Abstract
Obesity increases risk of falling, but the effect of bariatric surgery on fall-related injuries is unknown. The aim of this study was therefore to study the association between bariatric surgery and long-term incidence of fall-related injuries in the prospective, controlled Swedish Obese Subjects study. At inclusion, body-mass index was ≥34 kg/m2 in men and ≥38 kg/m2 in women. The surgery per-protocol group (n=2007) underwent gastric bypass (n=266), banding (n=376) or vertical banded gastroplasty (n=1365), and controls (n=2040) received usual care. At the time of analysis (December 31, 2013), median follow-up was 19 years (maximal 26 years). Fall-related injuries requiring hospital treatment were captured using data from the Swedish National Patient Register. During follow-up, there were 617 first-time fall-related injuries in the surgery group and 513 in the control group (adjusted hazard ratio (adjHR 1.21, 95% CI, 1.07 to 1.36; P=0.002). The incidence differed between treatment groups (P<0.001, log-rank test) and was higher after gastric bypass than after usual care, banding and vertical banded gastroplasty (adjHRs 0.50-0.52, P<0.001 for all three comparisons). In conclusion, gastric bypass surgery was associated with increased risk of serious fall-related injury requiring hospital treatment.
Introduction
Obesity is associated with premature mortality and increased risk for serious diseases such as type 2 diabetes, cardiovascular disease and cancer.1 In addition, studies have shown associations between obesity and falls in older and middle-aged adults,2-5 as well as in younger adults with obesity.6 While it is well established that bariatric surgery promotes sustained weight loss and improves several obesity-related comorbidities,7 it is not known whether it affects the long-term risk of a fall-related injury.
In the short term, bariatric surgery improves functional capacity8 and balance control,9 suggesting that the risk of falling may be reduced; however, to date there are no studies that support this hypothesis. On the contrary, a small, two-year, randomized controlled study in individuals with obesity and type 2 diabetes reported seven serious falls in those who had undergone gastric bypass but only three serious falls in the lifestyle group, suggesting that the risk of falling may in fact be increased after bariatric surgery.10
Fall-related injuries often infer large costs for both society and the affected individuals, and the long-term consequences can be extensive and seriously affect independence and quality of life.4, 11, 12 The aim of this study was therefore to examine whether the long-term risk of fall-related injury is altered after gastric bypass, banding or vertical banded gastroplasty compared to conventional obesity care.
Methods
Study design and treatment
The SOS study has previously been described (for details see Supplementary Appendix).13 In brief, the surgery group consists of 2010 subjects who chose surgical treatment, and the control group consists of 2037 individuals matched for 18 variables. The study groups had identical inclusion and exclusion criteria. The inclusion criteria were an age of 37-60 years and a body-mass index (BMI) of ≥34 kg/m2 in men and ≥38 kg/m2 in women before or at the time of the matching examination. The exclusion criteria were those that were relevant for the participants’ suitability for surgery. Seven regional ethics review boards (Gothenburg, Lund, Linköping, Örebro, Karolinska Institute, Uppsala, Umeå) approved the study, and written or oral informed consent was obtained from all participants. The study has been registered at ClinicalTrials.gov (NCT01479452).
In this study, data were analyzed per protocol. The intended surgical intervention was not performed in four patients. Three of these patients never underwent surgery and in the per-protocol analyses used in the current study they are therefore included in the control group. One patient was scheduled for a vertical banded gastroplasty but instead underwent a gastric bypass procedure and is therefore included in the gastric bypass group in per-protocol analyses. In the surgery per-protocol group (n=2007), participants underwent gastric bypass (n=266), banding (n=376) or vertical banded gastroplasty (n=1365). The control per-protocol group (n=2040) received the customary treatment for obesity at their primary health care centers (see Table 1 in Supplementary Appendix).
