Abstract
Objective
To explore the acceptability of peer mentoring for people with a traumatic brain injury (TBI) in New Zealand.
Design
This is a qualitative descriptive study exploring the experiences reported by mentees and mentors taking part in a feasibility study of peer mentoring. Interviews with five mentees and six mentors were carried out. Data were analysed using conventional content analysis.
Setting
The first mentoring session took place predischarge from the rehabilitation unit. The remaining five sessions took place in mentees’ homes or community as preferred.
Participants
Twelve people with TBI took part: six mentees (with moderate to severe TBI; aged 18–46) paired with six mentors (moderate to severe TBI >12 months previously; aged 21–59). Pairing occurred before mentee discharge from postacute inpatient brain injury rehabilitation. Mentors had been discharged from rehabilitation following a TBI between 1 and 5 years previously.
Intervention
The peer mentoring programme consisted of up to six face-to-face sessions between a mentee and a mentor over a 6-month period. The sessions focused on building rapport, exploring hopes for and supporting participation after discharge through further meetings and supported community activities.
Results
Data were synthesised into one overarching theme: making sense of recovery. This occurred through the sharing of experiences and stories; was pivotal to the mentoring relationship; and appeared to benefit both mentees and mentors. Mentors were perceived as valued experts because of their personal experience of injury and recovery, and could provide support in ways that were different from that provided by clinicians or family members. Mentors required support to manage the uncertainties inherent in the role.
Conclusions
The insight mentors developed through their own lived experience established them as a trusted and credible source of hope and support for people re-engaging in the community post-TBI. These findings indicate the potential for mentoring to result in positive outcomes.
Keywords: traumatic brain injury, peer mentoring, feasibility, neurology, qualitative research, rehabilitation medicine
Strengths and limitations of this study.
The use of qualitative interviews with both mentees and mentors engaged in a mentoring programme after traumatic brain injury (TBI) in order to understand their experiences is a strength.
The study design was informed by our previous work trialling rehabilitation interventions with this population and incorporated robust methods to collect and analyse qualitative data.
The intervention, developed using theory, evidence and consumer involvement, was delivered face to face and was flexible to the needs of both mentors and mentees.
This was mentors’ first experience of mentoring following TBI; therefore, the benefits and challenges presented here may change in a larger trial where mentors have the opportunity to support more than one mentee.
This study was designed to explore acceptability of peer mentoring; the efficacy of this intervention requires further investigation.
Introduction
An estimated 10 million people sustain a traumatic brain injury (TBI) each year worldwide.1 New Zealand has a very high incidence of this condition (811/100 000; these figures include people with mild to severe TBI).2 While some people with TBI make functional gains over time,3 many people deteriorate with time and often experience wide-ranging and significant long-term problems with physical, cognitive and psychological functioning. Indeed, the personal aftermath of TBI is characterised by disruption to a sense of self and personhood, with usual markers of productivity and reciprocity in roles and relationships threatened.4 As a consequence, many people report an enduring impact on social, community and vocational participation, with many suffering social isolation.3–13
Major long-term costs to society extend beyond acute healthcare to include compensation, support for independence, and social and physical rehabilitation.14 15 These findings suggest that more effective strategies that facilitate enhanced participation for this population in the long term are needed. However, current services, in New Zealand and elsewhere, primarily target the acute/subacute phase with only limited ongoing input.16 In addition, rehabilitation services largely focus on reducing impairment and improving activity (or reducing disability) with the assumption that this will lead to improvements in participation.17 18 However, findings from a longitudinal qualitative study exploring experiences of recovery over 2 years highlight the importance of developing a concept of TBI and what it means to live in the context of TBI, which are unique to the individual and which are socially and culturally located, for successful re-engagement in meaningful activities.19 20 Individuals and their families in this study highlighted that existing services (both in terms of their aim and purpose and the timing of those services) failed to provide them with the necessary support to manage these processes, leaving them to navigate and make sense of their recovery in isolation. These findings are consistent with arguments calling for new approaches to supporting recovery and adaptation after TBI, given recognition that it is more appropriately conceptualised as a ‘long term condition than a single episode injury’.21
Peer mentoring has been defined as ‘support provided by individuals who have successfully faced a particular experience and can provide good counsel and empathic understanding to help others, with similar salient population characteristics, through a comparable experience’ (p436).22 23 24 It has been used for over 50 years in mental health25 and is increasingly used in rehabilitation, for example with people with spinal cord injury22 23 26–28 and heart disease.24 29 Empirical work in these populations has reported positive outcomes. For example, peer mentoring led to better adjustment after spinal cord injury in a study in which mentors helped mentees to cope with practical, emotional and identity challenges and project future possibilities.23 26 Likewise, a review of peer mentoring in heart disease showed that it led to increased self-efficacy, improved activity, reduced pain and fewer emergency room visits.29
The case for peer mentoring can be found in a number of psychological theories, such as social cognitive theory30 and self-determination theory.31 These theories propose that observing others, feedback and modelling, and social exchanges that support autonomy lead to better outcomes for those receiving the mentoring, and were therefore selected as key to our programme. Peer mentoring interventions generally include some degree of informational, appraisal and emotional support.24
As noted above, many individuals with moderate to severe TBI experience significant ongoing consequences in domains of physical, cognitive and psychological functioning, and personality changes.3–10 19 32–34 This variety of consequence makes peer mentoring potentially challenging as candidate mentors may also be experiencing long-term consequences of their TBI. Consequently, it is not surprising to find a limited range of published research exploring peer mentoring in TBI.32–38 These studies report positive benefits on knowledge, quality of life general outlook, behavioural control and return to work. However, design limitations and trial issues hamper generalisability and adaptability of these findings.32–37 For example, limitations include a lack of formal outcomes,36 minimal detail provided limiting replication,37 lack of a control group,34 35 difficulties matching mentors with mentees,33 34 costs of transport and social outings to participants,33 and fewer sessions or contacts than planned.32 33 As a consequence, a more robust evaluation of peer mentoring with people with TBI is needed before tangible changes to practice and policy can be instigated. However, before proceeding to a full trial for such a complex intervention, it is important to establish if the proposed intervention is acceptable and if the study design is feasible.39
Our overarching study aim was to explore peer mentor and mentee views of the feasibility (eg, practicalities) and acceptability of a peer mentoring intervention in the New Zealand context. This paper describes our approach and reports on the qualitative data collected to evaluate the acceptability of the intervention with feasibility to be examined in a separate publication.
Methods
A qualitative descriptive methodology40 was employed to explore mentee and mentor perspectives and experiences of their participation in the peer mentoring intervention.41 In qualitative descriptive studies researchers stay close to their data and to the surface of words and events.40 This enables the explication and descriptive summary of complex experiences, which are valuable in their own right as end products, but also to inform further study. As a consequence, qualitative descriptive methodology has been argued to be a useful approach for the development and refinement of interventions41 and so was well suited for the current study. The academic members of the research team consisted of people with a range of expertise in rehabilitation, physiotherapy, psychology, psychiatry, medicine, statistics, project management, data analysis and some personal experience of TBI or as a carer.
The study was conducted in Auckland, New Zealand/Aotearoa. Due to the contracting of a single national funder of inpatient rehabilitation after TBI in New Zealand, nearly all moderate to severe cases of TBI in the North Island are treated by a single provider after their discharge from the acute hospital services. This provider cares for between 100 and 150 people per year,42 and their primary Auckland site was the sole site of recruitment for mentees.
