Abstract
Introduction
Mindfulness is one of the potential alternative interventions for children with attention-deficit hyperactivity disorder (ADHD). Some evidence suggests that mindfulness is related to changes in brain regions associated with ADHD. The potential benefits of mindfulness on children with ADHD, as well as the feasibility of this intervention approach, are warranted through prior local and foreign studies. This study aims to evaluate the effect of mindfulness-based group intervention for children with ADHD and their respective parents through a robust research design.
Methods and analysis
This study will adopt a randomised controlled trial design including 140 children aged 8–12 years with ADHD together with one of their parents (n=140). These families will be randomised into intervention group (n=70) who will be offered the MYmind programme delivered by trained healthcare professionals, and an active control group (n=70) who will be offered the CBT programme. The intervention includes 8 weekly 90 min group sessions for children with ADHD (aged 8–12 years) and their respective parents. The primary and secondary outcomes will include children’s attention, ADHD-related symptoms, behaviours, executive function and mindfulness levels measured by validated objective measures and parent’s reported instruments. Parents’ parental stress, parenting styles, ADHD related symptoms, well-being, rumination level and mindfulness levels will also be measured. Analysis is by intention to treat. The effects of intervention will be evaluated by comparing outcomes between the two arms, as well as comparing outcomes within subject through comparing measurements at baseline (T0), immediately after the 8 week intervention (T1) and at 3 (T2) and 6 (T3) months postintervention.
Ethics and dissemination
Ethics approval has been granted by the Joint Chinese University of Hong Kong – New Territories East Cluster Clinical Research Ethics Committee (The Joint CUHK-NTEC CREC). Participants will be required to sign informed consent form from both parents and children. Findings will be reported in conferences and peer-reviewed publications in accordance with recommendations of Consolidated Standards of Reporting Trials.
Trial registration number
ChiCTR1800014741; Pre-results.
Keywords: Mindfulness-based therapy (MBT), Attention-Deficit Hyperactivity Disorder (ADHD), randomized controlled trial (RCT), Chinese family, attention and impulsivity, stress
Strengths and limitations of this study.
A randomised controlled trial with a relatively large sample size and long follow-up period, as well as an active control group to control for non-specific effects.
Both children with attention-deficit hyperactivity disorder and their respective parents undergo intervention at the same time that may benefit them directly and indirectly, and the intervention is group based, which might be more cost-effective than one-on-one intervention.
Both objective and subjective measures are applied to test attention.
Only children aged 8–12 years with normal intelligence are included.
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a common neurodevelopmental childhood disorder.1 A study published in 2015 showed that the global prevalence was found to be 3.4%.2 In Hong Kong, the prevalence was found to be 3.9% among high school students aged 13.8 years.3 ADHD is regarded as a costly public health problem.4 The core symptoms of inattention, hyperactivity and impulsivity are associated with different pervasive functional problems among individuals with ADHD.5 They experience poorer academic achievements, poorer peer relationships, lack of constructive leisure activities, higher rates of job turnover, as well as higher rates of emergency room visits and automobile accidents as compared with their age-mates.5 Moreover, comorbid mental health problems are common among individuals with ADHD, such as disruptive mood dysregulation disorder, anxiety disorders, major depressive disorder, obsessive-compulsive disorder and substance use disorder.6 All these problems associated with ADHD cast a significant economic cost to society. The annual cost in USA of ADHD was estimated at between $36 billion and $52 billion in 2005.7
Pharmacological intervention is widely used as the main treatment option in view of the neurobiological nature of ADHD. Individuals with ADHD have abnormalities in the right prefrontal region, the basal ganglia and the cerebellum, as well as dysfunction in neurotransmitter, such as norepinephrine and dopamine.8–11 Stimulants such as methylphenidate are widely prescribed to regulate the associated brain functions and to control symptoms associated ADHD.12 The conservative attitude towards medication among Chinese parents likely explains why the prevalence of ADHD medication use among Hong Kong children is lower than that of other developed countries13 and that the medication adherence rate was found to be low in a community sample of children with ADHD.14 In Hong Kong, the adherence rate was found to be about 50%–80% after 1 year of medical treatment with the adherence rate further reduced to about 36%–46% after 5 years of medical treatment.12 It has been speculated that the low adherence rate is both related to the side effects and stigma associated with the use of medication.13 Therefore, alternative interventions for children with ADHD that carry fewer side effects and with less associated stigma are needed.
Behavioural parent management training and cognitive–behavioural therapy (CBT) for ADHD are common non-pharmacological interventions for children with ADHD. For behavioural parent management training, studies have shown that children who have parents diagnosed with ADHD have poor response to parent training, which is common among parents of children with ADHD.15 Another problem often experienced by families of children with ADHD is ‘parental over-reactivity’16 and elevated parenting stress.17 Although CBT has been used for adults with ADHD,15 very limited evidence supports the use of CBT among younger children.18–20 A recent meta-analysis also found limited evidence of behavioural training and CBT in improving children’s ADHD symptoms when blinded rating is used, and it shows no effect on parent’s mental well-being21 though other benefits are found such as parenting quality and children’s conduct problems.21 As there is no current intervention that targets both parents’ and children’s core problems at the same time, an intervention that helps both children’s behavioural (inattention, impulsivity and hyperactivity) problems and parents’ mental well-being can be a promising alternative intervention for families of children with ADHD.