Outcomes and follow-up
During follow-up, fall-related injury events were identified by searching the Swedish National Patient Register, which contains information on hospital stays and hospital-based outpatient care, using International Classification of Diseases (ICD) 8/9 (E826, E880-E888) and 10 codes (V01-V19, W00-W19).14 Fall-related injuries before entering the study were identified by searching for falls treated in hospital in the 12 months before inclusion.14 At the time of register linkage, the register was complete until December 31, 2013.
Statistical methods
Mean values and standard deviations were used for baseline characteristics of the participants. Differences between group means and proportions were analyzed with analysis of covariance (continuous variables) and logistic regression (dichotomous variables).
Time to first fall-related injury event was calculated from the date of inclusion into the study. Those who were never assigned a fall-related ICD code were censored at Dec 31, 2013, at date of emigration, or at date of death. Time of progression to first event after inclusion in the different treatment subgroups was compared with Kaplan-Meier estimates of cumulative incidence rates. Log-rank test was used to analyze differences in cumulative incidence. Cox proportional-hazards models were used to evaluate differences between groups while adjusting for preselected baseline risk factors (fall-related injuries during 12 months prior to inclusion, age, sex, diabetes, alcohol use smoking and depression). Total event rate taking into account recurrent falls (defined as hospitalizations more than 30 days apart) were evaluated with time to event methods.
Participants who underwent surgery during follow-up were identified using the National Patient Register and SOS questionnaires (at baseline and after 0.5, 1, 2, 3, 4, 6, 8, 10, 15 and 20 years) and censored at the time of surgery if it resulted in change of treatment group. All P values are two-sided, and P values of less than 0.05 were considered to indicate statistical significance. All statistical analyses were performed using Stata (version 12.1).
Results
Baseline characteristics and weight changes during follow-up
Patients in the surgery group were one year younger than the patients in the control group, while most metabolic risk factors were worse in the surgery group. Among surgical subgroups, patients in the gastric bypass group were heavier, had higher cholesterol levels and higher systolic blood pressure and higher rates of type 2 diabetes than those in the vertical banded gastroplasty and banding groups, while there was no significant difference in fall-related injuries in the year before study start (Table in Supplementary Appendix).
On the date of analysis, the follow-up time was up to 26 years, with a median of 19 years (interquartile range 15-21 years). During follow-up, two participants in the surgery group withdrew consent and were censored immediately after the date of inclusion. In addition, 23 patients in the control group and 26 in the surgery group emigrated and were censored at the date of emigration.
At the two-year follow-up the relative weight loss in the gastric bypass, vertical banded gastroplasty and banding subgroups were 31.6, 22.4 and 21.1 %, respectively. The weight change in the control group was minimal (weight increase 0.1%).
Incidence of fall-related injuries during follow-up
There were 513 first-time fall-related injuries in the control group and 617 in the surgery group during follow-up (Figure 1A), and the unadjusted hazard ratio with surgery was 1.19 (95% CI, 1.06 to 1.33; P=0.004). After multivariable adjustments, the hazard ratio was 1.21 (95% CI, 1.07 to 1.36; P=0.002).
Figure 1.
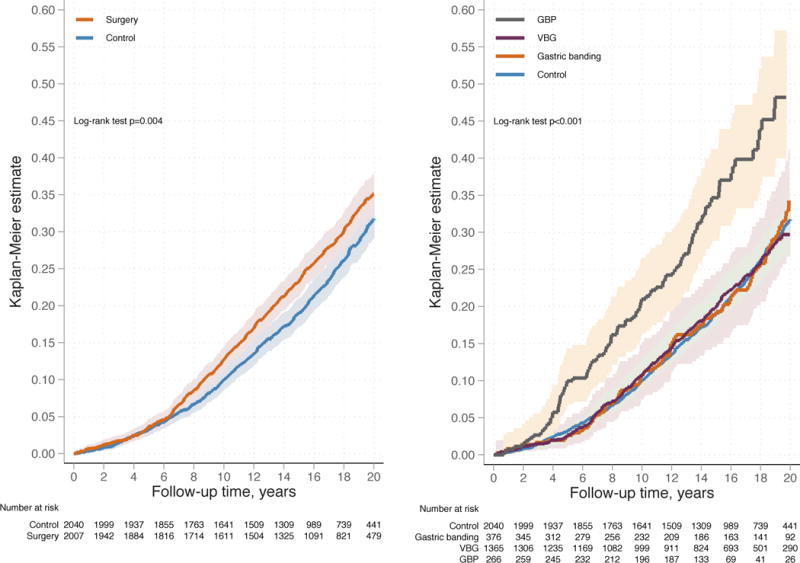
Cumulative incidence of first time fall-related injuries during follow-up in the bariatric surgery group and the control group (panel A) and divided by the method of treatment (panel B). Observations were censored at time of surgery if it resulted in change of treatment group (control patients who underwent bariatric surgery and patients in the surgery group who underwent surgical re-instatement during follow-up were censored at the time of surgery in panel A; reoperations resulting in change of surgical group were additionally censored in panel B). GBP, gastric bypass; VBG, vertical banded gastroplasty. The shaded areas represent the 95 percent confidence intervals.