We had funding to support inclusion of six mentees and six mentors. Invitations to take on the role of mentor were sent by letter in batches to those identified as eligible by the rehabilitation provider and followed up by phone to confirm eligibility. While the staff involved in the clinical management of mentors were involved in helping to identify potentially eligible people, the actual recruitment of mentors was overseen and carried out by the research team. In addition to those identified by the rehabilitation provider, letters were also sent out from our research centre to those who had previously taken part in other studies, had expressed an interest in being involved in further research and fitted the study criteria. Those who met the eligibility criteria and expressed a desire to take up a mentoring role were invited to attend a ‘job’ interview as this was a paid role. The interview panel consisted of members of the research team (which included a psychiatrist with expertise in TBI). The panel explored candidates’ motivation for applying to become a mentor, any challenges they may foresee, how they might overcome these challenges and what their support needs might be. All those offered the mentorship role underwent a criminal record check. The mentors were paid on a research assistant pay scale for their time on the project, and they were issued with a mobile phone to enable contact with their mentees and the research team at no cost to themselves and without the need to share their personal number.
Mentee recruitment was initiated by the rehabilitation staff approaching all eligible participants and handing them the study information leaflet. In this leaflet they were encouraged to discuss the study with their family. Rehabilitation staff passed contact details of those interested in hearing more about the study to the research officer (CC). The research officer then met with potential participants (and interested family member(s) if this was their wish), explained what the study involved and discussed any concerns. This meeting took place at least 24 hours after the person had first been informed about the study, and in many cases the researcher followed up with a second visit to answer further questions and meet with interested family members. This process was used to ensure all potential mentee participants were able to take the time to consider their participation and discuss it with their family members, before providing consent. The eligibility criteria for both the mentors and the mentees are displayed in table 1. The literature has shown that matching is important in peer mentoring.32–34 We were able to match by gender, and where possible shared interest (such as outdoor sports).
Table 1.
Inclusion and exclusion criteria
| Mentees | Mentors | |
| Inclusion criteria | ||
| Age (years) | ≥15 | ≥18 |
| Moderate or severe traumatic brain injury65 66 | √ | √ |
| Discharge from inpatient rehabilitation | Imminent | 1–5 years previously |
| Living in the greater Auckland region | √ | √ |
| Exclusion criteria | ||
| Unable to communicate in a way that enabled engagement with a mentor/mentee | √ | √ |
| Medical condition that precluded their participation | √ | √ |
| Discharge FIM cognitive domain score* ≥2467 | – | √ |
| Ongoing alcohol or drug abuse problems, communication difficulties, known gang affiliations, concerns in terms of safety or security (clinical judgement) | – | √ |
*FIM, Functional Independence Measure; data obtained from the rehabilitation centre. FIM discharge data were only used as an exclusion criterion for mentors.
Intervention
Our approach was informed by our own research19 20 43–45 and by that of others.32–34 For example, peer mentoring sessions were one to one and face to face (as opposed to by phone). The research officer introduced the mentor to the mentee (and their family members) prior to the first meeting. The first session occurred predischarge in the rehabilitation setting and the remaining five in the community. Mentors were provided with worksheets to support them with each mentoring session. These worksheets helped them to remember the focus of each session. It was also intended the sessions would be time-limited and would take place in the initial stages following discharge, that is, over a 3-month period. Dyads started the intervention within 2 weeks of the mentee agreeing to take part and prior to discharge. Three of the sessions were intended to involve a preplanned, supported participatory activity in the community, negotiated in advance by each mentee–mentor pair (to ensure dyads could focus on real-life experiences of participation and its challenges). Mentors were provided with petty cash to pay for any expenses during such activities (up to NZ$50 per activity).32–34 43–45 Table 2 displays the basic structure of the programme in more detail.
Table 2.
The mentoring programme
| Time point | Session purpose |
| 1–2 weeks before discharge from inpatient rehabilitation | Mentor meets with the mentee at the inpatient rehabilitation facility to get to know one another. Make provisional plans for meeting postdischarge. |
| 2 weeks after discharge | Mentor visits mentee at home, to re-establish connection, explore barriers and facilitators to participation, and support them to develop plan for social activities for the next couple of weeks. |
| 4 weeks after discharge | Participate in mentor-supported activity; check in with the mentee and discuss what has gone well over the last few weeks, what did not go well? Plan further activities. |
| 6 weeks after discharge | As for previous session. |
| 8 weeks after discharge | As for previous session, reminder that next visit will be the last. |
| 10 weeks after discharge | Final visit. The mentor and the mentee will review progress and the ending of mentee–mentor relationship. A mihi whakamutunga (cultural blessing or prayer) will be offered for those who wish this. |
Mentor training and support
Mentor training comprised a 2-day interactive training workshop, with each day held 1 week apart (see the online supplementary appendix for an overview of the training programme). This included a mix of presentations, discussion, role-play and skill-building activities, aiming to strengthen and build on the experience and skills of the mentors. Topic sessions included the role of the mentor, experience of TBI, sharing experiences and safety protocols. Skills in sharing experiences were developed by each mentor creating a pictorial map of their TBI journey, on their own then sharing this with the wider group. This helped the mentors to articulate their journey, decide what aspects they were willing to share and which ones they may not, and also gain insight into each other’s journeys. This in turn helped them develop listening skills and empathy.
bmjopen-2017-020672supp001.pdf (230KB, pdf)
We discussed ways of being respectful and keeping safe when visiting people in their homes. We established a safety protocol where mentors were required to notify the research officer of the time and date of their visits and check in (by phone) at the completion. Mentors were encouraged to share with the research team any concerns they had regarding the visit and any perceived threats to their own safety or the welfare of their mentee. We also took care not to professionalise the mentoring role as a key component was that mentors functioned as ‘peers’ not quasi-health professionals. To that end we provided limited education about the clinical consequences of TBI to mentors, instead giving primacy to their own personal experiences of TBI. The 45 min education session, led by a rehabilitation consultant (who was familiar to many of the mentors having been involved in their clinical management during their own inpatient stay), used material that all mentors had previously received as an inpatient during their rehabilitation.
Attention was paid to cultural protocols for the New Zealand context: for example, the encouragement to use an opening and closing karakia (blessing or prayer) for meetings with mentees when both parties agreed this was appropriate; and the intervention being delivered kanohi te kanohi (face to face), which is a preferred approach for Māori.46 Mentors had access to a resource containing information on locally available services they could refer mentees to if appropriate.
Mentors took part in three face-to-face group debrief sessions over the course of the intervention period, led by the principal investigator (PK) and accompanied by the research officer (CC) and one other member of the research team with psychology expertise (eg, KMcP, DB, RJS, each attending one session). These were held on Saturday mornings to accommodate those who were working or studying. Topics for the debriefs were set by the mentors and included, for example, sharing experiences of the first meeting with mentees (what went well, what were their concerns), practicalities of community activities and how to conclude the mentoring relationship. Access to additional psychological and psychiatric support was available for individual mentors but not requested.
Data collection and analysis
Semistructured interviews with mentees and mentors were conducted at the conclusion of the mentoring relationship, at the mentee and mentor homes, by one researcher (CC). She has over 10 years of experience of qualitative data collection and analysis, studying rehabilitation interventions in people with neurological conditions, in particular TBI (eg, refs 45 47). An interview guide (see box 1) was used. This focused on the mentoring experience, the timing of the intervention, the perceived impact of the relationship and suggestions for improving the programme. Mentors were asked additional questions relating to the adequacy of the training and support provided to them. In both cases, the interview guide was used as a prompt to focus the conversation, but otherwise the interview was kept open, exploring topics raised by the participants in more detail as they arose. Interviews were audio-recorded and transcribed verbatim by a contracted transcriber, then checked for accuracy by the researcher. They were anonymised prior to analysis.
Box 1. Interview guide (used flexibly).
