Abstract
PURPOSE:
To evaluate whether cerclage in twins reduces the rate of spontaneous preterm birth < 32 weeks when compared to expectant management.
METHODS:
This is a retrospective cohort study of twin pregnancies with the following indications for cerclage from two institutions: history of prior preterm birth, ultrasound-identified short cervix ≤2.5 cm, and cervical dilation ≥1.0 cm. The “cerclage” cohort received a cerclage from a single provider at a single institution from 2003–2016. The “no cerclage” group included all patients with similar indications that were expectantly managed from 2010–2015, at a second institution where cerclages are routinely not performed in twin pregnancies. The primary outcome was the rate of spontaneous preterm birth at <32 weeks. Secondary outcomes were the rates of spontaneous and overall (including medically-indicated) preterm births at <32 weeks, <34 weeks, and <36 weeks, chorioamnionitis, birth weight, and neonatal mortality within 30 days of life. We also performed a planned subgroup analysis stratified by cerclage indication.
RESULTS:
In all, 135 women were included in two cohorts: cerclage (n=96) or no cerclage (n=39). The rates of spontaneous preterm birth <32 weeks were 10.4% (n=10) with cerclage vs. 28.2% (n=11) without cerclage (OR 0.23, CI 0.08–0.70, p=0.017). After adjusting for cerclage indication, clinical history, age, chorionicity, insurance type, race, BMI, in-vitro fertilization, and multifetal reduction, there remained a significant reduction in the cerclage group of spontaneous preterm birth <32 weeks (aOR 0.24, CI 0.06–0.90, p=0.035), spontaneous preterm birth <36 weeks (aOR 0.34, CI 0.04–0.81, p=0.013) as well as in overall preterm birth < 32 weeks (aOR 0.31, CI 0.1–0.86, p=0.018) and overall preterm birth <36 weeks (aOR 0.37, CI 0.10–0.84, p=0.030). When stratified by short cervix or cervical dilation in the cerclage vs. no cerclage groups, there was a significant decrease in spontaneous preterm birth <32 weeks in the cerclage group with cervical dilation (11.1% vs. 41.2%, p=0.01) but not in the cerclage group with short cervix only, even for cervical length <1.5 cm. Pregnancy latency was 91 days in the cerclage group vs. 57 days in the no cerclage group (p=0.001), with a median gestational age at delivery of 35 vs. 32 weeks (p=0.002). There was no increase in chorioamnionitis in the cerclage group. Furthermore, there was a significant increase in birth weight (median 2278g vs. 1665g, p<0.001) and decrease in perinatal death <30 days (1.6% vs. 12.9%, p=0.001).
CONCLUSIONS:
Cerclage in twin pregnancies significantly decreased the rate of spontaneous preterm birth <32 weeks compared to expectant management. However, when stratified by cerclage indication, this decrease in primary outcome only remained significant in the group with cervical dilation.
Keywords: prematurity, multiple gestation, rescue, short cervix, cervical insufficiency
Introduction:
Preterm birth (PTB) is a major source of morbidity and mortality, and this problem is amplified in cases of multiple gestation. Twin pregnancies have a 12 times higher risk for PTB than singleton pregnancies.1 In 2013, the U.S. birth rate before 32 weeks was 11.3% for twins vs. 1.5% for singletons.1 Our current armamentarium to prevent PTB is limited, particularly in multiple gestations. While widely accepted in singleton pregnancies, the use of cervical cerclage has been a source of great controversy in twin pregnancies.
There are three indications for cerclage: history-indicated, ultrasound-indicated, and physical-exam indicated cerclage.2,3 A Cochrane review of cerclage in multiple gestations assessed two randomized control trials (RCT) (n=73 women) with history-indicated cerclage and three RCTs with ultrasound-indicated cerclage,4–6 and found cerclage did not decrease PTBs less than 34 weeks, perinatal death, or serious neonatal morbidity.7 A retrospective review by Roman et al. in 2005 reviewed 414 twin gestations and 92 triplet gestations with short cervix (<2.5 cm), and compared cerclage vs. bed rest.8 There were no significant differences in the median gestational age at delivery, the rate of spontaneous preterm delivery, or the rate of preterm premature rupture of membranes (PPROM).8 A meta-analysis of four RCTs by Berghella et al. in 2005 reviewed the use of ultrasound-indicated cerclage in both twin and singleton pregnancies.9 While cerclage was found to be helpful in preventing PTB in singleton pregnancies (n=552), in twin gestations (n= 49), cerclage was associated with a significant increase in PTB at less than 35 weeks gestation (RR 2.15, 95% confidence interval (CI) 1.15–4.01).9 However, a follow-up meta-analysis by the same group in 2015 of three RCTs of twin pregnancies with a cervical length of <2.5 cm (n=49) found no significant differences in prevention of PTB or latency from cerclage to delivery in the group with cerclage vs. the control group.10 Therefore, the authors concluded that ultrasound-indicated cerclage in twins is neither harmful nor beneficial. However, a few small retrospective studies have evaluated the outcomes of twin cerclages and suggested they can be successful in both ultrasound-indicated11 and physical exam-indicated12 cases, with a high rate of perinatal survival and similar efficacy as singleton pregnancies.13–18
Overall, studies show mixed results regarding cerclage efficacy in twin pregnancies. It is possible that these conflicting results may be confounded by variations in surgical technique and clinical management from multiple providers at different institutions. We sought to determine the outcomes of cerclage in twin pregnancies, placed and subsequently managed by a single provider at a single institution, when compared with twin pregnancies complicated by similar potential indications for cerclage, but expectantly managed. The primary outcome was the rate of spontaneous PTB prior to 32 weeks. Secondary outcomes were the rates of spontaneous and overall (including medically-indicated) PTB at <32 weeks, < 34 weeks, and <36 weeks, chorioamnionitis, birth weight, and perinatal mortality within 30 days of delivery. We also aimed to analyze these outcomes by cerclage indication.