During follow-up, there was a significant difference in the incidence of first-time fall-related injuries between treatment groups (P<0.001, log-rank test) with higher incidence after gastric bypass compared to the other two surgical groups and controls (Figure 1B, Table 1). Compared to the gastric bypass group, the adjusted hazard ratio for the control group was 0.50 (P<0.001) and 0.51-0.52 (P<0.001) for the other two surgical groups (Table 1).
Table 1.
Hazard Ratios for the Incidence of Fall-Related Injuries.
| Control (N=2040) |
Banding (N=376)b |
VBG (N=1365)b |
GBP (N=266)b |
|
|---|---|---|---|---|
| Number of first fall events | 513 | 84 | 324 | 100 |
| Person-years | 31148 | 4954 | 19742 | 3512 |
| Incidence rate per 1000 person-years (95% CI) | 16.5 (15.1-18.0) | 17.0 (13.7-21.0) | 16.4 (14.7-18.3) | 28.5 (23.4-34.6) |
| HR, unadjusted (95% CI) | 0.52 (0.42-0.65) | 0.54 (0.40-0.72) | 0.52 (0.42-0.66) | 1.0 (reference) |
| HR, adjusteda (95% CI) | 0.50 (0.40-0.62) | 0.52 (0.39-0.69) | 0.51 (0.41-0.64) | 1.0 (reference) |
| Total number of fall events | 886 | 128 | 600 | 235 |
| Person-years | 31949 | 5110 | 20328 | 3763 |
| Incidence rate per 1000 person-years (95% CI) | 27.7 (26.0-29.6) | 25.1 (21.1-29.8) | 29.5 (27.2-32.0) | 62.5 (55.0-71.0) |
| HR, unadjusted (95% CI) | 0.39 (0.30-0.51) | 0.35 (0.25-0.49) | 0.42 (0.32-0.55) | 1.0 (reference) |
| HR, adjusteda (95% CI) | 0.38 (0.29-0.49) | 0.34 (0.24-0.47) | 0.41 (0.31-0.54) | 1.0 (reference) |
Adjusted for fall-related injuries 12 months prior to inclusion, age, sex, diabetes, alcohol use and smoking and depression at baseline.
Censored at time of reoperation if it resulted in change of surgery group. CI, confidence interval; VBG, vertical banded gastroplasty; GBP, gastric bypass.
When also considering recurrent falls during follow-up, the adjusted hazard ratios for control, banding and vertical banded gastroplasty groups compared to the gastric bypass group were 0.38, 0.34 and 0.41, respectively (Table 1).
Sensitivity analysis
The gastric bypass group had a higher rate of type 2 diabetes at baseline and previous studies suggest an increased risk of falling in patients with type 2 diabetes.15 We therefore examined the incidence of fall-related injuries in groups of patients with or without type 2 diabetes at baseline (Figure 1 in Supplementary Appendix). This analysis showed that the incidence of fall-related injuries was higher in the gastric bypass group compared to other treatment groups regardless of diabetes status at baseline.
