Abstract
Background
Toddler-aged children are vulnerable to unintentional injuries, especially those in low-income families.
Objective
To examine the effectiveness of an intervention grounded in social cognitive theory (SCT) on the reduction of home safety problems among low-income families with toddlers.
Methods
277 low-income mother–toddler dyads were randomised into a safety promotion intervention (n=91) or an attention-control group (n=186). Mothers in the safety promotion intervention group received an eight-session, group-delivered safety intervention targeting fire prevention, fall prevention, poison control and car seat use, through health education, goal-setting and social support. Data collectors observed participants’ homes and completed a nine-item checklist of home safety problems at study enrolment (baseline), 6 and 12 months after baseline. A total score was summed, with high scores indicating more problems. Linear mixed models compared the changes over time in home safety problems between intervention and control groups.
Results
The intent-to-treat analysis indicated that the safety promotion intervention group significantly reduced safety problems to a greater degree than the attention-control group at the 12-month follow-up (between-group difference in change over time (β=−0.54, 95% CI −0.05 to −1.03, p=0.035), with no significant differences at the 6-month follow-up.
Conclusions
A safety promotion intervention built on principles of SCT has the potential to promote toddlers’ home safety environment. Future studies should examine additional strategies to determine whether better penetration/compliance can produce more clinically important improvement in home safety practices.
INTRODUCTION
Unintentional injuries are the leading cause of morbidity and mortality among children, with higher rates in low-income families in the USA.1,2 The U.S. National Center for Health Statistics estimates that in 2014, 6347 children age 0–18 years died from an unintentional injury—approximately 17 deaths/day.2 In 2010, the estimated cost of unintentional childhood injuries approached $85 billion.3 In 2012, the CDC initiated the National Action Plan for Child Injury Prevention to identify child safety promotion strategies.
Young children are especially vulnerable to unintentional injuries. In 2014, 2377 children under age 4 died from an unintentional injury and approximately 2.5 million sustained a non-fatal unintentional injury in the USA.2 Hospital emergency department records show that home safety problems (eg, no smoke alarm) increase the risk for unintentional injuries among young children.4 Most safety promotion trials for young children have been conducted in conjunction with primary healthcare visits, focusing on distribution of safety aids or installation of home safety devices, or improving parent knowledge,5–17 with mixed effects.18 Theory-guided interventions that include caregiver self-efficacy and motivation to adopt safety-promoting behaviours may be effective.19–21
Social cognitive theory (SCT) offers a theoretical basis for behavioural interventions by advancing principles of goal-setting and self-efficacy in a social support context.22 Goal-setting is a strategy for organising behaviour change into practical and manageable steps and self-efficacy promotes adoption and maintenance of health behaviours.23,24 Few safety promotion interventions have incorporated goal-setting and self-efficacy.25
We conducted a randomised, parallel group trial of safety promotion versus two obesity prevention trials (maternal diet/physical activity or toddler feeding behaviour) among low-income mothers with toddlers. The intervention groups were similar in structure (eight sessions with healthy snacks and child care), attention, location and underlying theory (SCT), using goal-setting in a social support context. The content was home safety promotion (intervention) or obesity prevention (attention-control). This paper examines the efficacy of the safety promotion intervention, in comparison with an attention-control intervention, in reducing home safety problems 6 and 12 months following enrolment and explores whether maternal self-efficacy mediates the intervention effect.
METHODS
Participants
Biological mothers of toddlers were recruited by research assistants in 2007–2010 from a Special Supplemental Nutrition Program for Women, Infants and Children clinic serving a semiurban community and a paediatric primary care clinic serving a low-income urban community. Inclusion criteria for mothers: age >18 years and not pregnant; for children: age 12–32 months, term birth, birth weight >2500 g, independent ambulation and no congenital or disabling conditions. Mother–toddler dyads participated in a baseline evaluation including demographics, maternal and toddler anthropometrics, and home safety problem assessment. The design included three interventions: (1) safety, (2) maternal diet/physical activity and (3) toddler feeding behaviour. After a cohort of ~30 dyads completed baseline, statisticians created SPSS randomisation syntax by generating random numbers, adopting a randomisation ratio of 1:1:1, stratified by maternal overweight/obesity (yes vs no) and birth order (first vs others). The project coordinator assigned the participants to interventions. The intervention group information was concealed to the mothers until attending the first session. For analyses, the two non-safety groups were combined. Recruitment stopped at the planned sample size of 277, based on a priori power analysis with STATA SAMPSI.26 The analysis assumed a repeated-measures correlation coefficient of 0.7, with 35% follow-up loss, and allows power (>80%) to detect a small-medium effect (Cohen’s d = 0.3).27
At recruitment closing, 509 mother–toddler dyads were screened; 4 were ineligible, 201 refused and 27 had incomplete assessments, leaving 277 (figure 1) with 91 safety intervention group members and 186 in the two attention-control groups. Mothers’ mean age was 27.3 years (SD 6.2, range 18.0–46.3), 72% single, widowed or divorced, 68% non-Hispanic black, 26% non-Hispanic white and 6% other racial/ethnic groups (table 1). Also, 81% completed high school/equivalent and 69% lived at/below the federal poverty line. Residence was 60% urban, 40% semiurban. Toddlers’ age ranged from 11.9 to 31.9 months (mean 20.1, SD 5.5) and 53% were males.
