedtime may be a contributor to short sleep durations.
Using objective assessments, we have demonstrated that important differences in sleep patterns exist by Hispanic/Latino background. Individuals of Mexican heritage had the most optimal sleep habits including the longest sleep duration, most consolidated sleep, higher regularity, and an earlier sleep midpoint. In contrast, sleep in individuals of Puerto Rican heritage was characterized by shorter sleep duration, the most fragmented sleep, a later sleep midpoint, and lower regularity. Individuals of South American heritage had the shortest sleep duration, while those of Dominican heritage had a relatively late sleep midpoint.
Differences in sleep patterns across Hispanic/Latino backgrounds may have important health implications. Sleep insufficiency is an independent risk factor for obesity, hypertension, and diabetes,1,43–45 all of which are more common among individuals of Puerto Rican heritage.46–49 Each hour reduction in sleep duration is associated with a 0.35 kg/m2 increase in BMI and a 37% increase in odds of incident hypertension.50,51 Even a 20-minute difference in nightly sleep over the course of a week has clinically important effects on attention and vigilance.52,53 Thus, the 13-minute difference observed between individuals of Mexican and Puerto Rican heritage and 19-minute difference between those of Mexican and South American heritage likely represent clinically meaningful differences. Differences in sleep quality, as assessed by fragmentation and maintenance efficiency, may also have important health consequences.
Our findings are consistent with surveys of self-reported sleep observing increased odds of long sleep duration among U.S. Hispanics of Mexican heritage and short sleep duration among U.S. Hispanics of non-Mexican heritage.14 Individuals of Puerto Rican heritage in our cohort live in the mainland United States; however, our findings are consistent with prior work reporting a high rate of insufficient sleep in Puerto Rico compared to the mainland United States.41 The causes of greater sleep insufficiency among individuals of Puerto Rican heritage are unknown. Those of Puerto Rican heritage have higher rates of depression and anxiety, both of which are associated with poor sleep.54–56 However, the disparity in individuals of Puerto Rican heritage persisted after adjusting for depressive symptoms. Further evaluation of other factors influencing sleep such as employment type, social support, home environment, acculturation stress as well as knowledge and attitudes about healthy sleep across Hispanic backgrounds is needed to better understand the source of the differences observed.57–60
This study has several strengths. A formalized algorithm was used to minimize actigraphy scoring variability.25 Additionally, the inclusion of at least 5 days of actigraphy, including weekend/nonwork days, increases the likelihood that sleep patterns observed are representative of habitual sleep. Elements of sleep beyond duration were also captured, including regularity, and quality, which provides for a richer description of sleep patterns.
There are several limitations that should be noted. Although polysomnography is the gold standard for objectively characterizing sleep, use of this technique is not feasible in large study samples, and it does not assess habitual sleep patterns over multiple nights. Sleep duration, sleep maintenance efficiency, and sleep timing from actigraphy have been characterized on an epoch-by-epoch basis with good correlation to polysomonography-based sleep metrics.27,40,50,61,62 However, detection of napping behavior by actigraphy may be limited due to inability to fully discriminate between quiet wakefulness and sleep and we are unable to distinguish whether these naps were planned or from inability to maintain wakefulness. The correlation of ethnic background with site limited our ability to some extent in drawing conclusions about cross-ethnic differences. Additionally, although data from other cohorts suggests the magnitude of sleep differences observed here may have important health consequences,50–53 we are unable to assess the longitudinal relationship with clinical outcomes at this time. Finally, although this study included multiple sites, our findings may not be generalizable to all Hispanic/Latinos living in the United States, including nonurban areas. Nevertheless, these sites are among cities with the highest Hispanic/Latino populations in the United States and represent a diverse collection of ethnic heritages.12
This one of is the largest studies of objective sleep patterns in a working-age population and to focus on Hispanic/Latino individuals. Sleep insufficiency was found to be highly prevalent although important differences exist by Hispanic/Latino background. Individuals of Mexican heritage have the healthiest sleep habits, particularly when compared to those of Puerto Rican heritage. Further research is needed to determine whether the observed differences in sleep may partially explain disparities in cardiovascular and metabolic diseases known to exist by Hispanic/Latino background. Additional research is also needed to explore the reasons behind these sleep differences and identify opportunities to improve the sleep health of U.S. Hispanics/Latinos.
SUPPLEMENTARY MATERIAL
Supplementary Material is available at Sleep online.
LOCATION OF STUDY
Field sites in Bronx, NY, Chicago, IL, Miami, FL, and San Diego, CA. Coordinating center in Boston, MA.