Mentees
What was your experience of the mentoring project?
What was useful about the mentoring? What was not?
How has the relationship impacted on you?
If you had a mentor in the future what would you like them to focus on?
What sort of things would you like to talk to/do with your mentor?
When would have been the best time to meet up with your mentor? Prompts: the first meeting, after the first meeting, how often?
How did you find answering the questionnaires that CC asked you to complete?
Additional questions for mentors
Did you feel that the training workshops prepared you for your role as mentor?
What would you change about those workshops?
If we needed to cut these down to one day what would you suggest we cut out?
Or what should we add instead?
Did you feel that you received enough support for your role as mentor?
What would you change about the support you received?
How did you find the planning and write-up requirements? How would you suggest that we do this in the future?
The mentors were given a format for keeping visit notes, asking them to record the activities they carried out and reflect on what had gone well or not and what they would do differently next time. Mentors maintained in contact with their mentee by texts and phone, but these were not recorded as data. The researcher noted when needing to provide mentors with practical support (such as connecting with their mentees). She collated the mentor notes, which supplemented interview data. Peer mentoring sessions were not observed as the team did not wish to interfere with the relational aspects of the intervention.
Data were analysed drawing on conventional content analysis.48 A core analysis group (PK, CC, NK and DB) was established, which was diverse in gender, ethnicity (New Zealand European, European and Australian) and professional background (rehabilitation, physiotherapy, health psychology, sociology and education). This group met several times to allow for an iterative and recursive approach to analysis before settling on the final interpretation of data presented here. In the first instance, CC and PK listened to the audio recordings and read and reread the transcripts to become familiar with the data. From there, data were read to identify key concepts relevant to the topic areas in the interview guide (eg, broad experiences and perspectives of the intervention, the mentoring relationship, and feedback on specific aspects of the programme). This led to the development of a coding framework which formed the initial frame for analysis. Data were coded manually, deriving new codes where an existing code did not fit the existing framework. Code definitions developed, and then illustrative quotes were extracted into word tables. Each core analysis group member became familiar with a set of interviews in preparation for group analysis discussions where preliminary ideas and concepts derived from early coding were presented and discussed. Following each analysis session, CC returned to the raw data to test out our interpretation of data, further refine our coding and categorise the data into meaningful themes. The analysis was deepened through exploration of mentor notes and the researcher’s notes of her conversations with mentors following their interactions with mentees. Interview data from mentors and mentees were initially coded separately before looking across data sets (ie, within dyads and across participant types) for patterns and meaningful clusters.
Patient and public involvement
Māori are the indigenous people of Aotearoa/New Zealand and almost 17.5% of the New Zealand population identify as Māori.49 Researchers have a responsibility to ensure their research is of value and culturally responsive to Māori.50 Therefore, guidance for the study was also sought from a University Mātauranga Māori committee, members of which are drawn from a wide range of Māori communities. While people with recent TBI were not explicitly involved in the design of the study, seeking mentor and mentee experiences and perspectives was built into the design of the study to ensure their voice was formative to future related work. Further, mentors were appointed to paid positions, and ongoing engagement with them through their training, debriefing and supervision sessions (see below for more detail) played a critical role in the operationalisation of peer mentoring in the current study.
Results
Letters were sent to 34 potential mentors, of whom 9 were not contactable. The researcher discussed the study with 13 people who responded positively to the initial approach, with 9 accepting the invitation for interview (36% of those contactable). The main reason for not taking part as a mentor were other commitments. All those interviewed were invited to attend mentor training. Eight mentors completed both training days, with one dropping out after the first day due to work circumstances (89% retention).
There were 12 potentially eligible mentee participants during the study period. Of these, nine agreed to talk further with the research officer, with six consenting to participate as mentees. Six of the mentors who had attended the mentor training were successfully paired with the six consenting mentees.
Demographic and disability data for mentors and mentees are provided in table 3. On enrolment to the study all mentors were able to walk independently and without a walking aid, although many had ongoing physical and cognitive difficulties.
Table 3.
Demographics
| Mentees (n=6) | Mentors (n=6) | |
| Inpatient stay (days), mean (SD) | 72 (54.4) | NA |
| Admission FIM* score, mean (SD) | ||
| Motor tasks | 57.7 (26.2) | NA |
| Cognitive tasks | 22.0 (5.7) | |
| Age (range) (years) | 18–46 | 21–59 |
| Frequencies | Frequencies | |
| Gender | ||
| Male | 4 | 4 |
| Female | 2 | 2 |
| Injury severity† | ||
| Severe | 5 | 4 |
| Moderate | 1 | 2 |
| Ethnicity | ||
| Māori | 1 | 1 |
| Māori/Samoan | 1 | |
| New Zealand European | 4 | 5 |
| Employment | Preinjury | |
| Studying | 1 | 2 |
| Working full time | 3 | 2 |
| Working part-time | 2 | 2 |
*FIM, Functional Independence Measure; higher scores denote greater dependency; total motor scores can range from 13 and 91, and total cognition scores from 5 to 35.
†Moderate TBI: initial GCS scores 9–12 (of a possible 15) and/or PTA duration >1 but <7 days; severe TBI: initial GCS score <9 and/or PTA ≥7 days.65 66
GCS, Glasgow Coma Scale; NA, not applicable; PTA, post-traumatic amnesia; TBI, traumatic brain injury.
Four mentees engaged in six peer mentoring sessions, with the remaining two engaging in one only. One mentee failed to meet again with the mentor after the initial mentoring session despite a number of attempts to arrange a face-to-face meeting, and eventually lost contact with their mentor and the research team. The other mentee was not available to take part in more than one mentoring session due to personal difficulties that restricted her participation and which had not been apparent during recruitment, but contributed to the postintervention interview data collection. Five mentees and six mentors were interviewed at the end of the intervention period, with an average duration of 45 min (range 15–60).
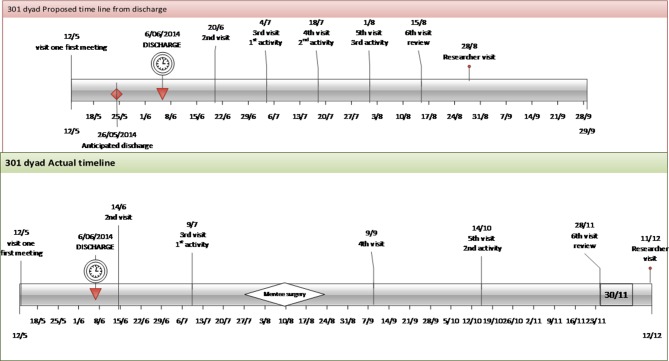
There were some deviations from the intended programme structure. For example, most dyads took more than 3 months to start and finish the programme (up to 6 months; see example in figure 1). This was mostly due to ongoing health issues the mentee was experiencing (eg, further surgery) or due to other commitments both for mentees and mentors (eg, work, study). Second, the intended community activities were not always possible, and as such for some dyads more mentor visits were at the mentees’ homes than intended.
Figure 1.
Example of mentoring timing. The top image in this figure shows the intended duration of the peer mentoring programme (3 months) and frequency of sessions (every 2 weeks) for one of the study dyads. The bottom image shows the actual duration (6 months) and frequency (gap of 4–8 weeks between sessions). The longest gap was due to the mentee requiring surgery.
The research officer called mentors following each mentoring session as per the agreed safety protocol to ‘check in’ and enquire what had gone well, if there were any issues or concerns, provide general reassurance and to remind mentors to maintain records of the sessions. Written reflections were provided by four mentors, and although these were generally brief one mentor provided comprehensive written reflections for each session.