Materials and Methods:
This is a retrospective cohort study of twin pregnancies with the following potential indications for cerclage from two institutions: history of prior preterm birth, ultrasound-identified short cervix ≤2.5 cm at 14–26 weeks, and/or cervical dilation ≥1.0 cm at 14–26 weeks. Subjects were included if they had a twin gestation at the time the cerclage was placed and if they had at least one of the aforementioned risk factors for PTB. Exclusion criteria included: major fetal anomaly, monochorionic-monoamniotic twins, termination of pregnancy, cerclage for delayed interval delivery, effective singleton pregnancy, or incomplete records. The study was approved by the institutional review boards at the University of California, Los Angeles (IRB# 15–000926) and at the University of California, San Francisco (IRB# 15–17198).
The cerclage cohort was retrospectively collected by searching the ICD-9 codes for twin pregnancy (651.03), cervical shortening (649.7, 622.5, 654.5), early or threatened labor (644), personal history of preterm labor (V13.21), and cerclage (67.5) in the medical billing records at the University of California, Los Angeles, between January of 2003 and December of 2016, performed by a single provider. The need for a cerclage was usually assessed in the outpatient clinic setting but occasionally was performed in the inpatient labor and delivery unit. Physical exam-indicated cerclage patients were generally managed as inpatients until delivery. Patients received a modified Shirodkar cerclage.
The control cohort of twin pregnancies at similar risk for preterm delivery and did not have a cerclage placed and was collected at the University of California, San Francisco (UCSF) by searching ICD-9 codes from January 2010 to December 2015 for twin pregnancy (651.03), cervical shortening (649.7, 622.5, 654.5), personal history of preterm labor (V13.21), and early or threatened labor (644) in the medical billing records. At this institution, cerclage placement for twin pregnancies is generally not offered. Patients with cervical dilation were generally managed as inpatients until delivery.
The following variables for baseline characteristics were collected from both institutions: maternal age, parity, race, tobacco use, body mass index (BMI), gestational age at presentation, insurance type (public, private, or unspecified), history of PTB or cervical insufficiency, pregnancies achieved through in vitro fertilization (IVF), chorionicity, cerclage type, the use of multifetal reduction, and progesterone use. Potential cerclage indication data was also collected from both institutions, including history of PTB, cervical length less than 2.5 cm by ultrasound, cervical dilation of greater than or equal to 1.0 cm, or more than one indication (ie history of PTB with short cervix and/or cervical dilation). Additionally, the gestational age at cerclage placement for the cerclage group, gestational age at presentation for the control group, and gestational age at delivery for both groups were collected to determine the latency (in days). Indication for delivery and whether delivery was spontaneous or iatrogenic was also recorded. Indications for delivery included spontaneous labor, rupture of membranes (confirmed by speculum exam with presence of ferning, pooling, nitrazine), maternal indication, fetal indication, or planned/ scheduled delivery.
Data was also collected from the neonatal intensive care unit (NICU) or nursery hospital stays of the babies born to all the women in each cohort. Outcomes collected included: birth weight, need for NICU admission of either or both twins, days in the NICU if necessary, the presence of fetal growth restriction of at least one twin (defined as estimated fetal weight before delivery <10 percentile), chorioamnionitis (based on maternal fever and maternal tachycardia, fetal tachycardia, or fundal tenderness), and perinatal death at less than 30 days of life.
The primary outcome was the rate of spontaneous PTB at <32 weeks, defined as PTB due to preterm labor and/or PPROM. Secondary outcomes were the rates of spontaneous and overall (including medically-indicated) PTB at <32 weeks, <34 weeks, and <36 weeks, chorioamnionitis, birth weight, and perinatal mortality within 30 days of delivery. We also performed a planned subgroup analysis stratified by cerclage indication. Outcomes were evaluated after excluding all subjects with the sole indication for cerclage being history of PTB, and stratifying by ultrasound vs. physical exam-indicated cerclage.
Statistical analysis was conducted using Stata 14 (College Park, TX). Data are shown as mean, median, range or number (percentages). Baseline differences between the cerclage and control group were analyzed using the T-test (parametric) or Mann-Whitney (non-parametric) for continuous variables, and the chi-square test or Fisher exact test for categorical variables. Frequencies of primary and secondary outcomes were compared with the Fisher exact test or Mann-Whitney tests as appropriate, and odds ratios were calculated with a 95% confidence interval (CI). An adjusted odds ratio (aOR) was calculated after adjusting for potential confounders. Kaplan-Meier curves were generated for gestational age at delivery comparing both cohorts as a whole, as well as ultrasound or physical exam indications in each cohort separately. P-values between each Kaplan-Meier curve were determined using the log-rank test. A p-value of <0.05 was considered statistically significant. All p-values were two-sided.
Results:
In the cerclage group, 152 records were obtained from medical billing from between January 2003 to December 2016 at UCLA (see Figure 1). Fifty-six charts were excluded for the following reasons: 20 were higher order multiples, ten underwent reductions to singleton pregnancy, eight did not undergo cerclage for pregnancy prolongation (for retaining a Bakri balloon postpartum), six had cerclages placed for delayed interval delivery of the second twin, four had cerclages placed by an outside provider and had transferred care, five resulted in elective termination of pregnancy, two had incomplete records or were lost to follow-up, and one had demise of both twins prior to cerclage placement. Therefore, 96 patients were eligible for the study and included in the final analysis. For the control group at UCSF, 221 records were retrieved from medical billing records from January 2010 to December 2015. 182 patients were excluded for the following reasons: 65 had their initial evaluation >26 weeks, 60 had no indication for cerclage (no history of PTB, no short cervix on ultrasound, no cervical dilation), 35 had no delivery records or were lost to follow-up, 11 had cerclages placed (6 at UCSF, 5 by outside provider), six underwent termination of pregnancy, and five had selective reduction to singleton pregnancies. Thus 39 patients were eligible and included in the study (Figure 1). In summary, there were 96 women in the cerclage group and 39 women in the control group for a total of 135 women in the study.