Figure 1.
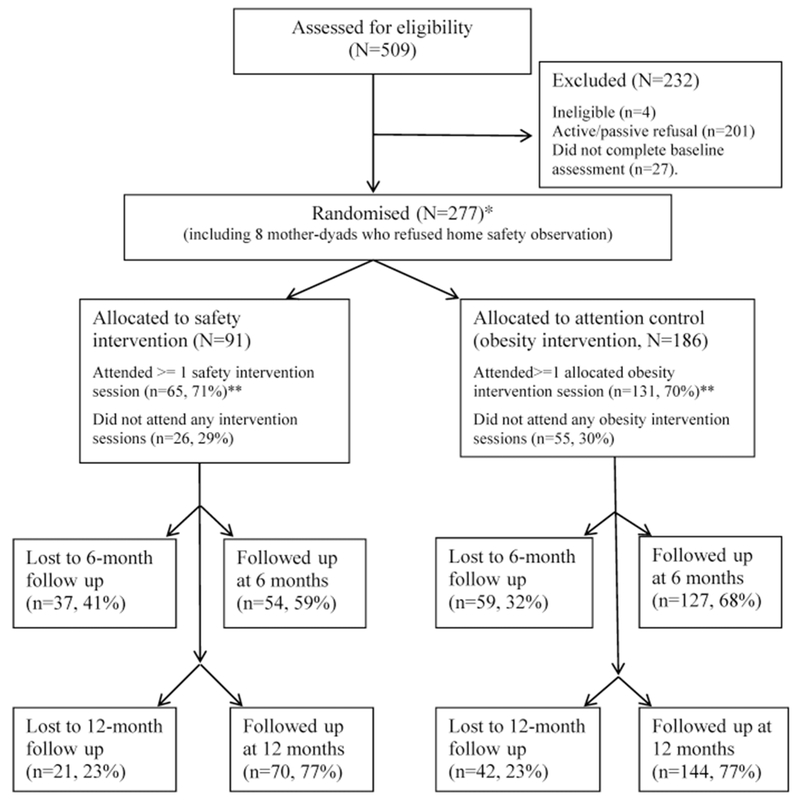
Flow of participants who were recruited, randomly assigned and followed for safety assessment in a safety promotion prevention programme among a sample of mother–toddler dyads from low-income families (n=277). *Intent-to-treat (ITT) analyses including all the 277 mother-toddler dyads; all the 277 mother-toddler dyads had at least one home safety observation. **In the control group, 55 (30%) attended none, 36 attended 1-4 sessions (19%), 95 (51%) attended 5-8 session. In the intervention group, 26 (29%) attended none, 19 attended 1-4 sessions (20%), 46 (51%) attended 5-8.
Table 1.
Selected sample characteristics at baseline (n=277)
| Total (n=277, column %) | Attention-control group (n=186, column %) | Safety intervention group (n=91, column %) | |
|---|---|---|---|
| Maternal characteristics | |||
| Age, mean (SD) | 27.3 (6.2) | 26.8 (6.2) | 28.2 (6.0) |
| Marital status | |||
| Single; divorced; widowed | 199 (71.8) | 137 (73.7) | 62 (68.1) |
| Married | 78 (28.2) | 49 (26.3) | 29 (31.9) |
| Race/ethnicity | |||
| Non-Hispanic black | 187 (67.5) | 128 (68.8) | 59 (64.8) |
| Non-Hispanic white | 74 (26.7) | 50 (26.9) | 24 (26.4) |
| Others | 16 (6.8) | 8 (4.3) | 8 (8.8) |
| Maternal education | |||
| No high school diploma | 53 (19.1) | 37 (19.9) | 16 (17.6) |
| High school diploma/equivalent or higher | 224 (80.9) | 149 (80.1) | 75 (82.4) |
| At or below poverty threshold | |||
| No | 85 (31.5) | 55 (30.2) | 30 (34.1) |
| Yes | 185 (68.5) | 127 (69.8) | 58 (65.9) |
| Residence | |||
| Urban | 167 (60.3) | 114 (61.3) | 53 (58.2) |
| Semiurban | 110 (39.7) | 72 (38.7) | 38 (41.8) |
| Toddler characteristics | |||
| Age, mean (SD) | 20.1 (5.5) | 20.1 (5.5) | 20.1 (5.5) |
| Gender | |||
| Female | 130 (46.9) | 85 (45.7) | 45 (49.4) |
| Male | 147 (53.1) | 101 (54.3) | 46 (50.6) |
No significant differences between intervention and control groups based on t-tests or χ2 tests (p value for maternal age=0.095, ps for other variables >0.10).