Discussion
In this prospective controlled long-term study, we showed that bariatric surgery, compared with usual obesity care, was associated with increased incidence of fall-related injuries severe enough to cause hospital visits. However, the risk of suffering a first-time fall-related injury was doubled in obese patients treated by gastric bypass compared to controls. By contrast, the risk of suffering a fall-related injury was not changed in patients who underwent banding or vertical banded gastroplasty, suggesting that weight loss per se does not alter the risk of falling and that the risk of falling remains higher compared to normal weight individuals even after substantial weight loss. Our study confirms and extends observations from an earlier very small study showing that serious falls are more common after gastric bypass surgery compared to intensive lifestyle treatment of diabetes,10 and is also consistent with reports suggesting that gastric bypass patients have an increased risk of dying from external causes such as accidents.16-18
Bariatric surgery procedures have changed over time and gastric bypass, which has long been considered to be the gold standard, is being gradually replaced by the sleeve gastrectomy technique. Nevertheless, a very large number of patients worldwide have undergone this procedure. It is unclear why fall risk is increased after gastric bypass, however, compared to restrictive procedures, it is associated with higher risk of micronutrient deficiency-related neurological complications,19 hypoglycemia,20 and dependence syndromes, in particular alcohol use disorders.16, 21
The SOS study and our analysis have some limitations. The SOS study was not randomized and fall-related injury was not a pre-specified endpoint. The Swedish National Patient Register used to trace fall-related injuries only contains inpatient data and for this reason, we could have missed minor fall-related injuries treated in primary care. Despite these limitations, the study is, to our knowledge, the best available source of data for evaluation of rare, long-term side effects after bariatric surgery.
In conclusion, our results show that gastric bypass, but not banding or vertical banded gastroplasty, increases the risk for fall-related injury and suggest that post-surgery care needs to be optimized to reduce this risk.
Supplementary Material
Acknowledgments
We thank the staff members at 480 primary health-care centers and 25 surgical departments in Sweden that participated in the study. We acknowledge Gerd Bergmark, Christina Torefalk, and Björn Henning for invaluable administrative support and Rosie Perkins for editing the manuscript.
Funding: Research reported in this publication was supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under Award Number R01DK105948. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Authors of this study were also supported by the Swedish Research Council (K2013-54X-11285-19 and 2016-00522), Västra Götaland Region ALF research grants and the Swedish Diabetes Foundation. The Wallenberg Centre for molecular and translational medicine (C.M.) is partly funded by AstraZeneca. The funders had no role in the interpretation of these data or in the writing of this article.
Footnotes
Author contributions:
Study concept and design: LMSC, KS, PAS, MP. Acquisition, analysis, or interpretation of data: LMSC, KS, SA, PJ, JCAA, LKL, CM, CK, SH, MT, PAS, BC, MP. Drafting of the manuscript: LMSC, KS, MP. Critical revision of the manuscript for important intellectual content: SA, PJ, JCAA, LKL, CM, CK, SH, MT, BC, PAS. Statistical analysis: MP. Obtained funding: LMSC, KS, SA, CM. Technical or material support: LMSC, KS, SA, PJ, JCAA, LKL, CM, CK, SH, MT, PAS, BC, MP. Study supervision: LMSC, MP. KS had full access to the data in the study and final responsibility for the decision to submit for publication.
Conflict of Interest Disclosures: LMSC has obtained lecture fees from AstraZeneca, Johnson&Johnson and MSD. BC and CK are employed by AstraZeneca and hold stocks in the same company. SH holds stocks in AstraZeneca. MT holds stocks in Umecrine AB, and has a patent licensed to Umecrine AB. No other conflict of interest relevant to this study was reported.
Supplementary information is available on the International Journal of Obesity’s website.
Contributor Information
Lena M.S. Carlsson, Institute of Medicine, the Sahlgrenska Academy at University of Gothenburg, Gothenburg, Sweden
Kajsa Sjöholm, Institute of Medicine, the Sahlgrenska Academy at University of Gothenburg, Gothenburg, Sweden.