Mindfulness training aims to cultivate awareness by teaching participants to pay attention at the present moment non-judgementally. It has been suggested as a self-regulatory method for strengthening attentional processes that include orienting, alerting and executive attention.22 Mindfulness training involves formal practices such as walking meditation, sitting mediation, mindful eating, mindful movements and body scan.23 It teaches participants to focus their attention on the experience of emotions, thoughts, body sensations and sounds and to observe them as they arise and subside. Over the last three to four decades, mindfulness-based interventions have become a popular type of intervention in mental health, and accumulating evidence supports the applicability of mindfulness-based interventions in treating common mental health problems.24
There is evidence from neuropsychological research that supports mindfulness training as a potential treatment specifically for children with ADHD. Mindfulness training can increase an individual’s ability to control attention and reduce automatic responses,25 which can be beneficial for people with ADHD as their impairments lie in their inability to control attention as well as their impulses to act. Studies show that mindfulness training can improve performance on executive functioning tasks such as attention, working memory and cognitive control.26 In addition, some evidence suggests that mindfulness is related to changes in grey matter concentration in brain regions involving attention regulation and emotion regulation,27 as well as neuroplastic changes in brain areas including the prefrontal cortex,28 which are also areas of abnormalities in individuals with ADHD. Hölzel et al 27 reviewed current evidence and proposed that mindfulness training works because it causes changes in attention regulation, body awareness, emotion regulation and so on.
With the potential benefits of mindfulness on children with ADHD, more research has been conducted in this area. In 2008, Bögels and colleagues29 in a mixed sample of adolescents with ADHD, oppositional defiant disorders and autism spectrum disorders showed that participating in a mindfulness meditation—MYmind—was associated with improvements on externalising problems and sustained attention. In view of the bidirectional effect between parenting stress and behavioural problems of children with developmental disability,30–32 parallel mindfulness group intervention for parents was rendered in addition to the mindfulness group training for the children with ADHD in this MYmind programme. Another pilot study33 using mindfulness training for children aged 8–12 years with ADHD (n=22) and their parents also showed promising results although only a preintervention and postintervention design was used. In the study, parenting stress and parental over-reactivity were significantly reduced with moderate to large effects, and there were significant improvements for adolescents’ ADHD symptoms. Another recent non-controlled preintervention and postintervention study on 10 adolescents and 19 of their parents, using the same mindfulness intervention for adolescents with ADHD and their parents, demonstrated improvements in both attention and behavioural problems reported by parents and teachers as well as improvement in performance measured by attention tests after mindfulness training.34 In addition, reductions in parenting stress among fathers and over-reactive parenting among mothers29 33 were observed. A study35 published in 2015 on 18 adolescents aged 13–18 years with ADHD and 17 of their parents, using the mindfulness-based intervention, demonstrated that adolescents who received mindfulness training had reductions in inattentiveness and conduct problems with improvements in adolescent peer relations. For parents, reductions in parenting stress and an increase in parental mindfulness were also observed.35
Although the feasibility of using mindfulness training for children with ADHD was demonstrated by previous studies, research in this area is still in its early stage. Only a few studies29 33–37 have been conducted to evaluate its effectiveness. None of the studies adopted robust research design such as randomised controlled trials with satisfactory sample size, and most did not include objective measurements such as neurocognitive tests that measure attention.38 Also, all the existing studies in this area were evaluated in Caucasian paediatric populations with ADHD.39 One pilot study with pretest and post-test without control was conducted among 11 Chinese children with ADHD and their parents (n=11). The preliminary results of this study were promising, and the intervention was well accepted by participants40 although the findings were limited by the small sample.
Given important cultural differences in parenting style41 as well as differences in academic environments42 in Hong Kong as compared with those of overseas countries, parents in Hong Kong have a greater general emphasis on academic achievements in school. The motivation of Hong Kong parents to engage their children with ADHD in regular mindfulness practices within this high academic stress environment may be less than those of parents in the West. Thus, it is important to evaluate the effectiveness of mindfulness-based training on Chinese children as well as their parents to further assess cultural acceptability and effectiveness. Moreover, since most studies conducted so far were not randomised controlled studies, a more rigorous study design with randomisation of participants and the inclusion of a control group is needed to further evaluate the validity of results from previous studies. Therefore, we adopt an active control group to control for therapist’s attention, group effect and social interaction. Finally, as many of the preliminary studies have relied only on self-reported outcomes, objective outcomes are used to reduce self-report bias and to further improve the validity of findings.
Objectives and hypotheses
Objectives
To evaluate the effectiveness of a mindfulness-based intervention—MYmind—in improving children’s attention, behaviour and executive function, and mindfulness level as well as reducing impulsivity associated with ADHD in children aged 8–12 years and who are diagnosed with ADHD in Hong Kong.
To evaluate the effectiveness of MYmind in reducing parental stress, ADHD symptoms and rumination level, and improving well-being among parents of children diagnosed with ADHD.
The hypotheses are:
Children and adolescents in the mindfulness intervention group would have improved attention, executive function, and mindfulness level, as well as reduced behavioural problems than those of the active control group.
Parents of children or adolescents with ADHD in mindfulness intervention would report significantly greater reduction in parental stress, ADHD symptoms and rumination level, and better well-being than those of the active control group.