Intervention
The protocol was approved by university and state Department of Health and Mental Hygiene ethical review boards. Written informed consent was obtained and participants were compensated for evaluations.
Based on the suggestions by American Academy of Pediatrics Committee on Injury, Violence and Poison Prevention guidelines on toddler safety,28 we targeted four toddler safety areas: fire prevention including prevention of exposed wires, non-covered outlets and installing/checking smoking detectors, fall prevention including using stair gate and repairing dangerous balcony, unsafe handrails etc, poison control including installing child-resistant latches on medication storage/cleaning supplies cabinets or avoiding paints or other poisons, and car seat use. Local safety providers (eg, Fire Department, Maryland Kids in Safety Seats) provided material and training and collaborated on the development of a manualised safety protocol, including information and hand-outs on free/inexpensive car seats, free smoke detectors, inexpensive stair gates and locking cabinets. The safety intervention was conducted in two community sites (church and preschool), located close to recruitment sites and participants’ homes. The intervention included eight sessions (four group, three telephone and a final review/celebration group). Health educators led the sessions using SCT principles, including self-monitoring, goal-setting, feedback, self-instruction and social support in a friendly, supportive context. Group activities (eg, sharing cabinet locking strategies) were conducted to build skills, encourage modelling, promote perceptions of social norms endorsing toddler safety over convenience, provide social support and build self-efficacy. During telephone sessions, mothers and health educators discussed specific safety goals, barriers and enablers.
The attention-control groups received a similarly designed intervention, focusing on promoting maternal diet/physical activity or toddler feeding behaviour. All groups received child-care, healthy snacks and compensation for transportation.
Compliance
Attendance was similar across groups (eg, 65/91 (71%) safety promotion and 131/186 (70%) attention control for attendance ≥1 session, p>0.10; for details, see figure 1). The mean number of sessions was equal across groups: 5.5 (SD 2.4). 30% did not attend any sessions, reporting transportation and work schedule issues.
Evaluations
The data collectors (not health educators), blinded to intervention group assignments, conducted evaluations at baseline, 6 and 12 months following baseline. In total, 277 mothers completed baseline assessment, including 8 who refused home safety observation (other evaluations conducted in clinics, figure 1). Refusal was higher among semiurban compared with urban mothers (6.4% vs 0.6%, p = 0.007) and among unmarried, compared with married mothers (6.0% vs 2.0%, p = 0.042), but did not differ in other mother/toddler characteristics. Mother–toddler dyads were re-evaluated 6 and 12 months following baseline (n = 181, 65%, and n=214, 77%, respectively). At 6 months, mothers lost to follow-up had higher baseline safety problem scores than evaluated mothers (3.1 vs 2.6, p = 0.041). At 12 months, mothers lost to follow-up did not differ in baseline home safety problems or any other variable from evaluated mothers.
Measures
Home safety problems (primary outcome)
Data collectors observed home safety using a nine-item checklist of danger/safety features, adapted from Healthy Homes Maintenance Checklist by the National Center for Healthy Housing,29 and the Household Safety Checklist by KidHealth from Nemours.30 The observations included yes/no responses: (1) exposed wires; (2) covered outlets; (3) working smoke detector on each floor; (4) stair gate for toddlers in homes with stairs; (5) dangerous balcony/porch; (6) unsafe outside handrails/steps/stairs; (7) chipped/peeled paint; (8) peeling paint/broken plaster >81/2 by 11 inches and (9) child-resistant latches on cleaning supply/medication cabinets. Car seat use could not be observed and was excluded. Data collectors received training to maximise observation reliability (eg, definitions of ‘dangerous balcony/porch’); inter-rater reliability exceeded 90%. Some participants refused inspection of certain areas of the homes. In total, 212 out of 269 (79%), 140 out of 181 dyads (77%) and 161 out of 214 (75%) homes were observed without missing values for any item at baseline, first and second follow-ups, respectively. There is no recommendation for stair gate use for toddlers ≥24 months. Missing and ineligible items (eg, no stairs, stair gate use for toddler ≤24 months) were substituted with participant-level mean. A summary score was calculated, ranging from 0 to 9 (Cronbach’s α=0.6); high scores indicate more safety problems.
Safety-related self-efficacy
Self-efficacy is behaviour-specific,31 measured with three questions related to smoke alarms, cleaning supplies and stair gates, such as ‘How sure are you that you can have and test smoke alarms on each floor of your house?’ with four-level responses ranging from 0 = ‘I know I cannot’, to 3 = ‘I know I can’. Due to skewness, responses were recoded into two levels: 1 = ‘I know I can’ vs 0 =‘other responses’. A summary score (range 0–3) was created; higher scores indicate higher self-efficacy.
Other variables
Mothers reported age, race/ethnicity, marital status and years of education. Urban/semiurban residence was based on recruitment site. Poverty ratio was calculated based on the federal threshold using mother-reported total family income and number of household members. Mothers reported toddlers’ birth date and gender.