FINANCIAL SUPPORT
This study was supported by NHLBI HL098297, HL007901, and HL124767. In addition, the Hispanic Community Health Study/Study of Latinos was carried out as a collaborative study supported by contracts from NHLBI to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). The following Institutes/Center/Offices contribute to the HCHS/SOL through a transfer of funds to the NHLBI: National Center on Minority Health and Health Disparities, the National Institute of Deafness and Other Communications Disorders, the National Institute of Dental and Craniofacial Research, the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of Neurological Disorders and Stroke, and the Office of Dietary Supplements.
DISCLOSURE STATEMENT
Material has been reviewed by the Walter Reed Army Institute of Research. There is no objection to its presentation and/or publication. The opinions or assertions contained herein are the private views of the author, and are not to be construed as official, or as reflecting true views of the Department of the Army or the Department of Defense.
Supplementary Material
REFERENCES
- 1. Ayas NT White DP Al-Delaimy WK, et al. . A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care. 2003; 26(2): 380–384. [DOI] [PubMed] [Google Scholar]
- 2. Ayas NT White DP Manson JE, et al. . A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003; 163(2): 205–209. [DOI] [PubMed] [Google Scholar]
- 3. Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring). 2008; 16(3): 643–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2010; 33(2): 414–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Van Den Berg JF Van Rooij FJ Vos H, et al. . Disagreement between subjective and actigraphic measures of sleep duration in a population-based study of elderly persons. J Sleep Res. 2008; 17(3): 295–302. [DOI] [PubMed] [Google Scholar]
- 6. Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: how similar are they?Epidemiology. 2008; 19(6): 838–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Girschik J, Fritschi L, Heyworth J, Waters F. Validation of self-reported sleep against actigraphy. J Epidemiol. 2012; 22(5): 462–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Czeisler CA. Duration, timing and quality of sleep are each vital for health, performance and safety. Sleep Health. 2015; 1(1): 5– 8. [DOI] [PubMed] [Google Scholar]
- 9. Buysse DJ. Sleep health: can we define it? Does it matter?Sleep. 2014; 37(1): 9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Basner M, Spaeth AM, Dinges DF. Sociodemographic characteristics and waking activities and their role in the timing and duration of sleep. Sleep. 2014; 37(12): 1889–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Patel SR Sotres-Alvarez D Castañeda SF, et al. . Social and Health Correlates of Sleep Duration in a US Hispanic Population: Results from the Hispanic Community Health Study/Study of Latinos. Sleep. 2015; 38(10): 1515–1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. U.S. Census Bureau. The Hispanic population: 2010. 2010 Census Briefs2011. Available at www.census/gov/prod/cen2010/briefs/c2010br-04.pdf, accessed August 3, 2015
- 13. Morales LS, Lara M, Kington RS, Valdez RO, Escarce JJ. Socioeconomic, cultural, and behavioral factors affecting Hispanic health outcomes. J Health Care Poor Underserved. 2002; 13(4): 477–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hale L, Do DP. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007; 30(9): 1096–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Stamatakis KA, Kaplan GA, Roberts RE. Short sleep duration across income, education, and race/ethnic groups: population prevalence and growing disparities during 34 years of follow-up. Ann Epidemiol. 2007; 17(12): 948–955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Schneiderman N Llabre M Cowie CC, et al. . Prevalence of diabetes among Hispanics/Latinos from diverse backgrounds: the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Diabetes Care. 2014; 37(8): 2233–2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Heiss G Snyder ML Teng Y, et al. . Prevalence of metabolic syndrome among Hispanics/Latinos of diverse background: the Hispanic Community Health Study/Study of Latinos. Diabetes Care. 2014; 37(8): 2391–2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Daviglus ML Talavera GA Avilés-Santa ML, et al. . Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012; 308(17): 1775–1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lavange LM Kalsbeek WD Sorlie PD, et al. . Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010; 20(8): 642–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sorlie PD Avilés-Santa LM Wassertheil-Smoller S, et al. . Design and implementation of the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010; 20(8): 629–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Redline S Sotres-Alvarez D Loredo J, et al. . Sleep-disordered breathing in Hispanic/Latino individuals of diverse backgrounds. The Hispanic Community Health Study/Study of Latinos. Am J Respir Crit Care Med. 2014; 189(3): 335–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Westbrook PR Levendowski DJ Cvetinovic M, et al. . Description and validation of the apnea risk evaluation system: a novel method to diagnose sleep apnea-hypopnea in the home. Chest. 2005; 128(4): 2166–2175. [DOI] [PubMed] [Google Scholar]