Data from mentor notes showed that mentors and mentees undertook a range of community activities, such as having their nails done, going for lunch, having coffee in a café, browsing for music or going for a walk. Topics of conversations during the session were wide-ranging, including going back to work, struggles with abstaining from alcohol and drugs, feeling different, strategies for remembering to do things and managing relationships.
The next section explores the qualitative findings from the interviews. Pseudonyms are used here, followed by the age of mentor/mentee.
Peer mentoring: making sense of recovery
Positive outcomes were reported both by mentees and mentors. A key theme identified in the analysis was that of making sense of recovery through shared experiences and stories. This sharing was pivotal to the mentor–mentee relationship, with both parties expressing benefit. Through stories of their lived experience of injury and recovery, mentors were perceived as valued experts and could provide support in ways that were different from that provided by clinicians or family members. This position posed some challenges to mentors who required support to manage uncertainties inherent in their role. These findings are discussed below with supporting quotes.
Sharing stories
The essence of the peer mentoring intervention was to provide support from someone who had also experienced a TBI.
It was very useful to have someone who has been through a similar accident to myself. It really meant a lot to me. (Mentee: Peter, 24)
Telling your own story was a key device this programme used to establish credentials and facilitate the mentor–mentee relationship. The outcome of sharing these experiences was something mentees reflected on.
He wasn’t asking me questions, he was a story teller. And that made me, yeah rather than ‘how do you feel today?’ Is what they [the clinicians] asked me and I would go ‘oh yeah up and down like a rollercoaster I guess.’ He would go ‘oh yeah it’s hard to explain isn’t it?’ […]It was just, like you say, an occasion to go out.[…] And that’s what allowed me to have someone who’s a friendly expert, who had been through a brain injury, to connect with. (Mentee: Dave, 45)
Similarly, mentors found it more beneficial to share their stories with other peer mentors on the programme (as they had also had a TBI) than people around them. Opportunities for this arose during the training programme and debrief sessions, as these mentors explained:
It was like a process of opening up to people who have been through the same as yourself and I thought that was very helpful, just opening up and just letting it out rather than bottling it up. (Mentor: Thomas, 23)
Listening to what everyone else was saying sort of gave me great confidence that I wasn’t the only one. (Mentor: John, 59)
Mentors as experts
Returning home following discharge from rehabilitation is reportedly a difficult time as adjustments are made to changed circumstance. Mentees trusted their mentors and viewed them as experts because they had experienced a TBI and attended inpatient rehabilitation and were now actively participating in life roles.
Because he had been through it. I guess I am just new at this. He made it flow. He was like a brain injury guru. [….] Because he had lived it and physically trained in that field, by being run over on his bike. […] It was more progressively rehabilitating for me than [name of the rehab centre]. (Mentee: Dave, 45)
Even though mentors and mentees had different experiences of a TBI, they reported the sharing of experiences and stories enabled them to develop a connection, a sense of trust and in some cases a friendship.
It was like you had a connection maybe that was what it was, you have a connection. You have both been there and hearing what she had been through. (Mentee: Jane, 42)
Mentees reflected their mentor provided an opportunity to talk through concerns and worries with “someone who had been there”. This was viewed as different from the support provided by clinicians or family and friends. Using mentors as a sounding board helped mentees to make sense of their experiences and what could be expected after a TBI.
It was nice to have someone, outside your family. Because family are too close to you and they seem to like be over protective. Whereas your buddy [mentor] sort of understood where you were coming from, understood what you were going through. And it was nice to be able to ask like any questions that I had like ‘is this normal? I’m doing this is this, you know what’s going on here?’ And get those answers. (Mentee: Kate, 45)
The relationship between the pairs meant mentees felt comfortable sharing their experiences, and contributed to a sense of trust and a willingness to discuss their difficulties with more transparency than they might have with clinicians and family members. Kate suggested the relationship with her mentor enabled her to open up:
You become friends in the way that you can actually openly communicate to someone. That’s where it changed. So instead of being careful about what you say and you know being reserved, you could actually be totally open and honest with someone that’s not a psychologist. (Mentee: Kate, 45)
Much of the discussion between mentees and mentors reportedly included talking through issues they were reluctant to address with clinicians and believed their family members or friends did not understand. Mentors in turn revealed coping strategies they had found helpful for issues raised such as dealing with fatigue, thinking about return to ‘normal’ and discussions about how to cope with social pressures regarding alcohol consumption following TBI. Discussions of such matters appeared to be facilitated by the relationship not being bound by the systems and structures clinicians operate in and, unlike clinicians, mentors had more time to be with mentees either in their own home or in the community.
Mentors were conscious of their position and reported they were clear they were not acting as clinicians and recognised they had to have boundaries in terms of the advice they could offer.
But I shouldn’t be giving him medical advice you know. I can’t tell him what to do I can only tell him what I did […] I can talk to him about that [alcohol consumption] but in that situation it should be more as a friend […] because I don’t want him thinking I’ve got some profound knowledge about how your brain is going to affect your drinking after a year. (Mentor: Michael, 24)
Mentoring as a source of hope
Meeting and talking with mentors provided mentees with a sense of hope for progress beyond the difficulties they were facing immediately postdischarge and enabled them to build their self-confidence. The mentees reported feeling pleased to learn their mentors were now getting on with their lives and involved in activities such as university studies or returning to work.
Just how where he’s come from, from his accident until now. How he’s accomplished the things that he needs to do […] What it helped me is he’s back to work. And that’s where I want to be. (Mentee: Tony, 43)
Because it helps you feel like you are understood and you are not the only person going through this trouble but there have been other people who have gone through similar things who are able to show you a glimpse of hope that life gets better. (Mentee: Peter, 24)
The challenge of mentoring
Despite the mentees’ endorsement of the help and the inspiration of their personalising stories during the intervention period, the mentors struggled with their own expectations of the mentoring role. Some were concerned they needed more “tools to do the job properly” and were sometimes worried about the extent of the external support their mentee was receiving. Frequent contact with the research staff was important to discuss these concerns, to check in and ensure the mentee was safe, and to reassure the mentor that what they were offering their mentee was valuable in its own right and was in keeping with the intentions of the programme.
Watching some of the hard stuff he was going through and just kind of really bumming me out. […] Everybody felt a bit of a pressure, a responsibility to the person because we kind of get what it was like to go through what they went through and so you don’t want to fail the person you know. (Mentor: Michael, 24)
The valuable insights the mentors had into the challenges their mentees were experiencing that enabled them to establish connections and support their mentee presented challenges to the mentors as it prompted a revisiting of their own injury experiences and an acknowledgement of their persistent residual symptoms.
Just because, you know, you process your own head injury issues when you are mentoring someone […]. Sort of re thinking my own head injury and my own thing to kind of try and be useful to him. […] so some of that stress probably wasn’t at all out of my relationship with him, was actually to do with my own sort of. Because like you say, we are mentors because we have been through something that was kind of shit, you know, so we are thinking about that difficult thing pretty deeply. (Mentor: Michael, 24)
Although they experienced these pressures over their concern for their mentee’s situation and dealing with their own concerns, the mentors reported the support they received from the research team helped them deal with these and be effective in their role.
I think even when (mentee) started being, even when he started being a little bit depressed, having you guys to call and just chat through things and sort of, I had never really had a moment where I called you and no one answered or something like that. It was always, there was always contact there. (Mentor: Louis, 23)
Another challenge concerned the intended community activities and the planned time frames. These community activities were not always practical as some mentees had ongoing medical problems that restricted their mobility or lack of access to transport. Therefore, more mentor visits were at the mentees’ homes than proposed in the programme. Where community activities did occur, they typically included meeting up in a café or browsing shops together. Time frames were stretched by circumstances, for example surgery for associated injuries resulting in temporary mentee unavailability. Mentors were encouraged by the research team to use the programme flexibly in response to the mentees preference, which was considered a strength by many.