Analyses
Preliminary analyses compared baseline characteristics of mothers/toddlers by intervention status, with t-tests for continuous and χ2 tests (or Fisher’s exact test) for categorical variables.
Both intent-to-treat (ITT) analyses and per-protocol analyses were conducted and compared. The home safety problem score was normally distributed (skewness=0.63). Linear mixed modelling (LMM, SAS PROC Mixed) assessed the intervention effect, accounting for clustering of repeated measures within individuals.32 Time (baseline, 6 months and 12 months) was recoded into dummy variables. Interactions between intervention status and time were included. We estimated within-group change of outcome over time and compared the change between the two parallel groups (intervention vs attention-control). Covariates were adjusted if related to missingness or compliance. We found no difference by inclusion/exclusion of stair gate use (toddlers <24 months) from home safety score; results include stair gate use.
ITT analyses included all the participants who were randomly assigned. To examine whether ITT underestimates the intervention effect given the low compliance (30% mothers did not attend any intervention sessions), we conducted a per-protocol analysis, restricted to compliers.33,34 Per-protocol analysis could lead to bias when randomisation is violated after excluding non-compliers. The primary intervention topic (safety, maternal diet/physical activity and toddler feeding behaviour) was introduced in the first session. The participants’ decision on attendance of >1 session may have been related to the specific topic. Therefore, we defined compliers as participants who attended ≤1 session and non-compliers as participants who did not attend any sessions. We compared baseline characteristics by intervention status and compliance, and examined the intervention effect among compliers and non-compliers for comparison.
To explore self-efficacy as a mediator, as predicted by SCT, we assessed (1) the relation between self-efficacy and outcome at baseline, (2) the relation between self-efficacy change and outcome over time and (3) the effect of intervention on self-efficacy. All analyses were conducted with SAS V9.3, with p<0.05 as significant, and 0.05≤p<0.10 as marginal.35
Missing values
About 0.3% of the mother–toddler dyads refused the home assessments at baseline, and 35% and 23% were lost at 6-month and 12-month evaluations. The assumption of missing completely at random (MCAR) for home safety problem scores was met (Little’s MCAR test χ2=12.2, df=8, p=0.14336). Maximum likelihood estimation (MLE) has advantages over some other methods with missing values and was used in LMM to handle missing values37 with full information (both complete/incomplete cases) to provide unbiased parameter estimates with MCAR/MAR data. We systematically assessed differences between mother–toddler dyads lost/retained at either follow-up (n=119/158). Lost dyads had marginally higher home safety problem scores (mean 2.66 vs 2.34, p=0.094) and marginally lower high school diploma/equivalent percentage at baseline (40.2% vs 54.7%, p=0.055) than retained dyads, with no significant differences for other baseline characteristics. A sensitivity analysis estimate obtained using listwise deletion (analyses restricted to participants with complete data) was compared with MLE. The two models showed similar intervention effects, suggesting that the intervention effect estimates are not sensitive to different methods. We report MLE results.
RESULTS
Descriptive statistics
Baseline maternal/toddler characteristics did not differ significantly by intervention group (ps>0.05, table 1).
Home safety problems
As shown in table 2, there were home safety concerns related to fire/electricity prevention, fall prevention and poison control at baseline, with no significant group differences (mean 2.52 control vs 2.36 safety intervention, p=0.433).
Table 2.
Prevalence of each safety problem by intervention at each assessment
| Attention-control group (%)† |
Safety intervention group (%)† |
|||||
|---|---|---|---|---|---|---|
| Safety categories | Baseline | Six-month follow-up | Twelve-month follow-up | Baseline | Six-month follow-up | Twelve-month follow-up |
| Fire/electricity safety | ||||||
| Exposed wires | 10.8 | 5.6 | 12.4 | 9.2 | 0 | 7.6 |
| Non-covered outlets | 70.1 | 72.3 | 70.1 | 71.4 | 72.3 | 61.9 |
| Lack of working smoke detector on each floor | 8.1 | 8.1 | 9.1 | 8.1 | 3.8 | 5.7 |
| Fall prevention | ||||||
| Lack of stair gate (homes with stairs/toddler <24 months)* | 64.9 | 73.7 | 75.0 | 51.4 | 60.0 | 0 |
| Dangerous balcony or porch | 4.7 | 2.4 | 5.1 | 5.1 | 0 | 0 |
| Unsafe outside handrails, steps or stairs | 6.8 | 2.4 | 6.8 | 6.7 | 2.6 | 2.3 |
| Poison control and others | ||||||
| Lack of child-resistant latches on cabinets for cleaning supplies or medications storage | 67.4 | 54.4 | 61.5 | 60.9 | 31.5 | 51.4 |
| Chipped or peeled paint by finger scraping | 17.6 | 11.1 | 7.1 | 21.1 | 14.3 | 3.7 |
| Page-size peeling paint or broken plaster | 3.1 | 0.9 | 1.8 | 0 | 2.4 | 0 |
The prevalence of ‘lack of stair gate’ was assessed only among mother-toddler dyads with stairs and with toddlers <24 months (n=131 baseline, 53, 6 months, and 9, 12 months).