Methods
Study design
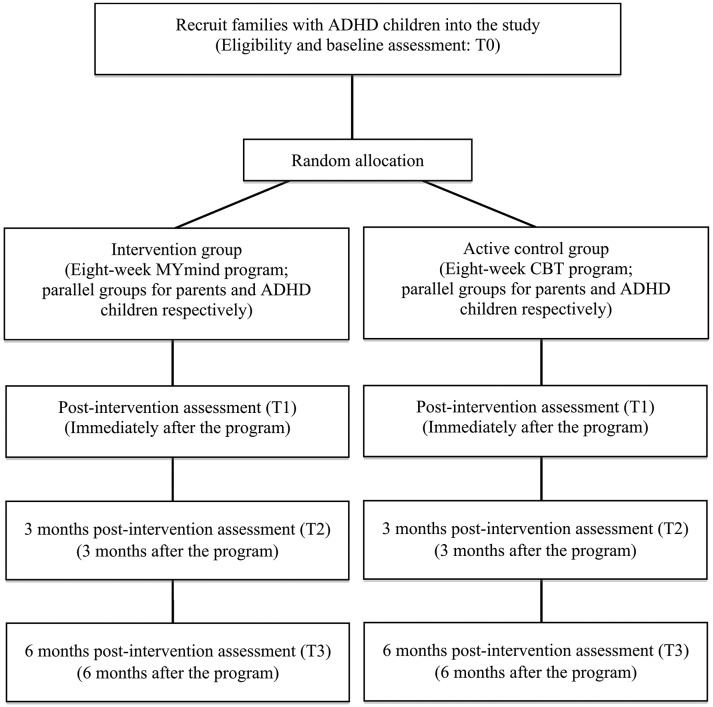
This will be a two-arm randomised controlled trial that compares the mindfulness training for children and mindful parenting (MYmind intervention) with CBT (active control) for children and psychoeducation for parents. Assessments of outcomes will be conducted at baseline (T0), immediately after the 8-week intervention (T1) and at 3 months and 6 months postintervention (T2 and T3). Summary of the study design is shown in figure 1.
Figure 1.
Proposed procedure and flow of participants of the study. ADHD, attention-deficit hyperactivity disorder; CBT, cognitive–behavioural therapy.
Participants
Participants will include children and one parent of each child. The inclusion criteria will be: (1) children aged 8–12 years with psychiatrist or psychologist diagnosed ADHD according to the Diagnostic and Statistical Manual of Mental Disorders – 52 diagnostic criteria or equivalent. The ADHD status will be reconfirmed by clinically elevated inattentive and/or hyperactive-impulsive symptoms as indicated by T-scores of either parent and teacher versions of Strengths and Weaknesses of ADHD-symptoms and Normal-behaviour (SWAN; Chinese version),43 at or above 95th percentile, or both parent and teacher versions of the SWAN (Chinese version),43 at or above 85th percentile; (2) with normal intellectual ability such that they can understand the materials delivered in MYmind and that they can complete home practice each week; and (3) children either not taking any medication or taking a stable dosage of the same medication for ADHD for at least 3 months prior to study enrolment and having no plan for changing medication during the study period.
The exclusion criteria of children and parents will be: (1) being unable to communicate and understand Cantonese as the intervention will be conducted in Cantonese; (2) the child having comorbid conduct/behaviour problems that are so severe that, during intake, the interaction between parent and assessor is interrupted by the child within 2 min, which makes it impossible for the child to participate in a group training (adapted from a task in the Autism Diagnostic Observation Schedule); (3) having a medical or mental health condition rendering him/her to be incapable of participating in the study; and (4) previous participation in mindfulness-based training.
Study setting and recruitment
This will be a collaborative study that involves non-governmental organisations (NGOs) serving families of children with ADHD. Both children and parents will be recruited through NGOs and parent support group during their regular education sessions for parents in the community, as well as through their monthly newsletter. The partnership between academic centre, community NGOs and parent support group will also enhance dissemination and implementation of findings in the future.
Intervention: MYmind for children with ADHD and their parents
The mindfulness-based intervention will be based on an established protocol (MYmind) used in previous studies conducted in the Netherlands,33 34 which is specifically designed for children with ADHD and their parents. This protocol will be used in the proposed study with modifications based on feedbacks and observation in our pilot that includes extending the break time for the children group and slight change of teaching order in the parent’s group. The protocol of MYmind was established based on Mindfulness-Based Cognitive Therapy (MBCT)44 and Mindfulness-Based Stress Reduction Training (MBSR)45 and was adapted for use with parents and children with ADHD. The intervention includes 8 weekly 90 min group sessions for children with ADHD and their respective parents, as shown in online supplementary appendix 1.29 The intervention will be delivered mainly in separate groups for parents and children concurrently, following the training manual.
bmjopen-2018-022514supp001.pdf (117.2KB, pdf)
To encourage participation and retention, tokens will be given to children for completing homework and for participating in exercises during the sessions. With accumulation of tokens, rewards will be given for encouragement. Other aspects of the programme that aim to increase treatment compliance (highly structured programme, establishment of ground rules, breaks at regular intervals and the inclusion of a helper in addition to the instructor) will also be adopted. The children’s group will consist of 5–6 children, and the parent group will consist of 6–12 parents. Parents and children will receive session handouts describing the session theme, instructions for practice and homework completion forms (mindfulness practice diaries) and will be given recordings of mindfulness exercises to practise at home. All the teaching materials and handouts and instructions for practice have been translated into Chinese by qualified health professionals and were used in our pilot. The content of the translated versions was further face validated by a group of educational psychologists, social workers and clinical psychologists who provide services for children with ADHD and their families and who have undergone formal training with mindfulness training.
Instructors will be recruited to provide the mindfulness training. They should be health professionals (in psychology, social work, education, nursing or medicine) and have completed an 8-week mindfulness training programme (either MBSR or MBCT) in addition to completing the MYmind intensive training programme run by Professor Susan Bögels, who is the founder of the programme, or other accredited MYmind trainers (over 80 health professionals have attended her training in January 2015 and November 2017 in Hong Kong).
Active control: CBT
Children in the active control group will be given group CBT, and their parents will be given group psychoeducation (online supplementary appendix 2) in 8 weekly 90 min sessions. The group psychoeducation conducted will be based on a treatment protocol designed by experienced healthcare professionals in psychology and family medicine, taking reference from the current guidance of CBT treatment for children with ADHD and their families46–48 and local training guidance.49 CBT for children will include training on problem solving, self-control, academic problems handling, understanding and response to emotions, listening and conversational skills, perspective taking in social situations and social problems handling. Parents will be trained with the above skills and will be invited to identify children’s related problems as well as to understand and support children’s CBT training. The intervention will also be delivered in separate groups for parents and children concurrently.
