Abstract
Background and study aims Endoscopic retrograde cholangiopancreatography (ERCP) in patients with a preexisting duodenal stent is particularly challenging and has a low success rate. Endoscopic ultrasound (EUS)-guided biliary drainage (EUS-BD) has been increasingly used as an alternative to percutaneous transhepatic biliary drainage after failed ERCP. EUS-guided choledochoduodenostomy (EUS-CD) and EUS-guided hepaticogastrostomy (EUS-HGS) have been reported to have similar efficacity. Recently, a novel dedicated fully-covered lumen-apposing metal stent (LAMS) has been developed for EUS-CD (Hot AXIOS; Boston Scientific, Massachusetts, United States). It seems that this new device decreases the morbidity of EUS-CD. We present a case in which EUS-CD with LAMS through an uncovered metal duodenal stent was used successfully.
Introduction
Endoscopic retrograde cholangiopancreatography (ERCP) in patients with a preexisting duodenal stent is particularly challenging and with low success rate 1 . Recently, a novel, dedicated fully-covered lumen-apposing metal stent (LAMS) has been developed for endoscopic ultrasound (EUS)-guided choledochoduodenostomy (EUS-CD) (Hot AXIOS; Boston Scientific, Massachusetts, United States). We present the case of a successful EUS-CD with LAMS through an uncovered metal duodenal stent.
Case report
A 56-year-old man with recent abdominal pain and postprandial vomiting underwent a computed tomography (CT) scan, which showed an enlarged tumor of the pancreatic head with duodenal obstruction. Endoscopic ultrasound fine-needle aspiration (EUS-FNA) confirmed the diagnosis of pancreatic adenocarcinoma. At that time, no dilatation of the main bile duct was seen, the liver function test was normal, and no biliary stent was inserted. For a complete duodenal obstruction, an uncovered metal stent duodenal stent was placed.
Two months later, the patient presented with abdominal pain and jaundice. Laboratory tests showed elevated liver function test results: ALT 229 U/L (5 – 45 U/L), AST 181 U/L (5 – 35 U/L), PAL 540 U/L (30 – 110 U/L), γGT 6329 U/L (7 – 50 U/L), Bilirubin 268 μmol/L (0 – 20.5 μmol/L). A computed tomography scan revealed biliary tree dilatation with extrinsic pancreatic compression ( Fig. 1 ).
Fig. 1 .
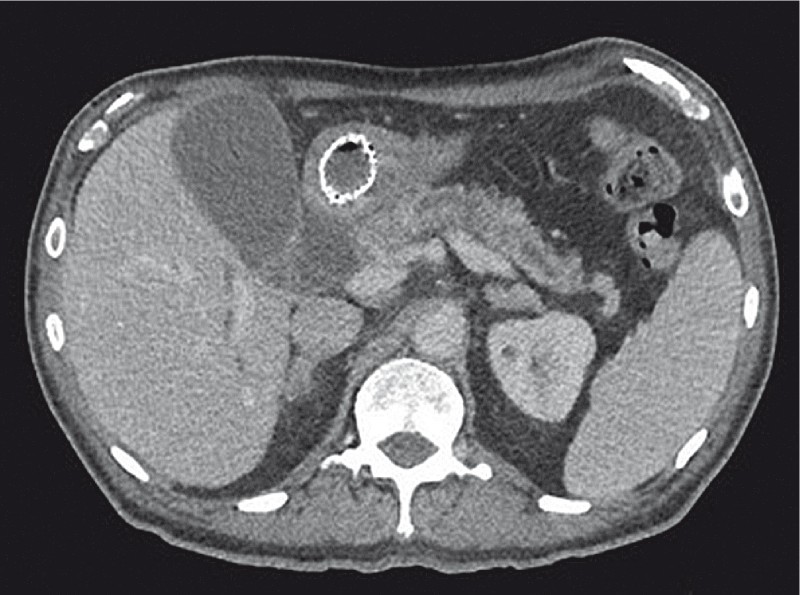
Computed tomography scan before endoscopic ultrasound-guided choledochoduodenostomy showed biliary tree dilatation with the duodenal stent in place.
First, ERCP failed to achieve biliary drainage because of an inability to cannulate the papilla due to tumor infiltration. Endoscopic ultrasound-guided hepaticogastrostomy (EUS-HGS) was not attempted because the left intrahepatic bile ducts were minimally dilated (3 mm). However, the common bile duct (CBD) was largely dilated (20 mm). A Hot AXIOS device with a stent of 8 × 6 mm was advanced through the uncovered metal stent. Pure cut electrocautery current was then applied, allowing the device to reach the CBD. Next, the distal flange was opened ( Fig. 2 ) and retracted towards the EUS transducer, and once a biliary and bulbar tissue apposition had been noted, the proximal flange was released ( Fig. 3 ). Good drainage of purulent bile was observed ( Video 1 ) ( Fig. 4 , Fig. 5 ) and no complications occurred during the procedure and 6 months after.
