Abstract
Rationale and objectives:
Kidney stones have been associated with an increased risk of ESRD. However, it is unclear if there is also an increased risk of mortality and if these risks are uniform across clinically distinct categories of stone formers.
Study Design:
Historical matched cohort study
Setting and Participants:
Stone formers in Olmsted County, Minnesota, between 1984 and 2012 identified using ICD-9 codes. Age and gender-matched individuals who had no codes for stones were the comparison group.
Predictor:
Stone formers were placed into 5 mutually exclusive categories after reviews of medical charts: incident symptomatic kidney, recurrent symptomatic kidney, asymptomatic kidney, bladder only, and miscoded (no stone).
Outcomes:
End-stage renal disease (ESRD), mortality, cardiovascular mortality, and cancer mortality.
Analytical Approach:
Cox proportional-hazards models with adjustment for baseline comorbidities
Results:
Overall, 65/6984 (0.93%) stone formers and 102/28044 (0.36%) non-stone formers developed ESRD over a mean follow up period of 12.0 years. After adjusting for baseline hypertension, diabetes mellitus, dyslipidemia, gout, obesity, and chronic kidney disease, the risk of ESRD was higher in recurrent symptomatic kidney (HR, 2.34; 95% CI, 1.08-5.077), asymptomatic kidney (HR, 3.94; 95% CI, 1.65-9.43) and miscoded (HR, 6.18; 95% CI, 2.25-16.93) stone formers, but not in incident symptomatic kidney or bladder stone formers. The adjusted risk of all-cause mortality was higher in asymptomatic kidney (HR, 1.40; 95% CI, 1.18-1.67) and bladder (HR, 1.37; 95% CI, 1.12-1.69) stone formers. Chart review of asymptomatic and miscoded stone formers suggested an increased risk of adverse outcomes related to diagnoses including urinary tract infection, cancer, and musculoskeletal or gastrointestinal pain.
Conclusions:
The higher risk of ESRD in recurrent symptomatic compared to incident symptomatic kidney stone formers suggests that stone events are associated with kidney injury. The clinical indication for imaging in asymptomatic stone formers, the correct diagnosis in miscoded stone formers, and the cause of a bladder outlet obstruction in bladder stone formers may explain the higher risk of ESRD or death in these groups.
Keywords: Kidney stones, bladder stones, chronic kidney disease (CKD), end-stage renal disease (ESRD), cardiovascular mortality, cancer mortality, all-cause mortality, kidney disease risk factor, recurrent stone formation, nephrolithiasis
Introduction
Kidney stone formers are at an increased risk for cardiovascular events, 1-3 chronic kidney disease (CKD), and end-stage renal disease (ESRD).4-7 If stone formers are at higher risk for cardiovascular and CKD complications, then a higher mortality rate may be expected as well. Stone formers also have an increased comorbidity burden with dyslipidemia,8 hypertension,8,9 diabetes, 8,10–12 and metabolic syndrome, 12-14 which results in a higher expected mortality rate.15 However, evidence that kidney stones directly lead to higher mortality, and moreover, higher mortality independent of these comorbidities, is lacking. Stone formers are a fairly heterogeneous population, and there may be certain subsets at higher risk for ESRD or mortality than others. Recurrent stone formers may be at higher risk of ESRD or mortality due to more kidney injury from obstructive nephropathy with stone events. Furthermore, if stone formers are at higher risk for mortality, it may primarily be cardiovascular mortality given the association of kidney stones with cardiovascular disease.1-3
Many studies rely on survey questions or administrative codes such as International Classification of Disease (ICD)-9 codes to study stone formers. Survey questions often lack the granular details regarding kidney stone events and are subject to recall bias or patient misconceptions about their disease. Administrative codes do not sufficiently distinguish between incident symptomatic, recurrent symptomatic, and asymptomatic kidney stone formers, and some, in fact, turn out to be miscoded/misdiagnosed.16 We previously found that symptomatic stone formers confirmed by chart review had a higher risk of ESRD, but had an insufficient sample size for meaningful subgroup analysis.5 Better categorization of stone formers in order to identify the subgroups at increased risk for ESRD or mortality may help with monitoring and preventative interventions in stone formers.