Intervention fidelity
The intervention will be assessed for fidelity of implementation by audio-taping all group sessions. Independent reviewers, who are healthcare professionals with prior training on psychotherapy and/or MYmind, will be recruited to review 20% of all audiotapes randomly selected and rate the level of compliance to the intervention protocol of MYmind treatment manual and CBT treatment protocol.
Randomisation, concealment and blindness
One research assistant will screen potential participants for eligibility through telephone interviews. Participants will be scheduled for an interview with an investigator and the research team to further confirm inclusion and exclusion criteria, explain the study objectives and procedures, obtain informed consent and conduct baseline assessments. The eligible participants will be allocated to the two treatment conditions by an experienced independent statistician using computer-generated random results. The allocation ratio is 1:1. The randomisation results will be kept in sealed, opaque envelopes by a research assistant who is not involved in the study. Participants will be informed of their group assignments by the research staff using the predetermined results in the sealed, opaque envelopes. Treatment allocation cannot be changed after randomisation. The research staff member who conducts the assessments or the statistical analysis will be kept blinded of the group assignment.
Outcome measures
Basic demographic data will be collected at baseline, for example, age, gender, education, income and employment. Children’s medication use including name, duration and dosage as well as the presence of any previous diagnosis of comorbidities will be recorded. Primary and secondary outcome measures will be collected by a trained research assistant blinded to the group assignment at baseline (T0), postintervention (T1) and 3 months and 6 months postintervention (T2 and T3).
Primary outcome (for children)
Attention score of Sky Search subtest of the Test of Everyday Attention for Children (TEA-Ch) 50 at T3 is adopted as the primary outcome for this study. The TEA-Ch, a game-like test, was widely used by healthcare professionals in Hong Kong to test for attention of local children.51 In the Sky Search subtest, children need to circle as many pairs of identical craft as possible on an A3-size sheet as quickly as possible. Children then complete a motor control version of the test. The attention score is then calculated by subtracting the motor control time per target from the Sky Search time per target. This subtest is measuring the selective attention of children.
Secondary outcomes (for children)
Sustained attention and attention control/switching: another three subtests of the TEA-Ch (Creature Counting, Opposite Worlds and Code Transmission) that measure sustained attention and attention control/switching.50 Creature Counting needs children to count the creatures following the route and use the up and down arrows to decide whether to switch the direction of their counting. The scores are the number of correct responses and the time score that is total time divided by total switches for correct items. In Opposite Worlds, children need to announce a number of digits, that is, 1 and 2, in a line in the same word and announce the digits 2 and 1 when they see 1 and 2 in the opposite world as quickly as possible. They need to correctly announce before they move on to the next digit. The time taken is the score. In Code Transmission, children listen to a 12 min audio record and immediately announce the number before a code once they hear them. The score is the number of correctly identified numbers.
Attention measured by computerised programme: The Child Attention Network Test (ANT) is a computerised assessment of attention.52 It is designed to test three attentional networks in children: alerting, orienting and executive control. Alerting is defined as attaining and maintaining an alert state. Orienting is defined as the selection of information from sensory input. The executive control is defined as resolving conflict among responses.52
ADHD symptoms: the SWAN Rating Scale (parent version) is an 18-item rating scale for children with ADHD to measure children’s abilities to focus attention, control activity and inhibit impulses. The Chinese version has satisfactory reliability and validity.43
Disruptive behaviour: The Eyberg Child Behaviour Inventory (ECBI) is a 36-item, self-report questionnaire to measure parents’ perception of disruptive behaviours in children aged 2–16 years old, such as non-compliance and aggression.53
Executive function: the Behavior Rating Inventory of Executive Function (BRIEF) will measure children’s executive function with high internal consistency. The tool was used among Han Chinese students in a previous study54 with higher scores indicate poorer executive functions.
Mindfulness: The Child and Adolescent Mindfulness Measure (CAMM) will measure the mindfulness levels among the children. The scale is currently under validation by our research team.55
Secondary outcomes (for parents)
Parenting stress: the Parenting Stress Index (PSI) a 36-item questionnaire measuring parenting stress, with higher scores indicating higher stress. The Chinese version was validated and used previously in Hong Kong.56 Three subscale scores will be computed in addition to the total score: parental distress, parent–child dysfunctional interaction and difficult child.
ADHD symptoms: Adult ADHD Self-Report Scale (ASRS) is an 18-item validated ASRS (version 1.1) symptom checklist will be used to assess parents’ ADHD symptoms. The Chinese version has showed good reliability and validity.57
Well-being: the WHO (Five) Well-Being Index (WHO-5) will measure well-being. A summed score below 13 indicates poor mental health. This scale has been translated into more than 30 languages including Chinese.58
Rumination: Rumination Response Scale (RRS): it is a 22-item measure of rumination level that describes ruminative responses to depressed mood that are self-focused, symptom-focused or behavioural.59
Patient and public involvement
Patients or the public are not involved in the design and will not involve in recruitment and conduction of the study. Perceived levels of easiness, usefulness and satisfaction of the intervention by both children and parents will be collected on a Likert scale of 1–10 representing ‘not easy/helpful/satisfied at all’ to ‘extremely easy/helpful/satisfied’. The study results or individual outcomes will be disseminated to study participants on request.
Data and statistical analysis
Data will be saved in password-protected computers and locked cabinet. Only the study team will have the access to the data. Data will be reported aggregately, and no personal identity will be revealed from any reports. The Consolidated Standards of Reporting Trials (CONSORT) 10 standards will be used in reporting the study results. Mean (SD), median (IQR), frequency and percentage and 95% CI will be used for data description. Linear mixed models will be used to assess whether MYmind improves TEA-Ch (primary outcome) and other results of TEA-Ch, ANT, SWAN, BRIEF, ECBI, PSI, PS, ASRS, RRS and WHO-5 (secondary outcomes). A series of χ2 and univariate analysis of variance will be conducted to examine whether there are any demographic differences between the intervention and control groups, such as gender or medication use. If there is any factor that is unbalanced between the two groups after randomisation, the factor would be put into the equation as a covariate.