Fig. 2.
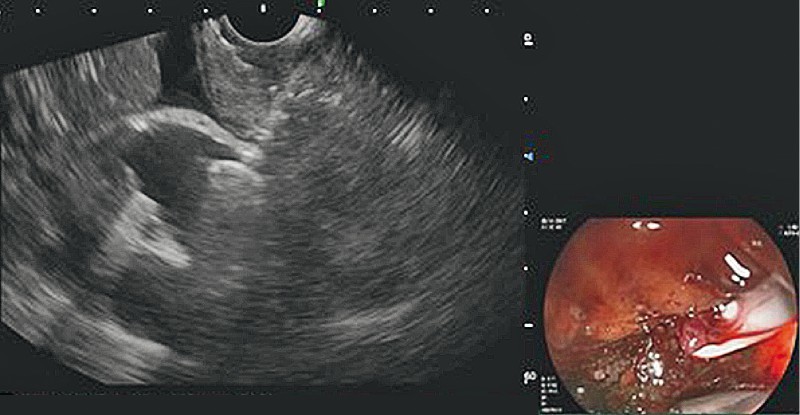
Endoscopic ultrasound-guided choledochoduodenostomy with the Hot AXIOS stent and deployment of the distal flange.
Fig. 3 .
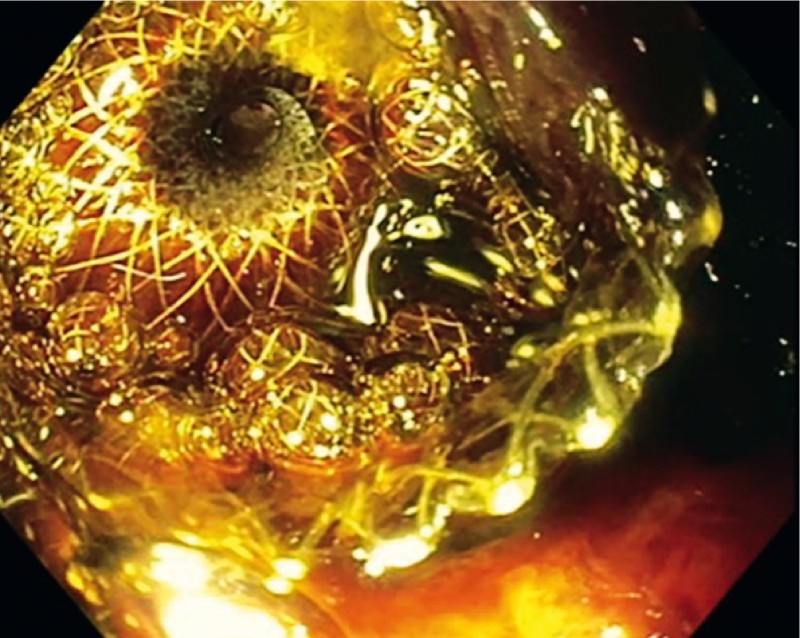
Endoscopic view of the lumen-apposing metal stent in the duodenum.
Fig. 4 .
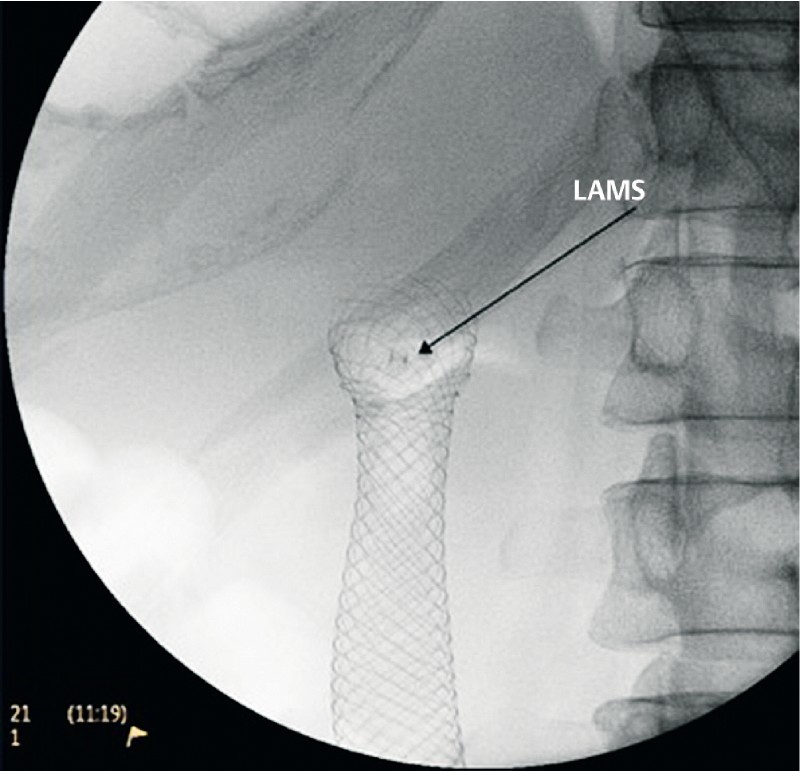
Radioscopic view of the lumen-apposing metal stent through the duodenal stent.
