Abstract
Myocarditis is mostly caused by viral infections and rarely caused by bacterial pathogens, especially in immunocompetent individuals. Bacterial myocarditis due to Salmonella is rare, especially in countries with improved sanitation that minimize contamination of Salmonella typhi serotypes. We here present a case of a previous healthy 22-year-old male that came to the emergency room with chest pain. His symptoms occurred after a period of profuse diarrhea, fever and hematochezia. Magnetic resonance imaging confirmed the diagnosis of myocarditis. Stool culture was positive for Salmonella enteritidis. Myocarditis due to Salmonella is rare but may still occur in western countries. The inter-individual response to the pathogens and its virulence mechanisms and male gender is factors for developing myocarditis. We here add to the numbers of cases with myocarditis due to S. enteritidis. A higher suspicion and more frequent ECG and troponin testing might result in an increase of patients with subclinical myocarditis.
INTRODUCTION
Myocarditis is an inflammation of the myocardium, caused by viruses, infections and immune mediated. The true incidence is unknown and the different clinical presentations range from asymptomatic to cardiogenic shock which result in difficulty to be sure of the diagnosis [1]. Myocarditis has been shown to be the third leading cause of death among young, athletes [2]. The inflammation can progress to acute heart failure and chronic dilated cardiomyopathy due to chronic remodeling [1, 3, 4]. The pathogenesis is not clear but testosterone, components of innate immunity and pro-fibrotic cytokines are factors associated with increased inflammation and susceptibility of heart failure [4]. The most common etiology is viruses, especially Coxsackie- and Adeno-viruses. Myocarditis due to bacterial infections are rare [5]. The gold standard for diagnosis is endo-myocardial biopsy but non-invasive methods are more commonly used since the biopsy holds multiple risks [4]. Troponins should be evaluated over time, when myocarditis shows a gradual rise in concentrations over more than 24 h, with a peak at Day 2 or 3 [4]. Cardiac magnetic resonance imaging (CMRI) is now the standard tool for determining diagnosis due to the safety profile and the accuracy [6].
Salmonella is a genus of gram negative bacteria with multiple serotypes that primarily cause diarrheal illness in humans by ingestion of contaminated food products, especially poultry and eggs [7]. The pathogens cause significant morbidity and mortality worldwide and are responsible for a wide spectrum of disease [7].
CASE REPORT
A previously healthy 22-year-old male came to the health center with a 2-day history of fever (40°C), abdominal pain and frequent diarrhea with mild hematochezia. He and his friend, with the same symptoms, had ingested poultry at a local festival prior to onset. He had no recent history of travel, no previous medications and no family history of gastrointestinal diseases. C-reactive protein (CRP) where elevated to 200 mg/L. Stool culture was positive for Salmonella and conservative treatment was recommended after consultation with a specialist of infectious diseases. Two days later the patient presented at the emergency room (ER) due to severe chest pain with radiating sensations to his left arm for a couple of hours. He had normal vital signs, including temperature, and his diarrhea had decreased. The first ECG showed mild anterior ST-elevation which easily could have been explained as early repolarization (Fig. 1). He was admitted to the cardiac intensive care unit since initial lab results where elevated with CRP at 92 mg/L (normal: <5mgL), troponin at 447 ng/L (normal: <10 ng/L), white blood count (WBC) at 9,0 × 10e9/L (normal: 3.5–8.8). During the first 6 h, the ECG developed more prominent, generalized ST-elevation (Fig. 2). He showed no signs of rhabdomyolysis with normal creatinine-kinase and estimated glomerular filtration rate of more than 90 mL/min/1,73 m2 (normal: >79 mL/min/1,73 m2). Intravenous, broad spectrum antibiotics (Cefotaxime) and fluids were started. Echocardiography on the second day revealed a normal sized left ventricle with mildly reduced left ventricular function with an ejection fraction (EF) of 46% (normal: >55%). NT-ProBNP was elevated to 1261 ng/L (normal: <125 ng/L). CRP decreased during the following days, 56–7 mg/L and his WBC normalized. The troponins continued to increase to a maximum of 2093 ng/L, three days after presentation at the ER, see Table 1 for the development of the laboratory results. Specification of the positive culture showed Salmonella enteritidis but the blood cultures showed no signs of bacteremia. After four days of intravenous antibiotics a shift to oral treatment with trimethoprim–sulfa (160 mg/800 mg) for a total length of antibiotic treatment of 10 days, was administered. CMRI at Day 5, revealed an active myocarditis involving the inferior/ inferoseptal lateral area of the left ventricle, conforming well to the ECG-findings (Fig. 3). The left ventricle was mildly dilated with a minor hypokinetic area. On Day 7 he was discharged with resolution of his symptoms. Treatment with Angiotensin Converting Enzyme Inhibitor (ACEI) was initiated. No beta-blockers were administrated due to a tendency of bradycardia. Exercise ECG, 4 weeks later showed a low-normal physical capacity (75% of reference), and an ECG reaction with post myocardial affection with normalization of negative T-waves at work (Fig. 4). At follow up, 6 weeks after discharge, the patient had made full recovery and was without residual symptoms. All laboratory testing was normal, including NT-proBNP at 50 ng/L. Echocardiography at follow up showed normalization of the previous function and the ECG were normal (Fig. 5). His friend recovered rapidly after his initial period of gastroenteritis and never developed any cardiac manifestations.
