Abstract
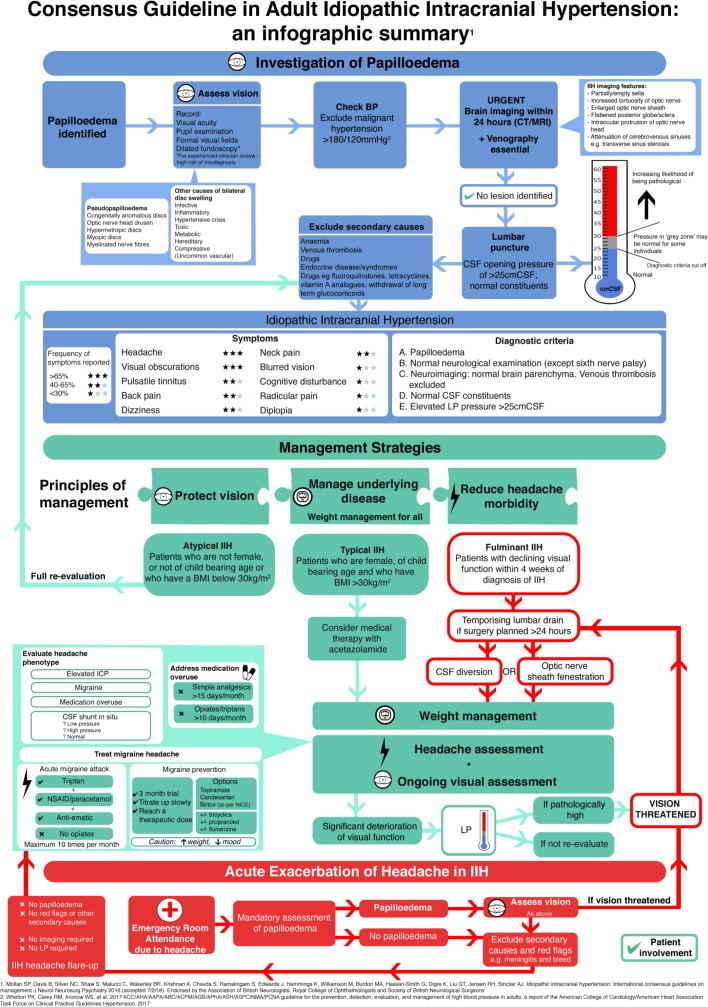
This paper summarises the first consensus guidelines for idiopathic intracranial hypertension as an infographic. Following a systematic literature review, a multidisciplinary specialist interest group met and established questions relating to population, interventions, controls and outcomes (PICO). A survey was sent to doctors who manage idiopathic intracranial hypertension (IIH) regularly. Statements were reviewed by national professional bodies, specifically the Association of British Neurologists, British Association for the Study of Headache, the Society of British Neurological Surgeons and the Royal College of Ophthalmologists and by international experts. Key areas are represented based on the guideline, namely: (1) investigation of papilloedema and diagnosis of IIH; (2) management strategies; and (3) investigation and management of acute exacerbation of headache in established IIH. We present an infographic as an aide-mémoire of the first consensus guidelines for IIH.
Keywords: idiopathic intracranial hypertension, headache, benign intracran hyp, neuroophthalmology, papilloedema
IIH is commonly associated with obesity, younger age and females.1 2 Patients present acutely to many different specialities and often have multiple acute visits through the course of their disease. The investigation and management of IIH is complex involving many specialities.3 This infographic summarises three key pathways based on the recommendations of a multidisciplinary, patient-involving and multiprofessional specialist interest group on the investigation and management of IIH.4
The basis of the specialist interest group included representation from neurology, neurosurgery, neuroradiology, ophthalmology, nursing, primary care doctors and patient representatives. Questions on PICO were defined and through a large Delphi group exercise; expertise was captured from a wide-reaching group of clinicians, thus reflecting practice from across the UK and internationally. The statements were then critically reviewed by key opinion leaders and by Association of British Neurologists, British Association for the Study of Headache, the Society of British Neurological Surgeons and the Royal College of Ophthalmologists. This is the first consensus guidance for optimal management of IIH.4
Identification of papilloedema can be challenging, and clinicians should be aware of the differential diagnosis of pseudopapilloedema (figure 1). Once papilloedema is confirmed, it requires urgent investigations, including lumbar puncture, where the patient experience could be greatly improved.5 Symptoms of IIH are not pathognomonic, and hence it is essential to apply the diagnostic criteria, including excluding secondary causes, for a definite diagnosis.4 The lumbar puncture opening pressure was one key area of debate. Within the wider Delphi group, it was clear that there is a ‘grey zone’ of lumbar puncture opening pressures between 25 cm cerebrospinal fluid (cmCSF) and 30 cmCSF, as to what each expert considered to be pathological, and this is reflected within the infographic thermometer for lumbar puncture opening pressure (figure 1).
Figure 1.