No group difference in frequency was found for each specific safety item (ps>0.10).
ITT analysis (n=277)
As shown in figure 2 and table 3, the intervention group significantly reduced the number of safety problems from baseline (mean 2.36, SD 1.58) to 6-month follow-up (mean 1.73, SD 1.55). The intervention group had 0.53 fewer safety problems on average at 6-month follow-up compared with baseline (β for change=−0.53, SE 0.23, p=0.021). The reduction was sustained through 12-month follow-up (mean 1.81, SD 1.44); the average number of problems was 0.58 fewer at 12-month follow-up compared with baseline (β for change=−0.58, SE 0.21, p = 0.006). In contrast, there was no significant change in the number of problems between baseline and 6-month or 12-month follow-up in the attention-control group. Comparing the changes in the mean number of safety problems in the intervention and attention-control group, there was no significant between-group difference at 6 months (p>0.10), but there was a significant difference at 12 months, with a greater reduction by 0.54 in safety problems among the intervention group than the attention-control group (β for difference in change=−0.54, SE 0.25, p=0.035). The intervention effect was modest based on Cohen’s d=0.38 (95% CI 0.09 to 0.67, table 3 and figure 2).27 It can also be interpreted as a reduction of 16% of families with home safety scores >4.0 (1 SD above the mean) to 9% after intervention, based on normal distribution. Results were similar after adjusting for poverty and maternal education (β for between-group difference in change at 12 months = −0.53, SE 0.23, p=0.020; no significant between-group difference at 6 months).
Figure 2.
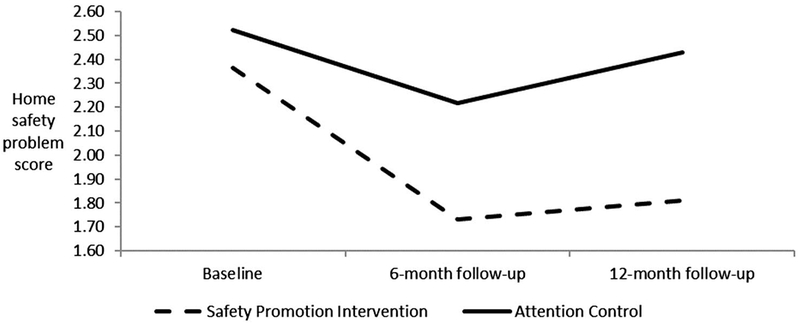
Mean sample-based home safety problem score by time and intervention status.
Table 3.
The effect of safety promotion intervention on the reduction of home safety problems
| Attention-control group |
Safety intervention group |
Estimated difference in change* (intervention vs control) | p Value | |||||
|---|---|---|---|---|---|---|---|---|
| Mean M (SD)† | Estimated change in mean* M (SE) | p Value | Mean M (SD)† | Estimated change in mean* M (SE) | p Value | |||
| Analysis among the total sample (intent-to-treat, n=186 control, n=91 intervention) | ||||||||
| Home safety problem score | ||||||||
| Baseline | 2.52 (1.58) | 2.36 (1.58) | ||||||
| Six-month follow-up | 2.22 (1.44) | −0.21 (0.15) | 0.169 | 1.73 (1.55) | −0.53 (0.23) | 0.021 | −0.32 (0.27) | 0.244 |
| Twelve-month follow-up | 2.43 (1.86) | −0.04 (0.15) | 0.794 | 1.81 (1.44) | −0.58 (0.21) | 0.006 | −0.54 (0.25) | 0.035 |
| Analysis of intervention effect among compliers only (n=131 control, n=65 intervention)‡ | ||||||||
| Home safety problem score | ||||||||
| Baseline | 2.43 (1.46) | 2.33 (1.69) | ||||||
| Six-month follow-up | 2.17 (1.42) | −0.21 (0.16) | 0.199 | 1.50 (1.17) | −0.77 (0.24) | 0.002 | −0.55 (0.29) | 0.060 |
| Twelve-month follow-up | 2.30 (1.79) | −0.09 (0.16) | 0.584 | 1.73 (1.44) | −0.65 (0.23) | 0.005 | −0.57 (0.28) | 0.045 |
| Analysis of intervention effect among non-compliers only (n=55 control, n=26 intervention)‡ | ||||||||
| Home safety problem score | ||||||||
| Baseline | 2.77 (1.84) | 2.45 (1.27) | ||||||
| Six-month follow-up | 2.45 (1.54) | −0.13 (0.37) | 0.721 | 2.88 (2.59) | 0.66 (0.58) | 0.260 | 0.79 (0.69) | 0.254 |
| Twelve-month follow-up | 2.85 (2.06) | 0.17 (0.33) | 0.595 | 2.07 (1.46) | −0.30 (0.46) | 0.506 | −0.48 (0.56) | 0.396 |
The changes over time and the differences in the changes over time between the safety promotion group and the control group and p values were estimated based on the linear mixed models including time, intervention and interactions between time and intervention.