Figure 1: Patient selection process and primary outcome for cerclage cohort (left) and control cohort (right).
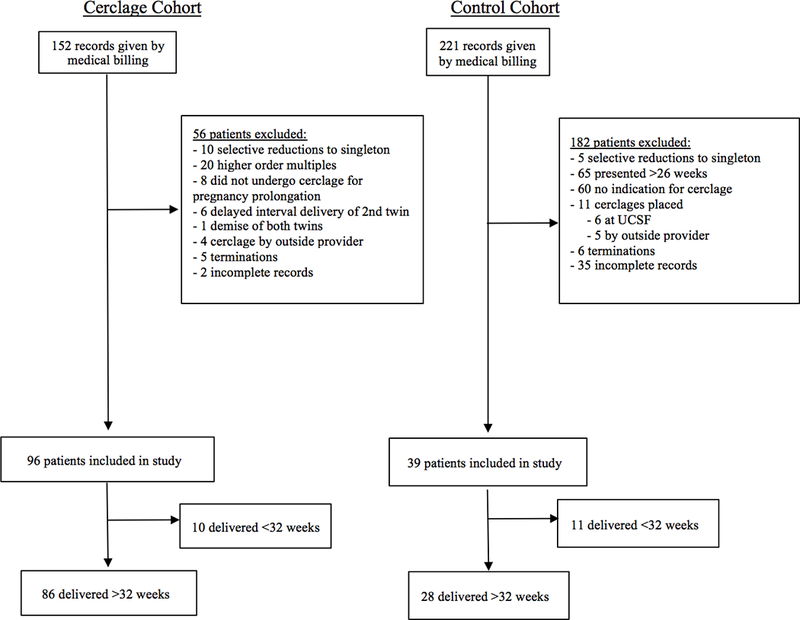
A flow sheet was generated demonstrating the patient selection process, reasons for exclusions, and gestational age at delivery for the cerclage and control group.
Baseline demographic data (Table 1) were analyzed between the two groups with some statistically significant differences. The cerclage group had a slightly higher median age, different racial composition, lower BMI, higher rate of private insurance, higher rate of IVF pregnancy, a higher proportion of dichorionic-diamniotic twins, higher rate of multifetal reduction, and different potential indications for cerclage. There were no differences in parity, tobacco use, mean cervical dilation, mean cervical length, or history of PTB. “History of PTB” in Table 1 included all women with a prior history, even if they had other indications for cerclage such as short cervical length. At both institutions, steroids, tocolytics, and progesterone were given at the discretion of the managing provider, and proportions of patients receiving any of the above were not statistically significant between institutions (Table 1).
Table 1:
Patient Demographics
| Patient Characteristics | No Cerclage n=39 | Cerclage n=96 | P |
|---|---|---|---|
| Age (years), median (range) | 32 (17 to 45) | 35 (24–51) | 0.003 |
| Gravidity, median (range) | 2.8 (1 to 11) | 2.5 (1 to 11) | 0.373 |
| Nulliparous | 19 (50%) | 55 (57.3%) | 0.444 |
| Race | <0.001 (fe) | ||
| White | 11 (28.2%) | 59 (61.5%) | |
| Black | 10 (25.6%) | 4 (4.2%) | |
| Hispanic | 8 (20.5%) | 6 (6.25%) | |
| Asian | 7 (17.9%) | 12 (12.5%) | |
| Other | 1 (2.6%) | 15 (15.6%) | |
| Smoking | 0 (0%) | 3 (3.1%) | 0.560 (fe) |
| BMI (kg/m2) | 27 (19–44) | 24 (18–39) | 0.008 |
| Obese | 9 (25.7%) | 9 (9.6%) | 0.019 |
| Insurance | <0.001 (fe) | ||
| Public | 19 (50%) | 1 (1.1%) | |
| Private | 17 (44.7%) | 94 (98.9%) | |
| Unspecified | 2 (5.3%) | 0 (0%) | |
| Medical Risk Factors* | 0.125 | ||
| No | 31 (83.8%) | 68 (70.8%) | |
| Yes | 6 (16.2%) | 28 (29.2%) | |
| Hx of PTB | 9 (23.7%) | 26 (27.1%) | 0.686 |
| Hx of cervical insufficiency | 2 (5.3%) | 18 (18.9%) | 0.059 (fe) |
| IVF | 9/38 (23.7%) | 73/95 (76.8%) | <0.001 |
| Chorionicity | 0.003 | ||
| Dichorionic-diamniotic | 23 (60.5%) | 81 (84.4%) | |
| Monochorionic-diamniotic | 15 (39.5%) | 15 (15.6%) | |
| Multifetal reduction | 0/36 (0%) | 17/87 (19.5%) | 0.001 (fe) |
| TTTS | 4/15 (26.7%) | 4/15 (26.7%) | 1.0 (fe) |
| Laser | 2/4 (50.0%) | 3/4 (75.0%) | 1.0 (fe) |
| Progesterone use | 6 (15.4%) | 20 (20.8%) | 0.467 |
| Tocolytic use | 25/39 (64.1%) | 69/96 (71.9%) | 0.373 |
| Betamethasone given | 32/39 (82.1%) | 76/96 (79.2%) | 0.704 |
Data presented is n (%) or median (range) unless otherwise indicated. P-values calculated with chi-squared, Fishers exact (fe) test or Mann-Whitney as appropriate. Significant values (p<0.05) are indicated in bold.