Sofie Ahlin, Institute of Medicine, the Sahlgrenska Academy at University of Gothenburg, Gothenburg, Sweden; Catholic University of the Sacred Heart, Rome, Italy.
Peter Jacobson, Institute of Medicine, the Sahlgrenska Academy at University of Gothenburg, Gothenburg, Sweden.
Johanna C. Andersson-Assarsson, Institute of Medicine, the Sahlgrenska Academy at University of Gothenburg, Gothenburg, Sweden
Linda Karlsson Lindahl, Institute of Medicine, the Sahlgrenska Academy at University of Gothenburg, Gothenburg, Sweden.
Cristina Maglio, Institute of Medicine, the Sahlgrenska Academy at University of Gothenburg, Gothenburg, Sweden; Wallenberg Centre for molecular and translational medicine, University of Gothenburg, Gothenburg, Sweden.
Cecilia Karlsson, Institute of Medicine, the Sahlgrenska Academy at University of Gothenburg, Gothenburg, Sweden; Global Medicines Development, AstraZeneca Gothenburg, Mölndal, Sweden.
Stephan Hjorth, Institute of Medicine, the Sahlgrenska Academy at University of Gothenburg, Gothenburg, Sweden.
Magdalena Taube, Institute of Medicine, the Sahlgrenska Academy at University of Gothenburg, Gothenburg, Sweden.
Björn Carlsson, Institute of Medicine, the Sahlgrenska Academy at University of Gothenburg, Gothenburg, Sweden; CVMD Translational Medicine Unit, Early Clinical Development, IMED Biotech Unit, AstraZeneca Gothenburg, Mölndal, Sweden.
Per-Arne Svensson, Institute of Medicine, the Sahlgrenska Academy at University of Gothenburg, Gothenburg, Sweden; Institute of Health and Care Sciences, the Sahlgrenska Academy at University of Gothenburg, Gothenburg, Sweden.
Markku Peltonen, National Institute for Health and Welfare, Helsinki, Finland.
References
- 1.Bray GA, Fruhbeck G, Ryan DH, Wilding JP. Management of obesity. Lancet. 2016;387(10031):1947–56. doi: 10.1016/S0140-6736(16)00271-3. [DOI] [PubMed] [Google Scholar]
- 2.Himes CL, Reynolds SL. Effect of obesity on falls, injury, and disability. J Am Geriatr Soc. 2012;60(1):124–9. doi: 10.1111/j.1532-5415.2011.03767.x. [DOI] [PubMed] [Google Scholar]
- 3.Mitchell RJ, Lord SR, Harvey LA, Close JC. Associations between obesity and overweight and fall risk, health status and quality of life in older people. Aust N Z J Public Health. 2014;38(1):13–8. doi: 10.1111/1753-6405.12152. [DOI] [PubMed] [Google Scholar]
- 4.Ylitalo KR, Karvonen-Gutierrez CA. Body mass index, falls, and injurious falls among U.S. adults: Findings from the 2014 Behavioral Risk Factor Surveillance System. Prev Med. 2016;91:217–223. doi: 10.1016/j.ypmed.2016.08.044. [DOI] [PubMed] [Google Scholar]
- 5.Fjeldstad C, Fjeldstad AS, Acree LS, Nickel KJ, Gardner AW. The influence of obesity on falls and quality of life. Dyn Med. 2008;7:4. doi: 10.1186/1476-5918-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim SY, Kim MS, Sim S, Park B, Choi HG. Association Between Obesity and Falls Among Korean Adults: A Population-Based Cross-Sectional Study. Medicine (Baltimore) 2016;95(12):e3130. doi: 10.1097/MD.0000000000003130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nguyen NT, Varela JE. Bariatric surgery for obesity and metabolic disorders: state of the art. Nat Rev Gastroenterol Hepatol. 2017;14(3):160–169. doi: 10.1038/nrgastro.2016.170. [DOI] [PubMed] [Google Scholar]