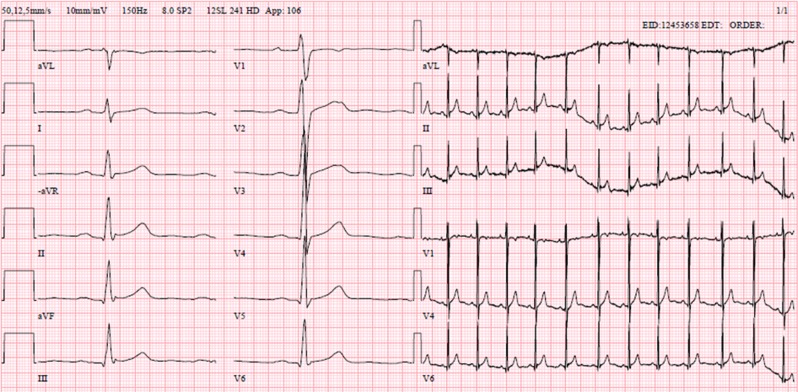
Figure 1:
ECG from arrival at the emergency room. ECG shows a normal sinus rhythm, frequency 73/min. Mild ST-elevation in the anterior and inferior leads may be suspected but can easily be described as early repolarization
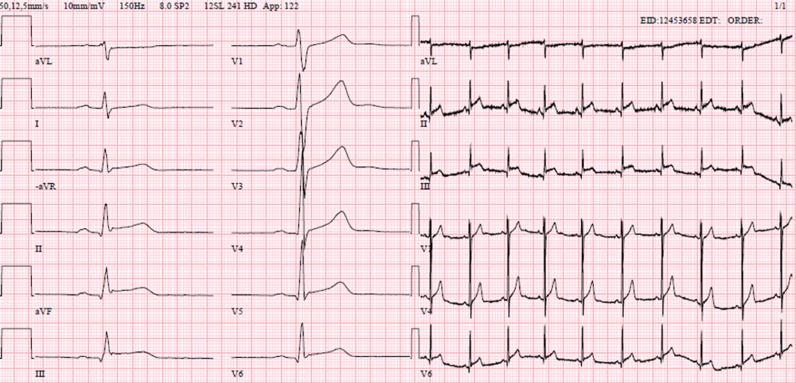
Figure 2:
ECG 6 h later, at the cardiac ICU. ECG shows normal sinus rhythm, frequency 57/min. Generalized ST-elevation, most prominent in the inferior leads
Table 1:
The table show the development of laboratory results of the patient. If empty, no laboratory testing were performed that day. CRP, C-reactive protein; leukocytes = white blood count, WBC
| P-troponin T | S-CRP | P-NT-proBNP | B-WBC | |
|---|---|---|---|---|
| Normal <15 ng/L | Normal <5 mg/L | Normal <125 ng/L | Normal 3.5–8.8×10e9/L | |
| Day 1 | 429 | 92 | 9.0 | |
| Day 2 | 992 | 56 | 1261 | 6.0 |
| Day 3 | 1878 | 36 | 6.6 | |
| Day 4 | 2093 | 26 | 6.9 | |
| Day 5 | 1240 | |||
| Day 6 | 399 | |||
| Day 7 | 47 | 7 |
Figure 3:
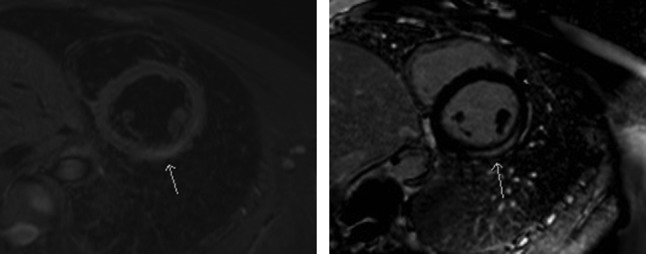
CMRI reveals a section with edema and inflammation corresponding to myocarditis. To the left, an image with a sequence sensitive for edema. This reveals an area that are shown with an arrow. To the right, the same area highlights with late enhancement