The peer mentoring was provided as a time-limited relationship, which for most mentors was not experienced as a problem as they felt their mentee had moved along in their recovery or that they had nothing more to offer as a mentor. However, for others, the consequence of the relationship being and becoming more personal created difficulty and concern about ending the series of sessions. These concerns were raised as a topic for discussion by mentors at each of the debriefing sessions, and mentors reported they needed this support in withdrawing from the formal mentoring relationship. Nevertheless, ending the mentoring relationship appeared to result in a sense of loss.
We did talk about, in the last session that we might see each other again, and then all of a sudden I am not a mentor anymore. (Mentor: Michael, 24)
Regardless, overall both the mentors and mentees reported the experience as beneficial. The opportunity to connect with others in a similar situation provided comradeship and a sense of hope:
I’ve just more than anything found like a friend. One that I can relate to. We have both had an injury.(Mentor: Sarah, 21)
The mentors all expressed enjoying their role and developed caring supportive relationships with their mentee. They appreciated the reciprocity the role offered them in the opportunity to give back and help someone.
I’d say it became a mutually beneficial relationship and one that to me meant a lot because it was, to me it was watching him recovering. (Mentor: Louis, 23)
Discussion
The findings of this study indicate the peer mentoring programme was perceived to be acceptable by both mentors and mentees. However, our experiences and that of our participants highlight a number of key lessons for future related work. For example, there is benefit to operationalising the intervention more flexibly than we initially intended. We found that a rigid approach to the number and frequency of community participatory activities is not always possible due to ongoing mentee health issues. Similarly, a 6-month time frame is more appropriate for a programme consisting of six sessions to allow for the complexity that mentees face postdischarge in re-engaging with their home life. Further, it is clear that mentors can sometimes require both practical support (eg, to get hold of their mentees and arrange times to meet) and emotional support (to help them navigate any emotional response they might have to sharing their story and re-engage with their own traumatic experiences in the sharing of those stories).
Although this study did not explicitly seek to explore programme benefits, both mentors and mentees reported a number of perceived benefits. We found that the peer mentoring relationship may be beneficial to both mentors and mentees through the sharing of experiences and stories, but also that mentors required support to manage the uncertainties inherent in the work. The time to talk and listen as well as the shared authentic experiences resonated with mentees, leading to feelings of hope and confidence as they re-engaged in life postdischarge to the community.
Just over a third of mentors approached and contactable took part in the study. This level of uptake could potentially impact on the feasibility of rolling this out to a larger study or service. However, given some declined due to other (immediate) commitments, it is possible that when mentoring is embedded in routine service delivery (without the time constraints associated with research) more people would come forward.
The strengths of this study include the use of qualitative interviews, which enabled an indepth exploration of the experiences of mentees and mentors engaged in a mentoring programme after TBI. The intervention was theory-based and developed incorporating both evidence and consumer (particularly Māori) involvement. An additional strength was the potential replicability of the study and delivering the mentoring face to face and in a way that was flexible to the needs of both mentors and mentees.
While mentors reported some challenges, this was mentors’ first experience of mentoring following TBI. Therefore, the benefits and challenges presented here may change in a larger trial where mentors have the opportunity to develop experience through supporting more than one mentee. Input into the study or intervention design was not sought from people with recent TBI at the time of commencing this research, which was a limitation. However, as noted in the methods, capturing their perspectives was a critical component of the current research so that they may inform refinement of the core processes (eg, mentor training, mentor support and intervention delivery) for future related work and peer mentoring service models.
We experienced other challenges. As noted above, two mentees did not complete the intervention, one did not stay in contact and the other had significant personal problems that precluded ongoing participation although was able to contribute to the qualitative data collection. Those who stayed in the study completed all sessions, which was a strength. Only four mentors recorded notes about their mentoring sessions. During the debrief sessions, it became apparent that taking such notes was often forgotten or perceived as not necessary. Future research should consider the best mechanisms for ongoing participation and capturing data about the content of sessions.
Since this was a small study, we were able to match on dyads gender only, although we also took into account shared interests. Ideally we would also have used the opportunity for matching by ethnicity, an important approach especially for Māori.46 We were also unable to pair by age or family circumstances due to the small mentor group. This resulted, for example, in one single mentor in their 20s mentoring a much older person with five children. Despite the limitations to our matching opportunities, the mentor–mentee pairs developed very good relationships, and their differences in age or life experience were not of relevance. This concurs with our previous longitudinal research with people with TBI, which has shown that assumptions should not be made concerning who would be the best match to provide mentorship.51
Our mentors had previously sustained a moderate to severe TBI. Although they initially appeared to be high-functioning, several had ongoing physical and cognitive difficulties while being part of our programme. For example, three required ongoing employment support, many experienced significant levels of fatigue and irritability, and not all had been able to return to driving. However, all were able to get to places to meet with their mentees and develop a meaningful relationship. Our findings suggest that even those who experience ongoing residual impairment following TBI are able to function well and safely in a mentoring role. Regardless, we are not able to comment on the potential mentoring ability of those with more severe residual impairment than our sample.
Mentors required more support from the research officer than anticipated at the outset of the study. For example, she supported them to maintain contact with their mentee during the study period, assisted with scheduling visits when they experienced difficulties and provided assistance with negotiating the university’s reimbursement procedures. The under-recognised need for this level of support was in part due to lack of evidence for delivering this service with this population and will inform future study design and service models.
Our exploration of mentees’ experiences should be considered in light of them taking part in a feasibility study. In addition, this was the first time each of our mentors had the opportunity to work with a mentee. Findings might be different if this had been a routine service or if mentors were more experienced in their role. This was a feasibility study and the findings are not designed to be transferable to other contexts; however, they have the potential to inform future peer mentoring intervention studies for people following TBI and point to the potentially reciprocal benefits of the mentoring relationship. A key feature of our study was the face-to-face delivery of the intervention. In the current study this was a culturally located decision, given this is a preferred method of service delivery for New Zealand Māori (the indigenous population of New Zealand). We also believe this to be a key component of this peer mentoring intervention and one that helped create opportunities for developing connections and building the relationship.
The stories our mentors used in their work with mentees were grounded in their own experiences of recovery and living with consequences of TBI. The actual sharing of these stories was a key component of the training workshops and debriefing sessions. Douglas and colleagues suggest that supportive relationships that promote this sense of being understood can facilitate people after injury to navigate their changed circumstances.52 Others have suggested that relating to other survivors acts as a source of self-cohesion in the process of identity reconstruction.13 Indeed, in our study, the sharing of stories helped both mentors and mentees realise they were not the only ones in this situation and not alone in what they were going through.
Mentees saw these stories as more authentic and more practically useful than receiving advice from clinicians. This is similar to the findings of Veith et al, where mentees saw professionals as forced into their life and as detached experts.23 Stories of people becoming more active after spinal cord injury recorded by actors have also been used in a study with people recently injured.53 Although they used a different delivery mechanism, people with spinal cord injury and healthcare staff considered the stories to be effective tools for communicating the message regarding re-engaging in activity after injury. They considered those in the stories to be credible messengers, who were emotionally realistic and provided context. Stories have also been shown to be key in the success of mentoring in a number of other settings, including mental health.25 54 In our study, the relationship that developed through this sharing led to mentees feeling able to express their concerns in a more honest and intimate way than perhaps would have occurred with clinicians.