Other medical risk factors for PTB, including chronic hypertension, obesity, fibroids.
fe, fishers exact; BMI, body mass index; RF, risk factors; PTB, preterm birth; Hx, history; IVF, in vitro fertilization; TTTS, twin twin transfusion syndrome
Latency from presentation or cerclage placement to delivery was noted to be significantly longer in the cerclage group, with a median of 91 days vs. 57 days (p=0.001). Cerclage placement was found to be associated with prolongation of pregnancy by a median of 34 days. Median gestational age at delivery was 35 weeks in the cerclage group vs. 32 weeks in the control group (p=0.002) (Table 2). On univariate analysis, the primary outcome of spontaneous PTB <32 weeks was significantly reduced in the cerclage group: 10 (10.4%) vs. 11 (28.2%), OR 0.23 (95% CI 0.08–0.70, p=0.017). (Table 3). The secondary outcomes of rates of spontaneous and overall preterm births at different gestational ages were also analyzed. There was a statistically significant reduction in spontaneous PTB <34 weeks (OR 0.33, CI 0.13–0.83, p=0.019), spontaneous PTB <36 weeks (OR 0.29, CI 0.12– 0.70, p= 0.006), overall preterm birth <32 weeks (OR 0.30, CI 0.11–0.80, p= 0.016), overall preterm birth <34 weeks (OR 0.28, CI 0.12–0.68, p= 0.005), and overall preterm birth <36 weeks (OR 0.27, CI 0.10–0.77, p= 0.014) in the cerclage group.
Table 2:
Cerclage Indications and Latency
| Variable | No Cerclage n=39 | Cerclage n=96 | P |
|---|---|---|---|
| Cerclage Indication | 0.21 (fe) | ||
| History of PTB only* | 2 (5.1%) | 6 (6.3%) | |
| US indicated (CL<2.5cm) | 20 (51.3%) | 36 (37.5%) | |
| CL< 1.5cm | 15 (38.5%) | 20 (20.8%) | |
| PE indicated (dil>1cm) | 17 (43.6%) | 54 (56.2%) | |
| Mean cervical length (cm) | 1.55 | 1.46 | 0.52 |
| Mean cervical dilation (cm) | 1.1 | 0.9 | 0.26 |
| GA at presentation (wks) † | 24.6 (19 to 32) | 21 (14 to 26) | <0.001 |
| GA at cerclage (wks) | NA | 20 (12 to 27) | |
| GA at delivery (wks) | 32 (21.7 to 38.7) | 35 (21.0 to 37.9) | 0.002 |
| Latency (d) † | 57 (3 to 108) | 91 (12 to 166) | 0.001 |
Data presented is n (%) or median (range) unless otherwise indicated. P-values calculated with Fishers exact (fe) test. Significant values (p<0.05) are indicated in bold.
CI, cervical insufficiency; CL, cervical length; US, ultrasound; PE, physical exam; dil, dilation; GA, gestational age; wks, weeks; d, days
Includes subjects with a history of PTB only. All subjects with a history of PTB and some other cerclage indication were grouped with the other cerclage indications
From presentation or cerclage to delivery, excluding history-indicated cerclages
Table 3:
Delivery Outcomes Between Cerclage and Control Group
| Variable | No Cerclage n=39 | Cerclage n=96 | P | OR (95%CI), p | aOR (95% CI), p* |
|---|---|---|---|---|---|
| Spontaneous PTB | |||||
| sPTB <32w | 11/39 (28.2%) | 10/96 (10.4%) | 0.017 | 0.23 (0.08– 0.70), 0.010 | 0.24 (0.06–0.90), 0.035 |
| sPTB <34w | 17/39 (43.6%) | 24/96 (25%) | 0.040 | 0.33 (0.13–0.83), 0.019 | 0.38, (0.12–1.16), 0.089 |
| sPTB <36w | 24/39 (61.54%) | 38/96 (39.6%) | 0.035 | 0.29 (0.12– 0.70), 0.006 | 0.34 (0.04–0.81), 0.013 |
| PTB (all indications) | |||||
| PTB <32w | 14/39 (35.9%) | 16/96 (16.7%) | 0.022 | 0.3 (0.11– 0.80), 0.016 | 0.31 (0.10–0.86), 0.018 |
| PTB <34w | 23/39 (60.0%) | 31/96 (32.3%) | 0.006 | 0.28 (0.12–0.68), 0.005 | 0.38 (0.11–1.01), 0.055 |
| PTB <36w | 33/39 (84.6%) | 59/96 (61.5%) | 0.009 | 0.27 (0.10–0.77), 0.014 | 0.37 (0.10–0.84), 0.030 |
Data presented is n (%) or median (range). P-values calculated with Fishers exact test. Significant values (p<0.05) are indicated in bold.
sPTB, spontaneous preterm birth; PTB, preterm birth; aOR, adjusted odds ratio; CI, confidence interval; w, weeks
aOR: adjusted for age, race, BMI, insurance, IVF, chorionicity, multifetal reduction
A multivariate analysis was performed controlling for differences between the cerclage and control cohorts (age, race, BMI, insurance type, IVF, chorionicity, indications for cerclage, and multifetal reduction). There remained a statistically significant decrease in the primary outcome of spontaneous PTB rate <32 weeks in the cerclage group (aOR 0.24, CI 0.06–0.90, p=0.035) and spontaneous PTB rate <36 weeks (aOR 0.34, CI 0.04–0.81), p=0.013), and there continued to be no significant differences in spontaneous PTB <34 weeks (aOR 0.38, CI 0.12–1.16, p=0.089). There remained significant decreases in overall PTB rate <32 weeks (aOR 0.31, CI 0.10–0.86, p=0.018) and <36 weeks (aOR 0.37, CI 0.10–0.84, p=0.030), but overall PTB rate <34 weeks lost statistical significance (aOR 0.38, CI 0.11–1.01, p=0.055). The indication for delivery was similar between groups, but the control group had a higher proportion of spontaneous PTB and PPROM (19.4% vs. 6.3%, p=0.032). We did not detect statistically significant differences between the groups for maternal indication for delivery, preeclampsia, chorioamnionitis, or fetal growth restriction.