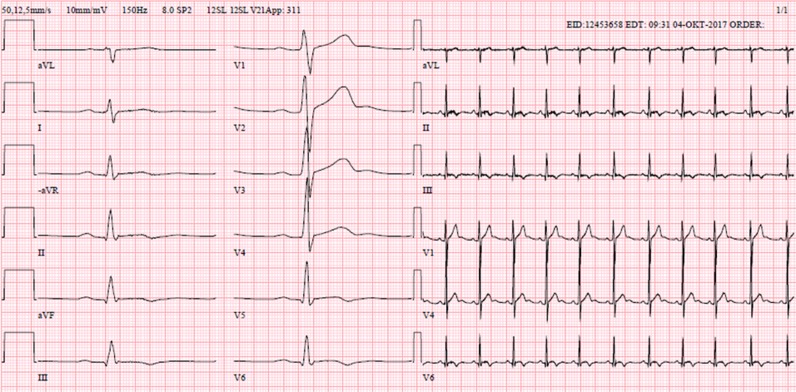
Figure 4:
ECG from exercise test, 1 month later. ECG Shows normal sinus rhythm, frequency 65/min. Negative T-waves in the inferior leads resulting from post myocarditis affection
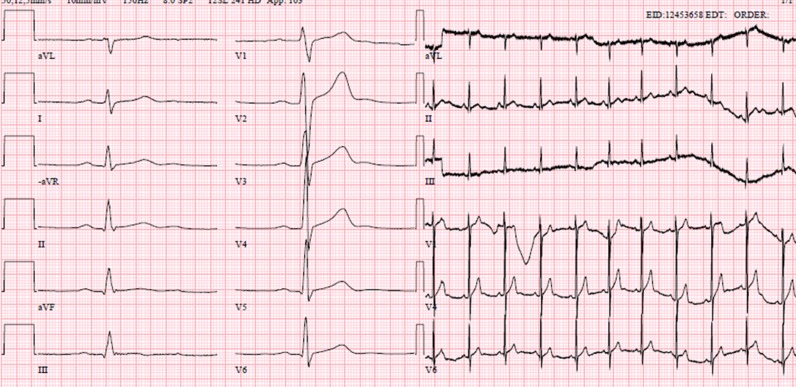
Figure 5:
ECG from follow-up, 6 weeks after admission. ECG shows normal sinus rhythm, frequency 64/min. Normalization of the previous ECG-reactions have occurred
DISCUSSION
In this case report we add to the limited numbers of patients with myocarditis due to salmonella infection. One risk factor for myocarditis is testosterone which can explain the fact that most cases, including ours, are males [4, 8]. However, other factors, such as immunological function and innate immunity are most likely present since his friend never developed any cardiac manifestations. The effect of innate immunity has been showed in animal models, but other studies also show a high prevalence of subclinical or under-recognized myocarditis indicating that, if tested, his friend might have had ECG changes or elevation of troponin [1, 4]. Molecular mimicry might also result in autoimmune like attack on myosin that contributes to the damage [9]. In our case, the diagnosis was determined by CMRI in conformity with the consensus document [6].