Additionally, we will conduct subanalysis to evaluate whether MYmind has different effects on different subtypes of ADHD (inattentive, impulse/hyperactive or combined). The intention-to-treat principle and per-protocol analyses will be applied. Missing values of participants will be input using the expectation-maximisation algorithm. Pearson correlation coefficients will be calculated to assess the strength of association between class participation, duration of mindfulness practice and all outcomes. Mediation analysis will be conducted using the structural equation modelling to detect if mindfulness levels (CAMM score) is the mediating factors between the intervention and results of TEA-Ch, ANT, SWAN, BRIEF and ECBI for children or rumination (RRS score) is the mediating factor between the intervention and results of PSI, ASRS, RRS and WHO-5 for parents. Effect size estimates will be obtained comparing preintervention and postintervention means and SD for results of TEA-Ch, ANT, SWAN, BRIEF, ECBI, PSI, ASRS, RRS and WHO-5 between and within groups.
Sample size
Based on previous studies,33–35 39 the study with the biggest sample size so far (n=22) using MYmind mindfulness training for children with ADHD and their parents by van der Oord and colleagues33 showed an effect size of 0.80/0.59 in children’s inattention and hyperactivity/impulsivity, and our pilot study showed a large effect size of 1.35 in the attention score of the Sky Search subtest of TEA-Ch.40 60 For the active control group, we would design the programme mainly with reference to the suggestions according to the National Institute for Health and Care Excellence guidelines48 and the content would not cover any attention training. Therefore, we assume the effect size of the active control group on the primary outcome would be small. We conservatively expect a medium effect size between the intervention group and the active control group on the attention score of the Sky Search subtest of TEA-Ch. For a two-tailed α error of 5%, an 80% power and a test of two independent groups, the required sample size will be 64 families per arm. With a conservative estimate of 10% drop-out rate based on our pilot study, we aim to recruit 70 families per group and 140 families (140 children and 140 parents) in total.
Ethics and dissemination
Detailed description of the objectives and procedure of the study will be given to the participants. Confidentiality of any identifiable personal information will be assured. Participants will be given a consent form regarding the present study. They can withdraw the study at any time. All the related documents, assessment protocols and results, as well as questionnaires will be locked in a secure location or with a security code and will be destroyed in 5 years after completion of the study. Any adverse event could consist of any unfavourable and unintended symptoms or disease aroused in the study will be recorded and reported, whether considered related to this interventional study. Any serious adverse events will be immediately reported to the ethical committee. Participants will be advised to seek help from a doctor or psychologist if needed. Study outcomes will be published in peer-reviewed research journals and presented in conferences according to the CONSORT recommendations.
Discussion
ADHD often has significant negative impact on both children and parents. Children affected with ADHD show deficits in emotion regulation, inattention and behavioural inhibition and parents of children with ADHD suffer from high levels of parenting stress. In addition, parents of children with ADHD often exhibit ADHD symptoms as it is highly heritable. This, together with high parental stress, often results in poor parent and child relationships. Research shows that there is greater conflict in families with children diagnosed with ADHD when compared with that of other families. Given the reciprocal nature of children and parent behaviour, an intervention that works simultaneously for parents and children can be more effective and may be cost-effective for families affected with ADHD.
This proposed study will evaluate the effectiveness of a mindfulness-based intervention programme designed specifically for children with ADHD and their parents. It is a group intervention led by trained health professionals providing mindfulness training for children and parents concurrently. As there is a lack of intervention that simultaneously addresses both behavioural issues relevant to children with ADHD and chronic stress common in their parents, findings from this study will shed light on the benefits of mindfulness in improving attention and behaviour among children with ADHD and in reducing stress among their parents. In addition, Raes and Williams61 reported that mindfulness was significantly negatively correlated with uncontrollable rumination, and Mckim62 reported that rumination significantly mediated the effects of mindfulness on depression. In order to advance our understanding of how mindfulness works, ruminative response to depressed mood in parents will be examined as a potential mediator between mindfulness intervention and parents’ outcomes.
Some limitations are anticipated in this study. First, only children between 8 years and 12 years of age with normal intelligence are included in this study. The results may not be able to generalise to other age groups. Second, we will not include teachers’ ratings as some of the groups will be run during summer holiday in the end of the school year. Teachers are usually changed every school year in Hong Kong and so we would not be able to collect preintervention and postintervention data from the same teacher. Therefore, we will not be able to investigate changes in school setting among the children participated in this study. Other than these limitations, the main challenge that we face is recruitment of participants. Since MYmind programme includes parallel group for parents in addition to the children’s group, parental involvement is essential in this study. However, it may be a challenge for working parents to engage in an 8-week programme. We will offer most of the groups in early evenings and weekends so that working parents will also be able to participate.
Group-based mindfulness-based interventions with 6–12 families in each class can be more cost-effective than one-on-one psychological interventions, while mental health services and resources are scarce for ADHD in the communities in Hong Kong. Group-based interventions can also reduce isolation and creates common bonds by acknowledging the universality of the ADHD experiences among parents and children. Mindfulness-based interventions could be a potential alternative intervention with potential long-term benefits for children with ADHD and their parents, as participants can practice mindfulness life long after they learn the skills. Findings from this work will: (1) provide evidence-based information on an innovative intervention that targets both parents and children diagnosed with ADHD; (2) provide an alternative intervention for children diagnosed with ADHD who cannot tolerate the side effects of medication or whose parents prefer non-medication treatment for ADHD; and (3) provide children diagnosed with ADHD with a potential skill (mindfulness meditation) that can increase resilience for them at times of adversity later in life.