- 23. Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. 1994; 10(2): 77–84. [PubMed] [Google Scholar]
- 24. Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Measure. 1977; 1(3): 385–401. [Google Scholar]
- 25. Patel SR Weng J Rueschman M, et al. . Reproducibility of a Standardized Actigraphy Scoring Algorithm for Sleep in a US Hispanic/Latino Population. Sleep. 2015; 38(9): 1497–1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kushida CA, Chang A, Gadkary C, Guilleminault C, Carrillo O, Dement WC. Comparison of actigraphic, polysomnographic, and subjective assessment of sleep parameters in sleep-disordered patients. Sleep Med. 2001; 2(5): 389–396. [DOI] [PubMed] [Google Scholar]
- 27. Marino M Li Y Rueschman MN, et al. . Measuring sleep: accuracy, sensitivity, and specificity of wrist actigraphy compared to polysomnography. Sleep. 2013; 36(11): 1747–1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Oakley NR. Validation with polysomnography of the sleep-watch sleep/wake scoring algorithm used by the actiwatch activity monitoring system. Bend, Oregon:Technical Report to Mini Mitter Co, Inc; 1997. [Google Scholar]
- 29. Watson NF Badr MS Belenky G, et al. . Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015; 38(6): 843–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kurina LM, Knutson KL, Hawkley LC, Cacioppo JT, Lauderdale DS, Ober C. Loneliness is associated with sleep fragmentation in a communal society. Sleep. 2011; 34(11): 1519–1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Van Someren EJ, Swaab DF, Colenda CC, Cohen W, McCall WV, Rosenquist PB. Bright light therapy: improved sensitivity to its effects on rest-activity rhythms in Alzheimer patients by application of nonparametric methods. Chronobiol Int. 1999; 16(4): 505–518. [DOI] [PubMed] [Google Scholar]
- 32. Luik AI, Zuurbier LA, Hofman A, Van Someren EJ, Tiemeier H. Stability and fragmentation of the activity rhythm across the sleep-wake cycle: the importance of age, lifestyle, and mental health. Chronobiol Int. 2013; 30(10): 1223–1230. [DOI] [PubMed] [Google Scholar]
- 33. Patel SR, Malhotra A, Gottlieb DJ, White DP, Hu FB. Correlates of long sleep duration. Sleep. 2006; 29(7): 881–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Thorleifsdottir B, Björnsson JK, Benediktsdottir B, Gislason T, Kristbjarnarson H. Sleep and sleep habits from childhood to young adulthood over a 10-year period. J Psychosom Res. 2002; 53(1): 529–537. [DOI] [PubMed] [Google Scholar]
- 35. Hjorth MF, Chaput JP, Michaelsen K, Astrup A, Tetens I, Sjödin A. Seasonal variation in objectively measured physical activity, sedentary time, cardio-respiratory fitness and sleep duration among 8-11 year-old Danish children: a repeated-measures study. BMC Public Health. 2013; 13: 808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Epstein LJ Kristo D Strollo PJ Jr, et al. . Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5(3):263–276. [PMC free article] [PubMed] [Google Scholar]
- 37. Iber C, Ancoli-Israel S, Chesson A, Jr, Quan S; for the American Academy of Sleep Medicine. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. 1st ed. Westchester, IL: American Academy of Sleep Medicine; 2007. [Google Scholar]
- 38. Center for Disease Control and Prevention. Alcohol use and health. Alcohol use and health Web site. Centers for Disease Control and Prevention. Alcohol use and health. Available at: http://www.cdc.gov/alcohol/fact-sheets/alcohol-use.htm Updated 2014. Accessed April 28, 2015
- 39. Dawson DA. Defining risk drinking. Alcohol Res Health. 2011; 34(2): 144–156. [PMC free article] [PubMed] [Google Scholar]
- 40. Lauderdale DS Knutson KL Yan LL, et al. . Objectively measured sleep characteristics among early-middle-aged adults: the CARDIA study. Am J Epidemiol. 2006; 164(1): 5–16. [DOI] [PubMed] [Google Scholar]
- 41. Centers for Disease Control and Prevention. Perceived insufficient rest or sleep among adults - United States, 2008. MMWR Morb Mortal Wkly Rep. 2009; 58(42): 1175–1179. [PubMed] [Google Scholar]