Sample-estimated means and SDs.
Compliers are participants who attended ≥1 session; non-compliers are participants who did not attend any sessions; the analysis of intervention effect among compliers/non-compliers included the compliers/non-compliers who had missing values for home safety problems at one or two assessments.
Per-protocol analysis
There were no significant differences by intervention status in baseline characteristics including home safety problem score among compliers (ps>0.10) or non-compliers (ps>0.10). Comparing complier and non-compliers in the safety intervention group, the compliers were more likely to be at/below poverty threshold (80.8% vs 59.7%, p = 0.049), without differences in other baseline characteristics.
The estimated intervention effect among compliers (n=196) is stronger than the estimate based on ITT analyses at 6 months, but similar at 12 months. Intervention group compliers significantly reduced their home safety problems at 6 months (β=−0.77, SE 0.24, p=0.002) and 12 months (β=−0.65, SE 0.23, p=0.005, table 3); with no significant changes over time among attention-control group compliers. Intervention group compliers reduced safety problems to a marginally greater degree at 6 months (β=−0.55, SE 0.29, p=0.060) and to a significantly greater degree at 12 months (β=−0.57, SE 0.28, p=0.045, table 3) compared with attention-control group compliers. Among the participants in the safety intervention group who attended at least one session, the number of sessions attended was not related to the changes of safety problems over time (ps>0.10).
Among non-compliers (n=81), there was no change within either safety or attention-control group, and no difference between the two groups in changes over time (ps>0, table 3).
Self-efficacy
The mean self-efficacy scores were 2.70 (SD 0.65), 2.52 (SD 0.74) and 2.42 (SD 0.83) at baseline, 6 months and 12 months, respectively, for the safety intervention group, and 2.62 (SD 0.62), 2.51 (SD 0.73) and 2.53 (SD 0.77) for the attention-control group, with no difference by intervention status. Based on LMM, the intervention group significantly decreased self-efficacy at 12 months (β=−0.27, SE 0.12, p=0.021) compared with baseline; self-efficacy did not significantly change for the attention-control group. There were no significant between-group differences in self-efficacy change at either 6 or 12 months (ps>0.10).
At baseline, self-efficacy was significantly related to fewer safety problems in the linear regression model (β=−0.36, SE 0.18, p = 0.045). Baseline self-efficacy was not related to changes in safety problems at either 6 or 12 months (ps>0.10). The change scores in self-efficacy at 6 and 12 months were not significantly related to change scores in home safety problems at 6 and 12 months (ps>0.10).
DISCUSSION
Low-income households with toddlers had multiple home safety problems (eg, at enrolment, >70% lacked covered outlets and >60% lacked child-resistant cabinet latches). A group-delivered safety promotion intervention had a modest effect on reducing home safety problems at 12 months. One possibility is that the baseline home safety assessment alerted mothers in both groups to safety problems, leading to reduction of safety problems in both groups at 6 months; significant in the intervention group and non-significant in the control group. At 12 months, the reduction was sustained in the intervention group, suggesting that mothers continued to operationalise safety promotion behaviours. In contrast, the reduction was not sustained in the control group, leading to a significant intervention effect at 12 months (figure 2).
Young children 1–4 years with rapid physical development, but limited ability to avoid potential dangers in homes, are especially vulnerable to unintentional injuries. Home injuries account for approximately 50% unintentional injuries.38 In our study among the low-income mother–toddler dyads, the safety intervention combining safety education with goal-setting and self-efficacy effectively modified the home environment by reducing home safety problems. At baseline, the highest prevalence of safety problems were lack of outlet covers (~70%) and cabinet latches (~65%). Environmental improvements were observed in outlet covers, cabinet latches and some other safety problems after intervention. Possible reasons include provision of information on free/inexpensive safety equipment to low-income mothers, along with adoption of strategies to promote maternal motivation to overcome management barriers and related inconvenience. The existing interventions involving provision of safety education or safety equipment showed mixed effects on promoting safety practices, suggesting that other components of behaviour change theories may be necessary.18 The reduction in home safety problems in this study may have resulted from the SCT components of the intervention as participants discussed goals, successes and challenges in installing, maintaining and using home safety devices.
At baseline, mothers with higher self-efficacy scores had fewer home safety problems, consistent with SCT that self-efficacy relates to health-related behaviours.19,20 Self-efficacy was not found to be a mediator for the intervention effect. In contrast to expectations, self-efficacy decreased over time among intervention group mothers, with no change among attention-control group mothers. One possible explanation is that although intervention group mothers successfully modified their safety behaviour, reducing home safety problems, they may have recognised the maintenance challenges. Living in less safe housing conditions or lacking means to make changes to their household maintenance for the low-income mothers in the intervention group could have been linked to their decreased self-efficacy. Additional research is necessary to understand the mechanisms driving safety-related behaviour, the role of self-efficacy and domain-specific measures of self-efficacy.