Fig. 5 .
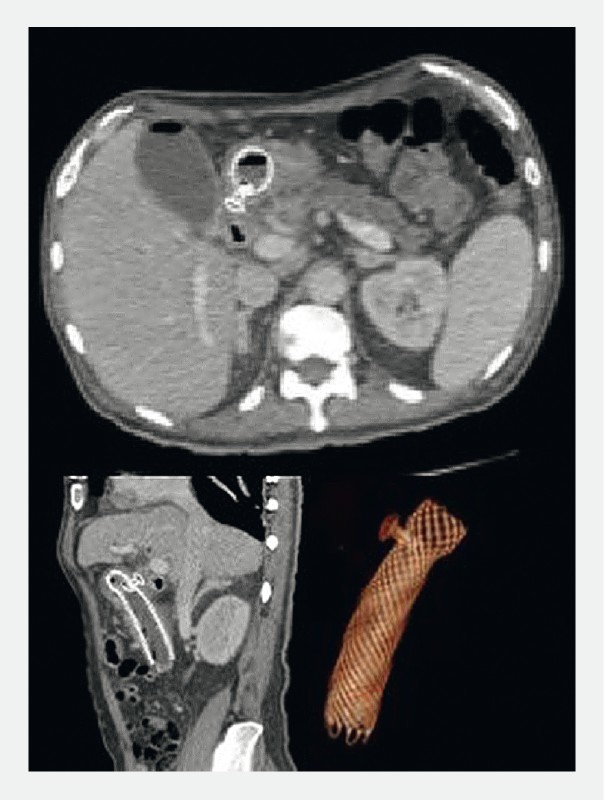
Computed tomography scan showing lumen-apposing metal stent through the duodenal stent.
Endoscopic ultrasound guided biliary drainage (EUS-BD) has been increasingly used as an alternative to percutaneous transhepatic biliary drainage after failed ERCP 2 3 . EUS-CD and EUS-HGS have been reported to have similar efficacity 4 . It seems that this new device decreases the morbidity of EUS-CD 5 .
Conclusion
This is the first reported case of EUS-CD through a duodenal metal stent. Failed ERCP after duodenal stent placement is a frequent situation faced by endoscopists during the progression of advanced pancreatic cancer, and ERCP can be easily done using this method.
Footnotes
Competing interests None
References
- 1.Khashab M A, Valeshabad A K, Leung W et al. Multicenter experience with performance of ERCP in patients with an indwelling duodenal stent. Endoscopy. 2014;46:252–255. doi: 10.1055/s-0033-1359214. [DOI] [PubMed] [Google Scholar]
- 2.Sharaiha R Z, Khan M A, Kamal F et al. Efficacy and safety of EUS-guided biliary drainage in comparison with percutaneous biliary drainage when ERCP fails: a systematic review and meta-analysis. Gastrointest Endosc. 2017;85:904–914. doi: 10.1016/j.gie.2016.12.023. [DOI] [PubMed] [Google Scholar]
- 3.Sportes A, Camus M, Greget M et al. Endoscopic ultrasound-guided hepaticogastrostomy versus percutaneous transhepatic drainage for malignant biliary obstruction after failed endoscopic retrograde cholangiopancreatography: a retrospective expertise-based study from two centers. Ther Adv Gastroenterol. 2017;10:483–493. doi: 10.1177/1756283X17702096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Uemura R S, Khan M A, Otoch J P et al. EUS-guided choledochoduodenostomy versus hepaticogastrostomy: a systematic review and meta-analysis. J Clin Gastroenterol. 2018;52:123–130. doi: 10.1097/MCG.0000000000000948. [DOI] [PubMed] [Google Scholar]
- 5.Kunda R, Pérez-Miranda M, Will U et al. EUS-guided choledochoduodenostomy for malignant distal biliary obstruction using a lumen-apposing fully covered metal stent after failed ERCP. Surg Endosc. 2016;30:5002–5008. doi: 10.1007/s00464-016-4845-6. [DOI] [PubMed] [Google Scholar]