- 42. Strine TW, Chapman DP. Associations of frequent sleep insufficiency with health-related quality of life and health behaviors. Sleep Med. 2005; 6(1): 23–27. [DOI] [PubMed] [Google Scholar]
- 43. van den Berg JF Knvistingh Neven A Tulen JH, et al. . Actigraphic sleep duration and fragmentation are related to obesity in the elderly: the Rotterdam Study. Int J Obes (Lond). 2008; 32(7): 1083–1090. [DOI] [PubMed] [Google Scholar]
- 44. Knutson KL, Ryden AM, Mander BA, Van Cauter E. Role of sleep duration and quality in the risk and severity of type 2 diabetes mellitus. Arch Intern Med. 2006; 166(16): 1768–1774. [DOI] [PubMed] [Google Scholar]
- 45. Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB. Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep. 2005; 28(10): 1289–1296. [DOI] [PubMed] [Google Scholar]
- 46. Pérez CM, Soto-Salgado M, Suárez E, Guzmán M, Ortiz AP. High Prevalence of Diabetes and Prediabetes and Their Coexistence with Cardiovascular Risk Factors in a Hispanic Community. J Immigr Minor Health. 2015; 17(4): 1002–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Pabon-Nau LP, Cohen A, Meigs JB, Grant RW. Hypertension and diabetes prevalence among U.S. Hispanics by country of origin: the National Health Interview Survey 2000-2005. J Gen Intern Med. 2010; 25(8): 847–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Ho GY Qian H Kim MY, et al. . Health disparities between island and mainland Puerto Ricans. Rev Panam Salud Publica. 2006; 19(5): 331–339. [DOI] [PubMed] [Google Scholar]
- 49. Smith CA, Barnett E. Diabetes-related mortality among Mexican Americans, Puerto Ricans, and Cuban Americans in the United States. Rev Panam Salud Publica. 2005; 18(6): 381–387. [DOI] [PubMed] [Google Scholar]
- 50. Knutson KL Van Cauter E Rathouz PJ, et al. . Association between sleep and blood pressure in midlife: the CARDIA sleep study. Arch Intern Med. 2009; 169(11): 1055–1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Knutson KL. Sleep duration and cardiometabolic risk: a review of the epidemiologic evidence. Best Pract Res Clin Endocrinol Metab. 2010; 24(5): 731–743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Mollicone DJ, Van Dongen HP, Rogers NL, Banks S, Dinges DF. Time of day effects on neurobehavioral performance during chronic sleep restriction. Aviat Space Environ Med. 2010; 81(8): 735–744. [DOI] [PubMed] [Google Scholar]
- 53. Mollicone DJ, Van Dongen HP, Rogers NL, Dinges DF. Response Surface Mapping of Neurobehavioral Performance: Testing the Feasibility of Split Sleep Schedules for Space Operations. Acta Astronaut. 2008; 63(7-10)(7-10): 833–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Alegria M, Canino G, Stinson FS, Grant BF. Nativity and DSM-IV psychiatric disorders among Puerto Ricans, Cuban Americans, and non-Latino Whites in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2006; 67(1): 56–65. [DOI] [PubMed] [Google Scholar]
- 55. Alegría M, Mulvaney-Day N, Torres M, Polo A, Cao Z, Canino G. Prevalence of psychiatric disorders across Latino subgroups in the United States. Am J Public Health. 2007; 97(1): 68–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Alegría M Canino G Shrout PE, et al. . Prevalence of mental illness in immigrant and non-immigrant U.S. Latino groups. Am J Psychiatry. 2008; 165(3): 359–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Schachter FF, Fuchs ML, Bijur PE, Stone RK. Cosleeping and sleep problems in Hispanic-American urban young children. Pediatrics. 1989; 84(3): 522–530. [PubMed] [Google Scholar]
- 58. Burnam MA, Hough RL, Karno M, Escobar JI, Telles CA. Acculturation and lifetime prevalence of psychiatric disorders among Mexican Americans in Los Angeles. J Health Soc Behav. 1987; 28(1): 89–102. [PubMed] [Google Scholar]
- 59. Wells KB, Golding JM, Hough RL, Burnam MA, Karno M. Acculturation and the probability of use of health services by Mexican Americans. Health Serv Res. 1989; 24(2): 237–257. [PMC free article] [PubMed] [Google Scholar]
- 60. Jerant A, Arellanes R, Franks P. Health status among US Hispanics: ethnic variation, nativity, and language moderation. Med Care. 2008; 46(7): 709–717. [DOI] [PubMed] [Google Scholar]
- 61. Lauderdale DS, Knutson KL, Rathouz PJ, Yan LL, Hulley SB, Liu K. Cross-sectional and longitudinal associations between objectively measured sleep duration and body mass index: the CARDIA Sleep Study. Am J Epidemiol. 2009; 170(7): 805–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Blackwell T Redline S Ancoli-Israel S, et al. ; Study of Osteoporotic Fractures Research Group. Comparison of sleep parameters from actigraphy and polysomnography in older women: the SOF study. Sleep. 2008; 31(2): 283–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.