Thus, we studied a stone former cohort carefully characterized by chart review to assess ESRD and mortality risk compared to age- and gender-matched non-stone formers. Our primary goal was to determine ESRD and mortality risk among incident symptomatic kidney, recurrent symptomatic kidney, asymptomatic kidney, bladder, and miscoded stone formers. If mortality was found to be increased in stone formers, our secondary goal was to determine the attributed cause of mortality.
Methods
Study population
The Rochester Epidemiology Project ( REP) established in 1966 is a medical records-linkage system that covers almost the entire population of Olmsted County Minnesota.17 After obtaining Institutional Review Board approval with a waiver for informed consent, residents’ first documented urinary stone in Olmsted County, Minnesota between January 1st 1984 and December 31st 2012 were identified by International Classification of Diseases (ICD) - 9 codes 592 (calculus of kidney or urinary calculus), 594 (calculus of lower urinary tract), and 274.11 (uric acid nephrolithiasis). These codes do not effectively distinguish between bladder and kidney stones. Non-stone formers were randomly sampled from the population of Olmsted county residents who are were at risk for an incident stone at the time of the stone former’s index date (date of stone diagnosis), and were matched to each stone former (4:1 ratio) on age ±1 year and gender. Both stone formers and non-stone formers were followed for subsequent ESRD and mortality outcomes. Non-stone formers who developed a stone after their index date during follow-up were censored at that point as a non-stone former (occurred in 3%). They were hence included in the stone former cohort with their own matched non-stone formers.
Stone formers categories
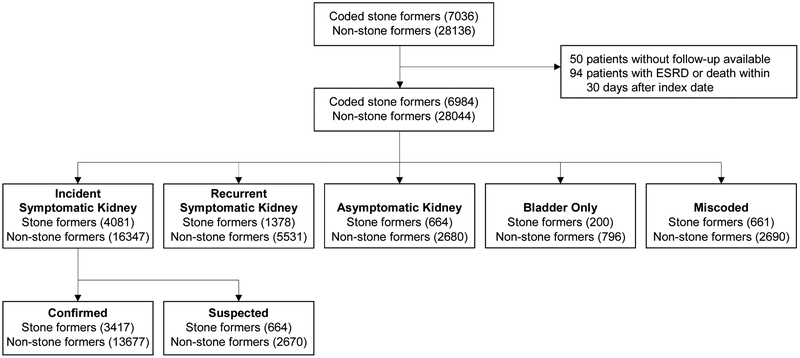
After chart review, stone formers were divided into five mutually exclusive categories (Figure 1): incident symptomatic kidney stone (first stone event during study period), recurrent symptomatic kidney stone (first stone event was prior to 1984 or residency in Olmsted County with recurrence in Olmsted County during the study period), asymptomatic kidney stone only (incidentally detected kidney stone on imaging in patients who did not have pain, gross hematuria, or ureteral obstruction from a stone), bladder stone only, and miscoded (not a urinary stone former). Symptomatic kidney stone formers were required to have abdominal pain and/or gross hematuria attributed to an obstructing kidney stone or to have a urinary tract infection attributed to the kidney stone (struvite composition or urine pH > 7.0). Incident symptomatic kidney stone formers were further subdivided into those that were confirmed (stone obstructing ureter on imaging or seen after passage) or suspected (clinical diagnosis with symptoms due to presumed stone passage but stone never imaged or seen after passage). In a random sample of 100 asymptomatic kidney stone formers and 100 miscoded stone formers, charts were reviewed to determine the reason imaging was obtained and the correct diagnoses, respectively.
Figure 1.
Stone former and non-stone former cohorts studied (sample size)
Comorbidities
Comorbidities known to be associated with kidney stones and ESRD were identified from ICD-9 codes. These included hypertension, diabetes mellitus, obesity, dyslipidemia, gout, and CKD (Table S1). Comorbidities were considered baseline (prevalent) if they occurred prior to the index date.
Outcomes
All ESRD events (i.e. renal replacement therapy in the form of maintenance dialysis or kidney transplantation) through August 20, 2015 were identified via a query conducted in the United States Renal Data System, a comprehensive national database which collects, analyzes, and distributes information about ESRD in the United States.18 Both Olmsted County stone formers and non-stone formers were matched with the USRDS database. Charts were manually reviewed for validation of ESRD events in all stone formers and non-stone formers to determine the perceived primary cause of ESRD, and to identify cardiovascular and urological comorbidities present before the development of ESRD. If the primary cause of ESRD could not be determined from chart review, the primary cause listed in the USRDS database was used.