Since prior retrospective studies showed potential benefit of cerclage in twin pregnancies when separating ultrasound-indicated (<2.5 cm and <1.5 cm) and physical exam-indicated cerclages,16,17,18 subgroup analysis was performed where all history only-indicated cerclages (history of PTB without short cervix or cervical dilation, n=6) were excluded. Table 4 displays a more detailed subgroup analysis of all patients with ultrasound-indicated (<2.5 cm cervical length) vs. physical exam- indicated cerclage (cervical dilation greater than or equal to 1.0 cm). When stratified by ultrasound vs. physical exam-indicated cerclage, only physical-exam indicated cerclage was associated with a statistically significant reduction in spontaneous PTB rates. Spontaneous PTB <32 weeks in patients with cervical dilation was 11.1% in the cerclage group vs. 41.2% in the control group (p=0.01). Also, spontaneous PTB <34 weeks in patients with cervical dilation was 29.6% in the cerclage group and 58.8% in the control group (p=0.043), with no difference in spontaneous PTB rates in the short cervix by ultrasound group. Overall, PTB <32 weeks (16.7% vs. 47.1%, p=0.02), <34 weeks (35.2% vs. 76.5%, p=0.009), and <36 weeks (61.1% vs. 100%, p=0.002) were also decreased in the cerclage group among women with a dilated cervix by physical exam (Table 4). When the ultrasound-indicated cerclage group was further sub-stratified to only include cervical length <1.5cm (n=20), no statistically significant differences were detected between the cerclage and control groups in overall or spontaneous PTB rates <32 weeks, <34 weeks, and <36 weeks.
Table 4:
Delivery Outcomes Stratified by Potential Cerclage Indication (excluded history-only indicated cerclages)
| Variable | No Cerclage n=37 | Cerclage n=90 | P |
|---|---|---|---|
| Spontaneous PTB | |||
| sPTB <32w | |||
| US indicated (all)* | 3/20 (15.0%) | 4/36 (11.1%) | 0.691 |
| US indicated (<1.5cm) | 5/15 (33.3%) | 4/20 (20%) | 0.451 |
| PE indicated | 7/17 (41.2%) | 6/54 (11.1%) | 0.01 |
| sPTB <34w | |||
| US indicated (all)* | 6/20 (30.0%) | 8/36 (22.2%) | 0.536 |
| US indicated (<1.5cm) | 10/15 (66.7%) | 6/20 (30%) | 0.055 |
| PE indicated | 10/17 (58.8%) | 16/54 (29.6%) | 0.043 |
| sPTB <36w | |||
| US indicated (all)* | 9/20 (45%) | 12/36 (33.3%) | 0.405 |
| US indicated (<1.5cm) | 11/15 (73.3%) | 9/20 (45%) | 0.167 |
| PE indicated | 13/17 (76.4%) | 26/54 (48.1%) | 0.055 |
| PTB (all indications) | |||
| PTB <32w | |||
| US indicated (all)* | 5/20 (25%) | 7/36 (19.4%) | 0.737 |
| US indicated (<1.5cm) | 7/15 (46.7%) | 6/20 (30%) | 0.481 |
| PE indicated | 8/17 (47.1%) | 9/54 (16.7%) | 0.02 |
| PTB <34w | |||
| US indicated (all)* | 9/20 (45.0%) | 12/36 (33.3%) | 0.405 |
| US indicated (<1.5cm) | 12/15 (80%) | 8/20 (40%) | 0.055 |
| PE indicated | 13/17 (76.5%) | 19/54 (35.2%) | 0.005 |
| PTB <36w | |||
| US indicated (all)* | 14/20 (70.0%) | 24/36 (66.7%) | 1.00 |
| US indicated (<1.5cm) | 14/15 (93.3%) | 15/20 (75%) | 0.207 |
| PE indicated | 17/17 (100%) | 33/54 (61.1%) | 0.002 |
P-values are from Fisher exact test. Significant values (p<0.05) are indicated in bold.
US, ultrasound; PE, physical exam; sPTB, spontaneous preterm birth; PTB, preterm birth; w, weeks.
Includes all CL<2.5cm
With respect to neonatal outcomes, the cerclage group had a statistically higher birth weight, lower perinatal death rate, and no differences in the rate of chorioamnionitis. Mean birth weight was 2179g in the cerclage group vs. 1722g in the control group (p<0.001), and perinatal death was 1.6% vs. 12.9% (p=0.001). The risk of perinatal death was reduced by 90% in the cerclage group even when adjusting for gestational age (aOR 0.1, CI 0.01–0.93, p=0.043). It is unclear why there was this difference between institutions. No statistically significant differences were found between rates of chorioamnionitis, fetal growth restriction, rates of NICU admission, or days spent in the NICU, after controlling for gestational age (Table 5).