This study has several strengths. First, this safety promotion intervention is based on SCT, focusing on bridging knowledge with goal-setting in a context of social support. Second, the parallel group design adjusts for intervention-associated attention and structure, assuring that differences can be attributed to content. Third, the home safety problem is a proxy of unintentional injury. We used objectively measured observations of home safety problems rather than maternal report. Fourth, the safety intervention focused on toddlers in low-income families, a subpopulation at high risk of injuries.
There are several methodological considerations. First, we did not assess car seat use in the home observation of safety problems. Second, the clinical importance of the modest intervention effect needs further examination. Third, attendance at initial sessions was low across both groups, suggesting a need for alternative intervention strategies. Finally, the finding needs to be repeated before being generalised to mother–toddler dyads from different socioeconomic status.
CONCLUSIONS
The prevalence of home safety problems indicates an urgent need for interventions to prevent toddlers from unintentional injuries. An SCT-based, group-delivered safety promotion intervention for low-income mothers of toddlers had a modest effect on reduction of home safety problems at 12 months. Future studies should examine additional strategies to retain low-income mothers in group-based intervention and to examine if an SCT-based approach with better penetration/compliance can produce more clinically important improvements in home safety practices and which components of the SCT-based approach are most effective.
What is already known on the subject?
-
►
Toddler-aged children are vulnerable to unintentional injuries, especially those in low-income families.
-
►
Most safety promotion trials for young children focused on distribution of safety aids or improving parent knowledge and had mixed effects.
-
►
There has been limited attention to goal setting and social support applied to safety promotion interventions for young children
What this study adds?
An eight-session, group-delivered, randomised, parallel group safety promotion intervention trial for low-income mothers with toddlers, grounded in social cognitive theory with goal setting and social support, is effective in reducing home safety problems.
Acknowledgements
The authors thank the participants in this study.
Funding This study was funded by National Institute of Child Health and Human Development (NICHD) R03HD077156 (principal investigator YW), R01HD056099 (principal investigator: MMB) and U.S. Department of Agriculture (USDA) CREES 2005-04808 (principal investigator: MMB).
Footnotes
Competing interests None declared.
Patient consent Obtained.
Ethics approval Ethical review boards of University of Maryland, Baltimore, ethic review boards from Maryland Department of Health and Mental Hygiene.
Provenance and peer review Not commissioned; externally peer reviewed.
Trial registration number NCT02615158; post-results.
REFERENCES
- 1.Borse NN, Gilchrist J, Dellinger AM, et al. CDC Childhood Injury Report: Patterns of Unintentional Injuries among 0–19-year-olds in the United States, 2000–2006. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, 2008. [Google Scholar]
- 2.Leading Causes of Death Reports, National and Regional, 1999–2014. http://webappa.cdc.gov/sasweb/ncipc/leadcaus10_us.html (accessed 29 Jul 2016).
- 3.Injury Prevention & Control: Data & Statistics (WISQARS™). http://www.cdc.gov/injury/wisqars/index.html (accessed 29 Jul 2016).
- 4.LeBlanc JC, Pless IB, King WJ, et al. Home safety measures and the risk of unintentional injury among young children: a multicentre case-control study. CMAJ 2006;175:883–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Achana FA, Sutton AJ, Kendrick D, et al. The effectiveness of different interventions to promote poison prevention behaviours in households with children: a network meta-analysis. PLoS ONE 2015;10:e0121122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hendrickson SG. Reaching an underserved population with a randomly assigned home safety intervention. Inj Prev 2005;11:313–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hubbard S, Cooper N, Kendrick D, et al. Network meta-analysis to evaluate the effectiveness of interventions to prevent falls in children under age 5 years. Inj Prev 2015;21:98–108. [DOI] [PubMed] [Google Scholar]
- 8.Tse J, Nansel TR, Weaver NL, et al. Implementation of a tailored kiosk-based injury prevention program in pediatric primary care. Health Promot Pract 2014;15:243–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gielen AC, McDonald EM, Wilson MEH, et al. Effects of improved access to safety counseling, products, and home visits on parents’ safety practices: results of a randomized trial. Arch Pediatr Adolesc Med 2002;156:33–40. [DOI] [PubMed] [Google Scholar]
- 10.Kendrick D, Marsh P, Fielding K, et al. Preventing injuries in children: cluster randomised controlled trial in primary care. BMJ 1999;318:980–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McDonald EM, Solomon B, Shields W, et al. Evaluation of kiosk-based tailoring to promote household safety behaviors in an urban pediatric primary care practice. Patient Educ Couns 2005;58:168–81. [DOI] [PubMed] [Google Scholar]