Mortality data was obtained from the REP database (which captures death certificates from Minnesota and the National Death Index). The underlying cause of death was grouped based upon the death certificate as follows: cardiovascular if “heart disease”, “cerebrovascular disease”, “peripheral vascular disease”, “aneurysm”, or other related terms were listed; or cancer if “neoplasm”, “malignancy”, “lymphoma”, “leukemia”, “carcinoma”, or other related terms were listed. Urinary tract cancers were also identified by cancers of the kidney, ureter, bladder, or urethra.
Statistical Analyses
Persons with prevalent ESRD (defined as before or within 30 days after the index date) or death within 30 days after the index date were excluded from all analyses. Because of these exclusions, matching was not retained in analyses. Analyses were performed separately for each category of stone former compared to their matched non-stone formers. Comparisons of baseline characteristics between stone formers and non-stone formers were assessed using the equal variance t-test for continuous variables and the Chi-square test for categorical variables. Event rates were calculated for stone formers and non-stone formers per 1000 person-years of follow-up. The association of stone formers with subsequent ESRD events was assessed using Cox proportional hazards models, both with and without adjustment for baseline comorbidities. Patients without ESRD were censored at death or August 20, 2015, whichever came first. Risk of ESRD was also assessed after stratifying by gender, given reported gender differences in the risk of ESRD.19 Models also evaluated the association of stone formers with all-cause mortality, cardiovascular mortality, and cancer mortality as events of interest, respectively, and were censored on death from other cause or August 20, 2015, whichever came first. Additional analyses assessed the risk of ESRD using Fine and Gray competing risk regression models, with death from any cause considered as a competing event. Hazard ratios and 95% confidence intervals were reported. The proportional hazards assumption was tested using Schoenfeld Residuals and was found to hold for all models. All analysis used SASv9.4 software (SAS Institute, Cary, NC).
Results
Characteristics of the cohort
There were 6984 coded stone formers and 28,044 matched non-stone formers studied. Coded stone formers categories were as follows: 49% confirmed incident symptomatic kidney, 9.5% suspected incident symptomatic kidney, 20% recurrent symptomatic kidney, 9.6% asymptomatic kidney, 2.8% bladder only, and 9.6% miscoded stone formers (Figure 1). The mean follow up period was 12.0 years in both stone formers and controls. Due to matching, stone formers and non-stone formers were similar in age and gender (Table 1). Stone formers were more likely to be obese, and all stone former categories except bladder stones were more likely to have hypertension or CKD. Incident and recurrent symptomatic kidney stone formers and bladder stone formers were more likely to have a history of diabetes. Dyslipidemia was more likely in symptomatic, asymptomatic, and miscoded stone formers. Gout was more likely in incident and recurrent symptomatic kidney stone formers.
Table 1.
Baseline characteristics of stone formers and age- and gender-matched non-stone formers by stone former category
| Incident symptomatic | Recurrent symptomatic | Asymptomatic | Bladder | Miscoded | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SF (n=4081) |