Consensus Guideline in Adult Idiopathic Intracranial Hypertension: an infographic summary.
Principles of management need to address both the rapidity of the disease that may lead to visual loss in some and require surgical intervention and the morbidity of the headache that can develop in the majority, which substantially affects the quality of life.6 Weight loss is currently the only established disease-modifying therapy7 and is notoriously difficult to achieve and maintain.
Evaluation of the headache phenotype is essential to target treatment and to help identify medication-overuse headache. Where there are features of migraine, topiramate may be the first line in treatment, and recent evidence indicates that it has a significant intracranial pressure-lowering effect in rodents.8 Acute exacerbation of headache often leads to reinvestigation with lumbar puncture, and the collective expert opinion reflected that lumbar puncture provides only temporary relief, can lead in some to longer term complications9 and exacerbation of headache.10 In those with acute exacerbation of headache, optic nerve examination is essential, and in those found not to have papilloedema, investigation with lumbar puncture and brain imaging is not required, so long as no other secondary causes of headache are suspected. The infographic illustrates the management of acute exacerbation of headache in IIH (figure 1).
Horizon scanning for IIH shows that research is active and that metabolic concepts may potentially provide more understanding of the cause and provide evidence for innovative therapeutic opportunities.11 A phase 2 randomised control trial with the first novel drug treatment for IIH has finished recruitment12; a phase 3 randomised control trial investigating the best method for weight loss is underway13; other surgical trials are in planning.
This infographic highlights three areas that are covered by the consensus guideline for adult IIH, which are: (1) investigation of papilloedema and diagnosis of IIH; (2) management strategies; and (3) investigation and management of acute exacerbation of headache in established IIH4 (figure 1).
Key points.
Cerebral venography is an essential part of the work-up to exclude venous sinus thrombosis as a cause of papilloedema.
Lumbar puncture opening pressure forms part of the diagnostic criteria; however, most clinicians feel there is a ‘grey zone’ between 25 cmCSF and 30 cmCSF, which may not be pathological.
Those with fulminant or precipitous visual decline need urgent surgical treatment, preferably with a ventriculoperintoneal shunt.
All patients diagnosed with idiopathic intracranial hypertension need sensitive and appropriate discussion regarding weight loss (the only disease-modifying treatment).
Those with acute exacerbation of headache do not require further neuroimaging or repeat lumbar puncture, unless there are red flag symptoms/signs of infection, or papilloedema with precipitous visual decline.
Acknowledgments
We acknowledge all those who contributed to the surveys and critiqued the document in the wider Delphi group. The specialist interest group members and international key opinion leaders: Brendan Davis (University Hospital North Midlands NHS Trust), Nick Silver (The Walton Centre NHS Foundation Trust), Simon Shaw S (University Hospital North Midlands NHS Trust), Conor Mallucci (The Walton Centre NHS Foundation Trust and Alder Hey Children’s NHS Foundation Trust), Ben Wakerley (Gloucestershire Hospitals NHS Foundation Trust), Anita Krishnan (The Walton Centre NHS Foundation Trust), Swarup Chavda (University Hospitals Birmingham NHS Foundation Trust), Sateesh Ramalingam (University Hospitals Birmingham NHS Foundation Trust), Julie Edwards (University Hospitals Birmingham NHS Foundation Trust and Sandwell and West Birmingham NHS Trust), Krystal Hemmings (IIH UK Charity), Shelly Williamson (IIH UK Charity), Mike Burdon (University Hospitals Birmingham NHS Foundation Trust), Ghaniah Hassan-Smith G(University of Birmingham), Kathleen Digre (Moran Eye Center, University of Utah) Grant Liu (Children’s Hospital of Philadelphia and Hospital of the University of Pennsylvania), Rigmor Jensen (Danish Headache Centre, Copenhagen). Collaborators:Jane Anderson, (Cambridge University Hospitals NHS Foundation Trust), Peter Goadsby (King’s College Hospital), Tim Matthews (University Hospitals Birmingham NHS Foundation Trust) and Jan Hoffman (University Medical Centre Hamburg).
Footnotes
Contributors: SPM and AJS drafted the infogram. CH executed the drawing of the infogram. SPM wrote the initial draft. JM and AJS critically reviewed the paper and infogram.
Funding: AJS is funded by an NIHR Clinician Scientist Fellowship (NIHR-CS-011-028) and by the Medical Research Council, UK (MR/K015184/1).
Competing interests: None declared.
Patient consent: Not required.
Provenance and peer review: Commissioned; externally peer reviewed by Joseph Anderson, Cardiff, UK and Mark Lawden, Leicester, UK. The guideline was also reviewed, critiqued and supported by the following professional bodies: The Association of British Neurologists, the Society of British Neurological Surgeons, the Royal College of Ophthalmologists and the British Association for the Study of Headache.