We chose to use the terminology peer mentor over that of a layperson, since we concurred with others that there are distinctive differences. A peer is someone ‘who has had a comparable experience’ (p436).22 23 We do, however, acknowledge that the term ‘lay’ is also used in self-management literature as people who ‘commonly, but not invariably, themselves have a chronic disease, which may or may not be the same as that affecting programme participants’.55 We see the role of the mentor as different from that of a layperson in the community. This is because mentors share the same experience (of an injury and of the associated traumatic experience, for example) and can be part of created social networks. Mentors are also different from paraprofessionals, who are laypeople or lay-leaders who have received extensive training to deliver more structured and educational self-management programmes and have essentially become professionalised.24 55 This approach is akin to that employed by other peer mentoring programmes in which mentors received more education about TBI from a clinical perspective.32 34 56 There is no strong evidence that such training impacts on health status, which provided us with the rationale not to use this approach.55 Further, our approach to mentoring was largely informed by contemporary models of rehabilitation with a focus on participation as a key outcome of interest. A sociological approach could reveal different insights and could be explored in further work.
In our study mentees talked about a sense of hope that came from being with their mentors, hope for the future and hope of recovery. This potential outcome is distinct from other studies of peer mentoring after TBI.32–34 Hope or hopefulness as a potentially important outcome is considered in a conceptual analysis by Bright and colleagues.57 Our findings are similar to research in spinal cord injury, which showed that mentors helped newly injured people see future possibilities.26 The authors described this in the context of temporality and conceptualised disabled peer mentors as bridges in the temporal disruption of newly injured persons. Similarly, in a study with people on acute stroke units, hope was also identified as a key outcome of a peer mentoring programme.58
The mentoring relationship appeared to benefit the mentors by allowing them to be, and to be seen as, able to make a meaningful contribution, thus promoting a sense of self-value. Douglas and colleagues report on the social isolation frequently reported by people with TBI and describe rehabilitation as a ‘social-relational affair’ (p154).52 They suggest that through social interactions we build our sense of self, and that social interactions and expressive social support are essential elements for recovery after major injury.52 Similarly, qualitative accounts of the experience of recovery captured over 2 years following TBI support this notion that recovery is a social relational process where people draw support from others to make sense of recovery and life after TBI.19 This is consistent with concepts previously discussed by others, such as relational autonomy, where autonomy is argued to occur within and because of relationships.59 Peer mentoring is one approach that explicitly attends to this important aspect of recovery. This was indeed found to be the case in our study, with mentees re-engaging in activities with mentors’ support, such as contributing to activities within the church or leaving the home for a manicure or lunch.
Peer mentoring interventions are also located within disability rights and advocacy (eg, refs 60 61) as a way of recognising and using the expertise of those with experience of disabling TBI, and supporting a non-clinical approach to supporting people to engage in life post-TBI. However, our peer mentoring intervention was not specifically conceptualised in this way. Rather, as highlighted in the introduction, the intervention in the current study was underpinned by recognised gaps in service provision and informed by the experiences of people facing the enduring consequences of TBI. Likewise, there has been a recent interest in self-advocacy programmes for people with TBI and their families (eg, refs 62–64). Self-advocacy can be defined as ‘asserting your own needs and taking action to fulfil those needs’.62 Findings from such programmes are mixed but encouraging. One trial showed that advocacy behaviour improved both in a group taking part in a curriculum-based advocacy programme and one that was self-directed, and concluded that bringing like-minded motivated people with TBI together is more important than programme structure or content in changing advocacy behaviour.64 Similarly, the Self-Advocacy for Independent Life programme showed improvements in self-efficacy, satisfaction with life and goal attainment both for those who took part in a curriculum-based programme and those who only accessed a workbook.63 However, neither study had a control group that did not receive an intervention, and the latter study was very small (n=12). Further, peer advocacy or the role of peers in developing capability for self-advocacy was not explored in either study. Future research could consider the relevance of these findings for integration into TBI peer mentoring programmes.
In conclusion, peer mentoring in the early stages postdischarge appeared acceptable to people with TBI, both as mentees and mentors. Sharing experiences and stories seems key to successful peer mentee–mentor relationships after TBI and appeared to lead to benefits for mentees. This approach is suggested to augment rather than replace clinical input, providing something valuable and distinctly different. This qualitative study is a first step in a larger programme of work aiming to examine the efficacy of peer mentoring in TBI. Our future work will more explicitly include the involvement of people with TBI and their families in the study design, and build on the experiences and inputs shared by the mentees and mentors in the findings of this study.
Supplementary Material
Acknowledgments
The authors thank the mentors and study participants for taking part in the study and the staff at ABI Rehabilitation New Zealand (Auckland site) for supporting recruitment. The authors acknowledge the contribution made by other members of the research team who contributed to some aspects of the implementation of this project, but who are not named authors on this paper.
Footnotes
Contributors: PK conceived of the study, led on study design, project management, data analysis and dissemination. NK, KMcP, MW and HE contributed to study design. CC, NK and DB contributed to the qualitative data analysis, and MW and GS to the quantitative data analysis. CC, NK, DB, AF, KMcP, RJS, HE and GS contributed operationally (eg, training, recruitment, data collection, mentor support and debriefing). PK drafted the manuscript and is the guarantor. All authors revised it critically for important intellectual content and approved the final version for publication. All authors agree to be accountable for all aspects of the work.
Funding: This work was supported by the Health Research Council of New Zealand (grant number 13/759).
Disclaimer: The funding body has not had input into the design, data collection, analysis, interpretation of data, in the writing of the manuscript nor in the decision to submit the manuscript for publication.
Competing interests: PK, NK, HE, MW and KMcP had financial support from the Health Research Council of New Zealand for the submitted work. AF is an employee of ABI Rehabilitation New Zealand. Subsequent to the completion of this project and data analysis, KMcP became the Chief Executive of the Health Research Council of New Zealand.
Patient consent: Not required.
Ethics approval: Ethics approval was obtained from the New Zealand Health and Disability Ethics Committee (ref 13/NTA/99/AM05) and the university (ref 13/288).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Quantitative data from the study are not presented in the paper but can be obtained from the authors, subject to the funder’s permission.