Non-SF (n=16347) |
P- value |
SF (n=1378) |
Non-SF (n=5531) |
P- value |
SF (n=664) |
Non-SF (n=2680) |
P- value |
SF (n=200) |
Non- SF (n=796) |
P- value |
SF (n=661) |
Non-SF (n=2690) |
P- value |
|
| Age, y | 46 (17) |
46 (17) |
0.9 | 50 (18) |
50 (18) |
0.8 | 55 (19) |
55 (19) |
0.9 | 67 (19) |
67 (19) |
0.8 | 47 (22) |
47 (22) |
0.9 |
| Male sex | 2399 (58.8%) |
9598 (58.7%) |
0.9 | 874 (63.4%) |
3498 (63.2%) |
0.9 | 299 (45.0%) |
1210 (45.1%) |
0.9 | 170 (85.0%) |
672 (84.4%) |
0.8 | 278 (42.1%) |
1122 (41.7%) |
0.9 |
| Diabetes | 373 (9.1%) |
1037 (6.3%) |
<0.001 | 152 (11.0%) |
419 (7.6%) |
<0.001 | 80 (12.0%) |
289 (10.8%) |
0.4 | 31 (15.5%) |
77 (9.7%) |
0.02 | 61 (9.2%) |
201 (7.5%) |
0.1 |
| Hypertension | 990 (24.3%) |
3111 (19.0%) |
<0.001 | 422 (30.6%) |
1281 (23.2%) |
<0.001 | 262 (39.5%) |
837 (31.2%) |
<0.001 | 81 (40.5%) |
264 (33.2%) |
0.05 | 194 (29.3%) |
616 (22.9%) |
<0.001 |
| CKD | 91 (2.2%) |
210 (1.3%) |
<0.001 | 44 (3.2%) |
103 (1.9%) |
0.002 | 39 (5.9%) |
57 (2.1%) |
<0.001 | 11 (5.5%) |
38 (4.8%) |
0.7 | 35 (5.3%) |
46 (1.7%) |
<0.001 |
| Obesity | 922 (22.6%) |
2246 (13.7%) |
<0.001 | 225 (16.3%) |
708 (12.8%) |
<0.001 | 146 (22.0%) |
453 (16.9%) |
0.002 | 29 (14.5%) |
71 (8.9%) |
0.02 | 149 (22.5%) |
351 (13.0%) |
<0.001 |
| Dyslipidemia | 1286 (31.5%) |
4054 (24.8%) |
<0.001 | 436 (31.6%) |
1612 (29.1%) |
0.07 | 273 (41.1%) |
950 (35.4%) |
0.007 | 72 (36.0%) |
248 (31.2%) |
0.2 | 208 (31.5%) |
727 (27.0%) |
0.03 |
| Gout | 129 (3.2%) |
305 (1.9%) |
<0.001 | 63 (4.6%) |
135 (2.4%) |
<0.001 | 26 (3.9%) |
75 (2.8%) |
0.1 | 10 (5.0%) |
38 (4.8%) |
0.9 | 29 (4.4%) |
48 (1.8%) |
<0.001 |
Note: values for continuous variables given as mean (SD); for categorical variables as count (percentage).
SF, stone former; CKD, chronic kidney disease;
P-values were derived using the equal variance t-test for continuous variables and the Chi-square test for categorical variables. Bolding indicates significant P values.
Clinical presentation of asymptomatic and miscoded stone formers
Clinical presentations that led to incidental discovery of kidney stones on imaging in a random subset of patients are shown in Table 2. Microscopic hematuria (26%), recurrent urinary tract infection (10%), and a variety of cancers were the more common indications for kidney imaging that led to detection of a stone. The correct diagnoses for miscoded stone formers in a random subset of patients are shown in Table 3. Urinary tract infection (23%), musculoskeletal back pain (17%), obstructive uropathy from prostate pathology or a neurogenic bladder (12%), and gastrointestinal pain (9%) were the more common correct diagnoses in these patients without kidney or bladder stones.
Table 2.
Imaging indications for asymptomatic (incidental) kidney stone formers based on review of 100 random charts
| Indications for imaging in asymptomatic stone formers | No. of patients |
|---|---|
| Microscopic hematuria (no gross hematuria) | 26 |
| Recurrent urinary tract infection (not attributed to stone) | 10 |
| Follow up of urothelial cancer | 8 |
| Follow up of renal cell cancer | 6 |
| Follow up of prostate cancer | 5 |
| Follow up of pancreatic cancer/ pancreatitis /colon cancer | 5 |
| Follow up of liver cirrhosis | 5 |
| Benign prostate hyperplasia post-surgical hematuria | 4 |
| Neurogenic bladder with urinary retention | 3 |
| Other | 28 |
Table 3.