Table 5:
Neonatal Outcomes
| Neonatal Outcomes | No Cerclage (n=39) | Cerclage (n=96) | P | aOR (95% CI), p* |
|---|---|---|---|---|
| Chorioamnionitis | 3/31 (9.7%) | 5/95 (5.3%) | 0.41 | 1.70 (0.26–11.18), 0.579 |
| FGR of at least one twin | 3/39 (7.7%) | 21/96 (21.9%) | 0.08 | 3.43 (0.93–12.69), 0.064 |
| NICU admission | 46/62 (74.2%) | 116/185 (62.7%) | 0.122 | 1.76 (0.71–4.36), 0.221 |
| Perinatal death <30d | 8/62 (12.9%) | 3/190 (1.6%) | 0.001 | 0.1 (0.01–0.93), 0.043 |
| Birth weight (g) | 1665 (410– 3235) | 2278 (635–3062) | <0.001 | N/A |
| Days in NICU | 29 (5–180) | 25 (1–189) | 0.66 | N/A |
Data is presented as N (%) or median (range). P-values were calculated from Fisher exact, multivariable logistic regression, or Kruskal-Wallis as appropriate. Significant values (p<0.05) are indicated in bold.
aOR, adjusted odds ratio; CI, confidence interval; FGR, fetal growth restriction; NICU, neonatal intensive care unit
adjusted for gestational age
Kaplan-Meier curves were generated for gestational age at delivery by comparing the cerclage vs. no cerclage groups overall, as well as comparing ultrasound or physical exam indications in each cohort. The log-rank test displayed a statistically significant difference between the cerclage and control curves (p=0.005) overall (Figure 2). However, when subdividing the groups by ultrasound indication and physical exam indication, there was only a significant difference in the curves between those with cervical dilation (p<0.001) (Figure 3).
Figure 2: Survival curves of pregnancies that remained undelivered, cerclage vs. control.
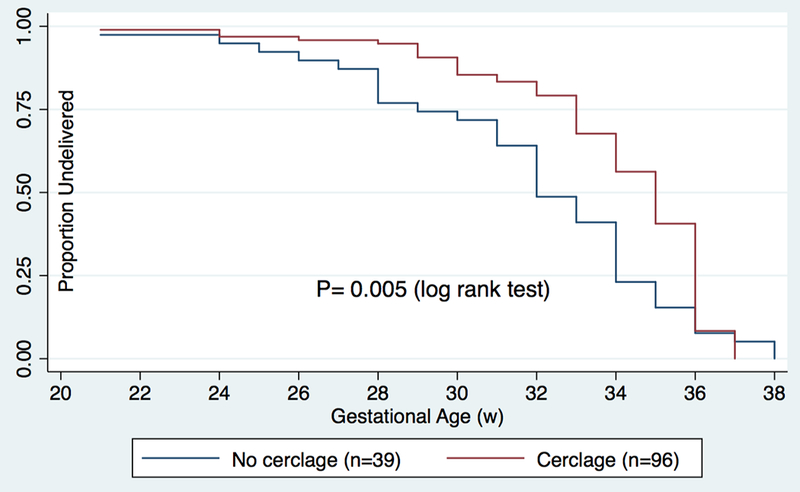
Kaplan-Meier curves were generated for gestational age at delivery for the cerclage and control groups. The log-rank test showed significant differences between the groups (p= 0.005).
Figure 3: Survival curves of pregnancies that remained undelivered, by indication.
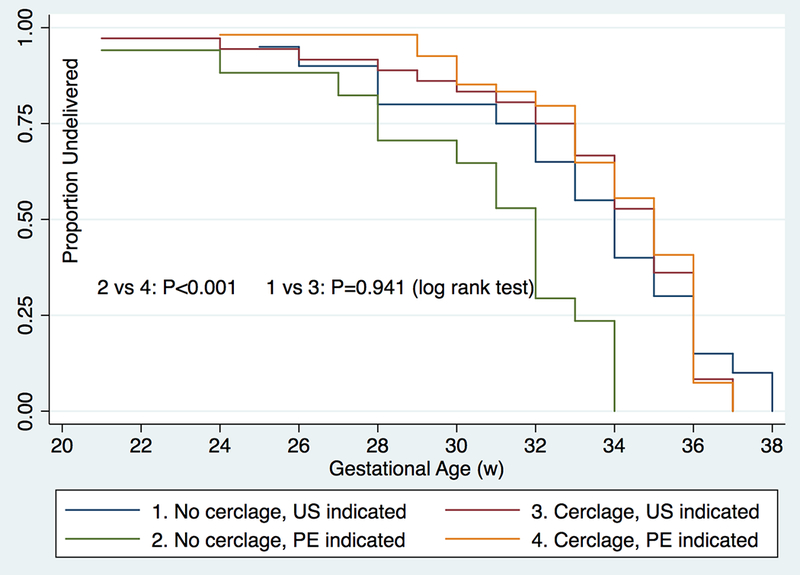
Kaplan-Meier curves were generated for gestational age at delivery by presence of cerclage, ultrasound indications and physical exam indications. The log-rank test showed significant differences between the cerclage vs. no cerclage group only for physical exam indications, or cervical dilation (p=<0.001).