References
- 1. Hyder AA, Wunderlich CA, Puvanachandra P, et al. . The impact of traumatic brain injuries: a global perspective. NeuroRehabilitation 2007;22:341–53. [PubMed] [Google Scholar]
- 2. Feigin VL, Theadom A, Barker-Collo S, et al. . Incidence of traumatic brain injury in New Zealand: a population-based study. Lancet Neurol 2013;12:53–64. 10.1016/S1474-4422(12)70262-4 [DOI] [PubMed] [Google Scholar]
- 3. Sendroy-Terrill M, Whiteneck GG, Brooks CA. Aging with traumatic brain injury: cross-sectional follow-up of people receiving inpatient rehabilitation over more than 3 decades. Arch Phys Med Rehabil 2010;91:489–97. 10.1016/j.apmr.2009.11.011 [DOI] [PubMed] [Google Scholar]
- 4. Levack WM, Kayes NM, Fadyl JK. Experience of recovery and outcome following traumatic brain injury: a metasynthesis of qualitative research. Disabil Rehabil 2010;32:986–99. 10.3109/09638281003775394 [DOI] [PubMed] [Google Scholar]
- 5. Andelic N, Stevens LF, Sigurdardottir S, et al. . Associations between disability and employment 1 year after traumatic brain injury in a working age population. Brain Inj 2012;26:261–9. 10.3109/02699052.2012.654589 [DOI] [PubMed] [Google Scholar]
- 6. Andelic N, Hammergren N, Bautz-Holter E, et al. . Functional outcome and health-related quality of life 10 years after moderate-to-severe traumatic brain injury. Acta Neurol Scand 2009;120:16–23. 10.1111/j.1600-0404.2008.01116.x [DOI] [PubMed] [Google Scholar]
- 7. Draper K, Ponsford J. Long-term outcome following traumatic brain injury: a comparison of subjective reports by those injured and their relatives. Neuropsychol Rehabil 2009;19:645–61. 10.1080/17405620802613935 [DOI] [PubMed] [Google Scholar]
- 8. Hofgren C, Esbjörnsson E, Sunnerhagen KS. Return to work after acquired brain injury: facilitators and hindrances observed in a sub-acute rehabilitation setting. Work 2010;36:431–9. 10.3233/WOR-2010-1039 [DOI] [PubMed] [Google Scholar]
- 9. Steel J, Youssef M, Pfeifer R, et al. . Health-related quality of life in patients with multiple injuries and traumatic brain injury 10+ years postinjury. J Trauma 2010;69:523–31. 10.1097/TA.0b013e3181e90c24 [DOI] [PubMed] [Google Scholar]
- 10. Grauwmeijer E, Heijenbrok-Kal MH, Haitsma IK, et al. . A prospective study on employment outcome 3 years after moderate to severe traumatic brain injury. Arch Phys Med Rehabil 2012;93:993–9. 10.1016/j.apmr.2012.01.018 [DOI] [PubMed] [Google Scholar]
- 11. Colantonio A, Ratcliff G, Chase S, et al. . Long-term outcomes after moderate to severe traumatic brain injury. Disabil Rehabil 2004;26:253–61. 10.1080/09638280310001639722 [DOI] [PubMed] [Google Scholar]
- 12. Doser K, Poulsen I, Wuensch A, et al. . Psychological outcome after severe traumatic brain injury in adolescents and young adults: The chronic phase. Brain Inj 2018;32:64–71. 10.1080/02699052.2017.1363408 [DOI] [PubMed] [Google Scholar]
- 13. Salas CE, Casassus M, Rowlands L, et al. . "Relating through sameness": a qualitative study of friendship and social isolation in chronic traumatic brain injury. Neuropsychol Rehabil 2018;28:1161–78. 10.1080/09602011.2016.1247730 [DOI] [PubMed] [Google Scholar]
- 14. Accident Compensation Corporation. ACC third quarterly report 2011-12, 2012. [Google Scholar]
- 15. Accident Compensation Corporation. ACC injury statistics 2008/2009. Section 15. Head claims. Secondary ACC injury statistics 2008/2009. Section 15. Head claims 2010. http://www.acc.co.nz/PRD_EXT_CSMP/groups/external_ip/documents/reports_results/wpc088577.pdf
- 16. Geurtsen GJ, van Heugten CM, Martina JD, et al. . Comprehensive rehabilitation programmes in the chronic phase after severe brain injury: a systematic review. J Rehabil Med 2010;42:97–110. 10.2340/16501977-0508 [DOI] [PubMed] [Google Scholar]
- 17. Ylvisaker M, Hanks R, Johnson-Greene D. Perspectives on rehabilitation of individuals with cognitive impairment after brain injury: rationale for reconsideration of theoretical paradigms. J Head Trauma Rehabil 2002;17:191–209. [DOI] [PubMed] [Google Scholar]
- 18. Carlson PM, Boudreau ML, Davis J, et al. . ’Participate to learn': a promising practice for community ABI rehabilitation. Brain Inj 2006;20:1111–7. 10.1080/02699050600955337 [DOI] [PubMed] [Google Scholar]
- 19. Fadyl JK, Theadom A, Channon A, et al. . Recovery and adaptation after traumatic brain injury in New Zealand: longitudinal qualitative findings over the first two years*. Neuropsychol Rehabil 2017:1–18. 10.1080/09602011.2017.1364653 [DOI] [PubMed] [Google Scholar]
- 20. Fadyl JK, Channon A, Theadom A, et al. . Optimising qualitative longitudinal analysis: insights from a study of traumatic brain injury recovery and adaptation. Nurs Inq 2017;24:e12170 10.1111/nin.12170 [DOI] [PubMed] [Google Scholar]
- 21. Malec JF, Hammond FM, Flanagan S, et al. . Recommendations from the 2013 galveston brain injury conference for implementation of a chronic care model in brain injury. J Head Trauma Rehabil 2013;28:476–83. 10.1097/HTR.0000000000000003 [DOI] [PubMed] [Google Scholar]
- 22. Ginis KA, Nigg CR, Smith AL. Peer-delivered physical activity interventions: an overlooked opportunity for physical activity promotion. Transl Behav Med 2013;3:434–43. 10.1007/s13142-013-0215-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Veith EM, Sherman JE, Pellino TA, et al. . Qualitative analysis of the peer-mentoring relationship among individuals with spinal cord injury. Rehabil Psychol 2006;51:289–98. 10.1037/0090-5550.51.4.289 [DOI] [Google Scholar]
- 24. Dennis CL. Peer support within a health care context: a concept analysis. Int J Nurs Stud 2003;40:321–32. 10.1016/S0020-7489(02)00092-5 [DOI] [PubMed] [Google Scholar]
- 25. MacNeil C, Mead S. A narrative approach to developing standards for trauma-informed peer support. Am J Eval 2005;26:231–44. 10.1177/1098214005275633 [DOI] [Google Scholar]
- 26. Papadimitriou C, Stone DA. Addressing existential disruption in traumatic spinal cord injury: a new approach to human temporality in inpatient rehabilitation. Disabil Rehabil 2011;33:2121–33. 10.3109/09638288.2011.555597 [DOI] [PubMed] [Google Scholar]
- 27. Haas BM, Price L, Freeman JA. Qualitative evaluation of a community peer support service for people with spinal cord injury. Spinal Cord 2013;51:295–9. 10.1038/sc.2012.143 [DOI] [PubMed] [Google Scholar]
- 28. Sherman JE, DeVinney DJ, Sperling KB. Social support and adjustment after spinal cord injury: influence of past peer-mentoring experiences and current live-in partner. Rehabil Psychol 2004;49:140–9. 10.1037/0090-5550.49.2.140 [DOI] [Google Scholar]
- 29. Parry M, Watt-Watson J. Peer support intervention trials for individuals with heart disease: a systematic review. Eur J Cardiovasc Nurs 2010;9:57–67. 10.1016/j.ejcnurse.2009.10.002 [DOI] [PubMed] [Google Scholar]
- 30. Bandura A. Social cognitive theory of self-regulation. Organ Behav Hum Decis Process 1991;50:248–87. 10.1016/0749-5978(91)90022-L [DOI] [Google Scholar]
- 31. Ryan RM, Deci EL. Self-regulation and the problem of human autonomy: does psychology need choice, self-determination, and will? J Pers 2006;74:1557–86. 10.1111/j.1467-6494.2006.00420.x [DOI] [PubMed] [Google Scholar]
- 32. Hanks RA, Rapport LJ, Wertheimer J, et al. . Randomized controlled trial of peer mentoring for individuals with traumatic brain injury and their significant others. Arch Phys Med Rehabil 2012;93:1297–304. 10.1016/j.apmr.2012.04.027 [DOI] [PubMed] [Google Scholar]