Correct diagnosis for patients miscoded as kidney or bladder stone formers after review of 100 random charts
| Correct diagnosis on chart review | No. of patients |
|---|---|
| Urinary tract infection | 23 |
| Musculoskeletal back pain | 17 |
| Obstructive uropathy due to benign prostate hyperplasia, prostate cancer, or neurogenic bladder |
12 |
| Gastrointestinal colic or pain due to small bowel obstruction, ileus, irritable bowel syndrome, colitis, diverticulitis, cholangitis, or cholecystitis |
9 |
| Ureteral stenosis or stricture | 8 |
| Urothelial carcinoma of bladder or ureter | 7 |
| Renal cysts | 4 |
| Others | 20 |
Risk of ESRD and mortality
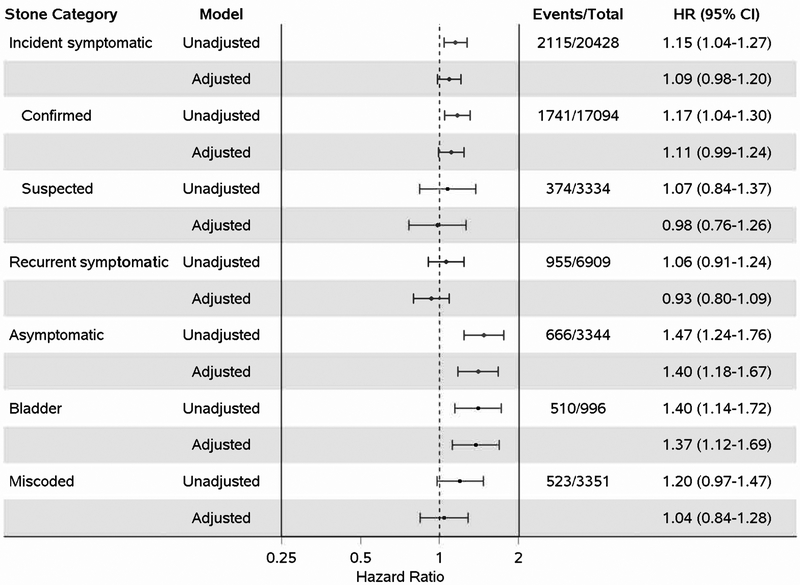
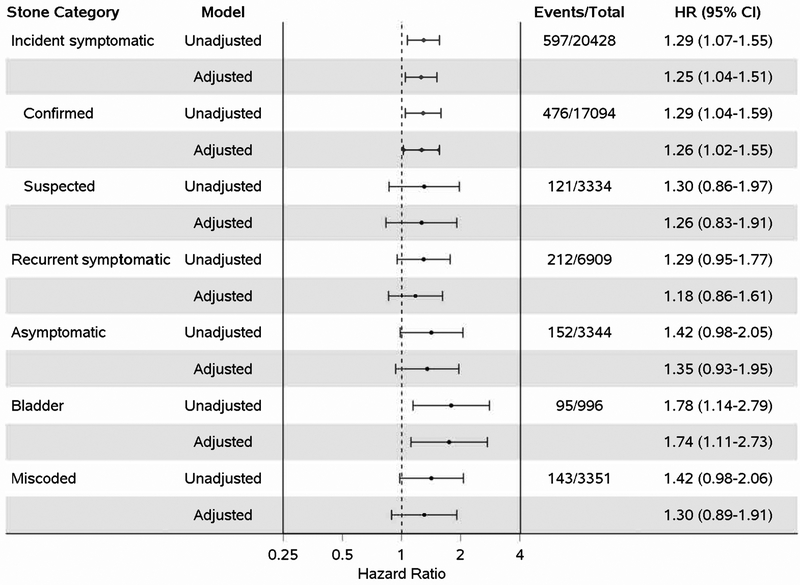
Overall, 65 stone formers (0.93%) and 102 non-stone formers (0.36%) developed ESRD. After adjustment for comorbidities, the risk of ESRD was significantly higher in recurrent symptomatic kidney, asymptomatic kidney, and miscoded stone formers (Figure 2). Findings were similar when death was modeled as a competing risk (Table S2) and there was no clear evidence of gender differences in risk of ESRD with stone formers (Table S3) Overall, 1083 stone formers (16%) and 3686 non-stone formers (13%) died. After adjustment for comorbidities, the risk of mortality was significantly higher in asymptomatic kidney, and bladder stone formers. (Figure 3). The ESRD and mortality event rates per 1000 person years show modest absolute differences between stone formers and non-stone formers (Table 4).
Figure 2.
Unadjusted and adjusted HRs and 95% confidence intervals for risk of end-stage renal disease by stone former category. Adjusted for chronic kidney disease, hypertension, diabetes mellitus, dyslipidemia, obesity and gout.
Figure 3.
Unadjusted and Adjusted HRs and 95% confidence intervals for all-cause mortality by stone former category. Adjusted for chronic kidney disease, hypertension, diabetes mellitus, dyslipidemia, obesity and gout.