Discussion:
There is limited data comparing the efficacy of cerclage vs. expectant management in twin pregnancies. A few small retrospective studies do demonstrate a beneficial effect of cerclages in reducing preterm birth in twin gestations. In a retrospective cohort study, Houlihan et al. matched 40 twin pregnancies with a cervical length of 0.1–2.4 cm undergoing cerclage with 40 controls receiving expectant management.15 Spontaneous birth <32 weeks was significantly less frequent (RR 0.4, CI 0.2–0.8) in the cerclage group. Another retrospective cohort study by Roman et al. compared twin pregnancies with short cervical length (<2.5cm at 16–24 weeks) who underwent an ultrasound-indicated cerclage (n=57) to those who received expectant management (n=83) from four institutions over a 17-year period.16 There were no significant differences of spontaneous PTB except in the subgroup of women with a cervical length <1.5 cm, in which the interval between diagnosis to delivery was significantly prolonged compared to controls (12.5 vs. 8.8 weeks).16 A recent study by Adams et al had similar findings, with cerclage reducing PTB only in a subgroup of women with cervical length <1.5cm.17 Roman et al. also examined the utility of physical exam-indicated cerclage (≥1.0 cm dilation) in twin gestations with 38 women who underwent cerclage and compared with 38 women who were expectantly managed.18 The interval from time of diagnosis of dilated cervix to delivery was significantly longer in the cerclage group compared to the control group (10.5 vs. 3.7 weeks). There were significant decreases in spontaneous PTB <34 weeks (aOR 0.02, CI 0.03–0.34), <32 weeks, < 28 weeks, and <24 weeks, as well as significant reductions in perinatal mortality, NICU admissions, and adverse neonatal outcomes.
In our study, women who underwent cerclage placement had greater prolongation of pregnancy and lower rate of spontaneous PTB less than 32 weeks by >75%, even after controlling for potential confounders. Pregnancy latency was increased with cerclage by a median of 34 days. Neonatal outcomes were also improved, with a increased mean birth weight and decreased perinatal death <30 days.
Interestingly, the cerclage group had a lower rate of overall PTB, not just spontaneous births, <32 weeks and <36 weeks that remained after multivariate analysis. This is likely due to the fact that a large proportion of controls were delivered due to spontaneous preterm labor or PPROM, which comprised a larger factor in the total PTBs for all indications. The number of indicated PTBs for maternal indication did not appear to be different between the two populations. Interestingly, when analyzing only ultrasound-indicated cerclages, there was no difference in the primary outcome of spontaneous PTB <32 weeks between the cerclage and control groups for short cervix, even when stratifying for cervical length <1.5cm. The difference in primary outcome was only noted for physical exam-indicated cerclages, suggesting that cerclage in twin pregnancies may be more beneficial in the setting of dilated cervix, rather than for the sole indication of short cervix. These findings are similar to the retrospective studies by Roman et al. that found no difference in spontaneous PTB <28 weeks, <32 weeks, or <34 weeks between the ultrasound-indicated cerclage group vs. expectant management group except in the subgroup of women with cervical length <1.5cm;16 however, there were significant decreases in spontaneous PTB for women with dilated cervix greater than or equal to 1cm who underwent cerclage.18 Our findings are consistent with several other studies that demonstrated that physical exam-indicated cerclage in twin pregnancies may decrease PTB rates or have similar efficacy as singleton pregnancies.11–15
One strength of our study is that it is one of the larger series of cerclages in twin pregnancies published so far. Furthermore, all cerclages were placed by a single provider at a single institution, which limits confounding factors of technique, experience, or differences in provider bias for offering the intervention that is present in other retrospective series. However, while variability in management is decreased, it is acknowledged that this does limit the potential generalizability of the study. Another strength includes the evaluation of neonatal data, such as birth weight, neonatal death rates, chorioamnionitis, NICU admissions, and length of stay in the NICU. Our positive findings in regard to neonatal data and decrease in neonatal deaths in the cerclage group are similar to findings in prior retrospective twin cerclage studies.18 Stratification by physical exam-indicated and ultrasound-indicated cerclage also provides further insight into the group that may most benefit from cerclage. Another strength is that the site of the control group (UCSF) does not place cerclages in twin pregnancies uniformly, thus limiting provider selection bias in management decisions for these high-risk pregnancies.
The main limitation of our study is the generalizability of the study, as a one provider placed all of the cerclages. Furthermore, there were differences of baseline demographic data between our control and cerclage groups. This is likely secondary to the differing demographics that comprise the two cities in which the institutions are based. Mainly, the control group had higher risk demographics, such as more monochorionic twins and a higher rate of public insurance. The cerclage cohort from Los Angeles had a higher median age, larger proportion of white patients, and higher rates of private insurance, but also had a higher proportion of physical exam-indicated cerclages. Thus, theoretically the control group would have more indicated preterm births and the cerclage group would have more spontaneous preterm births, but this result did not occur. While we controlled for the observed differences on multivariate analysis, other unknown differences in demographics may further confound our results. Additionally, management is likely different between our two institutions, which cannot be analyzed in a retrospective fashion. Another limitation is the difference in sample sizes between the two institutions, as more data was able to be collected for the cerclage cohort. Not all demographic or pregnancy course information could be collected for every patient included in the study due to limited detailed records, especially in the earlier years before a uniform electronic health record was established at the University of California, Los Angeles.
Our findings, add to the existing literature that cerclages in twins may be beneficial in certain circumstances (especially physical-exam indicated), and may be associated with improved pregnancy and neonatal outcomes. It is evident that there is lack of knowledge of cerclages in twin pregnancies, and current recommendations are based on very limited data. Current ACOG recommendations state that cerclage may increase the risk of PTB in women with twin pregnancies and is thus not recommended.19 However, the information cited for this recommendation is based on a retrospective cohort of 49 twin pregnancies with only 24 that received a cerclage displaying a non-statistically significant relative risk of 2.15 for PTB <35 weeks.9 It is clear that there is the need for more studies, particularly randomized control trials, comparing cerclage to no cerclage for women with twin pregnancies at risk for PTB before any definitive clinical recommendations can be made. Several large RCTs are ongoing evaluating both ultrasound-indicated and physical exam-indicated cerclages in twin pregnancies (NCT02912390, NCT02490384).20 The results of these studies are eagerly awaited.
Acknowledgments:
S.LG. is supported by the Reproductive Scientist Development Program, by the Eunice Kennedy Shriver National Institute of Child Health & Human Development (K12HD000849) and the Burroughs Wellcome Fund.