Supplementary Material
Footnotes
Contributors: SYSW, SKCC, DZ and TTG contributed to literature review, development of the original study protocol and drafting the initial manuscript. SMB, SKCC, CSC, HHML, ENSL, TTG and SYSW contributed to intervention design, training and implementation. SMB, CSC, KYCL, HHML and ENSL provided further research advice. BHKY contributed to the statistical analysis plan. All authors approved the final version of the manuscript.
Funding: The work is supported by General Research Fund (No. 14601017), University Grants Committee (UGC), Hong Kong. The authors sincerely thank UGC for the support to this research study.
Disclaimer: The funding body has no role in study design, collection, management, analysis, interpretation of data, writing of the report and the decision to submit the report for publication.
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: This study has been approved by the Joint Chinese University of Hong Kong ‐ New Territories East Cluster Clinical Research Ethics Committee (CREC).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Rhl M, Ccc L, Ccy H, et al. . A primer in common developmental disabilities: experience at child assessment service, Hong Kong. Hong Kong: Child Assessment Service, 2006. [Google Scholar]
- 2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). 5th edn Washington DC: American Psychiatric Assoication, 2013. [Google Scholar]
- 3. Leung PWL, Hung S-fong, Ho T-pong, et al. . Prevalence of DSM-IV disorders in Chinese adolescents and the effects of an impairment criterion. Eur Child Adolesc Psychiatry 2008;17:452–61. 10.1007/s00787-008-0687-7 [DOI] [PubMed] [Google Scholar]
- 4. Leung PW, Luk SL, Ho TP, et al. . The diagnosis and prevalence of hyperactivity in Chinese schoolboys. Br J Psychiatry 1996;168:486–96. 10.1192/bjp.168.4.486 [DOI] [PubMed] [Google Scholar]
- 5. Katusic SK, Barbaresi WJ, Colligan RC, et al. . Psychostimulant treatment and risk for substance abuse among young adults with a history of attention-deficit/hyperactivity disorder: a population-based, birth cohort study. J Child Adolesc Psychopharmacol 2005;15:764–76. 10.1089/cap.2005.15.764 [DOI] [PubMed] [Google Scholar]
- 6. Centers for Disease Control and Prevention. Attention Deficit / Hyperactivity Disorder (ADHD). Atlanta: Centers for Disease Control and Prevention, 2016. [Google Scholar]
- 7. Pelham WE, Foster EM, Robb JA. The economic impact of attention-deficit/hyperactivity disorder in children and adolescents. J Pediatr Psychol 2007;32:711–27. 10.1093/jpepsy/jsm022 [DOI] [PubMed] [Google Scholar]
- 8. Rubia K, Overmeyer S, Taylor E, et al. . Hypofrontality in attention deficit hyperactivity disorder during higher-order motor control: a study with functional MRI. Am J Psychiatry 1999;156:891–6. 10.1176/ajp.156.6.891 [DOI] [PubMed] [Google Scholar]
- 9. Teicher MH, Anderson CM, Polcari A, et al. . Functional deficits in basal ganglia of children with attention-deficit/hyperactivity disorder shown with functional magnetic resonance imaging relaxometry. Nat Med 2000;6:470–3. 10.1038/74737 [DOI] [PubMed] [Google Scholar]
- 10. Bymaster FP, Katner JS, Nelson DL, et al. . Atomoxetine increases extracellular levels of norepinephrine and dopamine in prefrontal cortex of rat: a potential mechanism for efficacy in attention deficit/hyperactivity disorder. Neuropsychopharmacology 2002;27:699–711. 10.1016/S0893-133X(02)00346-9 [DOI] [PubMed] [Google Scholar]
- 11. Kirley A, Hawi Z, Daly G, et al. . Dopaminergic system genes in ADHD: toward a biological hypothesis. Neuropsychopharmacology 2002;27:607–19. 10.1016/S0893-133X(02)00315-9 [DOI] [PubMed] [Google Scholar]
- 12. Faraone SV, Buitelaar J. Comparing the efficacy of stimulants for ADHD in children and adolescents using meta-analysis. Eur Child Adolesc Psychiatry 2010;19:353–64. 10.1007/s00787-009-0054-3 [DOI] [PubMed] [Google Scholar]
- 13. Man KKC, Ip P, Hsia Y, et al. . ADHD drug prescribing trend is increasing among children and adolescents in Hong Kong. J Atten Disord 2017;21 10.1177/1087054714536047 [DOI] [PubMed] [Google Scholar]
- 14. Chacko A, Newcorn JH, Feirsen N, et al. . Improving medication adherence in chronic pediatric health conditions: a focus on ADHD in youth. Curr Pharm Des 2010;16:2416–23. 10.2174/138161210791959908 [DOI] [PubMed] [Google Scholar]
- 15. Jensen CM, Amdisen BL, Jørgensen KJ, et al. . Cognitive behavioural therapy for ADHD in adults: systematic review and meta-analyses. Atten Defic Hyperact Disord 2016;8:3–11. 10.1007/s12402-016-0188-3 [DOI] [PubMed] [Google Scholar]
- 16. Miller-Lewis LR, Baghurst PA, Sawyer MG, et al. . Early childhood externalising behaviour problems: child, parenting, and family-related predictors over time. J Abnorm Child Psychol 2006;34:886–901. 10.1007/s10802-006-9071-6 [DOI] [PubMed] [Google Scholar]
- 17. Deault LC. A systematic review of parenting in relation to the development of comorbidities and functional impairments in children with attention-deficit/hyperactivity disorder (ADHD). Child Psychiatry Hum Dev 2010;41:168–92. 10.1007/s10578-009-0159-4 [DOI] [PubMed] [Google Scholar]