Table 4.
Event rates for ESRD, overall mortality, and cancer mortality for stone formers and age- and gender-matched non-stone formers by stone former category
| ESRD event rate per 1000 person-years |
Mortality event rate per 1000 person-years |
Cancer mortality event rate per 1000 person-years |
||||
|---|---|---|---|---|---|---|
| Stone Category | SF | Non-SF | SF | Non-SF | SF | Non-SF |
| Incident symptomatic | 0.54 | 0.30 | 9.45 | 8.21 | 2.91 | 2.26 |
| Confirmed | 0.55 | 0.30 | 9.82 | 8.40 | 2.89 | 2.25 |
| Suspected | 0.50 | 0.28 | 7.97 | 7.42 | 2.99 | 2.30 |
| Recurrent symptomatic | 0.65 | 0.24 | 11.89 | 11.22 | 3.08 | 2.38 |
| Asymptomatic | 1.87 | 0.36 | 26.30 | 17.88 | 5.88 | 4.11 |
| Bladder | 1.69 | 1.35 | 67.00 | 47.84 | 15.20 | 8.32 |
| Miscoded | 1.50 | 0.18 | 14.81 | 12.40 | 4.61 | 3.25 |
SF, stone former; ESRD, end-stage renal disease
Risk of cause-specific mortality
Cause specific mortality was evaluated using the underlying diagnoses on patients’ death certificates. Overall, 262 stone formers (3.8%) and 1105 non-stone formers (3.9%) had deaths attributed to cardiovascular disease. No category of stone former was associated with a higher risk of cardiovascular mortality (Table S4). Overall, 300 stone formers (4.3%) and 899 non-stone formers (3.2%) had deaths attributed to cancer. After adjustment for comorbidities, the risk of cancer mortality was higher in incident symptomatic kidney and bladder stone formers (Figure 4). Overall, only 17 stone formers and 33 non-stone formers had their deaths attributed to kidney or urinary tract cancers. The cancer mortality event rates per 1000 person years show modest absolute differences between stone formers and non-stone formers (Table 4).
Figure 4.
Unadjusted and Adjusted HRs and 95% confidence intervals for cancer mortality by stone former category. Adjusted for chronic kidney disease, hypertension, diabetes mellitus, dyslipidemia, obesity and gout.
Discussion
In this cohort of carefully validated and classified stone formers matched to non-stone formers, several key findings regarding ESRD and morality outcomes were evident. First, recurrent symptomatic kidney stone formers were at higher risk of ESRD compared to non-stone formers both before and after adjustment for other comorbidities, while increased risk of ESRD in incident symptomatic kidney stone formers was only significant in the unadjusted analysis. Second, asymptomatic kidney stone formers and miscoded stone formers have underlying medical conditions such as urinary tract infections, cancers, and gastrointestinal diseases that led to incidental detection of kidney stones with abdominal imaging or were misdiagnosed as kidney stones. These medical conditions, rather than kidney stones, likely explain the increased risk of ESRD or mortality. Third, the cause of the increased mortality observed in the stone formers compared to non-stone formers was more related to cancer than cardiovascular disease, and the increased cancer mortality was not specifically urinary tract cancers.