- 12.Nansel TR, Weaver N, Donlin M, et al. Baby, Be Safe: the effect of tailored communications for pediatric injury prevention provided in a primary care setting. Patient Educ Couns 2002;46:175–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nansel TR, Weaver NL, Jacobsen HA, et al. Preventing unintentional pediatric injuries: a tailored intervention for parents and providers. Health Educ Res 2008;23:656–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Watson M, Kendrick D, Coupland C, et al. Providing child safety equipment to prevent injuries: randomised controlled trial. BMJ 2005;330:178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gittelman MA, Pomerantz WJ, McClanahan N, et al. A computerized kiosk to teach injury prevention: is it as effective as human interaction?. J Trauma Acute Care Surg 2014;77:S2–7. [DOI] [PubMed] [Google Scholar]
- 16.Phelan KJ, Khoury J, Xu Y, et al. A randomized controlled trial of home injury hazard reduction: the HOME injury study. Arch Pediatr Adolesc Med 2011;165:339–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Posner JC, Hawkins LA, Garcia-Espana F, et al. A randomized, clinical trial of a home safety intervention based in an emergency department setting. Pediatrics 2004;113:1603–8. [DOI] [PubMed] [Google Scholar]
- 18.Kendrick D, Young B, Mason-Jones AJ, et al. Home safety education and provision of safety equipment for injury prevention (Review). Evid Based Child Health 2013;8:761–939. [DOI] [PubMed] [Google Scholar]
- 19.Beirens TM, Brug J, van Beeck EF, et al. Assessing psychosocial correlates of parental safety behaviour using Protection Motivation Theory: stair gate presence and use among parents of toddlers. Health Educ Res 2008;23:723–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beirens TM, van Beeck EF, Brug J, et al. Why do parents with toddlers store poisonous products safely? Int J Pediatr 2010;2010:702827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Winston FK, Erkoboni D, Xie D. Identifying interventions that promote belt-positioning booster seat use for parents with low educational attainment. J Trauma 2007;63:S29–38. [DOI] [PubMed] [Google Scholar]
- 22.Bandura A, ed. Social foundations of thought & action: a social cogntive theory. NJ: Prentice Hall, 1986. [Google Scholar]
- 23.Shilts MK, Horowitz M, Townsend MS. Goal setting as a strategy for dietary and physical activity behavior change: a review of the literature. Am J Health Promot 2004;19:81–93. [DOI] [PubMed] [Google Scholar]
- 24.Winters ER, Petosa RL, Charlton TE. Using social cognitive theory to explain discretionary, “leisure-time” physical exercise among high school students. J Adolesc Health 2003;32:436–42. [DOI] [PubMed] [Google Scholar]
- 25.Trifiletti LB, Gielen AC, Sleet DA, et al. Behavioral and social sciences theories and models: are they used in unintentional injury prevention research?. Health Educ Res 2005;20:298–307. [DOI] [PubMed] [Google Scholar]
- 26.Seed PT. Sample size calculations for clinical trials with repeated measures data. Stata Tech Bull 1997;7:16–18. [Google Scholar]
- 27.Feingold A Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychol Methods 2009;14:43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gardner HG. Office-based counseling for unintentional injury prevention. Pediatrics 2007;119:202–6. [DOI] [PubMed] [Google Scholar]
- 29.The National Center for Healthy Housing: Healthy Homes Maintenance Checklist. http://www.nchh.org/Portals/0/Contents/Healthy_Housing_Checklist.pdf (accessed 31 Jul 2015).
- 30.KidsHealth Household Safety Checklists. http://kidshealth.org/en/parents/household-checklist.html (accessed 22 May 2016).
- 31.Pajares F Current directions in self-efficacy research. Adv Motiv Achiev 1997;10:1–49. [Google Scholar]
- 32.Fitzmaurice GM, Laird NM, Ward JH. Applied longitudinal analysis. Wiley, 2012. [Google Scholar]
- 33.Armijo-Olivo S, Warren S, Magee D. Intention to treat analysis, compliance, drop-outs and how to deal with missing data in clinical research: a review. Phys Ther Rev 2009;14:36–49. [Google Scholar]
- 34.Prince RL, Devine A, Dhaliwal SS, et al. Effects of calcium supplementation on clinical fracture and bone structure: results of a 5-year, double-blind, placebo-controlled trial in elderly women. Arch Intern Med 2006;166:869–75. [DOI] [PubMed] [Google Scholar]
- 35.Pritschet L, Powell D, Horne Z. Marginally significant effects as evidence for hypotheses: changing attitudes over four decades. Psychol Sci 2016;27:1036–42. [DOI] [PubMed] [Google Scholar]
- 36.Little RJA. A test of missing completely at random for multivariate data with missing values. J Am Stat Assoc 1988;83:1198–202. [Google Scholar]
- 37.Allison P Handling missing data by maximum likelihood. SAS Global Forum 2012. [Google Scholar]
- 38.Mack KA, Rudd RA, Mickalide AD, et al. Fatal unintentional injuries in the home in the U.S., 2000–2008. Am J Prev Med 2013;44:239–46. [DOI] [PMC free article] [PubMed] [Google Scholar]