- 18. Coelho LF, Barbosa DL, Rizzutti S, et al. . Use of cognitive behavioral therapy and token economy to alleviate dysfunctional behavior in children with attention-deficit hyperactivity disorder. Front Psychiatry 2015;6:167 10.3389/fpsyt.2015.00167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bériault M, Turgeon L, Labrosse M, et al. . Comorbidity of ADHD and anxiety disorders in school-age children: impact on sleep and response to a cognitive-behavioral treatment. J Atten Disord 2018;22:414–24. 10.1177/1087054715605914 [DOI] [PubMed] [Google Scholar]
- 20. Bloomquist ML, August GJ, Ostrander R. Effects of a school-based cognitive-behavioral intervention for ADHD children. J Abnorm Child Psychol 1991;19:591–605. 10.1007/BF00925822 [DOI] [PubMed] [Google Scholar]
- 21. Daley D, van der Oord S, Ferrin M, et al. . European ADHD Guidelines Group. Behavioral interventions in attention-deficit/hyperactivity disorder: a meta-analysis of randomized controlled trials across multiple outcome domains. J Am Acad Child Adolesc Psychiatry 2014;53:835–47. 10.1016/j.jaac.2014.05.013 [DOI] [PubMed] [Google Scholar]
- 22. Martel MM, Nikolas M, Jernigan K, et al. . The dopamine receptor D4 gene (DRD4) moderates family environmental effects on ADHD. J Abnorm Child Psychol 2011;39:1–10. 10.1007/s10802-010-9439-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kabat-Zinn J. Mindfulness-based interventions in context: past, present, and future. Clinical Psychology: Science and Practice 2003;10:144–56. 10.1093/clipsy.bpg016 [DOI] [Google Scholar]
- 24. Keng SL, Smoski MJ, Robins CJ. Effects of mindfulness on psychological health: a review of empirical studies. Clin Psychol Rev 2011;31:1041–56. 10.1016/j.cpr.2011.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Teasdale JD, Segal Z, Williams JM. How does cognitive therapy prevent depressive relapse and why should attentional control (mindfulness) training help? Behav Res Ther 1995;33:25–39. 10.1016/0005-7967(94)E0011-7 [DOI] [PubMed] [Google Scholar]
- 26. Heeren A, Philippot P. Changes in ruminative thinking mediate the clinical benefits of mindfulness: preliminary findings. Mindfulness 2011;2:8–13. 10.1007/s12671-010-0037-y [DOI] [Google Scholar]
- 27. Hölzel BK, Lazar SW, Gard T, et al. . How does mindfulness meditation work? proposing mechanisms of action from a conceptual and neural perspective. Perspect Psychol Sci 2011;6:537–59. 10.1177/1745691611419671 [DOI] [PubMed] [Google Scholar]
- 28. Lazar SW, Kerr CE, Wasserman RH, et al. . Meditation experience is associated with increased cortical thickness. Neuroreport 2005;16:1893–7. 10.1097/01.wnr.0000186598.66243.19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bögels S, Hoogstad B, van Dun L, et al. . Mindfulness training for adolescents with externalizing disorders and their parents. Behav Cogn Psychother 2008;36:193–209. 10.1017/S1352465808004190 [DOI] [Google Scholar]
- 30. Bögels SM, Lehtonen A, Restifo K. Mindful parenting in mental health care. Mindfulness 2010;1:107–20. 10.1007/s12671-010-0014-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Neece CL, Green SA, Baker BL. Parenting stress and child behavior problems: a transactional relationship across time. Am J Intellect Dev Disabil 2012;117:48–66. 10.1352/1944-7558-117.1.48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hastings RP. Parental stress and behaviour problems of children with developmental disability. J Intellect Dev Disabil 2002;27:149–60. 10.1080/1366825021000008657 [DOI] [Google Scholar]
- 33. van der Oord S, Bögels SM, Peijnenburg D. The effectiveness of mindfulness training for children with ADHD and mindful parenting for their parents. J Child Fam Stud 2012;21:139–47. 10.1007/s10826-011-9457-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. van de Weijer-Bergsma E, Formsma AR, de Bruin EI, et al. . The effectiveness of mindfulness training on behavioral problems and attentional functioning in adolescents with ADHD. J Child Fam Stud 2012;21:775–87. 10.1007/s10826-011-9531-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Haydicky J, Shecter C, Wiener J, et al. . Evaluation of MBCT for adolescents with ADHD and their parents: impact on individual and family functioning. J Child Fam Stud 2015;24:76–94. 10.1007/s10826-013-9815-1 [DOI] [Google Scholar]
- 36. Harrison LJ, Manocha R, Rubia K. Sahaja yoga meditation as a family treatment programme for children with attention deficit-hyperactivity disorder. Clin Child Psychol Psychiatry 2004;9:479–97. 10.1177/1359104504046155 [DOI] [Google Scholar]
- 37. Singh NN, Singh AN, Lancioni GE, et al. . Mindfulness training for parents and their children with ADHD increases the children’s compliance. J Child Fam Stud 2010;19:157–66. 10.1007/s10826-009-9272-z [DOI] [Google Scholar]
- 38. Nikander D. Attention deficit hyperactivity disorder and mindfulness practice in children and adolescents: a comprehensive review of evidence-based research. 2015. https://scholarworks.sjsu.edu/etd_doctoral/15.