Although it is unclear precisely how kidney stones lead to an increased risk of ESRD, the most plausible mechanism could involve acute kidney injury from obstructive uropathy. Although known risk factors for ESRD such as hypertension, diabetes mellitus, dyslipidemia, obesity, gout, and CKD were more common in stone formers, adjustment for these comorbidities only slightly attenuated the increased ESRD risk among recurrent symptomatic kidney stone formers. The current study also suggests that the risk of ESRD is of more concern among recurrent compared to incident symptomatic stone formers. Recurrent stone formers might accrue incremental kidney injury with each stone event. Therefore, treatments to prevent kidney stone recurrence may be beneficial for delaying CKD progression, especially since kidney stone events are associated with reduction in GFR and rises in proteinuria.20
Since all-cause mortality risk was increased in asymptomatic kidney stone formers and bladder stone formers, even after adjustment for comorbidities, we also investigated cause-specific mortality. Several studies have reported an association between kidney stones and cardiovascular events including hypertension9, coronary artery disease2, and MI.3 Surprisingly, we did not find a higher risk of cardiovascular mortality in any category of stone former. However, cancer mortality was higher in incident symptomatic kidney stone formers as well as in bladder stone formers. Bladder stones are known to occur with a bladder outlet obstruction, which is commonly due to prostate cancer.21 Studies have reported associations between kidney stones and urinary tract cancers,21-23 but misdiagnosis of urinary tract cancer as a kidney stone has been a concern as we confirmed with manual chart review of miscoded stone formers. Kidney or urinary tract cancer mortality was too rare in our cohort to explain the increased risk of cancer mortality detected. Consistent with our finding, a large study from Taiwan found a higher risk of systemic cancers involving head and neck, gastrointestinal tract, lung, breast, thyroid and hematologic origin in addition to urinary tract cancers in stone formers when compared to the general population.24 The exact mechanism driving the higher risk of cancer mortality in stone formers is unclear. One speculative pathogenic mechanism is that local irritation and inflammation contributes to chronic systemic inflammation and cytokine release which promote tumorigenesis.24 Notably, our study could not address whether “onset” of cancer in those with cancer mortality occurred before or after kidney stones. Hypercalcuria can occur in cancer via a variety of mechanisms and hypercalcuria can cause kidney stones. Thus, the increased risk of cancer mortality may simply be hypercalcuria from cancer causing kidney stones rather than kidney stones causing cancer.
Strengths of our study include a relatively large cohort of chart-validated and categorized stone formers with age- and gender-matched non-stone formers with long-term assessment for ESRD and mortality. By separately analyzing asymptomatic, bladder, and miscoded stone formers, we avoided attributing ESRD or mortality risk from these stone types to symptomatic kidney stones. Limitations include the observational nature of the findings, reliance on administrative codes for comorbidities, and lack of medication data. We could not include asymptomatic stones or symptomatic stones events prior to 1984 or residency in Olmsted county in the analysis as we lacked those medical records. There was limited power and ability for multivariable adjustment with the few ESRD events. Death certificates also have limited accuracy for determining the underlying cause of death.
In summary, this carefully validated cohort study provides evidence that recurrent symptomatic kidney stones are associated with increased risk of ESRD. This risk for ESRD in recurrent rather than incident symptomatic stone formers suggests strategies to prevent stone recurrence may be of benefit. This study also demonstrated the benefits of careful chart validation when studying kidney stone disease instead of relying on administrative codes. In particular, miscoded and asymptomatic kidney stone formers can be at risk for morbidity and mortality from diseases that were misdiagnosed as kidney stones or from diseases that led to imaging with incidental detection of kidney stones.
Supplementary Material
Acknowledgments
Support: This project was supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases (Mayo Clinic O’Brien Urology Research Center: DK100227 and DK83007 and a K23 DK109134) and made possible by the Rochester Epidemiology Project (AG034676) from the National Institutes of Health, U.S. Public Health Service. The funding agency played no role in study design, data collection, analysis, interpretation, writing, or publishing.
Footnotes
Supplementary Material
Table S1. Diagnostic codes for comorbid conditions.
Table S2. Risk of ESRD in each stone former category with death as a competing risk.
Table S3. Risk of ESRD in each stone former category, stratified by sex.
Table S4. Risk of cardiovascular mortality in each stone former category.
Authors’ Contributions: research idea and study design: AR, JL, TD, WK; data acquisition: TD, WK, RM, AR; data analysis/interpretation: AR, JL, TD, WK, LH, FE, LV; statistical analysis: FE, LV, JC, TD, AR; supervision or mentorship: AR, JL. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Financial Disclosure: The authors declare that they have no relevant financial interests.