- 33. Struchen MA, Davis LC, Bogaards JA, et al. . Making connections after brain injury: development and evaluation of a social peer-mentoring program for persons with traumatic brain injury. J Head Trauma Rehabil 2011;26:4–19. 10.1097/HTR.0b013e3182048e98 [DOI] [PubMed] [Google Scholar]
- 34. Hibbard MR, Cantor J, Charatz H, et al. . Peer support in the community: initial findings of a mentoring program for individuals with traumatic brain injury and their families. J Head Trauma Rehabil 2002;17:112–31. [DOI] [PubMed] [Google Scholar]
- 35. Kolakowsky-Hayner SA, Wright J, Shem K, et al. . An effective community-based mentoring program for return to work and school after brain and spinal cord injury. NeuroRehabilitation 2012;31:63–73. 10.3233/NRE-2012-0775 [DOI] [PubMed] [Google Scholar]
- 36. Moreci G. A model system of traumatic brain injury peer support importance, development and process. NeuroRehabilitation 1996;7:211–8. 10.1016/1053-8135(96)00194-1 [DOI] [PubMed] [Google Scholar]
- 37. Hibbard MR, Cantor J. Evaluating the impact of a peer mentoring program for individuals with TBI and their families. Neurorehabilitation & Neural Repair 2005;19:388–9. [Google Scholar]
- 38. Morris RP, Fletcher-Smith JC, Radford KA. A systematic review of peer mentoring interventions for people with traumatic brain injury. Clin Rehabil 2017;31:1030–8. 10.1177/0269215516676303 [DOI] [PubMed] [Google Scholar]
- 39. Medical Research Council. Developing and evaluating complex interventions: new guidance. MRC, 2008. [Google Scholar]
- 40. Sandelowski M. Whatever happened to qualitative description? Res Nurs Health 2000;23:334–40. [DOI] [PubMed] [Google Scholar]
- 41. Sullivan-Bolyai S, Bova C, Harper D. Developing and refining interventions in persons with health disparities: the use of qualitative description. Nurs Outlook 2005;53:127–33. 10.1016/j.outlook.2005.03.005 [DOI] [PubMed] [Google Scholar]
- 42. Foster A, Buckley A, Cavit M. Acute and post-acute outcomes after moderate to severe traumatic brain injury: results from a comprehensive model of rehabilitation services. The 2011 New Zealand Rehabilitation Association Biennial Conference. Auckland, 2011. [Google Scholar]
- 43. Bright FA, Boland P, Rutherford SJ, et al. . Implementing a client-centred approach in rehabilitation: an autoethnography. Disabil Rehabil 2012;34:997–1004. 10.3109/09638288.2011.629712 [DOI] [PubMed] [Google Scholar]
- 44. Kayes NM, McPherson KM, Taylor D, et al. . Facilitators and barriers to engagement in physical activity for people with multiple sclerosis: a qualitative investigation. Disabil Rehabil 2011;33:625–42. 10.3109/09638288.2010.505992 [DOI] [PubMed] [Google Scholar]
- 45. McPherson KM, Kayes N, Weatherall M. Members of the Goals-SR Research Group. A pilot study of self-regulation informed goal setting in people with traumatic brain injury. Clin Rehabil 2009;23:296–309. 10.1177/0269215509102980 [DOI] [PubMed] [Google Scholar]
- 46. Mead HM. Tikanga Maori: living by Maori values. Wellington, Aotearoa New Zealand: Huia Publishers, 2003. [Google Scholar]
- 47. Greenwood A, Theadom A, Kersten P, et al. . Exploring researchers' experiences of working with people with acquired brain injury. Brain Inj 2015;29:592–600. 10.3109/02699052.2014.1002422 [DOI] [PubMed] [Google Scholar]
- 48. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277–88. 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- 49. Statistics New Zealand, 2014. 2013 Census QuickStats about culture and identity. http://www.stats.govt.nz
- 50. Hudson M, Milne M, Reynolds P, et al. . Te Ara Tika. Guidelines for Māori research ethics: a framework for researchers and ethics committee members. [Google Scholar]
- 51. McPherson K, Fadyl J, Theadom A, et al. . Living life after traumatic brain injury: phase 1 of a longitudinal qualitative study. J Head Trauma Rehabil 2018;33:E44–52. 10.1097/HTR.0000000000000321 [DOI] [PubMed] [Google Scholar]
- 52. Douglas J, Drummond M, Knox L, et al. . Rethinking social-relational perspectives in rehabilitation: traumatic brain injury as a case study : McPherson KM, Gibson BE, Leplege A, Rethinking rehabilitation theory and practice: CRC Press, 2015:137–62. [Google Scholar]
- 53. Smith B, Tomasone JR, Latimer-Cheung AE, et al. . Narrative as a knowledge translation tool for facilitating impact: translating physical activity knowledge to disabled people and health professionals. Health Psychol 2015;34:303–13. 10.1037/hea0000113 [DOI] [PubMed] [Google Scholar]
- 54. Jacobson N, Trojanowski L, Dewa CS. What do peer support workers do? A job description. BMC Health Serv Res 2012;12:205–05. 10.1186/1472-6963-12-205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Foster G, Taylor SJ, Eldridge SE, et al. . Self-management education programmes by lay leaders for people with chronic conditions. Cochrane Database Syst Rev 2007:CD005108 10.1002/14651858.CD005108.pub2 [DOI] [PubMed] [Google Scholar]
- 56. Struchen MA, West D, Cannon C, et al. ; Making connections after brain injury: a guide for social peer mentors. Houston, TX: Baylor College of Medicine, 2006. [Google Scholar]
- 57. Bright FA, Kayes NM, McCann CM, et al. . Understanding hope after stroke: a systematic review of the literature using concept analysis. Top Stroke Rehabil 2011;18:490–508. 10.1310/tsr1805-490 [DOI] [PubMed] [Google Scholar]
- 58. Kessler D, Egan M, Kubina LA. Peer support for stroke survivors: a case study. BMC Health Serv Res 2014;14:256–56. 10.1186/1472-6963-14-256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Ells C, Hunt MR, Chambers-Evans J. Relational autonomy as an essential component of patient-centered care. IJFAB: International Journal of Feminist Approaches to Bioethics 2011;4:79–101. 10.3138/ijfab.4.2.79 [DOI] [Google Scholar]
- 60. Disability Rights & Resources. Advancing independence: peer mentoring. http://www.disability-rights.org/?page_id=47.
- 61. Disability Rights UK, 2018. Peer support and mentoring https://www.disabilityrightsuk.org/how-we-can-help/special-projects/get-out-get-active/peer-support-and-mentoring.
- 62. Hawley LA. Self-advocacy for independent life: a program for personal self advocacy after brain injury. J Soc Work Disabil Rehabil 2016;15:201–12. 10.1080/1536710X.2016.1220885 [DOI] [PubMed] [Google Scholar]
- 63. Hawley L, Gerber D, Morey C. Improving personal self-advocacy skills for individuals with brain injury: a randomized pilot feasibility study. Brain Inj 2017;31:290–6. 10.1080/02699052.2016.1250952 [DOI] [PubMed] [Google Scholar]
- 64. Brown AW, Moessner AM, Bergquist TF, et al. . A randomized practical behavioural trial of curriculum-based advocacy training for individuals with traumatic brain injury and their families. Brain Inj 2015;29:1530–8. 10.3109/02699052.2015.1075173 [DOI] [PubMed] [Google Scholar]
- 65. New Zealand Guidelines Group. Traumatic brain injury: diagnosis, acute management and rehabilitation. Evidence-based best practice guideline produced for ACC. Wellington, New Zealand: ACC, 2006. [Google Scholar]
- 66. Department of Veterans Affairs and Department of Defense. VA/DoD clinical practice guideline for management of concussion/mild traumatic brain injury (mTBI. Washington, DC: Department of Veterans Affairs and Department of Defense, 2009. [Google Scholar]
- 67. Granger CV, Hamilton BB, Linacre JM, et al. . Performance profiles of the functional independence measure. Am J Phys Med Rehabil 1993;72:84–9. 10.1097/00002060-199304000-00005 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-020672supp001.pdf (230KB, pdf)