- 39. Cairncross M, Miller CJ. The effectiveness of mindfulness-based therapies for ADHD: a meta-analytic review. J Atten Disord 2016;10:1087054715625301 10.1177/1087054715625301 [DOI] [PubMed] [Google Scholar]
- 40. Zhang D, Chan SKC, Lo HHM, et al. . Mindfulness-based intervention for Chinese children with ADHD and their parents: a pilot mixed-method study. Mindfulness 2017;8:859–72. 10.1007/s12671-016-0660-3 [DOI] [Google Scholar]
- 41. Julian TW, McKenry PC, McKelvey MW. Cultural variations in parenting: perceptions of Caucasian, African-American, Hispanic, and Asian-American Parents. Fam Relat 1994;43:30–7. 10.2307/585139 [DOI] [Google Scholar]
- 42. Lee MT, Wong BP, Chow BW, et al. . Predictors of suicide ideation and depression in Hong Kong adolescents: perceptions of academic and family climates. Suicide Life Threat Behav 2006;36:82–96. 10.1521/suli.2006.36.1.82 [DOI] [PubMed] [Google Scholar]
- 43. Lai KY, Leung PW, Luk ES, et al. . Validation of the Chinese strengths and weaknesses of ADHD-symptoms and normal-behaviors questionnaire in Hong Kong. J Atten Disord 2013;17:194–202. 10.1177/1087054711430711 [DOI] [PubMed] [Google Scholar]
- 44. Segal ZV. Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. New York, USA: Guilford Press, 2002. [Google Scholar]
- 45. Kabat-Zinn J. Full catastrophe living: using the wisdom of your body and mind to face stress, pain, and illness. 15th anniversary ed New York, NY: Bantam Dell, 2005. [Google Scholar]
- 46. Young S. Cognitive-behavioural therapy for ADHD in adolescents and adults electronic resource]: a psychological guide to practice, 2012. [Google Scholar]
- 47. Kendall PC, Braswell L. Cognitive-behavioral therapy for impulsive children: therapist Manual. 3rd edn Pennsylvania: Workbook Publishing, 2007. [Google Scholar]
- 48. National Collaborating Centre for Mental Health (UK). Attention deficit hyperactivity disorder: diagnosis and management of adhd in children, young people and adults: National Collaborating Centre for Mental Health (UK), 2009. [PubMed] [Google Scholar]
- 49. Hong Kong Kwai Chung Hospital / Yau Ma Tei Child and Adolescent Psychiatric Day Center HA. Attention deficit hyperactivity disorder treatment and training. 2016. Available at http://www21haorghk/files/PDF/self%20tools_printed%20matter/ADHDpdf.
- 50. Manly T, Robertson IH, Anderson V, et al. . The Test of Everyday Attention (TEA-CH). Bury St. Edmunds, England: Thames Valley Test Company, 1999. [Google Scholar]
- 51. Chan RC, Wang L, Ye J, et al. . A psychometric study of the Test of Everyday Attention for Children in the Chinese setting. Arch Clin Neuropsychol 2008;23:455–66. 10.1016/j.acn.2008.03.007 [DOI] [PubMed] [Google Scholar]
- 52. Posner MI, Petersen SE. The attention system of the human brain. Annu Rev Neurosci 1990;13:25–42. 10.1146/annurev.ne.13.030190.000325 [DOI] [PubMed] [Google Scholar]
- 53. Leung C, Chan S, Pang R, et al. . Validation of the Chinese version of the Eyberg Child Behaviour Inventory for use in Hong Kong. Wanchai, Hong Kong: Education and Manpower Bureau, 2003. [Google Scholar]
- 54. Qian Y, Shuai L, Cao Q, et al. . Do executive function deficits differentiate between children with attention deficit hyperactivity disorder (ADHD) and ADHD comorbid with oppositional defiant disorder? A cross-cultural study using performance-based tests and the behavior rating inventory of executive function. Clin Neuropsychol 2010;24:793–810. 10.1080/13854041003749342 [DOI] [PubMed] [Google Scholar]
- 55. Greco LA, Baer RA, Smith GT. Assessing mindfulness in children and adolescents: development and validation of the Child and Adolescent Mindfulness Measure (CAMM). Psychol Assess 2011;23:606–14. 10.1037/a0022819 [DOI] [PubMed] [Google Scholar]
- 56. Tam K-K, Chan Y-C, Wong C-KM. Validation of the parenting stress index among Chinese mothers in Hong Kong. J Community Psychol 1994;22:211–23. [DOI] [Google Scholar]
- 57. Yeh CB, Gau SS, Kessler RC, et al. . Psychometric properties of the Chinese version of the adult ADHD Self-report Scale. Int J Methods Psychiatr Res 2008;17:45–54. 10.1002/mpr.241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Volinn E, Yang B, He J, et al. . West China hospital set of measures in Chinese to evaluate back pain treatment. Pain Med 2010;11:637–47. 10.1111/j.1526-4637.2010.00846.x [DOI] [PubMed] [Google Scholar]
- 59. Yang J, Ling Y, Xiao J, et al. . The Chinese Version of Ruminative Responses Scale in High School Students: Its Reliability and Validity. Chinese Journal of Clinical Psychology 2009;17:27–8. [Google Scholar]
- 60. Zhang D, Chan SKC, Lo HHM, et al. . Mindfulness-based intervention for Chinese Children with ADHD and their parents: a pilot mixed-method study. Mindfulness 2017;8:859–72. 10.1007/s12671-016-0660-3 [DOI] [Google Scholar]
- 61. Raes F, Williams JMG. The relationship between mindfulness and uncontrollability of ruminative thinking. Mindfulness 2010;1:199–203. 10.1007/s12671-010-0021-6 [DOI] [Google Scholar]
- 62. Mckim RD. Rumination as a mediator of the effects of mindfulness: Mindfulness-based stress reduction (MBSR) with a heterogeneous community sample experiencing anxiety, depression, and/or chronic pain. Dissertation Abstracts International: Section B: The Sciences and Engineering 2008;11(11-B):7673. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-022514supp001.pdf (117.2KB, pdf)