Disclaimer: Data reported here have been supplied by the United States Renal Data System (USRDS). The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy or interpretation of the U.S. government.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Alexander RT, Hemmelgarn BR, Wiebe N, et al. Kidney stones and cardiovascular events: a cohort study. Clin J Am Soc Nephrol. 2014;9(3):506–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferraro PM, Taylor EN, Eisner BH, et al. History of kidney stones and the risk of coronary heart disease. JAMA. 2013;310(4):408–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rule AD, Roger VL, Melton LJ 3rd, et al. Kidney stones associate with increased risk for myocardial infarction. Journal of the American Society of Nephrology. 2010;21(10):1641–1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhe M, Hang Z. Nephrolithiasis as a risk factor of chronic kidney disease: a meta-analysis of cohort studies with 4,770,691 participants. Urolithiasis. 2017;45(5):441–448. [DOI] [PubMed] [Google Scholar]
- 5.El-Zoghby ZM, Lieske JC, Foley RN, et al. Urolithiasis and the risk of ESRD. Clinical journal of the American Society of Nephrology : CJASN. 2012;7(9): 1409–1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alexander RT, Hemmelgarn BR, Wiebe N, et al. Kidney stones and kidney function loss: a cohort study. Bmj. 2012;345:e5287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shoag J, Halpern J, Goldfarb DS, Eisner BH. Risk of Chronic and End Stage Kidney Disease in Patients with Nephrolithiasis. The Journal of urology. 2014;192(5):1440–5. [DOI] [PubMed] [Google Scholar]
- 8.Rule AD, Bergstralh EJ, Melton LJ 3rd, Li X, Weaver AL, Lieske JC. Kidney stones and the risk for chronic kidney disease. Clin J Am Soc Nephrol. 2009;4(4):804–811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kittanamongkolchai W, Mara KC, Mehta RA, et al. Risk of Hypertension among First-Time Symptomatic Kidney Stone Formers. Clin J Am Soc Nephrol. 2017;12(3):476–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weinberg AE, Patel CJ, Chertow GM, Leppert JT. Diabetic severity and risk of kidney stone disease. Eur Urol. 2014;65(1):242–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taylor EN, Stampfer MJ, Curhan GC. Diabetes mellitus and the risk of nephrolithiasis. Kidney Int. 2005;68(3):1230–1235. [DOI] [PubMed] [Google Scholar]
- 12.Scales CD Jr., Smith AC, Hanley JM, Saigal CS Prevalence of kidney stones in the United States. European urology. 2012;62(1):160–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Taylor EN, Stampfer MJ, Curhan GC. Obesity, weight gain, and the risk of kidney stones. Jama. 2005;293(4):455–462. [DOI] [PubMed] [Google Scholar]
- 14.Liu YT, Yang PY, Yang YW, Sun HY, Lin IC. The association of nephrolithiasis with metabolic syndrome and its components: a cross-sectional analysis. Ther Clin Risk Manag. 2017;13:41–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aydin H, Yencilek F, Erihan IB, Okan B, Sarica K. Increased 10-year cardiovascular disease and mortality risk scores in asymptomatic patients with calcium oxalate urolithiasis. Urol Res. 2011;39(6):451–458. [DOI] [PubMed] [Google Scholar]
- 16.Kittanamongkolchai W, Vaughan LE, Enders FT, et al. The Changing Incidence and Presentation of Urinary Stones Over 3 Decades. Mayo Clin Proc. 2018;93(3):291–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.St Sauver JL, Grossardt BR, Yawn BP, et al. Data Resource Profile: The Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol. 2012:41(6): 1614–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saran R, Robinson B, Abbott KC, et al. US Renal Data System 2016 Annual Data Report: Epidemiology of Kidney Disease in the United States. Am J Kidney Dis. 2017;69(3 Suppl 1): A7–A8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Keddis MT, Rule AD. Nephrolithiasis and loss of kidney function. Curr Opin Nephrol Hypertens. 2013;22(4):390–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haley WE, Enders FT, Vaughan LE, et al. Kidney Function After the First Kidney Stone Event. Mayo Clin Proc. 2016;91(12):1744–1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chung SD, Liu SP, Lin HC. Association between prostate cancer and urinary calculi: a population-based study. PLoS One. 2013;8(2):e57743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cheungpasitporn W, Thongprayoon C, O'Corragain OA, et al. The risk of kidney cancer in patients with kidney stones: a systematic review and meta-analysis. QJM. 2015;108(3):205–212. [DOI] [PubMed] [Google Scholar]
- 23.Chung SD, Tsai MC, Lin CC, Lin HC. A case-control study on the association between bladder cancer and prior bladder calculus. BMC Cancer. 2013. ;13:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shih CJ, Chen YT, Ou SM, Yang WC, Chen TJ, Tarng DC. Urinary calculi and risk of cancer: a nationwide population-based study. Medicine (Baltimore). 2014;93(29):e342. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.