- 8.Vargas CB, Picolli F, Dani C, Padoin AV, Mottin CC. Functioning of obese individuals in pre- and postoperative periods of bariatric surgery. Obes Surg. 2013;23(10):1590–5. doi: 10.1007/s11695-013-0924-0. [DOI] [PubMed] [Google Scholar]
- 9.Teasdale N, Hue O, Marcotte J, Berrigan F, Simoneau M, Dore J, et al. Reducing weight increases postural stability in obese and morbid obese men. Int J Obes (Lond) 2007;31(1):153–60. doi: 10.1038/sj.ijo.0803360. [DOI] [PubMed] [Google Scholar]
- 10.Ikramuddin S, Billington CJ, Lee WJ, Bantle JP, Thomas AJ, Connett JE, et al. Roux-en-Y gastric bypass for diabetes (the Diabetes Surgery Study): 2-year outcomes of a 5-year, randomised, controlled trial. Lancet Diabetes Endocrinol. 2015;3(6):413–22. doi: 10.1016/S2213-8587(15)00089-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Burns ER, Stevens JA, Lee R. The direct costs of fatal and non-fatal falls among older adults - United States. Journal of Safety Research. 2016;58:99–103. doi: 10.1016/j.jsr.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Terroso M, Rosa N, Marques AT, Simoes R. Physical consequences of falls in the elderly: a literature review from 1995 to 2010. European Review of Aging and Physical Activity. 2014;11(1):51–59. [Google Scholar]
- 13.Sjöström L, Lindroos AK, Peltonen M, Torgerson J, Bouchard C, Carlsson B, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351(26):2683–93. doi: 10.1056/NEJMoa035622. [DOI] [PubMed] [Google Scholar]
- 14.Legrand H, Pihlsgard M, Nordell E, Elmstahl S. A long-recommended but seldom-used method of analysis for fall injuries found a unique pattern of risk factors in the youngest-old. Aging Clin Exp Res. 2015;27(4):439–45. doi: 10.1007/s40520-014-0308-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yau RK, Strotmeyer ES, Resnick HE, Sellmeyer DE, Feingold KR, Cauley JA, et al. Diabetes and risk of hospitalized fall injury among older adults. Diabetes Care. 2013;36(12):3985–91. doi: 10.2337/dc13-0429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Backman O, Stockeld D, Rasmussen F, Näslund E, Marsk R. Alcohol and substance abuse, depression and suicide attempts after Roux-en-Y gastric bypass surgery. Br J Surg. 2016;103(10):1336–42. doi: 10.1002/bjs.10258. [DOI] [PubMed] [Google Scholar]
- 17.Gribsholt SB, Thomsen RW, Svensson E, Richelsen B. Overall and cause-specific mortality after Roux-en-Y gastric bypass surgery: A nationwide cohort study. Surg Obes Relat Dis. 2016 doi: 10.1016/j.soard.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 18.Neovius M, Bruze G, Jacobson P, Sjöholm K, Johansson K, Granath F, et al. Risk of suicide and non-fatal self-harm after bariatric surgery: results from two matched cohort studies. Lancet Diabetes Endocrinol. 2018 doi: 10.1016/S2213-8587(17)30437-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goodman JC. Neurological Complications of Bariatric Surgery. Curr Neurol Neurosci Rep. 2015;15(12):79. doi: 10.1007/s11910-015-0597-2. [DOI] [PubMed] [Google Scholar]
- 20.Shantavasinkul PC, Torquati A, Corsino L. Post-gastric bypass hypoglycaemia: a review. Clin Endocrinol (Oxf) 2016;85(1):3–9. doi: 10.1111/cen.13033. [DOI] [PubMed] [Google Scholar]
- 21.King WC, Chen JY, Courcoulas AP, Dakin GF, Engel SG, Flum DR, et al. Alcohol and other substance use after bariatric surgery: prospective evidence from a U.S. multicenter cohort study. Surg Obes Relat Dis. 2017 doi: 10.1016/j.soard.2017.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