Footnotes
Disclosure of Interest: The authors report no conflicts of interest. The views expressed in the submitted article are of the authors and not an official position of the institution.
Presented in part as a poster presentation at the 36th Annual Meeting of the Society of Maternal-Fetal Medicine, Atlanta, GA, February 1–6, 2016
References:
- 1.Martin JA, Hamilton BE, Osterman MJK, Curtin SC, Mathews TJ. National vital statistics reports. Births: final data for 2013. 2015 [PubMed] [Google Scholar]
- 2.Practice Bulletin No. 171: Management of Preterm Labor. The American College of Obstetricians and Gynecologists 2016;128:931–933. [Google Scholar]
- 3.Dor J, Shalev J, Mashiach S, Blankstein J, Serr DM. Elective cervical suture of twin pregnancies diagnosed ultrasonically in the first trimester following induced ovulation. Gynecol Obstet Invest 1982;13:55e60. [DOI] [PubMed] [Google Scholar]
- 4.Rust OA, Atlas RO, Reed J, van Gaalen J, Balducci J. Revisiting the short cervix detected by transvaginal ultrasound in the second trimester: why cerclage therapy may not help. Am J Obstet Gynecol 2001;185: [DOI] [PubMed] [Google Scholar]
- 5.Althuisius SM, Dekker GA, Hummel P, Bekedam DJ, van Geijn HP. Final results of the Cervical Incompetence Prevention Randomized Cerclage Trial (CIPRACT): therapeutic cerclage with bed rest versus bed rest alone. Am J Obstet Gynecol 2001;185:1106e12. [DOI] [PubMed] [Google Scholar]
- 6.Berghella V, Odibo AO, Tolosa JE. Cerclage for prevention of preterm birth in women with a short cervix found on transvaginal ultrasound examination: a randomized trial. Am J Obstet Gynecol 2004;191:1311e7. [DOI] [PubMed] [Google Scholar]
- 7.Rafael TJ, Berghella V, Alfirevic Z. Cervical stitch (cerclage) for preventing preterm birth in multiple pregnancy. Cochrane Database Syst Rev 2014;(9): CD009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roman AS, Rebarber A, Pereira L, Sfakianaki AK, Mulholland J, Berghella V. The efficacy of sonographically indicated cerclage in multiple gestations. Journal of ultrasound in medicine 2005; 24(6), 763–8; quiz 770. [DOI] [PubMed] [Google Scholar]
- 9.Berghella V, Odibo AO, To MS, Rust OA, Althuisius SM. Cerclage for short cervix on ultrasonography: meta-analysis of trials using individual patient level data. Obstet Gynecol 2005;106:181e9. [DOI] [PubMed] [Google Scholar]
- 10.Saccone G, Rust O, Althuisius S, Roman AS, Berghella V. Cerclage for short cervix in twin pregnancies: systematic review and meta-analysis of randomized trials using individual patient-level data. Acta Obstet Gynecol Scand 2015;94:352e8. [DOI] [PubMed] [Google Scholar]
- 11.Zanardini C, Pagani G, Fichera A, Prefumo F, Frusca T. Cervical cerclage in twin pregnancies. Archives of Gynecology and Obstetrics 2013; 288(2), 267–271. [DOI] [PubMed] [Google Scholar]
- 12.Levin I, Salzer L, Maslovitz S, Avni A, Lessing JB, Groutz A, Almog B. Outcomes of mid-trimester emergency cerclage in twin pregnancies. Fetal diagnosis and therapy 2012; 32(4), 246–250. [DOI] [PubMed] [Google Scholar]
- 13.Miller ES, Rajan PV, Grobman WA. Outcomes after physical examination-indicated cerclage in twin gestations. American journal of obstetrics and gynecology 2014; 211(1), 46–45. [DOI] [PubMed] [Google Scholar]
- 14.Rebarber A, Bender S, Silverstein M, Saltzman DH, Klauser CK, Fox NS. Outcomes of emergency or physical examination-indicated cerclage in twin pregnancies compared to singleton pregnancies. European journal of obstetrics & gynecology and reproductive biology 2014; 173, 43–47. [DOI] [PubMed] [Google Scholar]
- 15.Houlihan C, Poon LC, Ciarlo M, Kim E, Guzman ER, et al. Cervical cerclage for preterm birth prevention in twin gestation with short cervix: a retrospective cohort study. Ultrasound in obstetrics & gynecology 2016;48(6):752–756. [DOI] [PubMed] [Google Scholar]
- 16.Roman A, Rochelson B, Fox NS, et al. Efficacy of ultrasound-indicated cerclage in twin pregnancies. American journal of obstetrics and gynecology 2015;212(6):788.e1–788.e6. [DOI] [PubMed] [Google Scholar]
- 17.Adams TM, Rafael TJ, Kunzier NB, et al. Does cervical cerclage decrease preterm birth in twin pregnancies with a short cervix?. Journal of Maternal - Fetal & Neonatal Medicine. 2017;1–7. [DOI] [PubMed] [Google Scholar]
- 18.Roman A, Rochelson B, Martinelli P, et al. Cerclage in twin pregnancy with dilated cervix between 16 to 24 weeks of gestation: retrospective cohort study. American journal of obstetrics and gynecology 2016;215(1):98.e1–98.e11. [DOI] [PubMed] [Google Scholar]
- 19.Practice Bulletin No. 142: Cerclage for the Management of Cervical Insufficiency. The American College of Obstetricians and Gynecologists 2014;123:372–379. [DOI] [PubMed] [Google Scholar]
- 20.Cerclage For Short Cervix In Twins. Clinicaltrials.Gov”. Clinicaltrials.gov. N.p., 2017. Web. 19 February 2017. [Google Scholar]