Collaborators: Brendan Davis (University Hospital North Midlands NHS Trust), Nick Silver (The Walton Centre NHS Foundation Trust), Simon Shaw (University Hospital North Midlands NHS Trust), Conor Mallucci (The Walton Centre NHS Foundation Trust and Alder Hey Children’s NHS Foundation Trust), Ben Wakerley (Gloucestershire Hospitals NHS Foundation Trust), Anita Krishnan (The Walton Centre NHS Foundation Trust), Swarup Chavda (University Hospitals Birmingham NHS Foundation Trust), Sateesh Ramalingham (University Hospitals Birmingham NHS Foundation Trust), Julie Edwards (University Hospitals Birmingham NHS Foundation Trust and Sandwell and West Birmingham NHS Trust), Krystal Hemmings (IIH UK Charity), Shelly Williamson (IIH UK Charity), Mike Burdon (University Hospitals Birmingham NHS Foundation Trust), Ghaniah Hassan-Smith (University of Birmingham), Kathleen Digre (Moran Eye Center, University of Utah) Grant Liu (Children’s Hospital of Philadelphia and Hospital of the University of Pennsylvania), Rigmor Jensen (Danish Headache Centre, Copenhagen), Jane Anderson, (Cambridge University Hospitals NHS Foundation Trust), Peter Goadsby (King’s College Hospital), Tim Matthews (University Hospitals Birmingham NHS Foundation Trust) and Jan Hoffman (University Medical Centre Hamburg).
Correction notice: This article has been corrected since it was published Online First. The provenance and peer review disclaimer incorrectly said the paper was not commissioned.
References
- 1. Mollan SP, Ali F, Hassan-Smith G, et al. Evolving evidence in adult idiopathic intracranial hypertension: pathophysiology and management. J Neurol Neurosurg Psychiatry 2016;87:982–92. 10.1136/jnnp-2015-311302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Markey KA, Mollan SP, Jensen RH, et al. Understanding idiopathic intracranial hypertension: mechanisms, management, and future directions. Lancet Neurol 2016;15:78–91. 10.1016/S1474-4422(15)00298-7 [DOI] [PubMed] [Google Scholar]
- 3. Mollan SP, Markey KA, Benzimra JD, et al. A practical approach to, diagnosis, assessment and management of idiopathic intracranial hypertension. Pract Neurol 2014;14:380–90. 10.1136/practneurol-2014-000821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mollan SP, Davies B, Silver NC, et al. Idiopathic intracranial hypertension: consensus guidelines on management. J Neurol Neurosurg Psychiatry 2018. 10.1136/jnnp-2017-317440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Scotton WJ, Mollan SP, Walters T, et al. Characterising the patient experience of diagnostic lumbar puncture in idiopathic intracranial hypertension: a cross-sectional online survey. BMJ Open 2018;8:e020445 10.1136/bmjopen-2017-020445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mulla Y, Markey KA, Woolley RL, et al. Headache determines quality of life in idiopathic intracranial hypertension. J Headache Pain 2015;16:45 10.1186/s10194-015-0521-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sinclair AJ, Burdon MA, Nightingale PG, et al. Low energy diet and intracranial pressure in women with idiopathic intracranial hypertension: prospective cohort study. BMJ 2010;341:c2701 10.1136/bmj.c2701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Scotton WJ, Botfield HF, Westgate CS, et al. Topiramate is more effective than acetazolamide at lowering intracranial pressure. Cephalalgia 2018;1:033310241877645 10.1177/0333102418776455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Engelborghs S, Niemantsverdriet E, Struyfs H, et al. Consensus guidelines for lumbar puncture in patients with neurological diseases. Alzheimers Dement 2017;8:111–26. 10.1016/j.dadm.2017.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Yiangou A, Mitchell J, Markey KA, et al. Therapeutic lumbar puncture for headache in idiopathic intracranial hypertension: Minimal gain, is it worth the pain? Cephalalgia 2018;1:033310241878219 10.1177/0333102418782192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hornby C, Mollan SP, Botfield H, et al. Metabolic concepts in idiopathic intracranial hypertension and their potential for therapeutic intervention. J Neuroophthalmol 2018. doi: 10.1097/WNO.0000000000000684 [Epub ahead of print 6 Jul 2018]. 10.1097/WNO.0000000000000684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Markey KA, Ottridge R, Mitchell JL, et al. Assessing the Efficacy and Safety of an 11β-Hydroxysteroid Dehydrogenase Type 1 Inhibitor (AZD4017) in the Idiopathic Intracranial Hypertension Drug Trial, IIH:DT: clinical methods and design for a phase II randomized controlled trial. JMIR Res Protoc 2017;6:e181 10.2196/resprot.7806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ottridge R, Mollan SP, Botfield H, et al. Randomised controlled trial of bariatric surgery versus a community weight loss programme for the sustained treatment of idiopathic intracranial hypertension: the Idiopathic Intracranial Hypertension Weight Trial (IIH:WT) protocol. BMJ Open 2017;7:e017426 10.1136/bmjopen-2017-017426 [DOI] [PMC free article] [PubMed] [Google Scholar]