The most known disease due to Salmonella is typhoid fever or enteric fever caused by Salmonella typhi (S. typhi and S. paratyphi) These species are the most frequent reported species causing salmonella associated myocarditis but other non-typhoid salmonella (NTS), as in our case, are also infrequently reported but the mortality rate and morbidity cannot be specified [8]. Myocarditis might however lead to dilated cardiomyopathy that hold severe morbidity and mortality. For patients with dilated cardiomyopathy the underlying cause is myocarditis in ~9% [10]. Our patient had no known risk factors indicating that otherwise healthy subject can also be at risk [7, 11].
NTS-myocarditis were studied in a systematic review including 24 patients, that showed that the most presenting signs were fever, abdominal pain and chest pain and the most common pathogen were S. enteritidis [8]. These results corresponds to our patients symptoms. S. enteritidis are one of the most common serotypes worldwide with acute gastroenteritis being the most common presentation. Normally, the illness follows a benign course of 4–7 days that resolves without antibiotics but fatal conditions might seldom occur [7].
The awareness of the potential lethal course of NTS is need of further recognition. A high suspicion and low threshold for ECG and troponin, in patients with NTS-infections might reveal more patients with subclinical myocarditis.
ACKNOWLEDGEMENTS
Futurum—the academy for healthcare, Region Jönköping County.
CONFLICT OF INTEREST STATEMENT
None of the authors has a financial relationship with a commercial entity that has an interest in the subject of the presented article, or any other conflict of interest to disclose.
FUNDING
There were no sources of funding.
ETHICAL APPROVAL
No approval is required.
CONSENT
A fully written consent to publish the case report was obtained from the patient.
GUARANTOR
Dr Per Sundbom, Dr Anne-Marie Suutari, Dr Karim Abdulhadi, Dr Wojciech Broda and Dr Melinda Csegedi.
REFERENCES
- 1. Trachtenberg BH, Hare JM. Inflammatory cardiomyopathic syndromes. Circ Res 2017;121:803–18. [DOI] [PubMed] [Google Scholar]
- 2. Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980–2006. Circulation 2009;119:1085–92. [DOI] [PubMed] [Google Scholar]
- 3. Cooper LT Jr., Keren A, Sliwa K, Matsumori A, Mensah GA. The global burden of myocarditis: part 1: a systematic literature review for the Global Burden of Diseases, Injuries, and Risk Factors 2010 study. Glob Heart 2014;9:121–9. [DOI] [PubMed] [Google Scholar]
- 4. Elamm C, Fairweather D, Cooper LT. Pathogenesis and diagnosis of myocarditis. Heart 2012;98:835–40. [DOI] [PubMed] [Google Scholar]
- 5. Cooper LT., Jr Myocarditis. N Engl J Med 2009;360:1526–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Friedrich MG, Sechtem U, Schulz-Menger J, Holmvang G, Alakija P, Cooper LT, et al. Cardiovascular magnetic resonance in myocarditis: a JACC White Paper. J Am Coll Cardiol 2009;53:1475–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gordon MA. Salmonella infections in immunocompromised adults. J Infect 2008;56:413–22. [DOI] [PubMed] [Google Scholar]
- 8. Villablanca P, Mohananey D, Meier G, Yap JE, Chouksey S, Abegunde AT. Salmonella Berta myocarditis: case report and systematic review of non-typhoid Salmonella myocarditis. World J Cardiol 2015;7:931–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bracamonte-Baran W, Cihakova D. Cardiac autoimmunity: myocarditis. Adv Exp Med Biol 2017;1003:187–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Felker GM, Hu W, Hare JM, Hruban RH, Baughman KL, Kasper EK. The spectrum of dilated cardiomyopathy. The Johns Hopkins experience with 1,278 patients. Medicine (Baltimore) 1999;78:270–83. [DOI] [PubMed] [Google Scholar]
- 11. Leonard J, Marshall JK, Moayyedi P. Systematic review of the risk of enteric infection in patients taking acid suppression. Am J Gastroenterol 2007;102:2047–56. quiz 57. [DOI] [PubMed] [Google Scholar]